Abstract
Purpose
This study explored the performance of the Patient Reported Outcomes Measurement Information System (PROMIS) Anxiety assessment relative to the Depression assessment in orthopedic patients, the relationship between Anxiety with self-reported Physical Function and Pain Interference, and to determine if Anxiety levels varied according to the location of orthopedic conditions.
Methods
This cross-sectional evaluation analyzed 14,962 consecutive adult new-patient visits to a tertiary orthopedic practice between 4/1/2016 and 12/31/2016. All patients completed PROMIS Anxiety, Depression, Physical Function, and Pain Interference computer adaptive tests (CATs) as routine clinical intake. Patients were grouped by the orthopedic service providing care and categorized as either affected with Anxiety if scoring >62 based on linkage to the Generalized Anxiety Disorder-7 survey. Spearman correlations between the PROMIS scores were calculated. Bivariate statistics assessed differences in Anxiety and Depression scores between patients of different orthopedic services.
Results
Twenty percent of patients scored above the threshold to be considered affected by Anxiety. PROMIS Anxiety scores demonstrated a stronger correlation than Depression scores with Physical Function and Pain Interference scores. Patients with spine conditions reported the highest median Anxiety scores and were more likely to exceed the Anxiety threshold than patients presenting to sports or upper extremity surgeons.
Conclusions
One in 5 new orthopedic patients reports Anxiety levels that may warrant intervention. This rate is heightened in patients needing spine care. Patient-reported Physical Function more strongly correlates with PROMIS Anxiety than Depression suggesting that the Anxiety CAT is a valuable addition to assess mental health among orthopedic patients.
Keywords: anxiety, mental health, orthopedic, patient-reported, depression
Introduction
Mental and physical health have a complex inter-relationship. The recognition of that relationship in orthopedic surgery has coincided with the increasing emphasis being placed on patient-reported musculoskeletal outcomes. At this time, it is clear that mental health strongly influences patient-reported physical function. When studied in orthopedic surgery, patients are often dichotomized into unaffected and affected groups regarding their mental health with those affected comprising all patients with heightened depression, anxiety, and/or pain-catastrophization[1; 2]. In orthopedic studies that examined more granular elements of mental health, depression is the most common isolated focus. When reporting on anxiety, the combined Hospital Anxiety and Depression Scale (HADS) is frequently used which still blends anxiety and depression to some degree [2; 3]. Therefore, it is currently unclear how these elements individually and differentially impact patient-reported physical function.
In part to enable effective assessment of patients’ mental and physical health, the NIH developed the Patient-Reported Outcomes Measurement Information System (PROMIS). PROMIS is unique compared to traditional patient-reported outcome tools in that their computer adaptive tests (CAT’s) enables automated scoring and efficient delivery and it incorporates distinct assessments for Anxiety, Depression, and Pain Interference. Furthermore, the lack of disease specificity has positioned PROMIS to assume a position as a consensus patient-reported outcome across specialties. To that end, PROMIS Physical Function is now the first patient-reported outcome required to be gathered from patients by orthopedic surgeons applying for board certification[4].
PROMIS assessments are all validated in large volunteer populations. In validation testing for the short form and entire item bank, PROMIS Anxiety has a high internal consistency and correlates well with other legacy anxiety measures, but may have a strong floor effect, with 17% of patients reporting the minimum score representing no anxiety symptoms[5; 6]. However, with increasing utilization of PROMIS in clinical practice, it is important to determine how the PROMIS CAT’s perform when administered to patients at the point of care. For instance, as opposed to during validation testing, hasty completion of the PROMIS Depression CAT is associated with an increased floor effect when delivered to orthopedic patients (Guattery et al. Publication pending, Clinical Orthopedics and Related Research). Therefore, the primary aim of this study was to assess the relationship of PROMIS Anxiety with PROMIS Physical Function and Pain Interference in patients presenting for an initial evaluation to an orthopedic surgeon. Secondary aims included 1) assessing the score distribution of PROMIS Anxiety, 2) calculating the prevalence of heightened anxiety potentially warranting treatment, and 3) evaluating score variations between populations of patients presenting for different types of orthopedic conditions. PROMIS Depression, which has been commonly used in orthopaedic research, was used as a comparison metric to assess the relative utility of the Anxiety CAT when assessing mental health[7; 8].
