Abstract
This pilot randomized clinical trial assessed the feasibility of implementing motor control exercise (MCE) and patient education (PE) program for the management of chronic low back pain (CLBP) in a low resource rural Nigerian community. Thirty patients with CLBP were recruited and randomly assigned to MCE, PE, or MCE plus PE groups. The MCE program was provided twice a week while the PE program was provided once a week all for 6 weeks. Feasibility was assessed through recruitment rate, treatment compliance, retention/dropout rate, report of adverse events, perceived helpfulness, overall satisfaction, and clinical outcome of pain (numeric pain rating scale) and functional disability (Oswestry Disability Index). Many patients were willing to participate in the study and the recruitment rate was 77%. Treatment compliance in all the three groups were >65% for supervised treatment sessions and <50% for prescribed home program. Retention rate was high and greater overall satisfaction with the interventions was reported. Compared with the baseline, all the three groups improved significantly in pain and disability (P<0.05) after 6 weeks. Pairwise comparison revealed that the MCE plus PE group was superior to the PE group for pain and to the MCE for disability (P<0.05), with large effect size. It was concluded that the designed interventions are promising and conducting a full-scale randomized clinical trial in the future is feasible to confirm the effectiveness of the interventions for the management CLBP in rural Nigeria. (Trial registration: ClinicalTrials.gov, NCT03398174)
Keywords: Chronic low back pain, Disability, Nigeria, Rural community, Motor control exercise, Patient education
INTRODUCTION
Low back pain (LBP) is one of the most prevalent musculoskeletal disorders that affect the well-being of many individuals. It is the leading cause of years lived with disability globally and imposes a significant economic burden on individuals, families, societies and governments (Hoy et al., 2010; Hoy et al., 2014). The impact, however, is likely to be more extreme in resource-constrained nations such as those situated in Africa where most people are rural residents and lack access to adequate health care (Hoy et al., 2010). Additionally, cultures and beliefs, as well as common practices such as peasant farming and heavy manual lifting, coupled with extreme poverty may intensify the impact of living with this condition (Hondras et al., 2016; Igwesi-Chidobe et al., 2017b; Omokhodion, 2002).
The annual LBP prevalence rates of 33%–74% estimated in Nigeria (Bello and Bello, 2017) is higher than the prevalence rates of 14%–51% reported in other African countries (Louw et al., 2007). The burden, however, seems to be greater among rural dwellers than urban dwellers as the prevalence rates of 40%–74% (Omokhodion, 2002; Tella et al., 2013) found in rural Nigeria is higher than the 44% rate found in urban Nigeria (Omokhodion, 2004). These figures are alarming and seem to suggest that Nigerians especially rural residents are likely to experience one of the greatest burdens of LBP (Igwesi-Chidobe et al., 2017a). Furthermore, results of cross-sectional studies conducted in rural Nigeria revealed that occupational biomechanical and psychosocial factors are likely to be associated with adverse outcomes of LBP (Igwesi-Chidobe et al., 2015; Igwesi-Chidobe et al., 2017a; Igwesi-Chidobe et al., 2017b; Omokhodion, 2002), with the latter being the most significant in explaining chronic low back pain (CLBP) disability (Igwesi-Chidobe et al., 2017a).
Despite the highlighted problems related to LBP in rural Nigeria, rehabilitation services are lacking. For instance, most physiotherapy outfits are confined to the cities and rural areas barely have access to this service even at the primary health care centre (Igwesi-Chidobe et al., 2012b). As a result, most rural dwellers in Nigeria have poor knowledge of the roles and scope of physiotherapy, poor healthcare-seeking behaviour, and patronize traditional health workers (Igwesi-Chidobe, 2012a).
Among the variety of conservative techniques used to address CLBP, exercise remains the most widely prescribed technique perhaps due to its efficacy in reducing pain and enhancing function in the adult management of CLBP (Hayden et al., 2005; van Middelkoop et al., 2010), even though effects are modest (van Middelkoop et al., 2010). While many forms of exercise exist, motor control exercise (MCE), also referred to as specific stabilization exercise is commonly used to manage CLBP. This exercise has been extensively researched and reported to be effective in reducing pain and disability among sufferers with CLBP (Byström et al., 2013; Gomes-Neto et al., 2017). Moreover, it appears to be commonly used by many physiotherapists in Nigeria for the rehabilitation of back pain disorders (Ganiyu and Gujba, 2015; Ibrahim and Akindele, 2018; Ojoawo et al., 2017; Sokunbi et al., 2015).
As CLBP is commonly linked with psychosocial factors such as fear-avoidance beliefs, catastrophizing, and negative emotions (Igwesi-Chidobe et al., 2017a; Ramond et al., 2011), such factors can be modified by providing educational training (Brox et al., 2008). Although different forms of patient education (PE) and how they are delivered exists in the literature, the most effective strategy for CLBP is still unclear (Dupeyron et al., 2011). However, PE incorporating at least part of cognitive-behavioural strategies with emphasis on self-management has been suggested by several reviews of literature (Dupeyron et al., 2011; Henrotin et al., 2006; Wood et al., 2016) and clinical practice guidelines (Chou et al., 2007; Delitto et al., 2012) as valuable approach to addressing CLBP.
Though exercise and education are essential and among the most commonly recommended nonpharmacological interventions for CLBP (Wong et al., 2017), community based randomized clinical trials using these interventions for rural dwellers with CLBP in Nigeria are lacking. In fact, most trials on exercise and or education for CLBP in Nigeria (Akodu and Akindutire, 2018; Aliyu et al., 2018; Johnson et al., 2010; Mbada et al., 2015; Odebiyi et al., 2009; Ojoawo et al., 2017; Sokunbi et al., 2015) are primarily hospital-based on urban patients who are likely to have higher literacy level and socioeconomic status compared to rural patients.
In view of the aforementioned research gaps, low-cost, accessible, and effective interventions aiming at these specific populations are therefore warranted and should be tested in the way of high-quality community randomized clinical trials. However, before conducting a large trial, it is considered important to carry out a pilot study or a preliminary investigation to assess the feasibility and acceptability of the study in order to avoid waste of resources (Thabane et al., 2010). The purpose of this study was therefore to assess the feasibility of implementing MCE and PE program in the management CLBP in a low resource rural Nigerian community.
MATERIALS AND METHODS
Study design
This study was a single-blind pilot randomized clinical trial, conducted at Tsakuwa Primary Healthcare Centre, located at Tsakuwa village of Dawakin-Kudu Local Government Area, Kano state, northwestern Nigeria. The study protocol was approved by the Health Research Ethics Committee, Ministry of Health Kano State (Ref: MOH/Off/797/T.I./632).
