Supplemental Digital Content is available in the text
Keywords: Chinese herbal medicine, dyslipidemia, protocol, systematic review
Abstract
Background:
Dyslipidemia is commonly characterized by the abnormal quantity and quality of lipids in plasma, which is strongly associated with an increased risk of cardiovascular disease and also a major cause of morbidity and even leads to mortality. In China and East Asia, Chinese herbal medicine has been widely used to treat diverse diseases for thousands of years. As an important means of traditional Chinese medicine treatment, Chinese herbal medicine plays a more important role in the treatment of dyslipidemia. The aim of this study is to assess the efficacy and safety of Chinese herbal medicine for dyslipidemia.
Methods:
Seven electronic databases (included The Cochrane Library, MEDLINE, Embase, CNKI, VIP, CBM, and WANGFANG) will be searched regardless of publication date or language. Randomized controlled trials will be included if they recruited participants with dyslipidemia for assessing the effect of Chinese herbal medicine vs control (placebo, no treatment, and other therapeutic agents). Primary outcomes will include serum lipid and advent events. Two authors will independently scan the articles searched, extract the data from articles included, and assess the risk of bias by Cochrane tool of risk of bias. Disagreements will be resolved by discussion among authors. All analysis will be performed based on the Cochrane Handbook for Systematic Reviews of Interventions. Dichotomous variables will be reported as risk ratio or odds ratio with 95% confidence intervals (CIs) and continuous variables will be summarized as mean difference or standard mean difference with 95% CIs.
Results:
This review will be to assess the efficacy and safety of Chinese herbal medicine for dyslipidemia.
Conclusions:
Our findings will assist clinicians and health professionals make clinical decisions regarding dyslipidemia prevention, and promising way for prevention and treatment of patients with dyslipidemia.
Ethics and dissemination:
This study is a protocol for systematic review of Chinese herbal medicine as a treatment of dyslipidemia. This review will be published in a journal and disseminated in print by peer-review.
Systematic review registration:
PROSPERO (CRD42018085556).
1. Introduction
1.1. Disease burden of dyslipidemia
Dyslipidemia, defined as the abnormal quantity and quality of lipids in plasma, is strongly associated with an increased risk of cardiovascular disease (CVD) and also a major cause of morbidity and leads to mortality. Dyslipidemia is commonly characterized by low levels of high-density lipoprotein cholesterol (HDL-C) and high levels of triglyceride (TG), total cholesterol (TC), and low-density lipoprotein cholesterol (LDL-C).[1,2] Millions of people around the world are affected dyslipidemia.[3] It is estimated that prevalent cases of dyslipidemia in the 9 major countries will increase at the rate of 1.76% per year to surpass 500 million in 2022.[4] In China, with rapid economic growth and associated lifestyle changes, the level of dyslipidemia has gradually increased for nearly 30 years, the prevalence of dyslipidemia also increased significantly. According to a 2012 survey, the overall prevalence of dyslipidemia in Chinese adult is 40.40%, which has risen sharply compared to the result from 2002.[5] Recent data show that the prevalence of dyslipidemia levels in some areas has increased further,[6–9] unfavorable trends in lipid levels have occurred among adults.
Paradoxically, with the update of the guidelines for the control of dyslipidemia, more effective interventions and drugs were introduced and applied to clinic; however, the number of people with dyslipidemia has no reduction. Dyslipidemia abnormalities are still a very serious burden of disease affecting human health, more effort and effective strategies are required for the prevention.
1.2. Advantages of Chinese herbal medicine for the treatment of dyslipidemia
In clinical practice, a variety of therapeutic strategies for dyslipidemia were used, involved pharmacotherapy, lifestyle modification, liposuction and plasma exchange, etc. Stains are widely used as the 1st line drug for dyslipidemia, especially hypercholesterolemia, which is likely to achieve a reduction of TG and LDL-C. Although it is generally well-tolerated in most of patients with dyslipidemia, each lowering-lipid drug has certain side effects, such as statin may result in myalgias and muscle weakness, reduced energy, increased fatigue, liver enzyme elevations, worsening hyperglycemia, and risk of incident diabetes.[10] Along with the long-term treatment with statins in combination with other hypolipidemic drugs or alone, its safety and the medication compliance of patient had attracted a particular attention in clinic.[11] So more and more comprehensive strategy is required in clinical practice. Chinese herbal medicine is one of the most common treatment in traditional Chinese medicine (TCM), using the medicine derived from botanical sources to treat medical conditions. In China and East Asia, Chinese herbal medicine has been widely used to treat diverse diseases for thousands of years, and have been involved in dyslipidemia intervention for decades, which enriched the treatment of dyslipidemia greatly. The distinction between humans and experimental animals is that the human population is a total mixture, unlike selected batches of laboratory animals (same age, weight, sex, strain, etc).[9] Dyslipidemia is also the result of multiple factors, including intrinsic and extrinsic causes, such as age, diabetes, hypertension, body size, smoking status, family history, alcohol consumption, etc. The clinical manifestations of dyslipidemia are also complex, causing a variety of disorders, not only in terms of elevated serum lipid. For this reason, we need to take a holistic approach to different individuals and different qualities. This is fully consistent with the characteristics of TCM syndrome differentiation. As an important means of TCM treatment, Chinese herbal medicine plays a more important role in the treatment of dyslipidemia.
