Abstract
Introduction
Informant-reported subjective cognitive decline (iSCD) has been associated with a higher risk of conversion to dementia, but the findings of whole brain functional connectivity strength (FCS) changes in iSCD are limited.
Methods
The sample comprised 39 participants with iSCD and 39 age- and sex- matched healthy controls. The global absolute (aFCS) and relative functional connectivity strengths were estimated using weighted degree centrality and the z-scores of the weighted degree centrality respectively. FreeSurfer was used for measuring cortical thickness.
Results
The aFCS was lower in iSCD primarily in left medial superior frontal, left precuneus, left parietal, right cuneus, and bilateral calcarine; while relative functional connectivity strength was higher in posterior cingulate cortex/precuneus compared with healthy controls. No significant differences in cortical thickness were observed.
Discussion
There are detectable changes of FCS in iSCD, with the precuneus possibly playing a compensatory role. FCS could therefore have a potential role to serve as one of the earliest neuroimaging markers of neurodegenerative disease.
Keywords: Subjective cognitive decline, Functional connectivity strength, Preclinical Alzheimer's disease, Aging, Precuneus
Highlights
-
•
Functional connectivity strength was examined in informant-reported subjective cognitive decline.
-
•
Absolute functional connectivity strength was lower in the default mode network in informant-reported subjective cognitive decline.
-
•
Individuals with informant-reported subjective cognitive decline showed higher relative functional connectivity strength in precuneus.
1. Background
Subjective (self- or informant-reported) cognitive decline (SCD), which may be present before any objective evidence of cognitive impairment, has been associated with an increased risk of future cognitive decline and conversion to mild cognitive impairment or dementia [1]. Although research into SCD has been associated with several unresolved challenges, primarily the variability in defining SCD across studies, the heterogeneity of factors related to SCD, and the limited knowledge of the neurobiological mechanisms underlying SCD [2], it has attracted significant attention because of the potential for SCD as an early marker of neurodegenerative conditions [3]. SCD may be based on self-report or that by an informant-reported subjective cognitive decline (iSCD) [4], [5], and it has been shown that informant-report is indicative, reliable, and more associated with objective markers of disease than self-report [6].
With the premise that SCD is indicative of early stage neuropathology, it should arguably be possible to detect changes at this stage using modern neuroimaging techniques. The resting-state functional MRI (r-fMRI) has emerged as a powerful tool to explore intrinsic functional networks. Although many studies have investigated SCD [7], only a few applied the r-fMRI to explore it based on informant-report [8]. In the previous studies, Wang found reduced default mode network (DMN) connectivity in 23 informant-verified cognitive complaints using independent component analysis [9]. Another r-fMRI group found that cognitive complaint index scores from self and informant were associated with altered resting-state networks [10]. In a self-reported SCD study, individuals in the SCD group had higher amplitude of low-frequency fluctuations than did those in the control group, with no significant group differences in gray matter (GM) volume [11]. However, these studies examined abnormalities at the network level or did not perform whole-brain voxel-wise comparison of functional connectivity strength (FCS) in iSCD. The voxel-wise methodology enables whole brain hub mapping but avoids parcellation-dependent effects on the topological organization of brain networks [12]. FCS that sums the weights of all the connections of a given voxel, measures the functional importance of a given voxel in support of information transfer in the whole brain [13]. Mean FCS has been applied to study functional hubs of Alzheimer's disease (AD) [12], [13], emphasizing AD-related degeneration of specific brain hubs. These studies found that brain hubs (i.e., the regions with higher FCS) were mainly distributed in several DMN regions in both AD and healthy control groups [12], [13]. However, the finding of FCS changes in patients with iSCD has not been well established in the literature.
In this study, we sought to determine whether brain FCS changes can be detected at the stage of iSCD. We studied participants with iSCD in community-dwelling elderly adults drawn from Sydney Memory and Aging Study (MAS). Given that the iSCD was associated with informant-reported memory-related complaints, we hypothesized that there would be disturbed functional connectivity at an early pre-dementia stage, which was indicated by lower absolute FCS in memory-related brain regions in iSCD compared with controls. We also hypothesized that there would be a possible compensatory role for some regions indicated by higher relative FCS in these regions in iSCD.
2. Methods
2.1. Participants
Participants were drawn from the MAS, a longitudinal study of community-dwelling individuals recruited randomly through the electoral roll from the Eastern region of Sydney [14]. Participants were excluded if they had suffered any medical or psychiatric conditions that may have prevented them from completing assessments, had a Mini–Mental State Examination score < 24 [15] adjusted for age and education or had received a diagnosis of dementia, schizophrenia, bipolar disorder, multiple sclerosis, motor neuron disease, developmental disability, or progressive malignancy. Participants were classified as cognitively normal if performance on all test measures was above the 6.68 percentile (-1.5 SDs) or equivalent score compared to normative published values, they were not demented and they had normal function or minimal impairment in IADLs defined by a total average score <3.0 on the Bayer ADL scale [16]. The iSCD was applied to individuals who have informant-reported memory-related complaints, such as having difficulty with remembering names and recalling where one has placed things, but exhibit a normal range neuropsychological test performance. For the current study, 348 cognitively normal participants were included, of which 107 had definite informant questionaires and r-fMRI data, and 101 had artefact-free fMRI scans. Of these, 39 met criteria for iSCD, and 39 age- and sex- matched healthy controls were randomly selected from the others. Written informed consent was obtained from both participants and informants. Ethics approval was obtained from the Human Research Ethics Committees of the University of New South Wales and the South Eastern Sydney Local Health District.
