Abstract
Background
The Pittsburgh Fatigability Scale (PFS) is the only validated scale for measuring perceived fatigability in older adults.
Aims
We validated the PFS Spanish version by assessing convergent validity with respect to several measures of physical performance, physical activity, physical function and disability.
Methods
A Cross-sectional validation study of 79 community-dwelling older adults aged 70 and older from Barcelona, Spain were included. Translation-retrotranslation was performed. Convergent validity was assessed in relation to physical activity and performance measurements, and analyzed with Spearman correlation coefficients, a linear trend test and non-linear regression. We also assessed the discriminant validity of the PFS physical score between participants with different physical activity and performance levels.
Results
Higher PFS physical scores were inversely associated with the Short Physical Performance Battery (r=−0.5, p<0.001) and weak to moderately correlated with gait speed (r=−0.38, p=0.001), and self-reported weekly walking time (r=−0.24, p=0.035).
Conclusion
The PFS is a novel, brief instrument to assess fatigability in Spanish-speaking older adults, with good convergent validity against physical performance measurements. Thus, the PFS can be used in Spanish speaking populations.
Keywords: fatigability, fatigue, validity, Spanish version
Introduction
Global fatigue is a common symptom in older adults, particularly in those with high comorbidity [1,2]. Perceived global fatigue refers to a subjective self-report of global tiredness and lack of energy, which leads to decreased physiological reserve, functional decline and disability [3–7] and it has been recognized as one of the key elements of frailty [8]. Fatigue can be the result of an inactive lifestyle, but can often be a symptom of underlying medical or psychiatric illnesses, or the result of medical treatments [4]. Prevalence rates vary widely across studies because of the lack of both consistent definitions and consensus on assessment tools. Currently, there are a number of available tools to evaluate fatigue, both self-reported and performance-based; however, no consensus about a gold standard measure has been reached [4].
The concept of fatigability-fatigue in relation to a defined activity of a specific intensity and duration, constitutes an objective metric to assess the degree to which someone is physically limited due to fatigue [3,4,9]. Measuring fatigability accounts for self-pacing bias and thus provides greater capacity to assess fatigue’s role in the disablement pathway. Recently, the Pittsburgh Fatigability Scale (PFS), a 10-item self-administered instrument designed to measure perceived physical and mental fatigability in older adults, was developed and validated [9]. PFS physical scores have shown good convergent validity against performance measures of mobility, physical function, and fitness, as well as good concurrent validity against performance-based measures of fatigability [9].
Given the emerging importance of measuring fatigability in older adults, its relation to declining function in this population [7], and the lack of a similar validated tool in Spanish, it is important to evaluate the validity of the PFS in Spanish community-dwelling older adults. The aim of this project was to validate the PFS Spanish version by assessing convergent validity against several measures of physical performance, physical activity, physical function and disability in a sample of inactive older adults.
Methods
Participants
We included all participants (N=79) from the randomized clinical trial “Exercise Park Equipment for Improving Physical Function and Physical Activity Levels in the Elderly” (NCT02375594), which compared a guided 3-month exercise program using public exercise equipment with a non-active control intervention. This study was approved by the Animal and Human Experimentation Ethics Committee of the Universitat Autonoma de Barcelona.
Community-dwelling older adults age 70 years and older were drawn from a convenient sample of older adults identified by General Practitioners, and were telephone screened for eligibility and willingness to participate. Enrollees had self-reported insufficient physical activity according to the optimal standards proposed by the World Health Organization (less than 30 minutes a day of moderate physical activity including leisure activities and travel, 5 days a week, or 30 minutes of vigorous physical activity three days a week) [10]. Eligibility also included preserved mobility (participant self-reported being able to walk 400m at a usual pace without help or only using a cane in 15 min, without needing to sit) [11]. Exclusion criteria included previous moderate and severe cognitive impairment; any moderate or severe chronic disease that precluded performing physical activity and inability to attend the intervention sessions or followup visits.