Methods
This cross-sectional study drew from 14,962 consecutive new outpatient clinic visits of adult patients, ages 18 or older, presenting to a single tertiary university orthopedic practice in the United States between 4/1/2016 and 12/31/2016. All patients were given a tablet computer (iPad mini, Apple, Cupertino, CA) preloaded with electronic PROMIS Anxiety v1.0, Depression v1.0, Physical Function v1.2, and Pain Interference v1.1 CAT’s at check-in. Automated scores were directly exported into the electronic medical record. All PROMIS scores are normalized to a standard population distribution with a mean of 50 and a standard deviation of 10. PROMIS assessments are scored so that a higher score represents more of each item being measured. For example, a higher Anxiety score represents more anxiety symptoms while a higher Physical Function score represents more, or better, function. Our software platform does not allow patients to skip questions, and only fully completed PROMIS CAT’s generate scores. New patient visits were selected to ensure that each patient only contributed one score per module. New visits were identified by the following CPT (Current Procedural Terminology) evaluation/management codes: “99201”, “99202”, “99203”, “99204”, or “99205”. When patients had multiple new visits to different providers during the study period, only the first visit to our practice was analyzed. Given the relevance to our primary study aim, patient encounters that were missing PROMIS Anxiety scores were excluded from analysis without any imputation.
PROMIS Anxiety
The PROMIS Anxiety module captures the respondent’s emotional distress caused by hyperarousal, fear, stress, and related somatic symptoms[9]. The questions are pulled from an item bank of 29 questions that refer to symptom occurring over the past week: for example, “In the past 7 days I had trouble relaxing” or “In the past 7 days I felt nervous”. These questions have been designed to capture the trait of anxiety rather than a temporary state[6; 10].
PROMIS Depression
PROMIS Depression measures negative affect, mood, self-image, and social interaction by pulling questions from a bank of 28 items[9]. Examples include “In the past 7 days I felt sad” and “In the past 7 days I withdrew from other people”.
Univariate descriptive analyses and histograms were used to statistically and graphically explore the PROMIS score distributions. Data normality was assessed by the Kolmogorov-Smirnov test as well as graphically with histograms. Maximum and minimum scores were noted and the percentage of patients affected by these ceiling and floor scores were recorded. For the purposes of this study, patients were categorized as affected or unaffected by heightened anxiety based on a PROMIS Anxiety score threshold of 62. Scores of 62 or higher have been validated to correspond with scores above 10 on the Generalized Anxiety Disorder 7 via established linkage tables[6; 11]. A score of ten or higher on the GAD-7 represents the optimal sensitivity and specificity for detection of moderate anxiety considered sufficient to prompt formal anxiety evaluation for potential treatment[12].
Spearman’s correlation was used to evaluate the relationship between PROMIS Anxiety scores and the other PROMIS scores. Correlation coefficients (r) were interpreted as follows: 0.00-0.29 no correlation, 0.30-0.49 weak correlation, 0.50-0.69 moderate correlation, 0.70-0.89 strong correlation, and 0.90-1.00 very strong correlation[13]. A Fisher r-to-z transformation was used to determine if significant differences existed between the correlations of Anxiety scores and Depression scores with the other health domains assessed.
Kruskal-Wallis H test with post-hoc testing compared the median PROMIS Anxiety scores across race, sex, and orthopedic division providing care. Any significant differences found by Kruskal-Wallis were examined for pairwise differences of five points or greater (effect size 0.5). This magnitude of difference has been suggested as a clinically relevant change on PROMIS measures which we considered a reasonable proxy for relevant between group differences[14-16]. Spearman’s correlations assessed the relationship between age and PROMIS scores. Pearson’s Chi-Square was utilized to assess the difference in proportions of patients scoring above the Anxiety score threshold between groups presenting to different orthopedic divisions.
Results
Among 14962 new patient visits, 14679 (98%) had valid PROMIS Anxiety scores and were included in analysis (Table 1). Therefore, 283 patients were treated during the study period and either refused or failed to complete the PROMIS assessment. PROMIS Anxiety (Figure 1) and Depression scores presented in a non-normal distribution, with the secondary peaks occurring at the floor value (Anxiety floor, 5.5% at score=32.9; Depression floor, 22.4% at score=34.2). Physical Function and Pain Interference scores were normally distributed. Median Anxiety and Depression scores approximated the normative population mean, while average Physical Function and Pain Interference scores indicated that each of these health domains were greater than one standard deviation worse than the normative population mean. Nineteen and a half percent of all patients scored greater than 62 on PROMIS Anxiety surpassing the threshold to be considered to have Anxiety possibly warranting treatment.
Table 1.