2.2. Informant-based cognitive complaints
Participants were asked to nominate an informant to answer questions relating to the participant's memory, thinking, and daily functioning. The informant had to have at least 1 hour of contact with the participant per week and preferably be cohabitating with them. Informants completed 19 questions about the participant's cognition by a mail-back questionnaire, including a modified short Informant Questionnaire on Cognitive Decline in the Elderly (IQCODE) [17], which asks informants to rate participants' function when compared with 5 years ago on several memory and nonmemory domains. In addition, the informant completed a questionnaire about care provision, a sleep questionnaire. The informant questions from the General Practitioner assessment of Cognition (GPCOG) [18], which included two memory and one language question, were asked over the phone by the research psychologist [14], [19].
2.3. Image acquisition
All MRI scans were obtained on a Philips 3T Achieva Quasar Dual scanner (Philips Medical Systems, Best, The Netherlands) located at the Neuroscience Research Australia, Sydney. For the resting-state scan, participants were required to ‘keep their eyes closed but not fall asleep and think of nothing in particular’. For each participant, we used a T2*-weighted echo planar imaging (EPI) sequence with the following parameters: repetition time/echo time = 2000/30 ms, flip angle = 90°, field of view (FOV) = 240 × 130.5 × 240 mm3, 29 continuous axial slices with slice thickness = 4.5 mm without interslice gap, matrix size = 128 × 128, yielding voxel size = 1.9 × 1.9 × 4.5 mm3. During about 7-min scan of fMRI, we acquired 208 volumes per participant. Acquisition parameters for T1-weighted structural MRI scans: TR = 6.39 ms, TE = 2.9 ms, flip angle = 8°, matrix size = 256 × 256, FOV = 256 × 256 × 190, and slice thickness = 1 mm with no gap in between, yielding 1 × 1 × 1 mm3 isotropic voxels.
2.4. Image processing
All the resting-state fMRI scans were pre-processed and analyzed using Data Processing Assistant for Resting-State fMRI (http://restfmri.net/forum/DPARSF), which was implemented as a toolbox for Statistical Parametric Mapping (SPM12) (http://www.fil.ion.ucl.ac.uk/spm/software/spm12/). The first 10 volumes were discarded due to signal equilibrium and to allow the participants’ adaptation to the scanning noise. The images were corrected for slice-timing and head movement correction. We further normalized all images to Montreal Neurological Institute (MNI) space by using the EPI template and resliced with a voxel size of 3 × 3 × 3 mm3 to agree with the GM probability maps. The images were then smoothed with a Gaussian kernel of a 4-mm full-width half maximum (FWHM) Gaussian Kernel. To remove the effect of physiological noise, we covaried global signals and signals from cerebrospinal fluid and white matter after removing linear trend. Finally, a band pass filter (0.01-0.1 Hz) was applied to reduce the low frequency drifts and high-frequency noise.
2.5. Computations of aFCS and rFCS
We measured the global absolute functional connectivity strengths (aFCS) based on the number of strongly correlated links to a given brain voxel. The aFCS was computed by sum of weights of all the connections of a given voxel that exceeded a predefined optimized threshold, which is also known as weighted degree centrality [12], [13]. Specifically, Pearson's correlation (r) between the BOLD (blood oxygen level–dependent) time series of each pair of voxels within a GM mask without cerebellum (with the number of voxels of the mask N = 45,381) was calculated and only Pearson's correlation coefficients above a threshold of r > 0.2 were used. Then Fisher's r-to-z transformation was applied to improve the normality of the correlation remaining coefficients. Finally, the whole-brain functional connectivity matrix for each participant was generated. The weighted degree centrality (i.e., aFCS) of each voxel was defined as . rij was the correlation coefficient (after Fisher's r-to-z transformation) between any two voxels within the mask. In this context, aFCS measures the correlation extent of a given voxel with all other voxels in the mask. A larger aFCS value indicates greater strength of functional connectivity of a voxel to other voxels in the brain.
The relative functional connectivity strength (rFCS) was defined as follows. After having constructed the degree map with the threshold of r ≥ 0.2, the values of the degree map were standardized to z-scores to make them comparable across subjects. The z-score standardization is,
where u and δ are the mean and SD of the degree measure aFCS across all N nodes.
The conversion to z-score of each degree map did not influence the topography of individual map but each participant's map could then become standardized for comparison [13]. Greater rFCS in a region suggests that there is more functional connectivity in that region relative to other brain regions. The peak locations in the map were considered as hubs [13].
2.6. Computations of cortical thickness
To measure cortical thickness, T1-weighted images were processed with the longitudinal pipeline available in FreeSurfer (http://surfer.nmr.mgh.harvard.edu/). Briefly, the steps involved removal of nonbrain tissue, intensity normalization, tessellation of the white/GM boundary, and inflation and registration of the cortical surface to the spherical atlas according to the folding patterns of each individual [20]. Cortical thickness is calculated in FreeSurfer as the closest distance from the white/gray boundary to the pia mater at each vertex on the tessellated surface.
2.7. Statistics
To explore the within-group rFCS patterns, voxel-wise one-sample t-tests were performed on the individual functional connectivity maps for iSCD and healthy controls separately (two-tailed GRF correction, voxel level: P < .005; cluster level: P < .05). We set this threshold to find the highly connected regions which can be considered as potential hub regions. The between-group differences of aFCS and rFCS were compared using permutation test for two sample t-test and corrected for multiple comparisons (10,000 times, cluster-defining threshold: P ≤ .01, FWE-corrected: P ≤ .05). Cortical thickness analyses were then performed using the QDEC toolbox of FreeSurfer. The intergroup differences were investigated using vertex-based two sample t-test obtained with general linear models using a false discovery rate of 0.05 (FDR < 0.05).