Linguistic Translation and Validation
The validated method of translation-retrotranslation was followed to obtain the final Spanish version of the PFS [12]. Two Spanish-speaking researchers independently translated the PFS into Spanish. Discrepancies were discussed and agreement was reached by consensus. Next, we assessed the preliminary version of the PFS with three independent native Spanish-speaking researchers, and their recommendations were considered when we derived the final version. We evaluated the proper understanding of the scale items by administering the PFS to two Spanish-older community-dwellers. To further check the fidelity against the original scale, the final Spanish version of the PFS was retro-translated into English by a bilingual researcher, and then translated and retrotranslated versions were checked for accuracy by an independent bilingual individual. After retro-translation, no additions changes were required. The final Spanish version of the PFS can be found as Supplementary data.
The PFS asks individuals to rate the level of physical and mental fatigue they would expect or imagine they would feel immediately after completing 10 different activities, and each statement is rated on a 6-point scale ranging from 0 (no fatigue) to 5 (extreme fatigue). Participants answer each item even if they have not performed the activity in the past month, and they are prompted to pay careful attention to the intensity and duration of each activity [9]. Due to the low educational level and advanced age of our sample, a member of the research team initially provided oral guidance on how to fill the questionnaire, and was available to clarify participants’ concerns, if needed. The scale comprises physical and mental fatigability scores, calculated by summing the ratings of the 10 items for physical and mental fatigue separately, with total scores ranging from 0 to 50 (higher score = higher fatigability). To date, only the original PFS physical score has been validated, so convergent validity and discrimination power were calculated only for this component of the PFS – Spanish version.
Other measures
Baseline socio-demographic characteristics (age, gender, marital status, education grade) were collected
The PFS – physical score Spanish version convergent validity was assessed for physical performance, physical activity, physical function and disability. Physical performance was assessed by the Short Physical Performance Battery (SPPB) test, a strong predictor of physical disability in older adults [13]. The SPPB includes the evaluation of balance, gait speed (m/sec), and chair stand performance (sec). The total score ranges from 0 (worst physical performance) to 12 (best performance) [13–16]. According to previous studies, poor physical performance was defined as SPPB< 10 points [14]. In order to obtain more information of each SPPB component, gait speed during a usual pace walk over 4-meters and chair stand performance (time to complete five chair stands without using the arms) were analyzed as independent variables. According to the literature, thresholds were set for gait speed and chair stand test. Gait speed ≤0.8m/sec was considered slow [17–19] and time >16.7 sec to performed the chair stand test or not be able to performed it was defined as low strength performance [13,14]. Physical activity was assessed by the self-report weekly walking time (WWT, hours/week). Low physical activity was defined according to WHO recommendations as WWT≤2.5 hours/week [20,21]. Physical function and disability were assessed by the Short Form Late Life Function and Disability Instrument (SF-LLFDI), which is a valid measure of functional limitations and disability in older adults [22]. The SF-LLFDI was developed as a selfreport instrument and it includes three subscales: one for functional assessment and two for disability (frequency and limitation) [23,24]. The function subscale is scored from 15 to 75 (maximal to minimal functional limitation) and both disability subscales range from 8 to 40 (severe to no disability) [23]. All data were collected at the baseline clinic visit prior to randomization.
Statistical analysis
We assessed convergent validity (degree to which two measures that theoretically should be related are related) of the Spanish version of the PFS physical score in relation to total SPPB, gait speed, chair stand time, WWT and the SF-LLFDI. Spearman correlation coefficients were analyzed and strength of correlations were interpreted as follows: <0.2: very weak correlation, 0.2-0.39: weak correlation, 0.4-0.59: moderate correlation and >0.6: strong correlation [25]. Reliability (internal consistency) of the final Spanish version of the PFS physical score was also measured using Cronbach’s alpha.
The least square means and standard error adjusted for age and gender, and the Area Under the Curve (AUC) were used to analyze the discriminant validity of the PFS physical score. Discriminant validity tests whether two measurements, not expected to be related are actually unrelated. In our study, this was assessed in order to evaluate the ability of the PFS physical score to differentiate between participants with good or normal vs. poor physical performance, faster or normal vs slower gait speed, good or normal vs low strength performance, and high or normal vs lower physical activity levels. The discriminant validity evaluated through the AUC was interpreted as follows: <0.6 not good, 0.6-0.7 poor, 0.7-0.8 fair, 0.8-0.9 good and 0.9-1.0 excellent.
