Abstract
Background and study aims Endoscopic treatment is the mainstay approach for gastrointestinal bleeding, in either upper (UGIB) or lower (LGIB) tract. The over-the-scope clip (OTSC) may overcome limitations of standard clips or thermocoagulation in high-risk bleeding lesions. We evaluate the main clinically relevant outcomes following endoscopic hemostasis with OTSC in high-risk lesions and/or patients.
Patients and methods This was a retrospective analysis of prospectively collected databases including all patients with UGIB and LGIB who underwent OTCS placement as first-line treatment in eleven tertiary endoscopic referral centers. Technical success, primary hemostasis, rebleeding, blood transfusion, hospital stay, and hemorrhage-related mortality rates were evaluated.
Results Data from 286 patients, with either UGIB (N = 214) or LGIB (N = 72) were available. Overall, 112 patients (39.2 %) were receiving antithrombotic therapy. Technical success and primary hemostasis rates were 97.9 % and 96.4 %, respectively. Early rebleeding occurred in 4.4 %, more frequently in those on antithrombotic therapy, and no late rebleeding was observed. Following a successful primary haemostasis, only 5.2 % patients needed blood transfusions, and the median hospital stay was 4 days (range: 3 – 11). Eighteen patients with either technical failure (N = 6) or rebleeding (N = 12) underwent radiological or surgical approaches. Overall, bleeding-related deaths occurred in 5 (1.7 %) patients, including 3 patients with technical procedural failure, and 2 in the rebleeding group.
Conclusions Data from our large, multicenter study show that OTSC placement is an effective first-line treatment for hemostasis in high-risk patients and/or lesions both in upper and lower gastrointestinal tract.
Introduction
Gastrointestinal bleeding, with an estimated annual incidence ranging from 20 to 172 cases per 100 000, frequently occurs in clinical practice 1 2 . The bleeding may originate from either the upper gastrointestinal tract (UGIB) or lower gastrointestinal tract (LGIB), with acute UGIB occurring four to six times more frequently than LGIB 3 4 . Gastrointestinal bleedings frequently lead to hospital admission, and are associated with morbidity and mortality, especially in the elderly patients 1 2 3 4 . Moreover, some patients develop a rebleeding episode, which is associated with increased mortality 5 . Endoscopic therapy was proven to be effective in stopping active gastrointestinal bleeding, also reducing risk of rebleeding, need for surgery, the number of erythrocytes units for transfusion, and length of hospital stay 6 .
Although endoscopic devices have been improved, achieving complete hemostasis still remains a challenge in those patients with complicated lesions, that is, severe bleeding from large vessels or large fibrotic ulcer. These patients, as well as those with endoscopic hemostasis failure, were generally treated with surgical or radiologic approaches 5 . For endoscopic hemostasis in these patients, use of over-the-scope clip (OTSC) was recently proposed. Indeed, emerging data support a role for such a device as both first-line and rescue endoscopic therapy in patients with non-variceal UGIB, and some data are available also for LGIB treatment 7 .
This multicenter study aimed to evaluate data from patients who underwent emergency endoscopy for either UGIB or LGIB in whom the OTSC was used as first-line therapy. The main clinically relevant outcomes were evaluated.
Patients and methods
Study patients and procedures
Data from all patients with UGIB or LGIB who were treated with OTSC as first-line therapy in 11 Italian tertiary Hospitals between 2014 and July 2017 were prospectively maintained in a specific database and retrospectively analyzed. The endoscopic procedures were performed by skilled operators under either anesthesiology-assisted deep sedation or midazolam sedation, according to the clinical condition of the patient. The decision to use an OTSC (Ovesco Endoscopy AG, Tubingen, Germany) as first-line endoscopic treatment depended on the endoscopist’s evaluation. Briefly, all high-risk patients and/or those with high-risk bleeding lesions were considered for such an approach. Patients on antithrombotic therapy and those with relevant comorbidities (heart, kidney, and hepatic impairment) were considered as high-risk. Bleeding lesions were classified as high-risk when at least one of the following conditions was present: lesion with bleeding artery or a vessel larger than 2 mm in diameter was visible; a lesion was deep penetrating, excavated or fibrotic in which presence of a microperforation could not completely be ruled out or thermal therapy could increase risk of perforation; and a lesion could not be safely treated by other endoscopic devices. Before the endoscopic procedure, written informed consent was obtained to the extent possible in emergency situations from patients or their family members. Because this was a retrospective study, no patient identification was involved, and no study-driven clinical intervention was performed, our Investigational Review Boards waived formal review and approval, deeming the study to be an extension of existing procedures.