2.8. Validation analysis
Previous studies have suggested that brain function could potentially be influenced by structural differences (e.g., GM differences) among groups [21], [22]. To explore the possible confounding effect of GM atrophy, in the present study, we performed a voxel-based morphometry analysis for structural images by SPM12. We reanalyzed the intergroup differences of aFCS and rFCS by taking GM volume as covariates (two-tailed Gaussian random field correction voxel level: P < .005; cluster level: P < .05).
3. Results
3.1. Demographic analysis
Descriptive statistics for each group are displayed in Table 1, and other cognitive scores are presented in Table S1 and Table S2 in the Supplementary Material. There were no significant group differences in age, sex, years of education, or Mini–Mental State Examination scores. The average age of all the participants is 83, and each group includes 19 males and 20 females.
Table 1.
Characteristics of iSCD and healthy controls
| Demographic variables | iSCD (n = 39) | Controls (n = 39) | P value |
|---|---|---|---|
| Age (mean(SD), years) | 83.00 (4.43) | 82.89 (4.13) | .913 |
| Sex (male; female) | 19; 20 | 19; 20 | 1.00 |
| Education (mean(SD), years) | 12.72 (3.77) | 11.85 (2. 99) | .261 |
| MMSE (mean(SD)) | 28.87 (1.031) | 28.36 (1.386) | .068 |
Abbreviations: iSCD, informant-reported subjective cognitive decline; MMSE, Mini–Mental State Examination.
NOTE. Values are number or mean (SD).
NOTE. P values refer to analysis of variance models, followed by two-sample t tests for continuous measures (age, education, MMSE) and χ2 test for sex.
3.2. Within-group functional connectivity
Fig. 1 shows the FCS maps of iSCD and healthy controls separately. Prominent rFCS hubs of both samples were located within precuneus, cuneus and parietal (two-tailed Gaussian random field correction, voxel level: P < .005; cluster level: P < .05). In addition, we also observed high rFCS in other brain regions such as the occipital cortex and medial frontal. The resulting functional connectivity maps were projected onto a standard brain surface as shown in Fig. 1.
Fig. 1.
Spatial FCS patterns of iSCD and healthy controls. Prominent hubs were indicated by colors in iSCD (left) and healthy controls (right) (two-tailed Gaussian random field (GRF) correction voxel level: P < .005; cluster level: P < .05). The color bars indicate T-statistic. Abbreviations: iSCD, informant-reported subjective cognitive decline; HC, healthy controls; FCS, functional connectivity strength.
3.3. Group differences in aFCS and rFCS
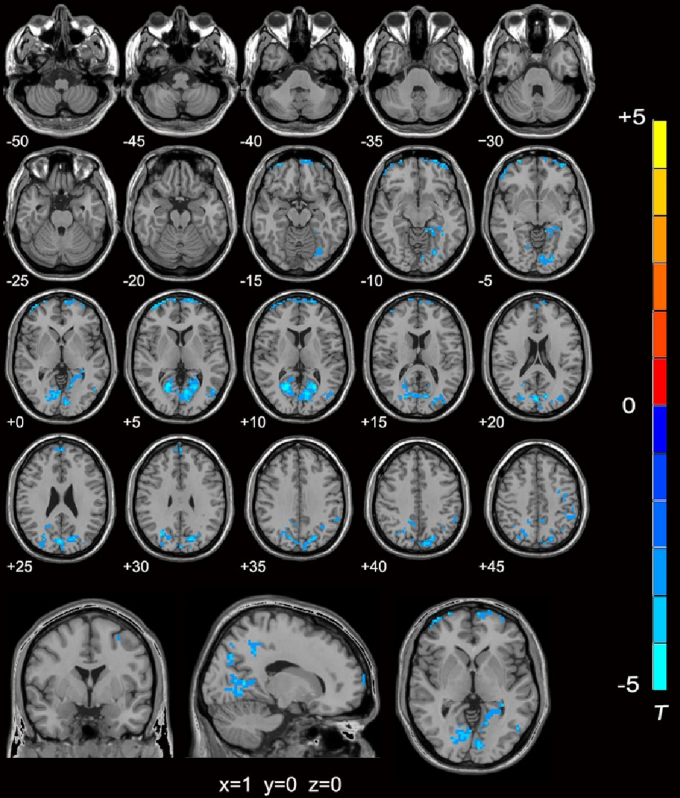
Permutation test revealed that aFCS in iSCD was significantly lower compared with healthy controls in left medial superior frontal (Brodmann areas, BA10/11), left precuneus (BA5/7), left parietal (BA7/40), right cuneus (BA18/19), and bilateral calcarine (BA17/19) as shown in Fig. 2 (10,000 permutations, cluster-defining threshold: P ≤ .01, FWE-corrected: P ≤ .05). Most of these regions are the main components of the DMN, and bilateral calcarine gyri are components of the visual cortex. No nodes with significantly higher aFCS were found in iSCD. See Table 2 for the list of main regions.
Fig. 2.
The aFCS difference maps between iSCD and healthy controls. Participants with iSCD showed significantly decreased aFCS compared with the healthy controls (10,000 random permutations, cluster-defining threshold: P ≤ .01, FWE-corrected: P ≤ .05). No significantly increased aFCS was found in iSCD. The color bars indicate T-statistic, and regions with blue colors indicate lower values in iSCD. Abbreviations: iSCD, informant-reported subjective cognitive decline; aFCS, absolute functional connectivity strength.