Additionally, linear trend tests were used to explore the linear and non-linear relationships among PFS physical score and tertiles of SPPB, gait speed, chair stands, WWT and SF-LLFDI.
All statistical tests were conducted using the SPSS software ver. 22.0 (SPSS Inc., Chicago, IL, USA).
Results
Baseline characteristics of our population (mean age±SD = 77.21±5.0 years, 76% women) can be found in Table 1. Values for the physical fatigability score were distributed across the range of potential values, with no sign of ceiling or floor effects. The final Spanish version of the PFS physical score showed strong internal consistency, with a Cronbach’s alpha of 0.83.
Table 1.
Sample baseline characteristics.
| Characteristics | Total sample N=79 |
|---|---|
|
| |
| Age, years | 77.2 (5.0) |
|
| |
| Female, % (N) | 75.9 (60) |
|
| |
| Education level, % (N) | |
| Illiterate | 3.8% (3) |
| Can write | 5.1% (4) |
| Primary education | 48.1% (38) |
| Secondary education | 21.5% (17) |
| Graduate education | 21.5% (17) |
|
| |
| PFS physical score | 21.4 (8.7) |
|
| |
| High fatigability, % (N) | 79.7 (63) |
|
| |
| Total SPPB score (SD) | 7.9 (2.4) |
|
| |
| SSPB categories, % (N) | |
| 0–3 points | 7.7% (6) |
| 4–6 points | 7.7% (6) |
| 7–9 points | 57.7% (45) |
| 10–12 points | 25.6% (20) |
|
| |
| Gait speed (m/sec) | 0.7 (0.2) |
|
| |
| Slow gait speed, % (N) | 67.1% (51) |
|
| |
| Chair stand test time (seconds) | 15.1 (7.3) |
|
| |
| Lower strength performance, % (N) | 55.8% (43) |
|
| |
| Weekly Walking Time (hours/week) | 3.4 (2.9) |
|
| |
| SF-LLFDI disability | |
| Disability limitation | 34.3 (5.2) |
| Disability frequency | 30.0 (5.2) |
|
| |
| SF-LLFDI function | 54.2 (9.9) |
Values are presented in % (N) and mean (SD) for categorical and continuous variables respectively. PFS: Pittsburg Fatigability Score, high fatigability PFS ≥15. SPPB: Short Physical Performance Battery, low physical performance SPPB≤10. Slow gait speed≤ 0.8m/sec. Lower strength performance: time to performed chair stand test ≥ 16.7seconds or not able to perform it. SF-LLFDI: Short Form Late Life Function and Disability Instrument.
The PFS physical score showed a moderate to strong negative correlation with physical function and disability scale (SF-LLFDI disability and function scores), a weak to moderate negative correlation with physical performance measures (moderate correlation with total SPPB score and weak correlation with gait speed and chair stand tests) and a weak correlation with physical activity measurement (WWT), Table 2.
Table 2.
Convergent validity of Spanish version of the PFS physical score.
| Characteristics | PFS Physical
|
|
|---|---|---|
| Spearman correlation | p value | |
|
| ||
| Age, years | 0.13 | 0.266 |
|
| ||
| Total SPPB score | −0.50 | <0.001 |
|
| ||
| Gait speed (m/sec) | −0.38 | 0.001 |
|
| ||
| Chair stand test time (sec) | −0.15 | 0.203 |
|
| ||
| Weekly Walking Time (hours/week) | −0.24 | 0.035 |
|
| ||
| SF- LLFDI disability | ||
| Disability limitation | −0.55 | <0.001 |
| Disability frequency | −0.40 | <0.001 |
|
| ||
| SF-LLFDI function | −0.72 | <0.001 |
SPPB: Short Physical Performance Battery. SF-LLFDI: Short Form Late Life Function and Disability Instrument.