1.3. Reasons for doing the study
With the knowledge and accumulated practice passing from generation to generation, many herbs have been proven to have therapeutic effects on dyslipidemia, such as Radix Et. Rhizoma Rhei (Da Huang), Polygonum cuspidatum (Hu Zhang), Semen Cassia (Jue Ming Zi), Rhizoma Coptidis (Huang Lian), Scutellaria baicalensis (Huang Qin), Gynostemma pentaphylla (Jiao Gu Lan), Radix Puerariae (Ge Gen), Fructus Crataegi (Shan Zha), Fermentum Rubrum (Red Yeast Rice), Rhizoma Chuanxiong (Chuan Xiong), Radix Salviae Miltiorrhizae (Dan Shen), Rhizoma Curcumae Longae (Jiang Huang), Rhizoma Alismatis (Ze Xie), Semen Plantaginis (Che Qian Zi), Folium Nelumbinis (He Ye), Radix Astragali (Huang Qi), Radix Ginseng (Ren Shen), and Radix Polygoni Multiflori (He Shou Wu).[11–15] A total of 57 TCM formulas, including Long-Dan-Xie-Gan Tang, Wen-Dan Tang, Er-Chen-Tang and Xue-Fu-Zhu-Yu Tang, Wei-Ling TangYi-Guan-Jian and Qi-Ju-Di-Huang Wan, You-Gui-Wan and Shen-Ling-Bai-Shu San, etc, have been approved by the China Food and Drug Administration to treat hyperlipidemia.[13,14] Recently, many studies also demonstrated a favorable effect of Chinese herbal medicine for treating dyslipidemia.[16–19] However, no comprehensive evaluation have been reported in recent years. So we aim to gather the up-to-date information on Chinese herbal medicine for dyslipidemia and evaluate the potential benefits and harms of the use of Chinese herbal medicine, and move forward to help inform clinical decisions.
2. Methods and analysis
2.1. Objectives and registration
This review will be to assess the efficacy and safety of Chinese herbal medicine for dyslipidemia. This review protocol is registered in the International Prospective Register of Systematic Reviews (PROSPERO: CRD42018085556). Additionally, this review will adhere to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses Statement.[20]
2.2. Eligibility criteria
2.2.1. Types of studies
Randomized controlled trials (RCTs) will be included in this systematic review regardless of publication status and language. Quasi-randomized controlled trials (QRCTs) and nonrandomized studies will be excluded.
2.2.2. Types of participants
Participants with primary dyslipidemia, who were 18 years or older, were included regardless of their age, sex, or race if the diagnosis of dyslipidemia was made by “Screening and management of lipids” or any other reasonable criteria. Dyslipidemia was defined as high TC, high TGs, low high-density lipoprotein, and elevated LDL-C. Secondary dyslipidemia was excluded, which included diabetes, hypothyroidism, nephrotic syndrome, liver and gallbladder disease, and so on.
2.2.3. Patient and public involvement
In this study, there is no patient and public involvement in consideration of this protocol for a systematic review.
2.2.4. Types of interventions
All types of Chinese herbal medicine will be included. There is no limitation on the number of herbs, administration methods, dosage, or duration of treatment. The comparisons will be either with other therapeutic agents, such as statin and fibrate, or with no other treatment or placebo.
2.3. Types of outcome measures
The main outcome measures we sought at the end of treatment and at maximal follow-up after completion of the treatment were as follows.
2.3.1. Primary outcomes
-
1.
Serum lipid levels (including TC, TG, LDL-C, and HDL-C)
-
2.
Adverse events
2.3.2. Secondary outcomes
-
1.
Health-related quality of life
-
2.
Weight, body mass index, waist circumference, waist-to-hip ratio (WHR)
2.4. Search methods for the identification of studies
2.4.1. Electronic searches
We will search the following electronic databases regardless of publication date or language:
-
1.
The Cochrane Library
-
2.