Table 2.
Regions showing aFCS/rFCS differences between iSCD and healthy controls
| FCS | Brain regions | BA | Cluster size | Peak MNI coordinates, mm |
T value | ||
|---|---|---|---|---|---|---|---|
| x | y | z | |||||
| Right calcarine | 17/19 | 1130 | 21 | −63 | 6 | 4.68 | |
| Right cuneus | 18/19 | 3 | −81 | 24 | 4.61 | ||
| Left calcarine | 17/19 | −12 | −72 | 9 | 4.53 | ||
| aFCS | Left parietal | 7/40 | 792 | −42 | −57 | 54 | 4.42 |
| Left precuneus | 5/7 | −12 | −54 | 57 | 4.22 | ||
| Medial superior frontal | 10/11 | 319 | 0 | 60 | 27 | 3.94 | |
| rFCS | Left precuneus/posterior cingulate cortex | 7/31 | 188 | 0 | −69 | 39 | 4.96 |
Abbreviations: FCS, functional connectivity strength; BA, Brodmann's area; MNI, Montreal Neurological Institute; T value, T-statistic value; aFCS, absolute functional connectivity strength; rFCS, relative functional connectivity strength; iSCD, informant-reported subjective cognitive decline.
The iSCD had higher rFCS than healthy controls in PCC/precuneus (BA7/31) in the left hemisphere as shown in Fig. 3 (10,000 permutations, cluster-defining threshold: P ≤ .01, FWE-corrected: P ≤ .05). No significantly lower rFCS was observed in iSCD. See Table 2 for the list of main regions.
Fig. 3.
The rFCS difference maps between iSCD and healthy controls. (A) Box plot for the group comparison in mean rFCS. Box plot shows that the mean rFCS values in iSCD are significantly higher than that of in healthy controls. (B) Sagittal view of the rFCS differences between groups. The rFCS values in iSCD were higher than healthy controls in precuneus/posterior cingulate cortex (10,000 random permutations for two-sample t test, cluster-defining threshold: P ≤ .01, FWE-corrected: P ≤ .05). The hot colors indicate the higher T values in iSCD. Abbreviations: iSCD, informant-reported subjective cognitive decline; rFCS, relative functional connectivity strength.
3.4. FCS analysis with GM volume as covariates
The results of inter-group comparisons in aFCS and rFCS by taking GM volume as covariate are shown in Fig. 4. We found that the results were almost the same with or without GM volume as covariate.
Fig. 4.
The intergroup FCS differences without/with GM volume as covariates. (A) The aFCS analysis. The left and the right are the aFCS differences without or with GM volume as covariates respectively. Both of the analysis had same significantly altered regions located in left precuneus (BA5/7), left occipital (BA19), left cuneus (BA18/19) and left calcarine (BA17/19) (two-tailed GRF correction, voxel level: P < .005; cluster level: P < .05). (B)The rFCS analysis. The left and the right are the rFCS differences without or with GM volume as covariates respectively. Similarly, both of the analysis had same significantly altered regions located in precuneus/PCC (BA7/31) (two-tailed GRF correction, voxel level: P < .005; cluster level: P < .05). The color bars indicate T-statistic. Abbreviations: iSCD, informant-reported subjective cognitive decline; aFCS, absolute functional connectivity strength; rFCS, relative functional connectivity strength; GM, gray matter.
3.5. Cortical differences
Because five participants (three iSCD, two HC) of our samples had unsatisfactory 3D T1-weighted scans, we compared the cortical thickness of 36 iSCD participants and 37 healthy controls. No significant differences in cortical thickness were observed after false discovery rate correction between iSCD and healthy controls.
4. Discussion
In this study, we examined the differences in FCS between participants with iSCD and age- and sex-matched healthy controls. Relative to healthy controls, individuals with iSCD had lower aFCS in regions, which are main components of DMN and the visual pathway. Individuals with iSCD also showed higher rFCS in PCC/precuneus in the left hemisphere. No significant structural (e.g., cortical thickness) group differences were found in the present study, suggesting that the functional changes (e.g., FCS) may be an early feature of cognitive decline. These data indicate that iSCD and healthy controls had significantly different patterns of FCS, which could be considered as the earliest evidence of neurocognitive decline before cognitive impairment became apparent on objective testing.
We observed that a set of regions showed decreased aFCS, partly supporting the idea that magnitude of whole-brain connectivity decreases in the course of disease progression [23]. Regionally, we found decreases of aFCS mostly in the precuneus, cuneus, parietal, medial superior frontal, and visual cortices. These regions are involved in high-level cognitive functions and decision-making. Specifically, medial frontal cortex is relevant to different aspects of social cognitive processing [24], medial prefrontal cortex has been implicated in self-related cognitive processing [25], parietal cortex contributes to episodic memory retrieval [26] and cuneus/precuneus are involved in learning and memory [27]. The changes in functional connectivity vary in the course of the disease and appear to be commensurate with disease severity in, for example, depression [28] and AD [29]. There has been considerable interest in examining the disruption of the brain's functional networks in AD and other dementias [12], [30], but investigations at the preclinical stage of SCD have been limited. Self-reported SCD was shown to have lower functional connectivity than healthy controls [31], and older adults with informant-verified cognitive complaints also showed lower DMN connectivity than healthy controls [9]. Our results are consistent with these findings.