Participants and flow
A one-day village-wide announcement, facilitated by the village head (traditional ruler) of Tsakuwa was utilized to recruit patients with nonspecific CLBP from January to April 2018. The inclusion criteria were: (a) male and female between 18 and 65 years old, (b) primary complaint of LBP experienced at least over the previous 3 months, and (c) ability to read/understand English or Hausa language. The participants’ exclusion criteria were: (a) previous history of thoracic spine or lumbosacral spine surgery, (b) any neurological findings indicating radiculopathy, (c) evidence of serious spine pathology (e.g., tumor, infection, fracture, spinal stenosis, inflammatory disease), (d) Unstable or severe disabling chronic cardiovascular and pulmonary disease, (e) History of serious psychological or psychiatric illness, and (f) current pregnancy.
Eligibility criteria were ensured by the primary researcher through an interview and general physical examination. All eligible participants were given verbal information about the study procedures and potential risks of interventions. Eligible participants were advised to take home the information and consent forms and to discuss with their family to decide whether or not to participate in the study. We emphasized that only those willing to be assigned to either study arm and capable of committing to all treatment sessions should return to the health centre on a scheduled day. Participants were informed about their rights and freedom to withdraw from the study at any time without prejudice. Attendance to all supervised treatment sessions and prescribed home program were highly emphasized. All baseline assessment was performed prior to group allocation by a physiotherapist who did not participate in any part of the study. The baseline assessment involves the recording of socio-demographic variables and completion of self-reported clinical outcomes.
Randomization
Because this is a pilot study, a formal sample size calculation was not performed. However, we assumed that 30 participants would be adequate to give an understanding of the feasibility of the study.
All eligible participants were allocated to one of three study groups; MCE (n=10), PE (n=10), or MCE plus PE groups (n= 10) at a 1:1:1 ratio using simple random sampling based on an electronic randomization table generated by a computer software programme. Allocation concealment was ensured using consecutively numbered, sealed, and opaque envelopes. An independent person, who was not involved in any other aspects of the study, carried out the randomization procedures. Outcome assessors were blinded to the participants’ treatment allocation.
Outcome assessment
A priori feasibility criteria
The recruitment rate – expressed as the percentage of eligible study participants that consented to participation.
Treatment compliance – an acceptable level of treatment compliance was set at least 65% and 50% of the participants in all the three groups completing all the prescribed supervised and non-supervised treatment (home program) sessions, respectively.
Retention/dropout rate – retention rate was expressed as the percentage of participants who completed an assigned intervention. Dropout rate (loss to follow-up) was expressed as the percentage of participants who were lost during follow-up and it was not possible to collect outcome data. An acceptable retention rate was set at least half (50%) of the participants completing the assigned interventions.
Adverse events – all study participants were informed at the point of enrollment to contact the research coordinator via phone or during follow-up visits in case they experience any unexpected serious adverse event during the study.
Perceived helpfulness – perceived helpfulness of intervention was assessed by a 5-point Likert scale, with response scores from 0 to 4, where 0=not at all helpful; 1=a little helpful; 2=somewhat helpful; 3=almost helpful; and 4= very helpful.
Treatment satisfaction – overall satisfaction with treatment was assessed by a 5-point Likert scale, with response scores from 0 to 4, where 0=completely dissatisfied; 1=dissatisfied; 2=neither satisfied nor dissatisfied; 3=satisfied; and 4=very satisfied.
Clinical outcomes
Pain intensity – assessed by the numeric pain rating scale (NPRS; 0–10 cm), with 0 representing no pain and 10 worst imaginable pain (Ferreira-Valente et al., 2011). The NPRS proved to be valid and responsive scale for measuring pain intensity (Ferreira-Valente et al., 2011).
Functional disability – assessed by the Oswestry Disability Index (ODI; 0%–100%), with a higher score indicating higher disability (Waddell et al., 1993). The questionnaire was translated into Hausa using the recommended guidelines for translation and cross-cultural adaptation of self-reported measures (Beaton et al., 2000). Both pain and functional disability were assessed at baseline and after treatment.
Interventions
All the interventions were provided by licensed physiotherapists (including the primary researcher) experienced in the management of LBP. Common interventions for all the three groups were stretching and non-supervised aerobic exercises. Both MCE and stretching were provided individually under supervision, twice per week (12 sessions) for 6 weeks. The PE program preceded exposure to exercise and was provided only once a week for 6 weeks (6 sessions) by the primary researcher. Participants were told to carry out their exercise program consistent with their group treatment at least twice per day at home. Participants in the PE only group were instructed to perform only stretching and aerobics as their home program.
Patient education
The PE program was designed considering the recommendations of most international clinical practice guidelines (Wong et al., 2017) and a review on the management of spinal disorders in low-income communities (Chou et al., 2018). The content of the program included evidenced-based information adapted from “The Back Book” (Burton et al., 1999) and ‘The Pain Toolkit’ (Moore and Cole, 2009), advice on postural hygiene, and healthy behaviours (lifestyle modifications). The main objectives of the program were to provide non-threatening information to enable patients to better understand their pain, change any unhelpful beliefs about LBP, promote positive attitudes, and integrate self-management and active coping strategies to deal with psychological issues such as fear-avoidance beliefs, catastrophization, and negative emotions. The educational sessions were delivered to the participants in groups of 3–5 patients. The sessions began with 15–20 min of interactive discussions and questions followed by a 1-hr lecture in the form of verbal communication and visual aids such as slides or prepared diagrams. Several simple cultural metaphors were used in reinforcing some information in the program. The details of the education program are provided in Table 1.
Table 1.