Demographic and PROMIS scores for entire study population.
| Mean age in years (SD) | 51.1 (16.8) | |
|---|---|---|
| Sex | Female | 8203 (55.9%) |
| Male | 6476 (44.1%) | |
|
| ||
| Race | White/Caucasian | 12436 (84.7%) |
| Black/African-American | 1706 (11.6%) | |
| Other | 537 (3.7%) | |
|
| ||
| Orthopaedic Division | Upper Extremity | 3835 (26.1%) |
| Sports | 3115 (21.2%) | |
| Joint Reconstruction | 2006 (13.7%) | |
| Foot and Ankle | 1521 (10.4%) | |
| Spine | 1050 (7.2%) | |
| Trauma | 637 (4.3%) | |
| Other | 2515 (17.1%) | |
|
| ||
| Median PROMIS Scores (IQR) | Anxiety | 53.7 (46.3-60.4) |
| Depression | 46.3 (38.9-54.1) | |
|
| ||
| Mean PROMIS Scores (SD) | Physical Function | 53.4 (10.3) |
| Pain Interference | 47.0 (9.9) | |
Figure 1.
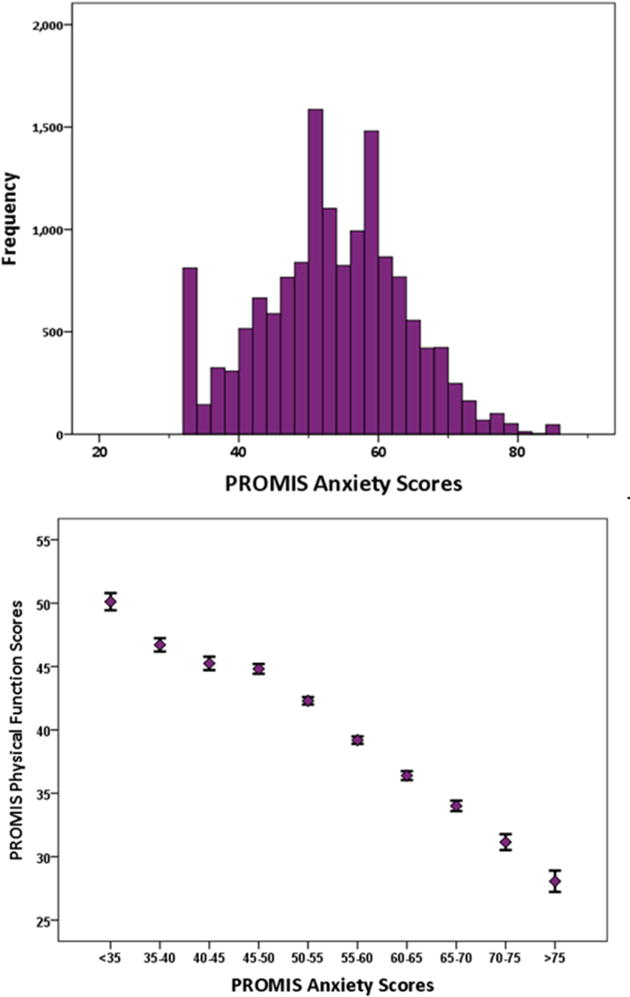
Histogram of PROMIS Anxiety scores for the entire study population.
PROMIS Anxiety scores were moderately correlated with Physical Function and Pain Interference scores (Table 2, Figure 2a,b). PROMIS Anxiety scores were strongly correlated with PROMIS Depression scores. The correlations of PROMIS Anxiety with Physical Function and Pain Interference were significantly greater than the correlations of those PROMIS domains with Depression scores (p<0.001).
Table 2.
Correlations between PROMIS scores (r values).
| Anxiety | Depression | Physical Function | Pain Interference | |
|---|---|---|---|---|
| Anxiety | 1 | |||
| Depression | 0.72 (0.71 - 0.72) | 1 | ||
| Physical Function | −0.51 (−0.52 - −0.50) | −0.38(−0.37 - −0.40) | 1 | |
| Pain Interference | 0.54 (0.52 - 0.55) | −0.37(−0.35 - −0.38) | −0.71(−0.70 - −0.72) | 1 |
Figure 2.
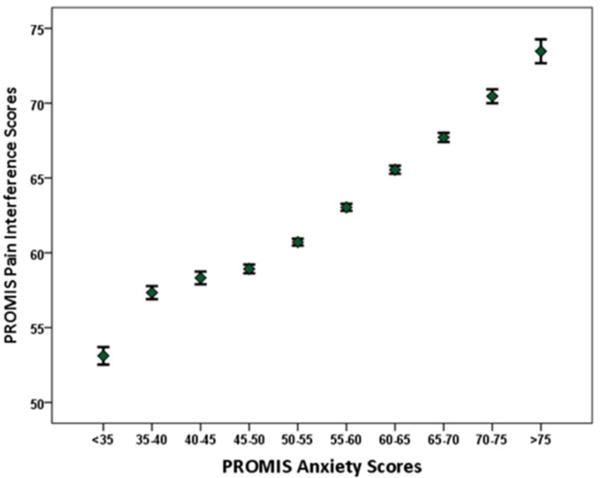
Relationship between PROMIS Anxiety scores with a) PROMIS Physical Function and b) PROMIS Pain Interference. (Error bars= 95% Confidence Interval).