In the present study, we compared the whole brain strength of functional connectivity in the two groups, permitting a more comprehensive characterization for the FCS property of each voxel. We investigated the highly connected regions, which were considered essential for optimal cognitive functioning. We found that the two groups exhibited similar FCS patterns: the regions with high connectivity were located primarily in the parts of DMN regions (including precuneus, cuneus, and parietal) and visual cortex (e.g., occipital), consistent with previous functional network studies [13], [29]. DMN is one of the earlier and most well-studied networks, and it is a set hub regions including the PCC/precuneus, medial prefrontal cortex, and lateral parietal cortex. DMN exhibits increased activity in the resting state, which is suppressed during cognitive tasks [32], [33], suggesting that DMN is fundamental for modulating cognitive processing [29]. Furthermore, the regions that are part of the structural core and the rich club, namely the cuneus, precuneus, medial superior frontal and parietal lobe, largely overlap with the regions of the DMN [30], [34]. These were also the regions where aFCS was significantly decreased in iSCD, suggesting that these specific brain hubs might be preferentially targeted by iSCD pathology.
Beyond parts of the DMN regions, the iSCD also exhibited decreased aFCS in bilateral calcarine regions, which are the main components of the visual cortices. A previous study showed that activity in the calcarine cortex was strongly correlated with spatial working memory response times, specifically at elementary memory load [35]. Zhang also found that individuals with AD had reduced connectivity with PCC in the bilateral visual cortex, right inferior parietal lobe, ventral medial prefrontal cortex and precuneus [29], and they suggested that the advancing functional connectivity deficits in the region of the visual cortex could also indicate AD progression. These studies provide crucial evidence that disrupted aFCS in DMN and visual cortex may lead to dysfunction in some cognitive task processing, and thereby contribute to informant-reported memory impairment.
Interestingly, our study showed that aFCS in precuneus was lower in iSCD relative to healthy controls, while the rFCS in precuneus was higher. PCC/precuneus is a highly connected and metabolically active brain region [36]. At the cognitive level, PCC was shown to play an important role in regulating the focus of attention [37], and one influential hypothesis is that the PCC plays a central role in supporting internally directed cognition [33], [38]. While the lower aFCS in precuneus indicated disturbed functional connectivity in iSCD, the greater rFCS in a region suggests that there was more functional or “level of hub” connectivity than other brain regions in iSCD compared to controls [13]. On the other hand, decreased aFCS but increased rFCS in precuneus may suggest an even greater decrease of aFCS in other brain areas for iSCD. We suggest that high rFCS in individuals at greater risk for dementia can be interpreted as part of a compensatory process for the loss. Thus, PCC/precuneus may play a compensatory role in the very early stage of preclinical dementia and more dynamically activate to balance brain workload than that of healthy controls. Another possible explanation is that the brain FCS is remodeled due to its plasticity after impairment of original brain topological networks. Together, our findings provide further support for the importance of the PCC/precuneus abnormalities in informant-reported cognitive decline.
As the central core of the DMN [38], PCC/precuneus has been described as one of the most important hubs in the brain [34]. The integrity of functional connectivity in PCC/precuneus is required to support healthy information flow, thus supporting normal functioning in many cognitive domains [36]. Because of the disturbed aFCS or other damage throughout the brain, the processing load may be forced to come toward the highly connected regions (e.g., precuneus), potentially improving the relative status of the precuneus in iSCD [39]. First, persistent hyper connectivity in some regions may place neurons under undue metabolic stress, reducing their viability and rendering them susceptible to degeneration [40], [41]. In addition, the structural and functional properties of hub regions might also predispose these regions for pathology, more so than other regions [30], [42]. Furthermore, some affective changes may relate to higher functional connectivity in regions critical for social-emotional processing [43]. Our findings suggest that the functional relevance of the PCC/precuneus is possibly increased when aFCS of other regions in iSCD is disturbed, in order to maintain the overall brain functioning. This important finding is worthy of independent replication.
We would like to point out that most regions with altered FCS were located in left side of the brain, including left medial superior frontal, left PCC/precuneus, left parietal, and left calcarine cortex. Previous findings [21], [29], [44] found that the left side of brain was more seriously affected in AD, both metabolically and structurally. Our results were partly similar to these findings. We speculate that the left side of the brain with altered FCS may be easily influenced in the course of disease progression, but future studies are needed to further explore.
Our findings should also be viewed in the context of the known progression of pathology in AD. All regions of decreased aFCS in the present study were mainly located in the posteromedial part of the brain network, regions that are particularly vulnerable for amyloid pathology at an early stage of the disease. Previous studies indicate that Amyloid β preferentially aggregates in areas of high intrinsic connectivity [45], especially in the default network [13], [46]. The presence of subjective cognitive impairment/decline was associated with greater β-amyloid and tau burdens [7], [47], [48], [49], and SCD was also regarded as an early indicator of neuropathology, including tauopathy and amyloid deposition, in clinically healthy older adults [48], [50]. Multiple biological factors must be considered when assessing SCD in clinically cognitively normal [8], therefore future studies are needed to use multimodal imaging in a fully data-driven way, which can help elucidate the complex relationship between imaging findings, neuropathology and preclinical SCD.
Our study has a number of limitations. First, the diagnosis of iSCD is subject to reporting bias, because complaints from informants can be influenced by a number of psychological factors [19]. Second, we did not have data from positron-emission tomography imaging for amyloid and tau, which may be associated with iSCD. SCD is a complex syndrome with great heterogeneity that is likely to be reflected in the neuroimaging findings, and future studies are needed to explore deeply in a fully data driven manner. Finally, this is a cross-sectional study and longitudinal studies are needed to assess the changes of FCS with the progression of the disease.