Patient education
| Steps | Topic/focus | Goal | Activity/message delivered |
|---|---|---|---|
| 1st | Interactive session/discussions/questions | To establish a good rapport and relationship To set goals To explore participants beliefs about low back pain (LBP) |
Treatment rationale and expected goals. Accept that you have persistent pain and then begin to move on. Importance of realistic goals setting or action plans. Participants were allowed to tell their story/experience about LBP. Unhelpful beliefs or information obtained in this step were addressed in the subsequent steps. |
| 2nd | Meaning of LBP | To promote understanding of the meaning of LBP | Definition of LBP, nonspecific LBP versus specific LBP, acute versus chronic LBP (CLBP) or persistent. Brief epidemiology of LBP with a focus on Nigeria. Disability related to LBP, burden of LBP and its costs. |
| 3rd | Common facts about CLBP | To understand the common facts/myth about CLBP | LBP is common, not serious due to any disease, settle eventually, reoccurrence is common but still does not mean it is serious. Extended bed rest does not help and may actually prolong pain and leads to more disability. |
| 4th | Common beliefs about LBP | To reshape false or unhelpful beliefs about LBP | Beliefs of having a serious injury, fear of movement due to pain or damage, beliefs about work or physical activity and pain are linked, excessive attention on pain, total bed rest or inactivity, and over-reliance on medications were addressed as unhelpful. Beliefs about LBP and infertility or impotence are linked, and other beliefs learned from participants that are un related to LBP were all addressed as false. False beliefs about pain can prolong pain experience. Avoiding movement and or activity due to fear of pain has negative consequences and can lead to pain persistence and loss of function. Total bed rest leads to stiff joints, weak muscles and bones, and decline physical fitness. Pain medications have doubtful effects and adverse effects on the long-term, unresearched herbal preparations may pose some undesirable health effects. |
| 5th | Basic anatomy | To promote understanding of the back (spine) as one of the strongest structure in the body | The spine is made of solid bony blocks joined by discs to give it strength and flexibility. It is reinforced by strong ligaments and surrounded by large and powerful muscles which protect it. Due to the inherent strength of the spine, it is surprisingly hard to damage it. |
| 6th | Pain causation | To promote better understanding about the cause of pain | Feeling pain does not necessarily mean tissue injury or damage as pain and picture diagnostics (e.g., X-ray) correlates poorly. Scans are more useful for specific LBP such as fractures. In most people, it is difficult to pinpoint the exact source of the problem. Though it is frustrating, it is good news in another way you do not have any serious injury or damage in your spine. Simple back strain does not result in any permanent damage. Permanent serious back injuries are usually caused by high-energy trauma. Most people with LBP do not have any damage in their spine. Many people have disc bulge or degeneration but have no symptoms. Presence of such changes may not be a predictive of future pain. Even though some people with back pain have slipped disc, it usually gets better by its self and very few cases ever require surgery. |
| 7th | Basics of pain physiology | To promote basic knowledge about pain mechanism and common factors influencing it | Meaning of pain. Basic noiciceptive pathways: noiciceptors, spinal cord, and brain. Why do we get pain?: pain as an alarm (warning), meant to protect and motivate to create an action. Pain gate: gate that controls flow of signals (pain messages) between the body and the brain. The gate opens and closes, which defends on many factors related to our beliefs, behaviour, experiences, and expectations. Examples of factors that open the gate include believing that hurt means harm, fear of movement due to pain, catastrophic thought, depression, anxiety, stress, tension, focusing on pain, sadness, and anger. These factors also play a key role in pain chronification. Examples of factors that close the gate include happiness/laughter, distraction from pain with physical activity, exercises/stretching, relaxations/calm, massage and some medications. Since it is the brain that makes us feel pain, knowing the things that cause us feel can help us reduce pain. Since we know what influences our pain, we can understand that pain is not necessarily due to injury or damage in the spine. It can be felt with no changes to the body structure. |
| 8th | Return to normal activities and stay active | To encourage the early return to normal activities and the importance of remaining active despite in pain | Make an early return to normal or vocational activities as tolerated without thinking that activities such as bending are harmful. Since the muscles, ligaments or joints of the spine helps you get moving and most pain are felt from these structures, when you stop moving, these structures stops working properly. To get your back working properly, you must move. It is safe to stay active and the sooner you get active, the sooner your back will feel better. Avoid unaccustomed or extended bed rest when there seems to be serious pain or overdo activities when there seems to be less pain. This is crucial in dealing with an acute attack, getting better faster, and preventing more back trouble. Physical activity even with pain is unlikely to further damage back. |
| 9th | Pain coping and pacing | To promote better active coping through adopting safe and effective pacing during flare-ups | Monitor your symptoms and identify the likely contributing factors to your pain exacerbations or amelioration. Safe pacing (e.g., alternating activity with rest, slowing down when performing tasks), especially during flare-ups, is useful. Modify your activity, adopt positive attitudes and engage in a variety of meaningful activities despite being in pain. Do not let your back take over your life. Performance of more natural spinal movements in less pain is essential to good pacing. Pacing for common activities like peasant farming was discussed. |
| 10th | Self-management | To promote active self-management strategies and reduce over-reliance on formal health care utilization | Effective self-care strategies are important in coping with pain and enhancing recovery. Self-care options including the use of common pain relievers (only prescribed by the physician), heat and cold packs, massage (with topical pain creams), stretching exercises, and relaxation techniques (e.g., listening to music, dancing, watching comedy, attending social events, Swedish relaxation) were advised/taught. Do not rely on single treatment; a combination of approaches will likely have the greatest benefit. |
| 11th | Postural hygiene | To promote healthy postural habit at home or at work as means of reducing the risk of temporary pain episodes | Postural modification is important to reduce risk of temporary pain episodes from physical overload or prolonged static activities. No clear correlation between posture and pain. Postural modifications for common daily tasks/activities such as standing, sitting, bending, and lifting were taught as a means of reducing back muscle tension to ease pain. Special considerations were given to some common practices like peasant farming and heavy manual lifting. For example, the use of modifiable farming tools and other means of carrying goods were advised. |
| 12th | Increasing activity level | To promote the importance of improving activity levels | Gradually increase physical activity levels that are tolerable, comfortable and safe. Moderate physical activities (based on the [ACSM’s] position statement) may include over ground brisk walks, bicycling, vacuuming, washing clothes, and swimming. Plan your days and have some exercise every day. You can try walking or bicycling instead of going by bus, or motor cycle. Regular activity develops muscles, gives stronger bones, release natural chemicals that reduce pain, promote fitness and sense of well-being. Monitor your own functional progress, and do more each day. |
| 13th | Lifestyle modification | To promote a healthy lifestyle and reduce risk of additional problem | Physical inactivity, sedentary lifestyle, obesity, smoking, sleeping less, and stress can have negative direct and indirect impact on your back and overall health. Adopt a healthy lifestyle and always check your health. Have adequate sleep (at least 7 hours per day), reduce or stop smoking, avoids physical and mental stress, and eats healthy food (balanced diet). Also, maintain good social participation. |
| 14th | Warning signs of LBP and what to do | Promote understanding of warning signs (red flags) of LBP and the importance of hospital visit | In case of signs such as weight loss, night sweating like legs weakness, sensory disturbances (pins and needles) around the buttocks, anus, genital area or inner surfaces of the thighs and difficulty in passing or controlling urine/bowel, consult a physician immediately. These symptoms, however, are rare and do not let them worry you. |
| 15th | Review of discussions and applications | To evaluate understanding and application of information/program learned | Previous concepts learned were reviewed. Their application was discussed. Areas of doubt or requiring additional explanations were further discussed. |
ACSM, American College of Sports Medicine.