MEDLINE
-
3.
Embase
-
4.
Chinese BioMedical Database (CBM)
-
5.
China National Knowledge Infrastructure (CNKI)
-
6.
Chinese VIP Information (VIP)
-
7.
Wangfang Database
2.4.2. Other sources
We will scan the reference lists of reviews and retrieve articles for additional studies. In addition, we will search Chinese Clinical Trials Registry (ChiCTR) (http://www.chictr.org.cn/), ClinicalTrials.gov (https://clinicaltrials.gov), and Google scholar (http://scholar.google.com).
2.4.3. Search strategy
We will model participant strategies for databases on the search MEDLINE and CNKI (see supplementary table). If this was the case, we would have modified electronic search strategies to incorporate these terms. We included studies published in any language.
2.5. Data collection and analysis
2.5.1. Selection of studies
To determine the studies to be searched further, 2 review authors (CHH and PF) will independently scan the titles and abstracts of all articles identified from electronic databases. Full-text articles will be scanned for all potentially relevant articles. If there is any disagreement on the selection of articles, they will be discussed with the 3rd author (YMY). The selection process will be shown in a Preferred Reporting Items for Systematic Review and Meta-analysis (PRISMA) flow chart (Fig. 1).
Figure 1.
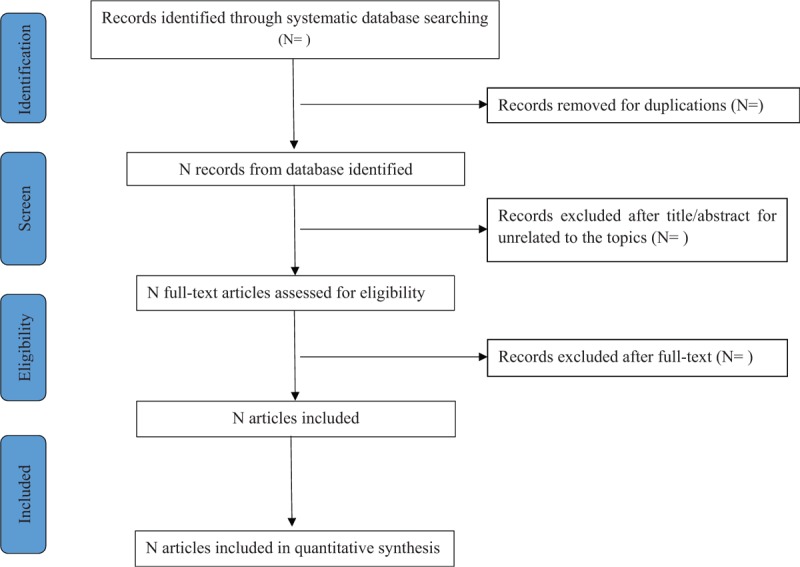
Flow chart of study selection.
2.5.2. Data extraction and management
For all studies included, 2 review authors (CHH and PF) will independently extract the relevant information using a standard data extraction table. Information will include publication of year, author, participants, intervention, control, duration of intervention, outcomes, and methodologic characteristics. Disagreements will be resolved by discussion by arbiter (LZX).
2.5.3. Assessment of the risk of bias in the included studies
The risk of bias will be assessed independently by 2 authors (CHH and PF) using the Cochrane tool of risk of bias (V.5.1.0). The following items will be assessed: random sequence generation (selection bias), allocation concealment (selection bias), blinding (performance bias and detection bias), incomplete outcome data (attrition bias), selective outcome reporting (reporting bias), and other bias. The judgments of evaluated domains will include high, low, and unclear. Disagreements will be resolved by discussion by arbiter (LZX).
2.5.4. Measurement of the treatment effect
Continuous variables will be reported as mean difference (MD) with 95% confidence intervals (CIs). For different measurement scales, standardized MD (SMD) analysis with 95% CI will be used, for example, TC and TG. Categorical variables will be summarized as risk ratios (RRs) or odds ratio (OR) with 95% CIs, for example, adverse event. All analysis will be performed based on the Cochrane Handbook for Systematic Reviews of Interventions.[21]
2.5.5. Units of analysis issues
All parallel-designed studies will be included in this review. For cross-over trials, only the 1st treatment period data will be analyzed. For studies with multiple control groups, the unit of analysis will be used to each of all control groups.
2.5.6. Dealing with missing data
For insufficient or missing data, we will contact the authors by e-mail or phone as much as possible. All analysis will be performed based on intent-to-treat principle.