Moreover, the PFS physical score showed moderate ability to discriminate between higher and lower levels of physical performance measures (SPPB total score and chair stand test). However, the ability to discriminate those participants with high or normal vs. low physical activity was low. Nevertheless, physical fatigability was lower in subgroups of participants with high functional levels as assessed by least square-means of the PFS physical score, with differences between 3.1 and 7.9, Table 3.
Table 3.
Discriminat validity of the PFS physical score – Spanish version with physical performance and physical activity measures.
| Measures | PFS Physical Score | ||||
|---|---|---|---|---|---|
| LS means (SE)a | Difference | AUC | |||
| Yes | No | Mean (SE) | 95%CI | ||
| Poor physical performance b | 23.5(1.0) | 15.6(1.2) | 7.9(0.3) | 7.3-8.5 | 0.77 |
| Slow gait speed c | 23.1(1.2) | 17.5(1.1) | 5.6(0.3) | 5.0-6.2 | 0.69 |
| Low strength performance d | 24.1(0.9) | 16.4(1.1) | 7.6 (0.3) | 7.0-8.2 | 0.79 |
| Low physical activity e | 23.1(1.1) | 20.2(1.7) | 3.1(0.3) | 2.5-3-7 | 0.64 |
LS means: Least squares means, SE: Standard Error, AUC: Area Under the Curve.
Adjusted by age and gender.
Defined as Short Physical Performance Battery (SPPB) <10 points.
Defined as low gait speed: gait speed ≤0.8 m/sec during a walk at usual pace over 4-meters.
Defined as time to performed chair stand test ≥16.7 seconds or not able to do 5 stands.
Defined as weekly walking time ≤2.5hours/week.
Finally, physical fatigability score showed a linear trend, with higher PFS scores for participants with low SPPB score, slow gait speed and higher functional limitation and disability according to SF-LLFDI, Figure 1.
Figure 1. Linear trend among the Spanish version PFS physical score and physical performance, physical activity and disability measures stratified by tertiles.
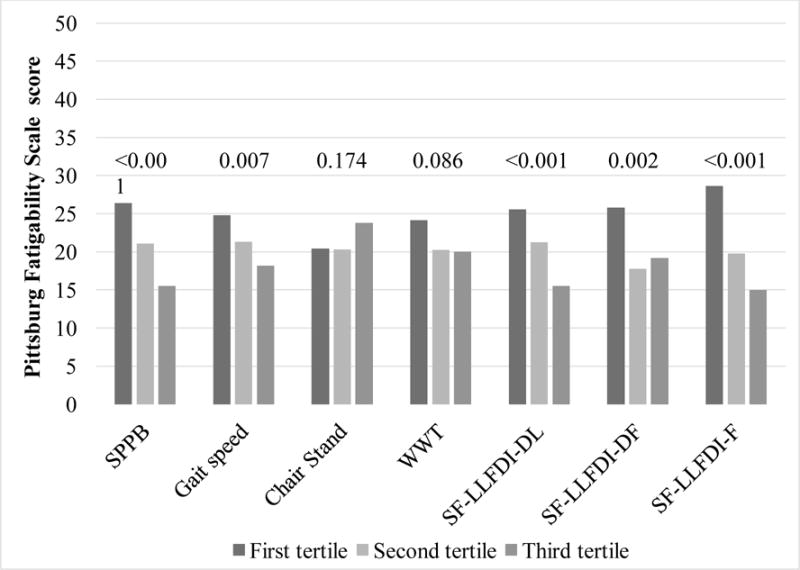
SPPB: Short Physical Performance Battery, WWT: Weekly Time Walking, SF-LLFDI-DL: Short Form Late Life Disability Instrument-Disability Limitation sub-scale, SF-LLFDI-DF: Short Form Late Life Disability - Disability Frequency, SF-LLFDI-F: Short Form Late Life Disability – Function sub-scale.
Discussion
Our study findings indicate that the Spanish version of the PFS is a valid, easy to use measurement of perceived physical fatigability in Spanish older adults. The PFS physical score has moderate to good convergent validity. Additionally, physical and functional performance was associated with lower physical fatigability.