Motor control exercise
The biological rationale for the MCE is based on the theory that the stability and control of the spine are altered in people with LBP. Hence, the program was designed to enhance the function of specific muscles of the lumbopelvic region and the control of posture and movement (Costa et al., 2009). The MCE protocol used in this study was similar as described in previous publications (Costa et al., 2009; Ibrahim and Akindele, 2018; Rabin et al., 2014). Initially, participants were received brief education on the anatomical location and function of the targeted trunk muscles. The exercise program involved three stages.
The first stage (1st to 3rd sessions) begun with isometric contraction of the local stability muscles (e.g., lumbar multifidus, transversus abdominis) through an abdominal drawing-in maneuver (ADIM) in minimally loading positions (supine lying, quadruped, sitting, and standing) by maintaining a neutral spine while maintaining normal breathing (Rabin et al., 2014). The participants were trained on how to activate the local stability muscles from the global muscles in an individualized manner (Costa et al., 2009). In the second stage (4th to 9th sessions) after the participants must have learned the ADIM, additional loads were placed on the spine through various upper and lower extremities and trunk movement patterns with the aim of recruiting a variety of trunk (local and global) muscles. In the third stage (10th to 12th sessions), functional movement patterns were incorporated into the training program while performing an ADIM and maintaining a neutral lumbar spine (Rabin et al., 2014). Additionally, continued implementation of the specific exercises by regular activation of the local stability muscles, into the performance of activities of daily-life living, especially those that set off pain was emphasized.
During each stage of the MCE program, the recruitment of the trunk muscles, posture, movement pattern, and breathing were assessed and corrected by the treating therapist. Progression of exercises was based on patient’s fatigue, pain thresholds or observed movement control. The MCE program lasted for about 20–30 min per session. Table 2 presents a summarized description of the MCE program.
Table 2.
Motor control exercise
| Stage/progression | Exercise | Intensity |
|---|---|---|
| Stage 1 (1st–3rd sessions) | 1. ADIM in supine | 7 sec hold, 10 reps |
| 2. ADIM in quadruped | ✓ | |
| 3. ADIM in sitting | ✓ | |
| 4. ADIM in standing | ✓ | |
|
| ||
| Stage 2 (4th–9th sessions) | 5. ADIM in supine with heel slide (each leg) | 4 sec hold, 10 reps |
| 6. ADIM in supine with leg lift (each leg) | ✓ | |
| 7. ADIM in supine with bridging (two legs) | 7 sec hold, 10 reps | |
| 8. ADIM in supine with single-leg bridge | ✓ | |
| 9. Supine ADIM with curl-up (elbows on the table) | ✓ | |
| 10. Supine ADIM with curl-up (hands over the forehead) | ✓ | |
| 11. ADIM in horizontal side support with knees bent | ✓ | |
| 12. ADIM in horizontal side support with knees straight | ✓ | |
| 13. Side-lying horizontal side support with ADIM | ✓ | |
| 14. ADIM in quadruped with arm raise | ✓ | |
| 15. ADIM in quadruped with leg raise | ✓ | |
| 16. ADIM in quadruped with alternate arm and leg raise | ✓ | |
|
| ||
| Stage 3 (10th–12th sessions) | 17. Rolling from side to side with ADIM | 10 reps |
| 18. Sit-stand transfer with ADIM | 10 reps | |
| 19. Wall squatting with ADIM | 5 sec hold, 10 reps | |
| 20. Walking with ADIM (10 min) | 7 sec hold, 10s relax, 10 reps | |
ADIM, abdominal drawing-in maneuver.
Stretching exercise
The participants performed active static stretching of muscles and connective tissue around the lumbopelvic-hip region and leg, aiming at increasing mobility and flexibility which are generally considered important in CLBP. The exercises were largely taken from a previous study (Ibrahim and Akindele, 2018). Details of the exercise are presented in Table 3. The stretching sessions lasted for about 20 min per session.
Table 3.
Stretching exercise
| Exercise type | Description | Intensity |
|---|---|---|
| 1. Double knees to chest stretch | In a supine lying position with the knees bend and feet flat on the floor, interlock fingers just under the knees and gently pull towards the chest to the maximum. | 15 sec hold, 5 reps |
| 2. Piriformis stretch | In a supine lying position with the knees bend and feet flat on the floor, the ankle of one leg crossed over the opposite hip crease. Interlock fingers just under the other knee and gently pull towards the chest until a comfortable stretch is felt. Switch sides. | 30 sec hold, 5 reps |
| 3. Hamstring stretch | In a supine position, while keeping knee and hip at 90°–90° position, extends the knee progressively with the foot moving towards the ceiling until a stretch is felt in the posterior aspect of the knee/thigh. Switch sides. | 30 sec hold, 5 reps |
| 4. Trunk rotation | In a supine lying position, cross the right foot over the left knee, using the left hand gently pull the right knee towards the floor while twisting the spine to the right and keeping the right arm and shoulder straight out on the floor. Switch sides. | 15 sec hold, 5 reps |
| 5. Erector spinae stretch | While sitting on the heels, bend the trunk with the abdomen resting on the front of the thighs while stretching arms forward. | 30 sec hold, 5 reps |
| 6. Prone on elbow | In a prone position with the hands under the shoulders, gently push with hands so that shoulders begin to lift off the floor. | 30 sec hold, 5 reps |
| 7. Hip adductor stretch | While sitting up right on the floor with soles of the feet together and the heels closes to the body, gently press down the knees with the hands until a comfortable a stretch is felt in the inner thighs region. | 30 sec hold, 5 reps |
| 8. Triceps surae stretch | In a standing position with both feet at a distance of 2 steps from a wall and both hands on a wall for balance, one leg is stretched in its place while taking a step forward with the other leg. Switch sides. | 30 sec hold, 5 reps |
| 9. Trunk extension stretch | In a standing position with the feet shoulders-width apart, place the hands on the pelvis and slowly bend the back backward as far as possible until a comfortable stretch is felt. | 15 reps |
Aerobic exercise
Aerobic exercise in the form of continuous overground walking at the desirable speed at home for the minimum of 30 min, 5 times per week was advised. This was to encourage aerobic activity and to achieve the recommended moderate-intensity exercise of ≥150 min per week provided by the American College of Sports Medicine (Garber et al., 2011).
Data analysis
All statistical analyses were performed using SPSS ver. 17.0 (SPSS Inc., Chicago, IL, USA). Intention-to-treat analysis was considered with randomized participants included in the originally assigned group. Descriptive statistics were performed to describe the outcomes of feasibility criteria. Normality test for the dependent variables was checked using the Shapiro Wilk test. Because the data had a normal distribution, one-way analysis of variance was used to analyze baseline socio-demographic characteristics and mean values of the outcome measures between the three groups. Paired t-test was conducted to detect the effects of intervention within each group. Post hoc analysis with Turkey test was applied for pairwise comparison of groups. Effect size was computed using partial eta squared (ηp2). A P-value of <0.05 was considered statistically significant.