Study outcomes
The measured outcomes were: 1) technical success defined as correct deployment of the device on the bleeding lesion; 2) primary hemostasis, defined as bleeding stopping without additional endoscopic treatments; 3) early (within 24 hours) or delayed (within 30 days) rebleeding rate; 4) management with non-endoscopic procedures following endoscopic failure; 5) need for blood transfusion post-procedure; 6) length of hospital stay; and 7) procedure-related 30-day mortality rate. A rebleeding episode was considered when hematemesis, melena, hematochezia, shock or loss of hemoglobin higher than 2 g/dL occurred within 24 hours. A second-look endoscopy was planned on demand, according to the endoscopist’s evaluation at the end of procedure.
Statistical analysis
Categorical variables are given as absolute and relative frequencies, and univariate analysis was performed by using the χ 2 test or the Fisher’s exact test, as appropriate. The 95 % confidence intervals (CI) were calculated. The Student’s t test for unpaired data was used for comparing age between different subgroups. A P value < 0.05 was considered statistically significant.
Results
Descriptive analysis
A total of 286 patients (mean age: 68 years, range: 28 – 89 years; M/F: 154/132) were treated during the study period. Overall, 112 patients (39.2 %) were receiving an antithrombotic (anticoagulant or antiplatelets) therapy. There were 214 (74.8 %) patients presenting with UGIB and 72 with LGIB. As compared to UGIB, patients with LGIB were significantly older (Mean age: 76 ± 11.7 vs 66 ± 10.2 years; P = 0.04), and were receiving more frequently antithrombotic therapy (52, 72.2 % vs 60, 28.1 %; P < 0.001), while no difference emerged in gender distribution (males: 56.9 % vs 53.8 %). Indications for OTSC treatment are reported in Table 1 . Peptic ulcers (gastric or duodenal) were the most frequent (131/214; 61.2 %) cause of bleeding in the UGIB patients, while post-endoscopic mucosal resection (EMR) or post-endoscopic submucosal dissection (ESD) bleeding was the main (47/72; 65.3 %) cause of LGIB. Overall, traumatic and non-traumatic OTSC clips were employed in 168 (58.7 %) and 118 (41.3 %) patients, respectively.
Table 1. Indications for endoscopic treatment in either upper (UGIB) or lower (LGIB) gastrointestinal bleeding patients.
| F1a | F1b | Spurting | Oozing | Patients | |
| UGIB (N = 214) | |||||
| Duodenal ulcer | 34 | 40 | 74 | ||
| Gastric ulcer | 24 | 33 | 57 | ||
| Mallory-Weiss lesion | 7 | 22 | 29 | ||
| Post-gastric ESD | 11 | 13 | 24 | ||
| Anastomosis | 10 | 9 | 19 | ||
| Dieulafoy lesion | 11 | 11 | |||
| LGIB (N = 72) | |||||
| Post-EMR | 9 | 16 | 25 | ||
| Post-ESD | 9 | 13 | 22 | ||
| Anastomosis | 8 | 11 | 19 | ||
| Diverticula | 4 | 4 | |||
| Rectal ulcer | 1 | 1 | 2 |
ESD, endoscopic submucosal dissection; EMR, endoscopic mucosal resection
Technical and clinical outcomes
Correct positioning of OTSC was successful in 280 cases, accounting for a technical success of 97.9 % (95 % CI = 96.2−99.6), while it failed in six patients with ulcers in either gastric body-fundus (3 cases) or posterior wall duodenal bulb (3 cases). Primary hemostasis was achieved in 270 patients (96.4 %; 95 % CI = 94.2−98.6) with a successful OTSC placement, while it failed in 10 patients treated for peptic ulcer (6 cases), post-mucosectomy bleeding (3 cases), and anastomotic bleeding (1 case). Early rebleeding occurred in 12 (4.4 %) patients who achieved primary hemostasis, and no late rebleeding was observed. Of note, patients with rebleeding were on antithrombotic therapy more frequently than those without it (12/12, 100 % vs 100/258, 38.8 %; P < 0.0001). Overall 14 (5.2 %) patients needed blood transfusions following a successful primary hemostasis, including 12 (100 %) and 2 (0.8 %) patients with or without rebleeding, respectively ( P < 0.001). These patients received median packed red cell units of 2 (range: 1 – 3). Median length of hospital stay was 4 days (3 – 11 days). All results are summarized in Fig. 1 and Table 2 .