Analyzing factors that potentially may influence PROMIS scores, there was no clinically relevant association between sex (2 point score difference), race (1-4 point score differences), or age (r= 0.09) with PROMIS Anxiety scores. Patients presenting with spine conditions reported higher median Anxiety scores, exceeding the proposed relevant difference of 5 points when compared to patients evaluated by the sports or upper extremity services. (Table 3) Patients with spine conditions were most likely to exceed the Anxiety threshold score, while patients presenting to the foot and ankle, sports, or upper extremity divisions were least likely to exceed the Anxiety threshold score. (Figure 3) A similar pattern was observed the spine division patients reporting floor Anxiety values least frequently (p<0.001).
Table 3.
PROMIS Anxiety scores stratified by orthopaedic specialty.
| Spine n=1050 |
Joint Reconstruction n=2006 |
Trauma n=637 |
Foot and Ankle n=1521 |
Sports n=3115 |
Upper Extremity n=3835 |
|
|---|---|---|---|---|---|---|
| Median Anxiety (IQR) |
58.0a (51.2-64.3) |
56.2b (49.3-61.8) |
54.2b (46.9-61.7) |
53.5 c (45.7-59.5) |
52.3c (46.0-58.3) |
51.2d (44.3-58.3) |
| Patients Above Treatment Threshold (score ≥62) (95% CI) |
32.4%a (29.6-35.3%) |
24.0%b (22.1-25.9%) |
23.5%b (20.3-27.0%) |
17.5%c (15.6-19.5%) |
15.5%c (14.3-16.8%) |
16.2%c (15.0-17.4%) |
| Floor Effect (95% CI) |
2.1%a (1.3-3.2%) |
3.5%b (2.8-4.4%) |
5.7%c (4.0-7.7%) |
6.2%c (5.1-7.6%) |
6.2%c (53-7.1%) |
7.0%c (6.2-78%) |
a,b,c,d indicate significantly distinct groups on statistical testing across each row
Figure 3.
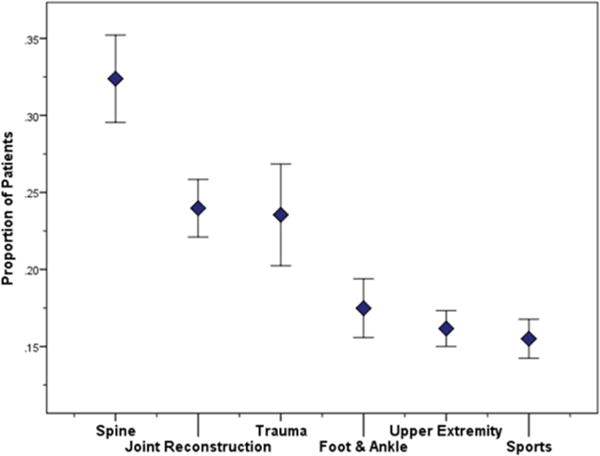
Proportion of patients scoring above the PROMIS Anxiety threshold according to orthopedic surgical specialty.
Discussion
PROMIS Anxiety and Depression scores each present in a non-normal distribution with floor effects in patients presenting to an orthopedic surgeons for initial evaluation for musculoskeletal conditions, while PROMIS Physical Function and Pain Interference scores are normally distributed. Of note, the floor effect, or minimal possible score, represents the score given if “never” is reported for the frequency of symptoms for every question. Despite the theoretical range on PROMIS CAT’s of 0-100, these actual floor values are different for each module: 32.9 for Anxiety, 34.2 for Depression, 38.7 for Pain Interference, and 15.4 for Physical Function. Substantial floor effects frequently compromise mental health questionnaires[17; 18]. In multiple sclerosis and osteoarthritis populations, floor values were returned by up to 17% of PROMIS short form Anxiety assessments[5] and by 24% of Depression PROMIS CAT scores[5; 18]. Within our orthopedic population, the incidence of patients scoring the floor value on the Depression CAT, 22.4%, was consistent with rates previously reported, while the 5.5% of patients scoring the floor value on the Anxiety CAT was much lower. Thus, among our population seeking orthopedic care, we found a smaller percentage of patients reaching a floor score on PROMIS Anxiety CAT than in Driban et al.’s osteoarthritis population taking the Anxiety short form[5]. This discrepancy persists even when considering only the subset of our patients evaluated for hip or knee total joint arthroplasty (3.5% floor values). This may indicate that the PROMIS Anxiety CAT is more effective than the fixed short form in avoiding floor scores.