The aging population phenomena and the increase in Spanish-speaking populations worldwide reinforce the need for Spanish translations of reliable tests to helps clinicians assess this growing population group. Fatigue and exhaustion have been recognized as one of the key elements of frailty [8], a symptom highly prevalent in older adults. Additionally, perceived fatigability assessment in older adults is becoming increasingly important due to its close relationship to frailty [26]. However, until now, available fatigability tools were developed and targeted to assess this symptom mainly in younger populations, with specific pathologies and without adjustment for physical activity or age. Thus, the PFS development takes a step forward and responds to the need to assess activity-anchored fatigue in older adults in clinical and research settings. Currently, the PFS is the only self-report validated instrument to measure perceived physical fatigability that takes into account a wide spectrum of activities usually performed by older populations.
The PFS physical score has previously demonstrated high concurrent validity and strong convergent validity against both functional and physical performance measures, including physical activity measurements such as 400 meters long distance corridor walk test, five chair stand test and gait speed [9]. The differences between the results shown by Glynn et al. and our study, may be explained by the differences between both samples in sample size, our sample was smaller, and socio-demographic characteristics, our population was older. However, there were also important differences in baseline physical activity performance, while our population was insufficiently active, 45.3% of participants in the original development sample, and 58.0% in the validation sample, performed moderate to vigorous physical activity.
Our study has some limitations: first, the small number of participants. Second, participants were insufficiently active and interested in taking part of a clinical trial, so this may have biased the results towards a specific group population among older adults, not a general elderly population. Main strengths include the rigorous methodology to translate the PFS and the assessment of convergent validity across a wide variety of objective measurements. Finally, it is the first scale developed and validated to assess fatigability in Spanish older adults.
In conclusion, the Spanish version of the PFS is a convenient and valid tool to assess perceived fatigability in Spanish older adults and it has strong convergent validity against physical and functional performance measurements. This is an important step, to improve the evaluation of perceived fatigability impact in Spanish-speaking older adults, which represent a growing population. This study has opened up the possibility of including an area of research through considering perceived fatigability as a predictor variable or an outcome measure in intervention studies.
Supplementary Material
Acknowledgments
Rosario Jimenez, Esperança Palacios and Palmira Villafuerte of the ABS Vallcarca-Sant Gervasi for their help in conducting the clinical trial and assessments. Jordi González-Guerra and Irene Garcia for their help in conducting the interviews. Àlex Domingo, Gabriela del Valle Gómez, Cristina Puchol, Ignasi Bolibar, Alejandro Carrera Rodriguez for their help in the translation procedure of the Spanish version of the PFS.
Funding
Funding sources: The sub-study is part of a clinical trial “Exercise Park Equipment for Improving Physical Function and Physical Activity Levels in the Elderly” (NCT02375594) that had partial funding by Lappset España - Lappset Group Oy. The NCT02375594 clinical trial sponsor had no role in conducting the analyses, interpreting or reviewing the data included in this paper.
The original Pittsburgh Fatigability Scale development and validation was funded by a Pittsburgh Claude D. Pepper Older Americans Independence Center Developmental Pilot Grant NIH P30 AG024826 and also from the Intramural Research Program, National Institute on Aging, National Institutes of Health.