RESULTS
One hundred seven participants made inquiries about the study at the health care centre following one-day village-wide announcements in January 2018. We were able to assess 62 out of the 107 participants (58%) responded. Individuals (42%) who were not assessed mainly returned to their homes due to business schedule or family commitments. Thirty-nine out of the 62 participants were eligible after screening, representing a recruitment rate of 77% (30 of 39). Only 30 out of the 39 eligible participants were randomized to intervention groups as 7 eligible participants failed to show up on the scheduled day, and 2 had family issues. The flow of participants through each stage is shown in Fig. 1.
Fig. 1.
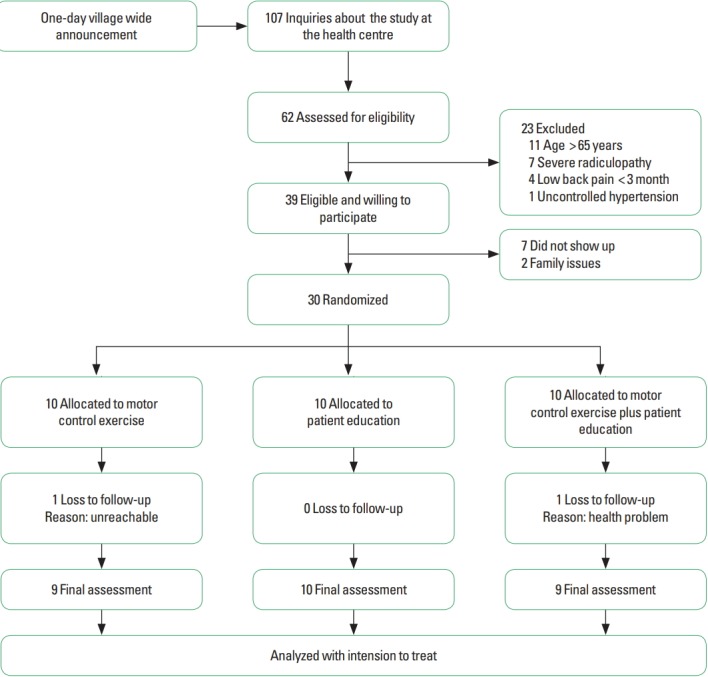
Consort diagram of random allocation of participants into the three groups.
The baseline socio-demographic characteristics of the participants assigned to the three study arms are presented in Table 4. There was no significant difference in the socio-demographic characteristics between the groups. Participants were younger in the MCE group, had a higher number of females, less duration of back pain, and low levels of education. Duration of back pain is slightly higher in the PE group. Majority of the participants in all the three groups were farmers or traders.
Table 4.
Socio-demographic variables of the participants
| Variable | MCE group (n=10) | PE group (n=10) | MCE+PE group (n=10) | P-value |
|---|---|---|---|---|
| Age (yr) | 48.5±14.9 | 50.3±9.09 | 49.9±8.82 | 0.994 |
|
| ||||
| Body mass index (kg/m2) | 22.0±2.92 | 21.5±2.66 | 21.9±3.14 | 0.954 |
|
| ||||
| Pain duration (yr) | 4.23±2.85 | 6.50±5.94 | 5.40±4.76 | 0.884 |
|
| ||||
| Gender | ||||
| Male | 7 (70.0) | 9 (90.0) | 8 (80.0) | 0.197 |
| Female | 3 (30.0) | 1 (10.0) | 2 (20.0) | |
|
| ||||
| Marital status | ||||
| Married | 9 (90.0) | 10 (100) | 10 (100) | 0.596 |
| Single | 1 (10.0) | 0 (0.0) | 0 (0.0) | |
|
| ||||
| Educational status | ||||
| None | 6 (60.0) | 7 (70.0) | 7 (70.0) | |
| Completed primary | 2 (20.0) | 3 (30.0) | 2 (20.0) | 0.956 |
| Completed secondary | 1 (10.0) | 0 (0.0) | 0 (0.0) | |
| Completed tertiary | 1 (10.0) | 0 (0.0) | 1 (10.0) | |
|
| ||||
| Occupational status | ||||
| Paid work (government or private) | 1 (10.0) | 2 (20.0) | 1 (10.0) | 0.796 |
| Self-employed (farming/trading) | 9 (90.0) | 8 (80.0) | 8 (80.0) | |
| Unemployed | 0 (0.0) | 0 (0.0) | 1 (10.0) | |
Values are presented as mean±standard deviation or number (%).
MCE, motor control exercise; PE, patient education.
Treatment compliance to the supervised treatment sessions in the MCE, PE, and MCE plus PE groups were 66% (6 of 9), 80% (8 of 10), and 75% (6 of 8), respectively, while for the home program, 33% (3 of 9), 30% (3 of 10), and 25% (2 of 8), respectively. The retention rate in the MCE, PE, and MCE plus PE groups were 90%, 100%, and 90%, with corresponding lost to follow up of 10%, 0%, and 10%, respectively. Regarding level of perceived helpfulness of intervention, average rating in the MCE, PE, and MCE plus groups were 3.5 (standard deviation [SD], 0.52, range, 3–4), 3.8 (SD, 0.42; range, 3–4), and 3.5 (SD, 0.52; range, 3–4), respectively on the 5-point Likert scale. For overall satisfaction with treatment, average rating in the MCE, PE, and MCE plus PE groups were 3.7 (SD, 0.48; range, 3–4), 3.7 (SD, 0.48; range, 3–4), and 3.8 (SD, 0.42; range, 3–4), respectively. No adverse events were reported during and after the study in all the three groups. During the course of the treatments, one participant in the MCE plus PE group expressed concern about the volume of the program.
Table 5 shows details of changes in clinical outcomes across the three groups. At baseline, no statistically significant difference in pain intensity and functional disability were observed between the three groups. Within-group changes in pain intensity and functional disability were statistically significant among the three groups (P<0.001) after the treatment. There was a statistically significant difference between the three groups for pain intensity (P=0.037, F=3.476) and functional disability (P=0.018, F= 4.967) after the interventions. The MCE plus PE group had a significant reduction in pain intensity with large effect size when compared to the PE group (P=0.028, ηp2=0.22) and in functional disability with large effect size when compared to the MCE group (P=0.018, ηp2=0.26) as indicated by the post hoc analysis. There was no statistically significant difference between the MCE and PE (P=0.326), or MCE plus PE (P=0.420) groups for pain intensity. Similarly, no statistically significant difference was found between the PE and MCE (P=0.766) or MCE plus PE (P=0.083) groups for functional disability.