It is unclear why fewer patients reported floor Anxiety scores than reported floor Depression scores. However, it is clear that orthopedic patients more frequently report measureable anxiety symptoms than depressive symptoms using PROMIS. This may impact surgeons in two ways. First, recognizing the relatively high prevalence of anxiety in patients seeing orthopedic surgeons is needed as anxiety is a modifiable disorder that, if treated, can directly impact surgical outcomes in a positive manner. To that end, heightened anxiety is associated with worse patient-reported function, greater pain, and less treatment satisfaction with musculoskeletal conditions [3; 19-27]. Second, although Anxiety and Depression may each be important to understand, if surgeons were only able to collect a single PROMIS assessment of mental health, the reduced floor effect may support the prioritization of PROMIS Anxiety over Depression.
Nearly one in five patients produced PROMIS Anxiety scores exceeding the proposed threshold set to indicate a level of anxiety that may warrant specific investigation and treatment. This rate is similar to those previously reported for the prevalence of moderate anxiety using other screening measures (18-23%)[3; 28; 29]. The similarity in prevalence using this PROMIS threshold versus alternative anxiety screening questionnaires suggests that our chosen threshold of 62 for PROMIS Anxiety is reasonable and further supports published linkage tables between PROMIS Anxiety and the GAD-7. Going forward, these data suggest that the PROMIS Anxiety CAT may reasonably replace existing static Anxiety screening measures. Notably, anxiety screening tests are typically used to detect patients that may warrant intervention, with dichotomized (affected, unaffected) or categorized (severe, moderate, mild) scores. This helps guide treatment but does not necessarily translate to each patient. The level of individual anxiety that can interfere with progress following an orthopedic surgery is variable. Some patients may not exceed anxiety thresholds and still benefit from intervention to reduce their anxiety, while others potentially indicated for mental health treatment may truly be affected only by a transient stressor.
Our data demonstrate a stronger correlation between PROMIS Anxiety and Physical Function and Anxiety and Pain Interference scores than between Depression and Physical Function or Pain Interference scores in patients presenting with musculoskeletal conditions to orthopedic surgeons. This finding is not one consistently demonstrated in similar studies. Among patients with neurofibromatosis, there were similarly weak correlations between both PROMIS Anxiety and Depression with Physical Function[30]. Hermanussen et al. found a weak correlation between PROMIS Depression and PROMIS Physical Function-Upper Extremity scores in a population with upper extremity conditions but Anxiety scores were not included[31]. We interpret our data as prioritizing intervention for heightened anxiety over heightened depression among orthopedic patients. Although orthopedic surgeons are unlikely to directly provide anxiety counseling, surgeons can likely reduce anxiety by carefully selecting their language used during encounters to demonstrate empathy and can assist patients needing to access mental health resources[32; 33].
Patients presenting to upper extremity and sports orthopedic surgeons on average reported less anxiety than patients presenting to other orthopedic surgical subspecialties. These patients also reported better function, less pain interference, and less depression. This suggests that these patients tend to have less debilitating injuries and thus report less anxiety. While these groups may be demographically different from groups presenting to other orthopaedic services, there were no significant differences in any PROMIS scores attributable to patient sex or races, and scores were not correlated with age. Thus, these group demographic differences are unlikely to be the source of score differences. Other variables that might explain differences between these surgical populations not evaluated with this study include: differences between acute and chronic disorders, if the potential surgical procedure they might receive is elective, ability to maintain function in the home and work place, number and impact of co-existing medical disorders, and how much the disorder impacts sleep. Likely, there is some interplay between these factors. Meanwhile, patients seeking care from our spine surgeons had, on average, the highest Anxiety scores. Spine patients often experience pain that is both musculoskeletal and neurogenic that can impact mobility, work, home responsibilities, and sleep, all which may contribute to anxiety and their overall ability to cope[34-36]. In the setting of limited resources, the differences in these patient populations would suggest focusing anxiety screening efforts among patients with spinal conditions.
Our study has several limitations. Specific diagnoses were not assessed in this dataset which prevents us from analysis more specific than the orthopedic division providing treatment. However, the large number of patients presenting to a broad range of orthopedic specialties suggests that these results can likely generalize to other populations seeking orthopedic surgical care. As this was a cross sectional evaluation, this study established the baseline performance of PROMIS Anxiety in the orthopedic setting but cannot yet determine the relative impact of PROMIS Anxiety versus Depression scores on the ultimate treatment outcomes.
