Abstract
A 71-year-old male appeared at the facility complaining of disturbance of consciousness and bilateral papilledema. The laboratory test revealed anemia and coagulation abnormality. A physical examination and magnetic resonance imaging (MRI) of the brain with and without gadolinium showed no abnormalities. A lumbar puncture showed a high pressure, but a normal cerebrospinal fluid (CSF) cell count. Cerebral angiography showed no morphological abnormalities, but it revealed an asymmetric right dominant type of confluence of the sinuses with the partially-communicating left transverse sinus in the late phase. Furthermore, there was a delay in the cerebral circulation time (CCT). Subsequently, venography and ultrasonography revealed right internal jugular vein thrombosis associated with lung cancer. The patient recovered from the disturbance of consciousness immediately after an emergency ventriculoperitoneal shunt and anticoagulation therapy. This case was diagnosed as secondary pseudotumor cerebri (PTC). In order to facilitate the early detection of secondary PTC, it is important to take note of symptoms of intracranial hypertension with no remarkable intracranial lesions and to consider the possibility of PTC, especially in the patients with high risk factors for coagulopathy including lung cancer.
Keywords: Cerebral circulation time, Confluence of sinuses (torcular Herophili), Idiopathic intracranial hypertension, Jugular vein thrombosis, Lung cancer, Pseudotumor cerebri
Highlights
-
•
A case of pseudotumor cerebri (PTC) caused by jugular vein thrombosis (JVT) is presented.
-
•
PTC was induced by the blockage of cerebral venous outflow caused by the JVT.
-
•
JVT was associated with hyper coagulopathy due to the lung cancer.
-
•
The blockage was also caused by asymmetric ipsilateral (right) dominant type of confluence of sinuses.
-
•
Physicians should pay attention to PTC caused by the JVT and the anatomical variation of confluence of sinuses.
1. Introduction
Pseudotumor cerebri (PTC), also known as idiopathic intracranial hypertension (IIH), is a condition associated with increased intracranial pressure in the absence of radiographic findings, such as mass lesions or ventriculomegaly [[1], [2], [3]]. The concept of PTC, introduced by Nonne in 1904, has developed historically along with neuroimaging [1,4]. Here, we report a case of secondary PTC caused by jugular vein thrombosis (JVT) associated with lung cancer, and consider the related anatomical variations of the superior sagittal sinus (SSS), confluence of sinuses (CS; torchlar Herophili), and transverse sinus (TS).
2. Case presentation
A 71-year-old male was transferred to our facility with disturbance of consciousness (Glasgow Coma Scale; GCS of E3V4M6). Bilateral papilledema was present. The laboratory test revealed anemia and coagulation abnormality (Table 1). Computed tomography (CT) without contrast material and magnetic resonance imaging (MRI) of the brain with and without gadolinium showed no intrusive mass, hydrocephalus, or any other structural lesion. A lumbar puncture showed an opening pressure of 510 mm H2O with normal CSF cell count. This case was diagnosed tentatively as PTC or IIH. On the second day, after being admitted to the hospital, the patient deteriorated to a comatose state (GCS of E1V1M4). Cerebral angiography showed no morphological abnormalities, but it revealed an asymmetric right dominant type of confluence of the sinuses with the partially-communicating left transverse sinus in the venous phase (Fig. 1). Furthermore, there was a delay in the cerebral circulation time (CCT) [5] of 9 s. Subsequently, venography of the right internal jugular vein (IJV) and ultrasonography revealed right internal jugular vein thrombosis (Fig. 2A and C). The patient recovered from the disturbance of consciousness immediately after an emergency ventriculoperitoneal shunt and subsequent anticoagulation therapy using warfarin at a dose of 3 mg/day. IJV venography and ultrasonography showed the resolution and recanalization of the right JVT (Fig. 2B and D).
Table 1.