Table 5.
Comparison of pre and post intervention for pain and functional disability in the intervention groups
| Group | Pain intensity | P-value | Functional disability | P-value | ||||
|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||
| Pretest | Posttest | Difference (95% CI) | Pretest | Posttest | Difference (95% CI) | |||
| MCE+ PE | 6.80±1.31 | 2.20±1.13 | 4.60±1.34 (3.63–5.56) | 0.000** | 34.1±7.68 | 18.2±6.38 | 15.9±8.63 (9.76–22.1) | 0.000* |
|
| ||||||||
| MCE | 6.00±1.41 | 3.00±1.15 | 3.00±1.24 (3.63–5.56) | 0.000** | 37.5±10.4 | 27.4±9.38 | 10.1±9.19 (3.52–16.6) | 0.007* |
|
| ||||||||
| PE | 6.00±1.41 | 3.70±1.33 | 2.30±1.63 (1.12–3.47) | 0.002** | 36.9±10.6 | 25.2±4.23 | 11.7±10.0 (4.58–18.9) | 0.005* |
|
| ||||||||
| F-value | 1.116 | 3.476 | 7.161 | 0.342 | 4.967 | 1.047 | ||
|
| ||||||||
| P-value | 0.342 | 0.037* | 0.003** | 0.713 | 0.018* | 0.365 | ||
Values are presented as mean±standard deviation.
CI, confidence interval; MCE, motor control exercise; PE, patient education.
Significant at *P<0.05, **P<0.01.
DISCUSSION
To the best of our knowledge, this is the first study assessing the benefits of MCE and PE program in a low resource rural Nigerian community. This pilot study demonstrated the feasibility for recruitment, treatment compliance with supervised sessions, safety, acceptability and potential effects of treatment on clinical outcomes. These results suggest the feasibility of conducting a forthcoming full-scale randomized clinical trial in this context.
We found that village-wide announcement was an effective method to recruit potential participants in rural community. Since this is a pilot study, a one-day village-wide announcement was utilized so as to recruit a small number of patients. However, many individuals were willing to participate in the study and came to the health centre in masses. During the eligibility screening, many elderly individuals (>65 years) were excluded largely due to the age criteria set for the study (18–65 years). Very few younger individuals especially males responded to the village-wide announcement which may not guarantee a more representative sample. Nevertheless, our recruitment rate (77%) was high and comparable to the rate (80%) obtained by a previous feasibility study (Igwesi-Chidobe et al., 2016) conducted in another rural community in Nigeria.
The results of this study indicate homogeneity of the study participants as the socio-demographic and clinical variables were balanced between the three groups at baseline. The participants were predominantly males, farmers, and had low levels of education. The fact that the participants were mainly peasant farmers with low literacy rates may partly explain why the consequences of living with LBP may increase in rural Nigeria (Igwesi-Chidobe et al., 2017b; Omokhodion, 2002).
Feasibility of our study was also demonstrated by the excellent treatment compliance (>65%) with the supervised treatment sessions in all the three groups. However, treatment compliance with the prescribed home program was not encouraging (<50%) in all the three groups despite the short duration of the study. The MCE plus PE group had the least compliance in this regard. A possible explanation for the poor compliance with the home program may be due to cultural factors which might have influenced some patients for being reluctant (possibly due to shyness) to perform home exercises especially in the presence of family members. However, the low compliance rate to the home program found this study is not surprising as it occurs in many studies. Patient compliance with physiotherapy advice and exercise generally constitutes a serious problem to physiotherapists in the management of CLBP (Middleton, 2004).
The retention rates found in this study were excellent (90%–100%) as very few participants were lost to follow-up similar to the findings of Igwesi-Chidobe et al. (2016) who found a high retention rate (92%) with a 6-week self-management program for CLBP in similar setting. Our results, however, should be interpreted with caution as the study is small. It is worth noting that our study participants regardless of their group allocation found their treatment very useful and satisfactory as the level of helpfulness were rated from “almost helpful” to “very helpful,” and for overall satisfaction rated from “satisfied” to “very satisfied.” These findings suggest that the interventions were relevant and acceptable.
Although qualitative feedback interview was not conducted in the present study, the participants were given the opportunity to discuss with the research team after completion of the study. Majority of the participants who had received PE admitted that the program was essential for managing their back pain. This is highly relevant to the population due to the lack of effective health care in the community. Patients can be more active in the management of their symptoms using the self-management strategies learned. Additionally, two participants in the MCE group testified that the program was quite interesting as a treatment for CLBP. However, one participant in the MCE plus PE group expressed a concern about the volume of the program. This could be attributed to the fact that the time taken to complete a treatment session in this particular group was relatively long compared to the time taken to complete a treatment session in the MCE or PE alone groups.
Regarding treatment outcomes, all the three groups demonstrated significant within-group improvements in pain intensity implying that the interventions are capable of inducing favourable effects despite the fewer sessions. The MCE plus PE group, however, had significantly better improvements with large effect size when compared to the PE group. Even though, no statistically significant difference was reached between the MCE plus PE group and the MCE group, the mean change in pain intensity after treatment was lower in the combination group. These results were similar to the results obtained by previous studies that combined exercise with cognitive-based education for patients with CLBP (Bodes Pardo et al., 2018; Moseley, 2003).
In terms of functional disability, we also observed substantial within-group improvements with more favourable results for the MCE plus PE group compared to the MCE group. This could be interpreted that the addition of education to exercise conferred more benefits. Our results were analogous to that obtained by Bodes Pardo et al. (2018) who found exercise combined with education to be more effective than exercise alone in reducing disability in patients with CLBP. Though the MCE plus PE group generally had better improvements in the disability scores compared to the rest of the groups, we believe that providing the PE program played an important role in enhancing the function of the patients by providing evidence-based information on LBP and encouraging self-management as well as active coping strategies. A pilot study by Ryan et al. (2010), however, showed that providing education alone appears to be better than exercise classes combined with education in reducing disability. In another trial (Sorensen et al., 2010), a cognitive, educational intervention resulted in at least as good outcomes (e.g., pain, disability, activity limitation) as a symptom-based physical training (exercises) method in patients with CLBP, which is in agreement with the results of our study that shows PE alone may be as good as MCE for pain and disability. Thus, implying that, a carefully designed PE is likely to be more cost-efficient for patients CLBP.