Conclusion
Assessing mental, social, and physical health are priorities as addressing each of these interrelated health domains may offer the most appropriate strategies to improve the overall health status of our country[37]. Given the substantial governmental investment, its computer adaptive testing, and assessments that capture each of these health domains, PROMIS is positioned to become a consensus patient-reported outcome. The relationship of PROMIS mental health scores and physical function scores in our study appear consistent both in direction and magnitude when compared to previous studies using legacy health measures thus adding data toward the validity of PROMIS Anxiety when administered as part of routine orthopedic practice[5; 19; 20; 23; 24; 29; 30]. Our data have uniquely assessed the clinical use of the PROMIS CAT’s and distinguished that Anxiety scores demonstrate stronger correlations with patient-reported Physical Function and Pain Interference than Depression scores do. The relationships between Anxiety and patient-reported Pain Interference and Physical Function provides an opportunity for surgeons to recommend evaluation for Anxiety that, if modified, might directly impact the patient’s perceived musculoskeletal function[19; 21-26; 38]. During routine care, the PROMIS Anxiety has reduced floor effects when compared to PROMIS Depression. As PROMIS is increasingly used throughout orthopedic surgery and other fields of medicine, the Anxiety CAT should be considered as a potentially valuable mental health measure for patients with musculoskeletal conditions. Our department continues to collect both PROMIS Anxiety and Depression as we continue to investigate their utility in practice. Future studies exploring the changes in anxiety and depression over time correlated with the patient’s treatment course will provide healthcare practitioners greater insight in how to effectively offer treatment that impacts the patient’s biopsychosocial and physical health.
Acknowledgments
Funding: This study was funded by: Research reported in this publication was supported by the Washington University Institute of Clinical and Translational Sciences grant UL1TR000448, sub-award TL1TR000449, from the National Center for Advancing Translational Sciences (NCATS) of the National Institutes of Health (NIH), and Siteman Comprehensive Cancer Center and NCI Cancer Center Support Grant P30 CA091842, which supported the maintenance and use of REDCap electronic data capture tools, hosted in the Biostatistics Division of Washington University School of Medicine. The content is solely the responsibility of the authors and does not necessarily represent the official view of the NIH. This funding did not play a direct role in this investigation.
Footnotes
Institution for work: Washington University School of Medicine
Level of Evidence: Diagnostic Level III
Compliance with Ethical Standards:
Conflict of Interest: All Authors (Beleckas, Guattery, Prather, Kelly, Calfee, Wright) of this manuscript report no conflicts of interest for this research and this manuscript.
Human Research: Ethical approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Human Research: Informed consent: This study was allowed as “exempt” by our Institutional Review Board as no protected health information was accessed and therefore this review of de-identified data did not require written consent from participants included in the study.
References
- 1.London DA, Stepan JG, Boyer MI, Calfee RP. The impact of depression and pain catastrophization on initial presentation and treatment outcomes for atraumatic hand conditions. J Bone Joint Surg Am. 2014;96(10):806–814. doi: 10.2106/JBJS.M.00755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dekker AP, Salar O, Karuppiah SV, Bayley E, Kurian J. Anxiety and depression predict poor outcomes in arthroscopic subacromial decompression. J Shoulder Elbow Surg. 2016;25(6):873–880. doi: 10.1016/j.jse.2016.01.031. [DOI] [PubMed] [Google Scholar]
- 3.Duivenvoorden T, Vissers MM, Verhaar JA, Busschbach JJ, Gosens T, Bloem RM, Bierma-Zeinstra SM, Reijman M. Anxiety and depressive symptoms before and after total hip and knee arthroplasty: a prospective multicentre study. Osteoarthritis Cartilage. 2013;21(12):1834–1840. doi: 10.1016/j.joca.2013.08.022. [DOI] [PubMed] [Google Scholar]
- 4.The American Board of Orthopaedic Surgery Certification Examinations. from https://www.abos.org/certification-exams/part-ii/patient-reported-outcomes.aspx.