Laboratory data on admission.
| Hematology | Coagulation | Biochemistry |
|---|---|---|
| WBC 8200 /μL | PT 100% | AST 24 IU/L |
| RBC 4.27 × 106/μL | PT-INR 1.1 | ALT 21 IU/L |
| Hb 9.4 g/dL | APTT 21.9 s. | LDH 561 IU/L |
| Ht 28.8% | Fbg 278 mg/dL | T-Bil 0.8 mg/dL |
| PLT 12.3 × 104/μL | FDP 15.2 μg/mL | ALP 229 IU/L |
| D-dimer 5.6 μg/mL | BUN 22.1 mg/dL | |
| Cr 0.8 mg/dL | ||
| Na 136 mEq/dL | ||
| K 4.1 mEq/dL | ||
| Cl 101 mEq/dL | ||
| CRP 0.8 mg |
WBC: white blood cell, RBC: red blood cell, prothrombin time, Hb: Hemoglobin, PLT: platelet, PT: prothrombin time, PT-INR: prothrombin time international normalized ratio, APTT: activated partial thromboplastin time, Fbg: fibrinogen, FDP: fibrinogen/fibrin degradation products, CRP: C-reactive protein,
Fig. 1.

This figure shows the late phase of the internal carotid artery angiogram in frontal projection and indicates the right dominant confluence of the sinuses with the partially-communicating left transverse sinus (TS). The arrows indicate the superior sagittal sinus and the right TS. The arrowheads indicate the left TS.
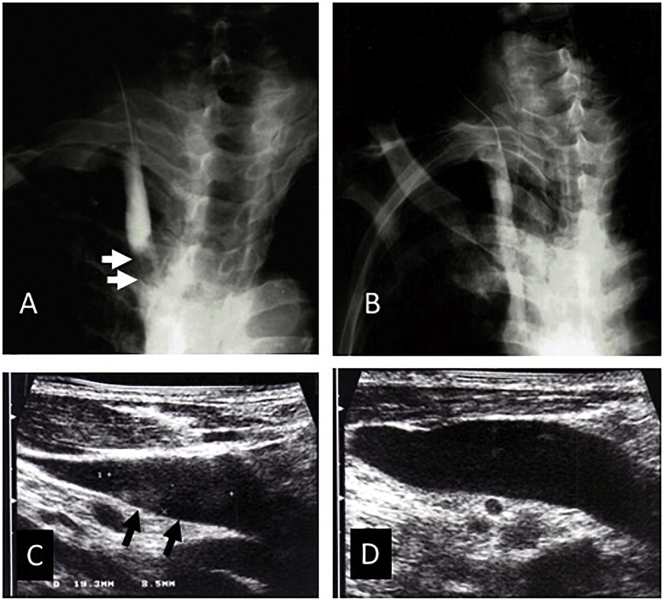
Fig. 2.
(A) The pre-therapeutic venogram of the right internal jugular vein (IJV), in frontal projection, shows the obstruction of the lower IJV. The arrows indicate the filling defect of the jugular vein thrombosis (JVT). (B) A post-therapeutic venogram obtained after anticoagulation therapy using warfarin shows the resolution and recanalization of the JVT.
(C) A pre-therapeutic ultrasonogram of the right internal jugular vein (IJV) shows the jugular vein thrombosis (JVT). The arrows indicate the thrombus in the right IJV.
(D) A post-therapeutic ultrasonogram after the anticoagulation therapy using warfarin shows the resolution and recanalization of the JVT.
On the other hand, a chest X-ray of this patient revealed an atelectasis in the right upper lobe of the lung. A CT of the chest confirmed the presence of the mass together with mediastinal and neck lymph nodes. A biopsy revealed the presence of an infiltrating adenocarcinoma.
3. Discussion
A definite diagnosis of pseudotumor cerebri syndrome requires the following criteria [3]: (A) Papilledema, (B) Normal neurologic examination findings except for cranial nerve abnormalities, (C) Neuroimaging; Normal brain parenchyma without any evidence of hydrocephalus, intrusive mass, or structural lesion, and no abnormal meningeal enhancement on MRI, with and without gadolinium, for typical patients (female and obese), and MRI, with and without gadolinium, and magnetic resonance venography for others, (D) Normal CSF composition, (E) Elevated lumbar puncture opening pressure (250 mm CSF in adults in a properly performed lumbar puncture). Based on these criteria, the patient was diagnosed definitely as PTC.
CCT was determined by angiography of the carotid artery and taken, according to Greitz, at an interval between the maximum contrast filling of the carotid siphon and the maximum filling of parietal veins [5]. The normal limit of CCT is from 2.5 to 6 s (the average is 4.3 s). The delay shown in the CCT, in the venous phase of the angiography, which showed the right dominant transverse sinus with partially-communicating left transverse sinus, the venography findings and the ultrasonography indicated that the PTC of this patient may have been induced by the blockage of cerebral venous outflow caused by JVT associated with hyper coagulopathy due to the adenocarcinoma of the lung.