Though a formal, a priori power calculation and hypothesis were not performed in the present study, all the treatment groups showed promising results evidenced by the within-group reduction in pain and disability after the interventions. However, combining MCE with PE resulted in significantly better results with a large effect size compared to using MCE or PE alone. These findings are in line with the general recommendation that advice and education programs should be combined with exercise programs for the effective management of CLBP (May, 2010).
The strengths of this pilot study aside from the feasibility assessments include randomized assignment, blinding of outcome assessors and evaluation of important clinical outcomes (i.e., pain and disability) related to CLBP. A potential limitation of this study was the small sample size hence statistical inferences are not definitive. Additionally, the lack of prior studies on the topic in rural Nigeria has limited the direct comparisons of our results with other studies. Nevertheless, this pilot study demonstrates important preliminary findings for conducting a full-scale trial of MCE and PE in this part of the world.
In response to this study, only a few modifications were made to the full-scale trial protocol. We will involve more communities through multiple village-wide announcements and adverts via local posters. Recruitment rate will be enhanced by relaxing inclusion especially with regard to age criteria. We will facilitate compliance with home program and follow-ups as much as possible by a frequent reminder through phone calls to the participants. Other lessons learned which will inform the full trial include the need for conducting a qualitative interview to gather in-depth information about patients experience with the interventions.
In conclusion, findings of this pilot study suggest that the interventions are promising and conducting a full-scale randomized clinical trial in the future is feasible to confirm the effectiveness of the interventions for the management of CLBP in rural Nigerian community, taking into account the possible arrears of improvements.
ACKNOWLEDGMENTS
The authors wish to acknowledge the effort of Kabiru Umar, the in-charge, Tsakuwa Primary Healthcare Center, Yakubu H. Abdullahi, Ibrahim Muhammad, Shua’ibu M. Gambo, Halima Bukar Tarfa, and Binta Ashiru for research assistance, and all the participants involved in this study.
Footnotes
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.
REFERENCES
- Akodu AK, Akindutire OM. The effect of stabilization exercise on pain-related disability, sleep disturbance, and psychological status of patients with non-specific chronic low back pain. Korean J Pain. 2018;31:199–205. doi: 10.3344/kjp.2018.31.3.199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aliyu FY, Wasiu AA, Bello B. Effects of a combined lumbar stabilization exercise and cognitive behavioural therapy on selected variables of individuals with non-specific low back pain: a randomized clinical trial. Fisioterapia. 2018;40:257–264. [Google Scholar]
- Beaton DE, Bombardier C, Guillemin F, Ferraz MB. Guidelines for the process of cross-cultural adaptation of self-report measures. Spine. 2000;25:3186–3191. doi: 10.1097/00007632-200012150-00014. [DOI] [PubMed] [Google Scholar]
- Bello B, Bello AH. A systematic review on the prevalence of low back pain in Nigeria. Middle East J Rehabil Health Stud. 2017;4:e45262. [Google Scholar]
- Bodes Pardo G, Lluch Girbés E, Roussel NA, Gallego Izquierdo T, Jiménez Penick V, Pecos Martín D. Pain neurophysiology education and therapeutic exercise for patients with chronic low back pain: a single-blind randomized controlled trial. Arch Phys Med Rehabil. 2018;99:338–347. doi: 10.1016/j.apmr.2017.10.016. [DOI] [PubMed] [Google Scholar]
- Brox JI, Storheim K, Grotle M, Tveito TH, Indahl A, Eriksen HR. Systematic review of back schools, brief education, and fear-avoidance training for chronic low back pain. Spine J. 2008;8:948–958. doi: 10.1016/j.spinee.2007.07.389. [DOI] [PubMed] [Google Scholar]
- Burton AK, Waddell G, Tillotson KM, Summerton N. Information and advice to patients with back pain can have a positive effect. A randomized controlled trial of a novel educational booklet in primary care. Spine. 1999;24:2484–2491. doi: 10.1097/00007632-199912010-00010. [DOI] [PubMed] [Google Scholar]
- Byström MG, Rasmussen-Barr E, Johannes W, Grooten A, Grooten WJA. Motor control exercises reduces pain and disability in chronic and recurrent low back pain: a meta-analysis. Spine (Phila Pa 1976) 2013;38:E350–358. doi: 10.1097/BRS.0b013e31828435fb. [DOI] [PubMed] [Google Scholar]
- Chou R, Côté P, Randhawa K, Torres P, Yu H, Nordin M, Hurwitz EL, Haldeman S, Cedraschi C. The Global Spine Care Initiative: applying evidence-based guidelines on the non-invasive management of back and neck pain to low- and middle-income communities. Eur Spine J. 2018 Feb 19; doi: 10.1007/s00586-017-5433-8. [Epub]. [DOI] [PubMed] [Google Scholar]
- Chou R, Qaseem A, Snow V, Casey D, Cross JT, Jr, Shekelle P, Owens DK, Clinical Efficacy Assessment Subcommittee of the American College of Physicians; American College of Physicians; American Pain Society Low Back Pain Guidelines Panel Diagnosis and treatment of low back pain: a joint clinical practice guideline from the American College of Physicians and the American Pain Society. Ann Intern Med. 2007;147:478–491. doi: 10.7326/0003-4819-147-7-200710020-00006. [DOI] [PubMed] [Google Scholar]
- Costa LO, Maher CG, Latimer J, Hodges PW, Herbert RD, Refshauge KM, McAuley JH, Jennings MD. Motor control exercise for chronic low back pain: a randomized placebo-controlled trial. Phys Ther. 2009;89:1275–1286. doi: 10.2522/ptj.20090218. [DOI] [PubMed] [Google Scholar]
- Delitto A, George SZ, Van Dillen LR, Whitman JM, Sowa G, Shekelle P, Denninger TR, Godges JJ, Orthopaedic Section of the American Physical Therapy Association Low back pain. J Orthop Sports Phys Ther. 2012;42:A1–57. doi: 10.2519/jospt.2012.42.4.A1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dupeyron A, Ribinik P, Gélis A, Genty M, Claus D, Hérisson C, Coudeyre E. Education in the management of low back pain: literature review and recall of key recommendations for practice. Ann Phys Rehabil Med. 2011;54:319–335. doi: 10.1016/j.rehab.2011.06.001. [DOI] [PubMed] [Google Scholar]