2.5.7. Assessment of heterogeneity
Heterogeneity will be identified by visual inspection of the forest and tested by standard Chi-squared statistic and a significance level of 0.1. Additionally, the I2 statistic will be used to examine heterogeneity for quantifying inconsistency in the included studies. Fixed or random effects models will be performed in meta-analysis. If I2 >0.5, random effects models will be used.[21]
2.5.8. Assessment of reporting biases
Funnel plots will be used to assess the potential for small study bias if there are sufficient studies. Asymmetry of funnel plots will suggest possible small study effects and the results will be explained cautiously.[22,23]
2.5.9. Data synthesis
If there are sufficient studies and comparable outcomes, we will perform a meta-analysis using random effect modeling.
-
1.
Chinese herbal medicine vs conventional medical treatments
-
2.
Chinese herbal medicine vs no treatment
-
3.
Chinese herbal medicine vs placebo
-
4.
Chinese herbal medicine plus conventional medical treatment vs conventional medical treatment only
2.5.10. Subgroup analysis and investigation of heterogeneity
Subgroup analysis will be performed to explore the differences in the methodologic quality, subtypes of dyslipidemia, race/ethnicity, and types of herbal medicine.
2.5.11. Sensitivity analysis
Sensitivity analysis will be performed to test the robustness of findings if there are sufficient studies included. The factors on effect are as follows:
-
1.
Methodologic quality: analysis will be performed excluding studies of poor methodologic quality
-
2.
Published status: analysis will be performed excluding unpublished studies
-
3.
Sample size: analysis will be performed excluding small sample size studies
-
4.
Diagnostic criteria: analysis will be performed in studies of the same diagnostic criteria
-
5.
Race/ethnicity: analysis will be performed in studies of the same race or ethnicity
2.5.12. Confidence in cumulative evidence
In this study, the level of evidence on outcomes will be assessed using an approach based on the Grading of Recommendations Assessment, Development and Evaluation (GRADE). The quality of the body of evidence will be assessed based on 5 factors, including study limitations, effect consistency, imprecision, indirectness, and publication bias. The assessments will be categorized as high, moderate, low, and very low quality.
3. Discussion
The effective treatment of dyslipidemia is significant. Chinese herbal medicine has an advantage in treating dyslipidemia,[24] is able to help make up for the deficiency of current treatment, and is worth studying. The Cochrane Database of systematic reviews on dyslipidemia in 2011[18] and 2013[17] were focused on hypercholesterolemia and hypertriglyceridemia, respectively. All forms of dyslipidemia will be included in our review. We will summarize the available evidence for Chinese herbal medicine on dyslipidemia, and evaluate the effectiveness and the adverse effects of these treatments on dyslipidemia. Our findings may assist clinicians and health professionals make clinical decisions regarding dyslipidemia prevention, and promising way for prevention and treatment of patients with dyslipidemia. For the status of this study, we begin formal screening of search results against eligibility criteria.
3.1. Ethics and dissemination
Ethical approval is not required, in consideration of this protocol for a systematic review. In this study, there will be no participants recruited, and no data gathered from participants. This review will be disseminated by the approach of peer-reviewed publications.
Author contributions
LZX, YMY, CHH, and PF developed the study protocol. LZX, YMY, CHH, and PF developed the search strategy. CHH and PF will scan the included studies, extract the data and assess the risk of bias. LZX and YMY will act as an arbiter if there is any disagreement in this study. CHH and PF will perform data analysis with supervision of LZX. All authors (CHH, PF, KXZ, QX, YMY, and LZX) will contribute to data interpretation. CHH, PF, YMY, and LZX drafted and revised the manuscript. All authors have read and approved the final version of the manuscript.
Conceptualization: Caihong He, Peng Fu, Yunmei Yang, Liangzhen Xie.
Data curation: Caihong He, Peng Fu.
Formal analysis: Caihong He, Peng Fu, Liangzhen Xie.
Methodology: Liangzhen Xie.
Software: Qing Xia, Liangzhen Xie.
Supervision: Yunmei Yang, Liangzhen Xie.
Writing – original draft: Caihong He, Peng Fu.
Writing – review & editing: Kexin Zhang, Qing Xia, Yunmei Yang, Liangzhen Xie.
Supplementary Material
Footnotes
Abbreviations: CIs = confidence intervals, CVD = cardiovascular disease, HDL-C = high-density lipoprotein cholesterol, LDL-C = low-density lipoprotein cholesterol, MD = mean difference, OR = odds ratio, RR = risk ratio, SMD = standard mean difference, TC = total cholesterol, TCM = traditional Chinese medicine, TG = triglyceride.
CH and PF share first authorship.
This study was supported by Zhejiang Administration of Traditional Chinese Medicine (no: 2018ZA066).