The risk of venous thrombosis in lung cancer patients is increased in compared to the general population. Furthermore, patients with adenocarcinoma have a higher risk than patients with squamous cell carcinoma [6]. To the best of our knowledge, there is no previous report of the case with PTC and lung cancer. We must emphasize the fact because the incidence of lung cancer is and will be increasing especially in Japan.
In regard to the morphological aspects, it is important to interpret the anatomical variations of the CS. Since the fetal CS is plexiform, the possible adult patterns are numerous. Subsequently, many variations have been reported in the dural sinuses. The SSS drains typically somewhat preferentially towards the right TS, while the straight sinus passes typically into the left TS [7].
In order to discuss the anatomical relationship between the right internal jugular vein thrombosis and increased intracranial pressure, we conducted literature review of anatomical variations of CS (Torcular Herophili) by cadaver dissection. In the review, the words, ‘anatomy’, ‘torcular’, ‘Herophili’ were selected as search terms using PubMed on the October 1, 2018. As a result, 63 articles were retrieved and 6 of 63 ones were selected as related and well-written studies to our own patient case [[8], [9], [10], [11], [12], [13]]. Furthermore, other 4 studies were added from the references of the selected articles [[14], [15], [16], [17]].
These studies showed that the symmetric group of CS (confluence and bifurcation) accounted for about a half of the cases (31–76%), and the asymmetric right dominant type accounted for most of the rest of the cases (17–53%), while the asymmetric left dominant type accounted for the remaining cases (3–16%) [[8], [9], [10], [11], [12], [13], [14], [15], [16], [17]]. In compared to these anatomical variations of the CS, the characteristic of our own case is the asymmetric right dominant type.
Several previous reports have described cases with PTC following internal jugular vein catheterization, unilateral radial neck dissection, or hyper coagulopathy [[18], [19], [20], [21], [22]]. In these cases, it was assumed that the cause of the PTC was the draining pattern from the SSS to the TS. In the event of JVT due to catheterization or radial neck dissection on a patient with the asymmetric ipsilateral dominant type of confluence, the patient will be deprived of the major venous drainage from the cerebrum, which may provoke PTC.
In summary, the secondary PTC found in this case was likely caused by the right internal jugular vein thrombosis, precipitated by hyper coagulopathy due to lung cancer and the asymmetric right dominant type of CS. In order to avoid secondary PTC or to facilitate early detection, it is important for physicians to take note of any symptoms of intracranial hypertension, even with no evidence of remarkable intracranial lesions and to consider the possibility of PTC. This is especially true in patients with high risk factors for coagulopathy and the asymmetrical unilateral dominant type of CS.
Acknowledgments
Acknowledgements
This work was supported by a Grant-in-Aid for Scientific Research (C) 15K10360, (C) 17K01481, Grants-in-Aid from The Ministry of Education, Culture, Sports, Science, and Technology (MEXT) for Scientific Research (25282247 and 15K12770), and Scientific Researches on Innovative Areas “Adaptive Circuit Shift” (26112001).
Conflicts of interest
None of the authors have any conflicts of interest to report.