In conclusion, using r-fMRI, we were able to detect abnormalities of FCS in brain networks in iSCD which arguably is an early pre-clinical stage of dementia. Of particular interest is the abnormality in some parts of the DMN, and the possible compensatory role of the precuneus. The altered patterns in iSCD may help elucidate the complex course of cognitive decline in the elderly, which may serve as a biomarker of very early change, with relevance to prevention strategies in the future.
Research in Context.
-
1.
Systematic review: The authors reviewed the literature using traditional (e.g., PubMed) sources as well as meeting abstracts and presentations. While the whole brain functional connectivity strength (FCS) changes measured by the voxel-wise weighted degree centrality in informant-based Subjective Cognitive Disorder is not yet widely studied, there have been several recent publications describing the functional connectivity in SCD using different measures, which are cited as appropriate.
-
2.
Interpretation: We found lower absolute FCS in memory-related regions in informant-based Subjective Cognitive Disorder compared with controls, indicating disturbed functional connectivity at an early predementia stage. However, relative FCS was higher in the precuneus, suggesting a possible compensatory role for this region.
-
3.
Future directions: The manuscript proposes a framework for additional studies to further understand: (a) informants' bias in the evaluation of SCD; (b) the influences of amyloid β levels on inter-group FCS changes; and (d) the longitudinal changes in FCS with the progression of disease.
Acknowledgments
The authors thank all the participants in the Sydney Memory and Aging Study. This research received support from the Natural Science Foundation of China (Grant No. 81871434) and the National Health and Medical Research Council (NHMRC) Program Grants of Australia (350833, 56896, 109308).
Footnotes
Conflict of interest: none.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.dadm.2018.08.011.
Supplementary data
References
- 1.Mitchell A.J., Beaumont H., Ferguson D., Yadegarfar M., Stubbs B. Risk of dementia and mild cognitive impairment in older people with subjective memory complaints: meta-analysis. Acta Psychiatr Scand. 2014;130:439–451. doi: 10.1111/acps.12336. [DOI] [PubMed] [Google Scholar]
- 2.Ossenkoppele R., Jagust W.J. The Complexity of Subjective Cognitive Decline. JAMA Neurol. 2017;74:1400–1402. doi: 10.1001/jamaneurol.2017.2224. [DOI] [PubMed] [Google Scholar]
- 3.Reisberg B., Prichep L., Mosconi L., John E.R., Glodzik-Sobanska L., Boksay I. The pre-mild cognitive impairment, subjective cognitive impairment stage of Alzheimer's disease. Alzheimer's & dementia. J Alzheimers Assoc. 2008;4:S98–S108. doi: 10.1016/j.jalz.2007.11.017. [DOI] [PubMed] [Google Scholar]
- 4.Jessen F., Amariglio R.E., Van Boxtel M., Breteler M., Ceccaldi M., Chételat G. A conceptual framework for research on subjective cognitive decline in preclinical Alzheimer's disease. Alzheimers Dement. 2014;10:844–852. doi: 10.1016/j.jalz.2014.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Caselli R.J., Chen K., Locke D.E., Lee W., Roontiva A., Bandy D. Subjective cognitive decline: self and informant comparisons. Alzheimer's & dementia. J Alzheimers Assoc. 2014;10:93–98. doi: 10.1016/j.jalz.2013.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rueda A.D., Lau K.M., Saito N., Harvey D., Risacher S.L., Aisen P.S. Self-rated and informant-rated everyday function in comparison to objective markers of Alzheimer's disease. Alzheimers Dement. 2015;11:1080–1089. doi: 10.1016/j.jalz.2014.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Swinford C.G., Risacher S.L., Charil A., Schwarz A.J., Saykin A.J. Memory concerns in the early Alzheimer's disease prodrome: Regional association with tau deposition. Alzheimers Dement (Amst) 2018;10:322–331. doi: 10.1016/j.dadm.2018.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rabin L.A., Smart C.M., Amariglio R.E. Subjective Cognitive Decline in Preclinical Alzheimer's Disease. Annu Rev Clin Psychol. 2017;13:369–396. doi: 10.1146/annurev-clinpsy-032816-045136. [DOI] [PubMed] [Google Scholar]
- 9.Wang Y., Risacher S.L., West J.D., McDonald B.C., Magee T.R., Farlow M.R. Altered default mode network connectivity in older adults with cognitive complaints and amnestic mild cognitive impairment. J Alzheimers Dis. 2013;35:751–760. doi: 10.3233/JAD-130080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Contreras J.A., Goni J., Risacher S.L., Amico E., Yoder K., Dzemidzic M. Cognitive complaints in older adults at risk for Alzheimer's disease are associated with altered resting-state networks. Alzheimers Dement (Amst) 2017;6:40–49. doi: 10.1016/j.dadm.2016.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sun Y., Dai Z., Li Y., Sheng C., Li H., Wang X. Subjective Cognitive Decline: Mapping Functional and Structural Brain Changes-A Combined Resting-State Functional and Structural MR Imaging Study. Radiology. 2016;281:185–192. doi: 10.1148/radiol.2016151771. [DOI] [PubMed] [Google Scholar]