Footnotes
ORCID ID: 0000-0003-3152-9882
Conflicts of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
References
- 1.Swain MG. Fatigue in chronic disease. Clin Sci (Lond) 2000;99:1–8. [PubMed] [Google Scholar]
- 2.Meng H, Hale L, Friedberg F. Prevalence and predictors of fatigue in middle-aged and older adults: evidence from the health and retirement study. J Am Geriatr Soc. 2010;58:2033–4. doi: 10.1111/j.1532-5415.2010.03088.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Eldadah BA. Fatigue and Fatigability in Older Adults. PM R. 2010;2:406–413. doi: 10.1016/j.pmrj.2010.03.022. [DOI] [PubMed] [Google Scholar]
- 4.Alexander NB, Taffet GE, Horne FM, Eldadah BA, Ferrucci L, Nayfield S, Studenski S. Bedside-to-bench conference: Research agenda for idiopathic fatigue and aging. J Am Geriatr Soc. 2010;58:967–975. doi: 10.1111/j.1532-5415.2010.02811.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Basu N, Yang X, Luben RN, Whibley D, Macfarlane GJ, Wareham NJ, Khaw KT, Myint PK. Fatigue is associated with excess mortality in the general population: results from the EPIC-Norfolk study. BMC Med. 2016;14:122. doi: 10.1186/s12916-016-0662-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Richardson CA, Glynn NW, Ferrucci LG, Mackey DC. Walking energetics, fatigability, and fatigue in older adults: The study of energy and aging pilot. Journals Gerontol - Ser A Biol Sci Med Sci. 2015;70:487–494. doi: 10.1093/gerona/glu146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Simonsick EM, Glynn NW, Jerome GJ, Shardell M, Schrack JA, Ferrucci L. Fatigued, but Not Frail: Perceived Fatigability as a Marker of Impending Decline in Mobility-Intact Older Adults. J Am Geriatr Soc. 2016;64:1287–1292. doi: 10.1111/jgs.14138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, Seeman T, Tracy R, Kop WJ, Burke G, McBurnie MA. Cardiovascular Health Study Collaborative Research Group, Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;56:M146–56. doi: 10.1186/s12877-015-0078-0. [DOI] [PubMed] [Google Scholar]
- 9.Glynn NW, Santanasto AJ, Simonsick EM, Boudreau RM, Beach SR, Schulz R, Newman AB. The Pittsburgh fatigability scale for older adults: Development and validation. J Am Geriatr Soc. 2015;63:130–135. doi: 10.1111/jgs.13191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.World Health Organization. Global recommendations on physical activity for health. Geneva: 2010. [PubMed] [Google Scholar]
- 11.Pahor M, Blair S, Espeland M, Fielding R, Gill T, Guralnik J, Hadley E, King A, Kritchevsky S, Maraldi C, Miller M, Newman A, Rejeski W, Romashkan S, Studenski S. Effects of a Physical Activity Intervention on Measures of Physical Performance: Results of the Lifestyle Interventions and Independence for Elders Pilot (LIFE-P) Study. Journals Gerontol Ser A Biol Sci Med Sci. 2006;61:1157–1165. doi: 10.1093/gerona/61.11.1157. [DOI] [PubMed] [Google Scholar]
- 12.Beaton DE, Bombardier C, Guillemin F, Ferraz MB. Guidelines for the process of cross-cultural adaptation of self-report measures. Spine (Phila Pa 1976) 2000;25:3186–91. doi: 10.1097/00007632-200012150-00014. [DOI] [PubMed] [Google Scholar]
- 13.Guralnik JM, Ferrucci L, Simonsick EM, Salive ME, Wallace RB. Lower-extremity function in persons over the age of 70 years as a predictor of subsequent disability. N Engl J Med. 1995;332:556–61. doi: 10.1056/NEJM199503023320902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cabrero-García J, Muñoz-Mendoza CL, Cabañero-Martínez MJ, González-Llopís L, Ramos-Pichardo JD, Reig-Ferrer A. Valores de referenda de la Short Physical Performance Battery para pacientes de 70 y más años en atención primaria de salud. Aten Primaria. 2012;44:540–548. doi: 10.1016/j.aprim.2012.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Guralnik JM, Simonsick EM, Ferrucci L, Glynn RJ, Berkman LF, Blazer DG, Scherr PA, Wallace RB. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994;49:M85–94. doi: 10.1093/geronj/49.2.m85. [DOI] [PubMed] [Google Scholar]