References
- 1.Degnan A.J., Levy L.M. Pseudotumor cerebri: brief review of clinical syndrome and imaging findings. AJNR. 2011;32:1986–1993. doi: 10.3174/ajnr.A2404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Friedman D.I., Jacobson D.M. Diagnostic criteria for idiopathic intracranial hypertension. Neurology. 2002;59:1492–1495. doi: 10.1212/01.wnl.0000029570.69134.1b. [DOI] [PubMed] [Google Scholar]
- 3.Friedman D.I., Liu G.T., Digre K.B. Revised diagnostic criteria for the pseudotumor cerebri syndrome in adults and children. Neurology. 2013;81:1159–1165. doi: 10.1212/WNL.0b013e3182a55f17. [DOI] [PubMed] [Google Scholar]
- 4.Johnston I. The historical development of the pseudotumor concept. Neurosurg. Focus. 2001;11 doi: 10.3171/foc.2001.11.2.3. [DOI] [PubMed] [Google Scholar]
- 5.Greitz T. A radiologic study of the brain circulation by rapid serial angiography of the carotid artery. Acta Radiol. Suppl. 1956;1956:1–123. [PubMed] [Google Scholar]
- 6.Blom J.W., Osanto S., Rosendaal R. The risk of a venous thrombotic event in lung cancer patients: higher risk for adenocarcioma than squamous cell carcinoma. J. Thromb. Haemost. 2004;2:1760–1765. doi: 10.1111/j.1538-7836.2004.00928.x. [DOI] [PubMed] [Google Scholar]
- 7.Lasjaunias P., Berenstein A., ter Brugge K.G. Surgical Neuroangiography. Springer-Verlag; Berlin, Heidelberg, New York: 2001. Intracranial venous system; pp. 631–713. [Google Scholar]
- 8.Bisaria K.K. Anatomic variations of venous sinuses in the region of the torcular Herophili. J. Neurosurg. 1985;62:90–95. doi: 10.3171/jns.1985.62.1.0090. [DOI] [PubMed] [Google Scholar]
- 9.Ishizaka H. Anatomical study of the torcular Herophili. Neurol. Med. Chir. (Tokyo) 1985;25:873–880. doi: 10.2176/nmc.25.873. (in Japanese with English abstract) [DOI] [PubMed] [Google Scholar]
- 10.Kaplan H.A., Browder J., Knightly J.J. Variations of the cerebral dural sinuses at the torcular herophili. Importance in radical neck dissection. Am. J. Surg. 1972;124:456–461. doi: 10.1016/0002-9610(72)90066-9. [DOI] [PubMed] [Google Scholar]
- 11.Matsuda W., Sonomura T., Honma S. Anatomical variations of the torcular Herophili: macroscopic study and clinical aspects. Anat. Sci. Int. 2018;93:464–468. doi: 10.1007/s12565-018-0436-z. [DOI] [PubMed] [Google Scholar]
- 12.Park H.K., Bae H.G., Choi S.K. Morphological study of sinus flow in the confluence of sinuses. Clin. Anat. 2008;21:294–300. doi: 10.1002/ca.20620. [DOI] [PubMed] [Google Scholar]
- 13.Singh M., Nagashima M., Inoue Y. Anatomical variations of occipital bone impressions for dural venous sinuses around the torcular Herophili, with special reference to the consideration of clinical significance. Surg. Radiol. Anat. 2004;26:480–487. doi: 10.1007/s00276-004-0269-4. [DOI] [PubMed] [Google Scholar]
- 14.Browning H. The confluence of dural venous sinuses. Am. J. Anat. 1953;93:307–329. doi: 10.1002/aja.1000930302. [DOI] [PubMed] [Google Scholar]
- 15.Edwards E.A. Anatomic variations of the cranial venous sinuses. Their relation to the effect of jugular compression in lumbar manometric tests. Arch. Neurol. Psychiatr. 1931;26:801–814. [Google Scholar]
- 16.Goto N., Koda M. Blood vessels in the central nervous system. In: Sato T., Akita K., editors. Anatomical Variations in Japanese. University of Tokyo Press; Tokyo: 2000. pp. 401–429. (in Japanese) [Google Scholar]
- 17.Woodhall B. Variations of the cranial venous sinuses in the region of the torcular Herophili. Arch. Surg. (Chicago) 1936;33:297–314. [Google Scholar]
- 18.Marr W.G., Chambers R.G. Pseudotumor cerebri syndrome following unilateral radical neck dissection. Am J. Ophthalmol. 1961;51:605–611. [PubMed] [Google Scholar]
- 19.Morfit H.M., Cleveland H., Jr. Permanent increased intracranial pressure following unilateral radical neck dissection. AMA Arch. Surg. 1958;76:713–719. doi: 10.1001/archsurg.1958.01280230053008. [DOI] [PubMed] [Google Scholar]
- 20.Stephens P.H., Lennox G., Hirsch N. Superior sagittal sinus thrombosis after internal jugular vein cannulation. Br. J. Anaesth. 1991;67:476–479. doi: 10.1093/bja/67.4.476. [DOI] [PubMed] [Google Scholar]
- 21.Suetterlin K., Borg N., Joy H. When is ‘idiopathic intracranial hypertension’ no longer idiopathic? Pract. Neurol. 2014;14:102–106. doi: 10.1136/practneurol-2013-000680. [DOI] [PubMed] [Google Scholar]
- 22.Perez M.A., Glaser J.S., Schatz N.J. "Idiopathic" intracranial hypertension caused by venous sinus thrombosis associated with contraceptive usage. Optometry. 2010;81:351–358. doi: 10.1016/j.optm.2010.01.010. [DOI] [PubMed] [Google Scholar]