- 12.Dai Z.J., Yan C.G., Li K.C., Wang Z.Q., Wang J.H., Cao M. Identifying and Mapping Connectivity Patterns of Brain Network Hubs in Alzheimer's Disease. Cereb Cortex. 2015;25:3723–3742. doi: 10.1093/cercor/bhu246. [DOI] [PubMed] [Google Scholar]
- 13.Buckner R.L., Sepulcre J., Talukdar T., Krienen F.M., Liu H., Hedden T. Cortical hubs revealed by intrinsic functional connectivity: mapping, assessment of stability, and relation to Alzheimer's disease. J Neurosci. 2009;29:1860–1873. doi: 10.1523/JNEUROSCI.5062-08.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sachdev P.S., Brodaty H., Reppermund S., Kochan N.A., Trollor J.N., Draper B. The Sydney Memory and Ageing Study (MAS): methodology and baseline medical and neuropsychiatric characteristics of an elderly epidemiological non-demented cohort of Australians aged 70-90 years. Int Psychogeriatr. 2010;22:1248–1264. doi: 10.1017/S1041610210001067. [DOI] [PubMed] [Google Scholar]
- 15.Folstein M.F., Folstein S.E., McHugh P.R. “Mini-mental state”: A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 16.Hindmarch I., Lehfeld H., de Jongh P., Erzigkeit H. The Bayer activities of daily living scale (B-ADL) Dement Geriatr Cogn. 1998;9:20–26. doi: 10.1159/000051195. [DOI] [PubMed] [Google Scholar]
- 17.Jorm A.F. A short form of the Informant Questionnaire on Cognitive Decline in the Elderly (IQCODE): development and cross-validation. Psychol Med. 1994;24:145–153. doi: 10.1017/s003329170002691x. [DOI] [PubMed] [Google Scholar]
- 18.Brodaty H., Pond D., Kemp N.M., Luscombe G., Harding L., Berman K. The GPCOG: A new screening test for dementia designed for general practice. J Am Geriatr Soc. 2002;50:530–534. doi: 10.1046/j.1532-5415.2002.50122.x. [DOI] [PubMed] [Google Scholar]
- 19.Slavin M.J., Brodaty H., Kochan N.A., Crawford J.D., Trollor J.N., Draper B. Prevalence and Predictors of “Subjective Cognitive Complaints” in the Sydney Memory and Ageing Study. Am J Geriatr Psychiatry. 2010;18:701–710. doi: 10.1097/jgp.0b013e3181df49fb. [DOI] [PubMed] [Google Scholar]
- 20.Fischl B., Dale A.M. Measuring the thickness of the human cerebral cortex from magnetic resonance images. Proc Natl Acad Sci U S A. 2000;97:11050–11055. doi: 10.1073/pnas.200033797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Thompson P.M., Hayashi K.M., de Zubicaray G., Janke A.L., Rose S.E., Semple J. Dynamics of gray matter loss in Alzheimer's disease. J Neurosci. 2003;23:994–1005. doi: 10.1523/JNEUROSCI.23-03-00994.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Oakes T.R., Fox A.S., Johnstone T., Chung M.K., Kalin N., Davidson R.J. Integrating VBM into the General Linear Model with voxelwise anatomical covariates. NeuroImage. 2007;34:500–508. doi: 10.1016/j.neuroimage.2006.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sheline Y.I., Raichle M.E. Resting state functional connectivity in preclinical Alzheimer's disease. Biol Psychiatry. 2013;74:340–347. doi: 10.1016/j.biopsych.2012.11.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Amodio D.M., Frith C.D. Meeting of minds: the medial frontal cortex and social cognition. Nat Rev Neurosci. 2006;7:268–277. doi: 10.1038/nrn1884. [DOI] [PubMed] [Google Scholar]
- 25.Northoff G., Bermpohl F. Cortical midline structures and the self. Trends Cognitive Sciences. 2004;8:102–107. doi: 10.1016/j.tics.2004.01.004. [DOI] [PubMed] [Google Scholar]
- 26.Wagner A.D., Shannon B.J., Kahn I., Buckner R.L. Parietal lobe contributions to episodic memory retrieval. Trends Cognitive Sciences. 2005;9:445–453. doi: 10.1016/j.tics.2005.07.001. [DOI] [PubMed] [Google Scholar]
- 27.Price D.D. Psychological and neural mechanisms of the affective dimension of pain. Science. 2000;288:1769–1772. doi: 10.1126/science.288.5472.1769. [DOI] [PubMed] [Google Scholar]
- 28.Greicius M.D., Flores B.H., Menon V., Glover G.H., Solvason H.B., Kenna H. Resting-state functional connectivity in major depression: abnormally increased contributions from subgenual cingulate cortex and thalamus. Biol Psychiatry. 2007;62:429–437. doi: 10.1016/j.biopsych.2006.09.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zhang H.Y., Wang S.J., Liu B., Ma Z.L., Yang M., Zhang Z.J. Resting Brain Connectivity: Changes during the Progress of Alzheimer Disease. Radiology. 2010;256:598–606. doi: 10.1148/radiol.10091701. [DOI] [PubMed] [Google Scholar]