Fig. 1.
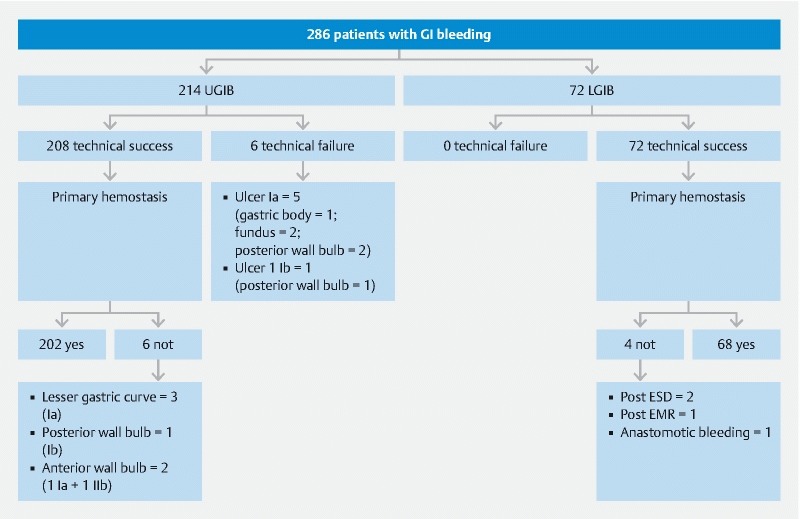
Main results of the study.
Table 2. Main outcomes following endoscopic treatment.
| Total (N = 286) | UGIB (N = 214) | LGIB (N = 72) | |
| Technical success (%) | 280 (97.9) | 208 (97.2) | 72 (100) |
| Primary hemostasis (%) 1 | 270 (96.4) | 202 (97.1) | 68 (94.4) |
| Early rebleeding (%) 2 | 12 (4.4) | 9 (4.5) | 3 (4.4) |
| Post-treatment blood trasfusion (%) | 14 (4.9) | 8 (3.7) | 6 (8.3) |
| Hospital stay, median (range); days | 4 (3 – 11) | 4 (2 – 10) | 4 (3 – 11) |
| Mortality (%) | 5 (1.9) | 4 (2) | 1 (1.5) |
UGIB, upper gastrointestinal bleeding; LGIB, lower gastrointestinal bleeding
Calculated in 280 patients who achieved technical success.
Calculated in 270 patients who achieved primary hemostasis.
Management of failure patients
Of the six patients with technical failure, four were treated with radiological arterial embolization and two with surgery (1 laparoscopic ulcer closure; 1 Whipple intervention). Of them, one and two patients who underwent surgical or radiological approach, respectively, died within 30 days. In the 10 patients with primary hemostasis failure, hemorrhage was successfully stopped by using an additional endoscopic technique in the same session (N = 4), radiological vascular embolization (N = 5), or surgery (N = 1). Finally, the 12 patients with early rebleeding were managed with epinephrine injection and/or endoscopic clip (N = 8) or radiological vascular embolization (N = 4). In this group, one patient died 8 days following vascular embolization, and another patient 22 days following surgical treatment performed after vascular embolization failure. Thus, a total of 5 patients (1.7 %; 95 % CI = 0.22−3.26) died within 30 days from procedure for a bleeding-related cause, including three of six patients following technical failure, and two of 12 with early rebleeding.
Discussion
Gastrointestinal bleeding is often a dramatic and potentially life-threatening event, particularly in the elderly and in patients with relevant comorbidities in whom a definite mortality rate has been reported 1 2 3 4 . An effective endoscopic procedure at the first attempt is clinically relevant not only for achieving stable primary hemostasis, but also for preventing rebleeding 5 . Endoscopic hemostasis is currently performed with different approaches, by using diverse devices 8 . Unfortunately, endoscopic thermocoagulation is able to consistently seal only small bleeding arteries (< 2 mm). On the other hand, application of standard hemostatic clips can be difficult in chronic ulcers with a fibrotic base or in lesions located in the posterior wall of the duodenal bulb or the lesser gastric curvature 9 . Moreover, these clips not infrequently dislodge, leading to recurrent bleeding. More than 10 years ago, the OTSC was introduced for endoscopic closure of gastrointestinal perforations, leaks, and fistulas by firmly approximating tissues 10 11 . Recently, OTSC has been proven to be effective in reducing complications (perforation and bleeding) when preventively positioned after ESD in the duodenum 12 . Few case series highlighted the usefulness of OTSC application also in patients with gastrointestinal bleeding 13 14 , allowing simultaneous sealing of the blood vessel and closure of the ulcer by compressing the surrounding tissue around the lesion. In a recent German study, OTSC application achieved a high success rate (92.4 %) in 118 patients with UGIB 15 . Our large, multicenter study found that OTSC is a valid hemostatic option as first-line therapy in both UGIB and LGIB patients. Indeed, it may be successfully applied in the vast majority of patients, with a procedure-related failure rate as low as 2.1 %, mainly including lesions localized in the gastric fundus or in the posterior wall of the duodenal bulb. Similarly, clinical success was impressively high when considering that primary hemostasis was achieved in more than 96 % of patients in whom the OTSC was correctly positioned.