- 5.Driban JB, Morgan N, Price LL, Cook KF, Wang C. Patient-Reported Outcomes Measurement Information System (PROMIS) instruments among individuals with symptomatic knee osteoarthritis: a cross-sectional study of floor/ceiling effects and construct validity. BMC Musculoskelet Disord. 2015;16:253. doi: 10.1186/s12891-015-0715-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schalet BD, Cook KF, Choi SW, Cella D. Establishing a common metric for self-reported anxiety: linking the MASQ, PANAS, and GAD-7 to PROMIS Anxiety. J Anxiety Disord. 2014;28(1):88–96. doi: 10.1016/j.janxdis.2013.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Talaei-Khoei M, Fischerauer SF, Jha R, Ring D, Chen N, Vranceanu AM. Bidirectional mediation of depression and pain intensity on their associations with upper extremity physical function. J Behav Med. 2017 doi: 10.1007/s10865-017-9891-6. [DOI] [PubMed] [Google Scholar]
- 8.Peters RM, Menendez ME, Mellema JJ, Ring D, Vranceanu AM. Sleep Disturbance and Upper-Extremity Disability. Arch Bone Jt Surg. 2016;4(1):35–40. [PMC free article] [PubMed] [Google Scholar]
- 9.Pilkonis PA, Choi SW, Reise SP, Stover AM, Riley WT, Cella D, Group, P.C. Item banks for measuring emotional distress from the Patient-Reported Outcomes Measurement Information System (PROMIS®): depression, anxiety, and anger. Assessment. 2011;18(3):263–283. doi: 10.1177/1073191111411667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.AssessmentCenter. PROMIS - Anxiety Scoring Manual. 2015 Vol. https://www.assessmentcenter.net/documents/PROMIS%20Anxiety%20Scoring%20Manual.pdf.
- 11.Stone P. http://www.prosettastone.org/LinkingTables/Documents/PROMIS%20Anxiety%20and%20GAD-7%20Linking%20Table.pdf). Appendix Table 34: Raw Score to T-Score Conversion Table for GAD-7 to PROMIS Anxiety.
- 12.Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- 13.Calkins K. Applied Statistics-Lesson 5: Correlation Coefficients. 2016 from http://www.andrews.edu/~calkins/math/edrm611/edrm05.htm.
- 14.Broderick JE, Schneider S, Junghaenel DU, Schwartz JE, Stone AA. Validity and reliability of patient-reported outcomes measurement information system instruments in osteoarthritis. Arthritis Care Res (Hoboken) 2013;65(10):1625–1633. doi: 10.1002/acr.22025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yost KJ, Eton DT, Garcia SF, Cella D. Minimally important differences were estimated for six Patient-Reported Outcomes Measurement Information System-Cancer scales in advanced-stage cancer patients. J Clin Epidemiol. 2011;64(5):507–516. doi: 10.1016/j.jclinepi.2010.11.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ho B, Houck JR, Flemister AS, Ketz J, Oh I, DiGiovanni BF, Baumhauer JF. Preoperative PROMIS Scores Predict Postoperative Success in Foot and Ankle Patients. Foot Ankle Int. 2016;37(9):911–918. doi: 10.1177/1071100716665113. [DOI] [PubMed] [Google Scholar]
- 17.Gibbons CJ, Mills RJ, Thornton EW, Ealing J, Mitchell JD, Shaw PJ, Talbot K, Tennant A, Young CA. Rasch analysis of the hospital anxiety and depression scale (HADS) for use in motor neurone disease. Health Qual Life Outcomes. 2011;9:82. doi: 10.1186/1477-7525-9-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Amtmann D, Kim J, Chung H, Bamer AM, Askew RL, Wu S, Cook KF, Johnson KL. Comparing CESD-10, PHQ-9, and PROMIS depression instruments in individuals with multiple sclerosis. Rehabil Psychol. 2014;59(2):220–229. doi: 10.1037/a0035919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wolfensberger A, Vuistiner P, Konzelmann M, Plomb-Holmes C, Leger B, Luthi F. Clinician and Patient-reported Outcomes Are Associated With Psychological Factors in Patients With Chronic Shoulder Pain. Clin Orthop Relat Res. 2016;474(9):2030–2039. doi: 10.1007/s11999-016-4894-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Skeppholm M, Fransson R, Hammar M, Olerud C. The association between preoperative mental distress and patient reported outcome measures in patients treated surgically for cervical radiculopathy. Spine J. 2016 doi: 10.1016/j.spinee.2016.02.037. [DOI] [PubMed] [Google Scholar]
- 21.Koorevaar RC, van ‘t Riet E, Gerritsen MJ, Madden K, Bulstra SK. The Influence of Preoperative and Postoperative Psychological Symptoms on Clinical Outcome after Shoulder Surgery: A Prospective Longitudinal Cohort Study. PLoS One. 2016;11(11):e0166555. doi: 10.1371/journal.pone.0166555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bagheri F, Ebrahimzadeh MH, Moradi A, Bidgoli HF. Factors Associated with Pain, Disability and Quality of Life in Patients Suffering from Frozen Shoulder. Arch Bone Jt Surg. 2016;4(3):243–247. [PMC free article] [PubMed] [Google Scholar]