- 30.Crossley N.A., Mechelli A., Scott J., Carletti F., Fox P.T., McGuire P. The hubs of the human connectome are generally implicated in the anatomy of brain disorders. Brain. 2014;137:2382–2395. doi: 10.1093/brain/awu132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lopez-Sanz D., Bruna R., Garces P., Martin-Buro M.C., Walter S., Delgado M.L. Functional Connectivity Disruption in Subjective Cognitive Decline and Mild Cognitive Impairment: A Common Pattern of Alterations. Front Aging Neurosci. 2017;9:109. doi: 10.3389/fnagi.2017.00109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Greicius M.D., Krasnow B., Reiss A.L., Menon V. Functional connectivity in the resting brain: a network analysis of the default mode hypothesis. Proc Natl Acad Sci U S A. 2003;100:253–258. doi: 10.1073/pnas.0135058100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Raichle M.E., MacLeod A.M., Snyder A.Z., Powers W.J., Gusnard D.A., Shulman G.L. A default mode of brain function. Proc Natl Acad Sci U S A. 2001;98:676–682. doi: 10.1073/pnas.98.2.676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.van den Heuvel M.P., Sporns O. Network hubs in the human brain. Trends Cognitive Sciences. 2013;17:683–696. doi: 10.1016/j.tics.2013.09.012. [DOI] [PubMed] [Google Scholar]
- 35.Valenzuela M.J., Turner A.J., Kochan N.A., Wen W., Suo C., Hallock H. Posterior compensatory network in cognitively intact elders with hippocampal atrophy. Hippocampus. 2015;25:581–593. doi: 10.1002/hipo.22395. [DOI] [PubMed] [Google Scholar]
- 36.Leech R., Sharp D.J. The role of the posterior cingulate cortex in cognition and disease. Brain. 2014;137:12–32. doi: 10.1093/brain/awt162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hahn B., Ross T.J., Stein E.A. Cingulate activation increases dynamically with response speed under stimulus unpredictability. Cereb Cortex. 2007;17:1664–1671. doi: 10.1093/cercor/bhl075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Buckner R.L., Andrews-Hanna J.R., Schacter D.L. The brain's default network - Anatomy, function, and relevance to disease. Ann Ny Acad Sci. 2008;1124:1–38. doi: 10.1196/annals.1440.011. [DOI] [PubMed] [Google Scholar]
- 39.Stam C.J. Modern network science of neurological disorders. Nat Rev Neurosci. 2014;15:683–695. doi: 10.1038/nrn3801. [DOI] [PubMed] [Google Scholar]
- 40.Fornito A., Zalesky A., Breakspear M. The connectomics of brain disorders. Nat Rev Neurosci. 2015;16:159–172. doi: 10.1038/nrn3901. [DOI] [PubMed] [Google Scholar]
- 41.Filippi M., Basaia S., Canu E., Imperiale F., Meani A., Caso F. Brain network connectivity differs in early-onset neurodegenerative dementia. Neurology. 2017;89:1764–1772. doi: 10.1212/WNL.0000000000004577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Meijer K.A., Eijlers A.J.C., Douw L., Uitdehaag B.M.J., Barkhof F., Geurts J.J.G. Increased connectivity of hub networks and cognitive impairment in multiple sclerosis. Neurology. 2017;88:2107–2114. doi: 10.1212/WNL.0000000000003982. [DOI] [PubMed] [Google Scholar]
- 43.Fredericks C.A., Sturm V.E., Brown J.A., Hua A.Y., Bilgel M., Wong D.F. Early Affective Changes and Increased Connectivity in Preclinical Alzheimer's Disease. Alzheimer's & Dementia: Diagnosis, Assessment & Disease Monitoring. 2018;10:471–479. doi: 10.1016/j.dadm.2018.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Janke A.L., de Zubicaray G., Rose S.E., Griffin M., Chalk J.B., Galloway G.J. 4D deformation modeling of cortical disease progression in Alzheimer's dementia. Magn Reson Med. 2001;46:661–666. doi: 10.1002/mrm.1243. [DOI] [PubMed] [Google Scholar]
- 45.Myers N., Pasquini L., Gottler J., Grimmer T., Koch K., Ortner M. Within-patient correspondence of amyloid-beta and intrinsic network connectivity in Alzheimer's disease. Brain. 2014;137:2052–2064. doi: 10.1093/brain/awu103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Vlassenko A.G., Vaishnavi S.N., Couture L., Sacco D., Shannon B.J., Mach R.H. Spatial correlation between brain aerobic glycolysis and amyloid-β (Aβ) deposition. Proc Natl Acad Sci U S A. 2010;107:17763–17767. doi: 10.1073/pnas.1010461107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Visser P.J., Verhey F., Knol D.L., Scheltens P., Wahlund L.O., Freund-Levi Y. Prevalence and prognostic value of CSF markers of Alzheimer's disease pathology in patients with subjective cognitive impairment or mild cognitive impairment in the DESCRIPA study: a prospective cohort study. Lancet Neurol. 2009;8:619–627. doi: 10.1016/S1474-4422(09)70139-5. [DOI] [PubMed] [Google Scholar]
- 48.Buckley R.F., Hanseeuw B., Schultz A.P., Vannini P., Aghjayan S.L., Properzi M.J. Region-Specific Association of Subjective Cognitive Decline With Tauopathy Independent of Global beta-Amyloid Burden. JAMA Neurol. 2017;74:1455–1463. doi: 10.1001/jamaneurol.2017.2216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Vannini P., Hanseeuw B., Munro C.E., Amariglio R.E., Marshall G.A., Rentz D.M. Hippocampal hypometabolism in older adults with memory complaints and increased amyloid burden. Neurology. 2017;88:1759–1767. doi: 10.1212/WNL.0000000000003889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hu X., Uhle F., Fliessbach K., Wagner M., Han Y., Weber B. Reduced future-oriented decision making in individuals with subjective cognitive decline: A functional MRI study. Alzheimers Dement (Amst) 2017;6:222–231. doi: 10.1016/j.dadm.2017.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.