Another clinically relevant finding was that only 5.2 % of patients needed blood transfusions following a successful primary hemostasis with OTSC, and that it was possible to discharge patients within few days (median: 4 days). This would suggest a firm and definitive closure of bleeding source with such a device. Of note, the early rebleeding rate was acceptably low (< 5 %), and it mainly occurred in patients on antithrombotic therapy in our study. Such a finding is consistent with the rebleeding rate ranging from 0 % to 22 % reported in other studies 7 , and with observation that rebleeding following OTSC placement occurs in up to 35 % of patients receiving antithrombotic therapy 16 . However, other studies failed to show that antithrombotic therapy was an independent factor of rebleeding in these patients 14 17 .
To our knowledge, this the largest, multicenter study on OTSC use for first-line therapy in fitting patients with either UGIB or LGIB. Indeed, a recent overview of data from the last decade found a total of 14 case series, mainly focused on UGIB, with a median of only 8 patients (range: 1 to 44) enrolled 13 . Overall, in these studies, clinical success rates ranged from 77.7 % to 100 % when OTSC was used as first-line therapy, with a rebleeding rate of 7.4 % to 13.6 % in the few series including more than 20 patients. Similar data were found in the most recent multicenter study 15 . In addition, preliminary data from a randomized study found that OTSC application was more effective than standard hemostasis (through-the-scope clip or thermal plus adrenaline) as rescue therapy in patients with peptic ulcer rebleeding 18 .
Data on OTSC as first-line treatment in LGIB patients are still scanty, with the largest series including only 22 cases 13 . Therefore, our data on 71 patients with LGIB could be regarded as particularly relevant. In our series, the most frequent causes of LGIB were those post-endoscopic or surgical procedures (EMR, ESD, and anastomosis). We observed that technical and clinical successes were similarly high in UGIB patients, suggesting that OTSC may also be used successfully in patients with lower gastrointestinal bleeding.
Finally, an overall bleeding-related mortality rate as low as 1.7 % was observed in our case series. This would appear consistent with the zero mortality reported in another study enrolling patients receiving antithrombotic therapy who were managed with OTSC placement as first-line treatment 14 . In our series, death occurred only in patients in whom the OTSC placement was impossible or who experienced rebleeding. Unfortunately, the fatal event happened despite the interventional radiology or surgical approaches that were performed. These observations would suggest that further therapeutic improvement is required in these patient subgroups.
Conclusion
In conclusion, data from our large, multicenter study found that OTSC placement is an effective first-line treatment for hemostasis in high-risk patients and/or who have lesions both in the upper and lower gastrointestinal tract. Therefore, cost-effectiveness studies are urged to establish whether this approach is cost-effective as compared to other endoscopic treatments.