The authors have no conflicts of interest to disclose.
Supplemental Digital Content is available for this article.
References
- [1].Sarzynski MA, Schuna JM, Jr, Carnethon MR, et al. Association of fitness with incident dyslipidemias over 25 years in the coronary artery risk development in young adults study. Am J Prev Med 2015;49:745–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Shenoy C, Shenoy MM, Rao GK. Dyslipidemia in dermatological disorders. N Am J Med Sci 2015;7:421–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Go A, Mozaffarian D, Roger V, et al. American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics - 2013 update: a report from the American Heart Association. Circulation 2013;129:e28–92.24352519 [Google Scholar]
- [4].Comanor WS, Scherer FM. Mergers and innovation in the pharmaceutical industry. J Health Econ 2013;32:106–13. [DOI] [PubMed] [Google Scholar]
- [5].Gao R, Zhao S, Lu G, et al. Guidelines for the prevention and treatment of dyslipidemia in Chinese adults (revised edition in 2016). Chinese Circulation Journal 2016;31:15–35. [Google Scholar]
- [6].Ni WQ, Liu XL, Zhuo ZP, et al. Serum lipids and associated factors of dyslipidemia in the adult population in Shenzhen. Lipids Health Dis 2015;14:71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Qi L, Ding X, Tang W, et al. Prevalence and risk factors associated with dyslipidemia in Chongqing, China. Int J Environ Res Public Health 2015;12:13455–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Sun GZ, Li Z, Guo L, et al. High prevalence of dyslipidemia and associated risk factors among rural Chinese adults. Lipids Health Dis 2014;13:189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Yang W, Xiao J, Yang Z, et al. Serum lipids and lipoproteins in Chinese men and women. Circulation 2012;125:2212–21. [DOI] [PubMed] [Google Scholar]
- [10].Li Y, Jiang L, Jia Z, et al. A meta-analysis of red yeast rice: an effective and relatively safe alternative approach for dyslipidemia. PLoS One 2014;9:e98611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Guo M, Liu Y, Gao ZY, et al. Chinese herbal medicine on dyslipidemia: progress and perspective. Evid Based Complement Alternat Med 2014;2014:163036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Bounda GA, Feng YU. Review of clinical studies of Polygonum multiflorum Thunb. and its isolated bioactive compounds. Pharmacognosy Res 2015;7:225–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Hu M, Zeng W, Tomlinson B. Evaluation of a crataegus-based multiherb formula for dyslipidemia: a randomized, double-blind, placebo-controlled clinical trial. Evid Based Complement Alternat Med 2014;2014:365742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Liu C, Huang Y. Chinese herbal medicine on cardiovascular diseases and the mechanisms of action. Front Pharmacol 2016;7:469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Wang M, Zhao R, Wang W, et al. Lipid regulation effects of Polygoni Multiflori Radix, its processed products and its major substances on steatosis human liver cell line L02. J Ethnopharmacol 2012;139:287–93. [DOI] [PubMed] [Google Scholar]
- [16].Liao J, Tian J, Li T, et al. Xuefuzhuyu decoction for hyperlipidemia: a systematic review and meta-analysis of randomized clinical trails. J Tradit Chin Med 2014;34:411–8. [DOI] [PubMed] [Google Scholar]
- [17].Liu ZL, Li GQ, Bensoussan A, et al. Chinese herbal medicines for hypertriglyceridaemia. Cochrane Database Syst Rev 2013;6:CD009560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Liu ZL, Liu JP, Zhang AL, et al. Chinese herbal medicines for hypercholesterolemia. Cochrane Database Syst Rev 2011;7:CD008305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Yao H, Zhang Z, Wang J, et al. Efficacy and safety of Yinchenwuling powder for hyperlipidemia: a systematic review and meta-analysis. J Tradit Chin Med 2016;36:135–43. [DOI] [PubMed] [Google Scholar]
- [20].Moher D, Shamseer L, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev 2015;4:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Higgins JP, Green S. Cochrane handbook for systematic reviews of interventions. Naunyn-Schmiedebergs Arch Exp Pathol Pharmakol 2008;5:S38. [Google Scholar]
- [22].Lau J, Ioannidis JPA, Terrin N, et al. The case of the misleading funnel plot. BMJ 2006;333:597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Sterne JA, Egger M, Smith GD. Systematic reviews in health care: Investigating and dealing with publication and other biases in meta-analysis. BMJ 2001;323:101–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Sham TT, Chan CO, Wang YH, et al. A review on the traditional Chinese medicinal herbs and formulae with hypolipidemic effect. Biomed Res Int 2014;2014:925302. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