- 16.Studenski S, Perera S, Patel K, Rosano C, Faulkner K, Inzitari M, Brach J, Chandler J, Cawthon P, Connor EB, Nevitt M, Visser M, Kritchevsky S, Badinelli S, Harris T, Newman AB, Cauley J, Ferrucci L, Guralnik J. Gait speed and survival in older adults. JAMA. 2011;305:50–58. doi: 10.1001/jama.2010.1923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Abellan van Kan G, Rolland Y, Andrieu S, Bauer J, Beauchet O, Bonnefoy M, Cesari M, Donini LM, Gillette Guyonnet S, Inzitari M, Nourhashemi F, Onder G, Ritz P, Salva A, Visser M, Vellas B. Gait speed at usual pace as a predictor of adverse outcomes in community-dwelling older people an International Academy on Nutrition and Aging (IANA) Task Force. J Nutr Health Aging. 2009;13:881–9. doi: 10.1007/s12603-009-0246-z. [DOI] [PubMed] [Google Scholar]
- 18.Cruz-Jentoft AJ, Baeyens JP, Bauer JM, Boirie Y, Cederholm T, Landi F, Martin FC, Michel JP, Rolland Y, Schneider SM, Topinková E, Vandewoude M, Zamboni M. European Working Group on Sarcopenia in Older People, Sarcopenia: European consensus on definition and diagnosis: Report of the European Working Group on Sarcopenia in Older People. Age Ageing. 2010;39:412–23. doi: 10.1093/ageing/afq034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lauretani F, Russo CR, Bandinelli S, Bartali B, Cavazzini C, Di Iorio A, Corsi AM, Rantanen T, Guralnik JM, Ferrucci L. Age-associated changes in skeletal muscles and their effect on mobility: an operational diagnosis of sarcopenia. J Appl Physiol. 2003;95:1851–60. doi: 10.1152/japplphysiol.00246.2003. [DOI] [PubMed] [Google Scholar]
- 20.Martinez-Gonzalez MA, Lopez-Fontana C, Varo JJ, Sanchez-Villegas A, Martinez JA. Validation of the Spanish version of the physical activity questionnaire used in the Nurses’ Health Study and the Health Professionals’ Follow-up Study. Public Heal Nutr. 2005;8:920–927. doi: 10.1079/phn2005745. doi: S1368980005001230 [pii] [DOI] [PubMed] [Google Scholar]
- 21.Craig CL, Marshall AL, Sjöström M, Bauman AE, Booth ML, Ainsworth BE, Pratt M, Ekelund U, Yngve A, Sallis JF, Oja P. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2003;35:1381–95. doi: 10.1249/01.MSS.0000078924.61453.FB. [DOI] [PubMed] [Google Scholar]
- 22.Denkinger MD, Igl W, Coll-Planas L, Bleicher J, Nikolaus T, Jamour M. Evaluation of the short form of the late-life function and disability instrument in geriatric inpatients-validity, responsiveness, and sensitivity to change. J Am Geriatr Soc. 2009;57:309–14. doi: 10.1111/j.1532-5415.2008.02095.x. [DOI] [PubMed] [Google Scholar]
- 23.Abizanda P, López-Jiménez M, López-Torres J, Atienzar-Núñez P, Naranjo JM, McAuley E. Validation of the Spanish version of the short-form late-life function and disability instrument. J Am Geriatr Soc. 2011;59:893–899. doi: 10.1111/j.1532-5415.2011.03392.x. [DOI] [PubMed] [Google Scholar]
- 24.McAuley E, Konopack JF, Motl RW, Rosengren K, Morris KS. Measuring disability and function in older women: psychometric properties of the late-life function and disability instrument. J Gerontol A Biol Sci Med Sci. 2005;60:901–9. doi: 10.1093/gerona/60.7.901. [DOI] [PubMed] [Google Scholar]
- 25.Swinscow TDV. MJ (University of S Campbell (Ed), Stat Sq One. 9th. BMJ Publishing Group; 1997. Correlation and regression. [Google Scholar]
- 26.Schnelle JF, Buchowski MS, Ikizler TA, Durkin DW, Beuscher L, Simmons SF. Evaluation of Two Fatigability Severity Measures in Elderly Adults. J Am Geriatr Soc. 2012;60:1527–1533. doi: 10.1111/j.1532-5415.2012.04062.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