Footnotes
Competing interests None
References
- 1.van Leerdam M E. Epidemiology of acute upper gastrointestinal bleeding. Best Pract Res Clin Gastroenterol. 2008;22:209–224. doi: 10.1016/j.bpg.2007.10.011. [DOI] [PubMed] [Google Scholar]
- 2.Hearnshaw S A, Logan R F, Lowe D et al. Acute upper gastrointestinal bleeding in the UK: patient characteristics, diagnoses and outcomes in the 2007 UK audit. Gut. 2011;60:1327–1335. doi: 10.1136/gut.2010.228437. [DOI] [PubMed] [Google Scholar]
- 3.Laine L, Yang H, Chang S C et al. Trends for incidence of hospitalization and death due to GI complications in the United States from 2001 to 2009. Am J Gastroenterol. 2012;107:1190–1195. doi: 10.1038/ajg.2012.168. [DOI] [PubMed] [Google Scholar]
- 4.Strate L L, Ayanian J Z, Kotler G et al. Risk factors for mortality in lower intestinal bleeding. Clin. Gastroenterol Hepatol. 2008;6:1004–1010. doi: 10.1016/j.cgh.2008.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gralnek I M, Dumonceau J M, Kuipers E J et al. Diagnosis and management of nonvariceal upper gastrointestinal hemorrhage: European Society of Gastrointestinal Endoscopy (ESGE) guideline. Endoscopy. 2015;47:1–46. doi: 10.1055/s-0034-1393172. [DOI] [PubMed] [Google Scholar]
- 6.Garber A, Jang S. Novel therapeutic strategies in the management of non-variceal upper gastrointestinal bleeding. Clin Endosc. 2016;49:421–424. doi: 10.5946/ce.2016.110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chan S M, Lau J YW. Can we now recommend OTSC as first-line therapy in case of non-variceal upper gastrointestinal bleeding? Endosc Int Open. 2017;05:E883–E885. doi: 10.1055/s-0043-111722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Beales I.Recent advances in the management of peptic ulcer bleeding F1000Research 201761763, (F1000 Faculty Rev) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Goelder S K, Brueckner J, Messmann H. Endoscopic hemostasis state of the art - nonvariceal bleeding. World J Gastrointest Endosc. 2016;8:205–211. doi: 10.4253/wjge.v8.i4.205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kirschniak A, Kratt T, Stüker D et al. A new endoscopic over-the-scope clip system for treatment of lesions and bleeding in the GI tract: first clinical experiences. Gastrointest Endosc. 2007;66:162–167. doi: 10.1016/j.gie.2007.01.034. [DOI] [PubMed] [Google Scholar]
- 11.Manta R, Caruso A, Cellini C et al. Endoscopic management of patients with post-surgical leaks involving the gastrointestinal tract: a large case series. United European Gastroenterol J. 2016;4:770–777. doi: 10.1177/2050640615626051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tashima T, Ohata K, 1, Sakai E et al. Efficacy of an over-the-scope clip for preventing adverse events after duodenal endoscopic submucosal dissection: a prospective interventional study. Endoscopy. 2018;50:487–496. doi: 10.1055/s-0044-102255. [DOI] [PubMed] [Google Scholar]
- 13.Manta R, Galloro G, Mangiavillano B et al. Over-the-scope clip (OTSC) represents an effective endoscopic treatment for acute GI bleeding after failure of conventional techniques. Surg Endosc. 2013;27:3162–3164. doi: 10.1007/s00464-013-2871-1. [DOI] [PubMed] [Google Scholar]
- 14.Richter-Schrag H J, Glatz T, Walker C et al. First-line endoscopic treatment with over-the-scope clips significantly improves the primary failure and rebleeding rates in high-risk gastrointestinal bleeding: a single-center experience with 100 cases. World J Gastroenterol. 2016;22:9162–171. doi: 10.3748/wjg.v22.i41.9162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wedi E, Fischer A, Hochberger J et al. Multicenter evaluation of first-line endoscopic treatment with the OTSC in acute non-variceal upper gastrointestinal bleeding and comparison with the Rockall cohort: the FLETRock study. Surg Endosc. 2018;32:307–314. doi: 10.1007/s00464-017-5678-7. [DOI] [PubMed] [Google Scholar]
- 16.Lamberts R, Koch A, Binner C et al. Use of over-the-scope clips (OTSC) for hemostasis in gastrointestinal bleeding in patients under antithrombotic therapy. Endoscopy International Open. 2017;05:E324–E330. doi: 10.1055/s-0043-104860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Brandler J, Buttar N, Baruah A et al. Efficacy of Over the Scope Clips in management of high-risk gastrointestinal bleeding. Clin Gastroenterol Hepatol. 2018;16:690–6960. doi: 10.1016/j.cgh.2017.07.020. [DOI] [PubMed] [Google Scholar]
- 18.Schmidt A, Goelder S, Messmann H et al. Over-the-scope-clips versus standard endoscopic therapy in patients with recurrent peptic ulcer bleeding. A prospective, randomized, multicenter trial (Sting) Gastroenterology. 2018;155:674–686. doi: 10.1053/j.gastro.2018.05.037. [DOI] [PubMed] [Google Scholar]