- 23.Engel-Yeger B, Keren A, Berkovich Y, Sarfaty E, Merom L. The role of physical status versus mental status in predicting the quality of life of patients with lumbar disk herniation. Disabil Rehabil. 2016:1–7. doi: 10.1080/09638288.2016.1253114. [DOI] [PubMed] [Google Scholar]
- 24.Tonelli SM, Rakel BA, Cooper NA, Angstom WL, Sluka KA. Women with knee osteoarthritis have more pain and poorer function than men, but similar physical activity prior to total knee replacement. Biol Sex Differ. 2011;2:12. doi: 10.1186/2042-6410-2-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Noiseux NO, Callaghan JJ, Clark CR, Zimmerman MB, Sluka KA, Rakel BA. Preoperative predictors of pain following total knee arthroplasty. J Arthroplasty. 2014;29(7):1383–1387. doi: 10.1016/j.arth.2014.01.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pinto PR, McIntyre T, Ferrero R, Almeida A, Araujo-Soares V. Predictors of acute postsurgical pain and anxiety following primary total hip and knee arthroplasty. J Pain. 2013;14(5):502–515. doi: 10.1016/j.jpain.2012.12.020. [DOI] [PubMed] [Google Scholar]
- 27.Ali A, Lindstrand A, Sundberg M, Flivik G. Preoperative Anxiety and Depression Correlate With Dissatisfaction After Total Knee Arthroplasty: A Prospective Longitudinal Cohort Study of 186 Patients, With 4-Year Follow-Up. J Arthroplasty. 2017;32(3):767–770. doi: 10.1016/j.arth.2016.08.033. [DOI] [PubMed] [Google Scholar]
- 28.Demir B, Gürsu S, Yildirim T, Er T. Evaluation of anxiety levels in patients with chronic orthopedic diseases. Acta Orthop Traumatol Turc. 2012;46(6):420–424. doi: 10.3944/aott.2012.2756. [DOI] [PubMed] [Google Scholar]
- 29.Attal N, Masselin-Dubois A, Martinez V, Jayr C, Albi A, Fermanian J, Bouhassira D, Baudic S. Does cognitive functioning predict chronic pain? Results from a prospective surgical cohort. Brain. 2014;137(Pt 3):904–917. doi: 10.1093/brain/awt354. [DOI] [PubMed] [Google Scholar]
- 30.Talaei-Khoei M, Riklin E, Merker VL, Sheridan MR, Jordan JT, Plotkin SR, Vranceanu AM. First use of patient reported outcomes measurement information system (PROMIS) measures in adults with neurofibromatosis. J Neurooncol. 2016 doi: 10.1007/s11060-016-2314-7. [DOI] [PubMed] [Google Scholar]
- 31.Hermanussen HH, Menendez ME, Chen NC, Ring D, Vranceanu AM. Predictors of Upper-Extremity Physical Function in Older Adults. Arch Bone Jt Surg. 2016;4(4):359–365. [PMC free article] [PubMed] [Google Scholar]
- 32.Bot AG, Vranceanu AM, Herndon JH, Ring DC. Correspondence of patient word choice with psychologic factors in patients with upper extremity illness. Clin Orthop Relat Res. 2012;470(11):3180–3186. doi: 10.1007/s11999-012-2436-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Menendez ME, Chen NC, Mudgal CS, Jupiter JB, Ring D. Physician Empathy as a Driver of Hand Surgery Patient Satisfaction. J Hand Surg Am. 2015;40(9):1860–1865 e1862. doi: 10.1016/j.jhsa.2015.06.105. [DOI] [PubMed] [Google Scholar]
- 34.Kawai K, Kawai AT, Wollan P, Yawn BP. Adverse impacts of chronic pain on health-related quality of life, work productivity, depression and anxiety in a community-based study. Fam Pract. 2017;34(6):656–661. doi: 10.1093/fampra/cmx034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Coyle PC, Velasco T, Sions JM, Hicks GE. Lumbar Mobility and Performance-Based Function: An Investigation in Older Adults with and without Chronic Low Back Pain. Pain Med. 2017;18(1):161–168. doi: 10.1093/pm/pnw136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Staner L. Sleep and anxiety disorders. Dialogues Clin Neurosci. 2003;5(3):249–258. doi: 10.31887/DCNS.2003.5.3/lstaner. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Medicine C. o. t. R. S. a. B. D. a. M. f. E. H. R. B. o. P. H. a. P. H. P. I. o. Capturing Social and Behavioral Domains in Electronic Health Records: Phase 1. Washington (DC): Nathional Academics Press (US); 2014. Jun 23, [PubMed] [Google Scholar]
- 38.Skeppholm M, Fransson R, Hammar M, Olerud C. The association between preoperative mental distress and patient-reported outcome measures in patients treated surgically for cervical radiculopathy. Spine J. 2017;17(6):790–798. doi: 10.1016/j.spinee.2016.02.037. [DOI] [PubMed] [Google Scholar]