- Ferreira-Valente MA, Pais-Ribeiro JL, Jensen MP. Validity of four pain intensity rating scales. Pain. 2011;152:2399–2404. doi: 10.1016/j.pain.2011.07.005. [DOI] [PubMed] [Google Scholar]
- Ganiyu SO, Gujba KF. Effects of acupuncture, core-stability exercises, and treadmill walking exercises in treating a patient with postsurgical lumbar disc herniation: a clinical case report. J Acupunct Meridian Stud. 2015;8:48–52. doi: 10.1016/j.jams.2014.08.002. [DOI] [PubMed] [Google Scholar]
- Garber CE, Blissmer B, Deschenes MR, Franklin BA, Lamonte MJ, Lee IM, Nieman DC, Swain DP, American College of Sports Medicine. American College of Sports Medicine position stand Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: guidance for prescribing exercise. Med Sci Sports Exerc. 2011;43:1334–1359. doi: 10.1249/MSS.0b013e318213fefb. [DOI] [PubMed] [Google Scholar]
- Gomes-Neto M, Lopes JM, Conceição CS, Araujo A, Brasileiro A, Sousa C, Carvalho VO, Arcanjo FL. Stabilization exercise compared to general exercises or manual therapy for the management of low back pain: a systematic review and meta-analysis. Phys Ther Sport. 2017;23:136–142. doi: 10.1016/j.ptsp.2016.08.004. [DOI] [PubMed] [Google Scholar]
- Hayden JA, van Tulder MW, Tomlinson G. Systematic review: strategies for using exercise therapy to improve outcomes in chronic low back pain. Ann Intern Med. 2005;142:776–785. doi: 10.7326/0003-4819-142-9-200505030-00014. [DOI] [PubMed] [Google Scholar]
- Henrotin YE, Cedraschi C, Duplan B, Bazin T, Duquesnoy B. Information and low back pain management: a systematic review. Spine (Phila Pa 1976) 2006;31:E326–334. doi: 10.1097/01.brs.0000217620.85893.32. [DOI] [PubMed] [Google Scholar]
- Hondras M, Hartvigsen J, Myburgh C, Johannessen H. Everyday burden of musculoskeletal conditions among villagers in rural Botswana: a focused ethnography. J Rehabil Med. 2016;48:449–455. doi: 10.2340/16501977-2083. [DOI] [PubMed] [Google Scholar]
- Hoy D, Brooks P, Blyth F, Buchbinder R. The epidemiology of low back pain. Best Pract Res Clin Rheumatol. 2010;24:769–781. doi: 10.1016/j.berh.2010.10.002. [DOI] [PubMed] [Google Scholar]
- Hoy D, March L, Brooks P, Blyth F, Woolf A, Bain C, Williams G, Smith E, Vos T, Barendregt J, Murray C, Burstein R, Buchbinder R. The global burden of low back pain: estimates from the Global Burden of Disease 2010 study. Ann Rheum Dis. 2014;73:968–974. doi: 10.1136/annrheumdis-2013-204428. [DOI] [PubMed] [Google Scholar]
- Ibrahim AA, Akindele MO. Combined effects of postural education, therapeutic massage, segmental sretching, and motor control exercise in a 19-year-old male with chronic back pain and kypholordotic posture: a case report. Middle East J Rehabil Health Stud. 2018;5:e74186. [Google Scholar]
- Igwesi-Chidobe C. Obstacles to obtaining optimal physiotherapy services in a rural community in southeastern Nigeria. Rehabil Res Pract. 2012;2012a doi: 10.1155/2012/909675. 909675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Igwesi-Chidobe CN, Coker B, Onwasigwe CN, Sorinola IO, Godfrey EL. Biopsychosocial factors associated with chronic low back pain disability in rural Nigeria: a population-based cross-sectional study. BMJ Glob Health. 2017a;2:e000284. doi: 10.1136/bmjgh-2017-000284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Igwesi-Chidobe CN, Kitchen S, Godfrey E, Sorinola I. Feasibility of a physiotherapist-led community-based self-management programme for reducing non-specific chronic low back pain disability in rural Nigeria. Physiotherapy. 2016;102(Suppl 1):e61. [Google Scholar]
- Igwesi-Chidobe CN, Kitchen S, Sorinola IO, Godfrey E. Qualitative exploration of non-specific chronic low back pain in rural Nigeria: towards evidence-informed physiotherapy practice. Physiotherapy. 2015;101:e636–637. [Google Scholar]
- Igwesi-Chidobe CN, Kitchen S, Sorinola IO, Godfrey EL. “A life of living death”: the experiences of people living with chronic low back pain in rural Nigeria. Disabil Rehabil. 2017b;39:779–790. doi: 10.3109/09638288.2016.1161844. [DOI] [PubMed] [Google Scholar]
- Igwesi-Chidobe CN, Odebiyi DO, Okafor UA. Characterisation of physiotherapy needs in a rural community in South Eastern Nigeria. Nig Q J Hosp Med. 2012b;22:168–176. [PubMed] [Google Scholar]
- Johnson OE, Adegoke BO, Ogunlade SO. Comparison of four physiotherapy regimens in the treatment of long-term mechanical low back pain. J Jpn Phys Ther Assoc. 2010;13:9–16. doi: 10.1298/jjpta.13.9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Louw QA, Morris LD, Grimmer-Somers K. The prevalence of low back pain in Africa: a systematic review. BMC Musculoskelet Disord. 2007;8:105. doi: 10.1186/1471-2474-8-105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- May S. Self-management of chronic low back pain and osteoarthritis. Nat Rev Rheumatol. 2010;6:199–209. doi: 10.1038/nrrheum.2010.26. [DOI] [PubMed] [Google Scholar]
- Mbada CE, Ayanniyi O, Ogunlade SO. Comparative efficacy of three active treatment modules on psychosocial variables in patients with long-term mechanical low-back pain: a randomized-controlled trial. Arch Physiother. 2015;5:10. doi: 10.1186/s40945-015-0010-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Middleton A. Chronic low back pain: patient compliance with physiotherapy advice and exercise, perceived barriers and motivation. Phys Ther Rev. 2004;9:153–160. [Google Scholar]
- Moore P, Cole F. The Pain Toolkit [Internet] The Pain Toolkit. 2009 [cited 2017 Oct 25]. Available from: http://www.paintoolkit.org/
- Moseley GL. Joining forces–combining cognition-targeted motor control training with group or individual pain physiology education: a successful treatment for chronic low back pain. J Man Manip Ther. 2003;11:88–94. [Google Scholar]
- Odebiyi DO, Akinpelu OA, Alonge TO, Adegoke BO. Back school: the development of a Nigerian urban model. Nig Q J Hosp Med. 2009;19:135–141. doi: 10.4314/nqjhm.v19i3.54489. [DOI] [PubMed] [Google Scholar]
- Ojoawo AO, Hassan MA, Olaogun MOB, Johnson EO, Mbada CE. Comparative effectiveness of two stabilization exercise positions on pain and functional disability of patients with low back pain. J Exerc Rehabil. 2017;13:363–371. doi: 10.12965//jer.1734932.466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Omokhodion FO. Low back pain in a rural community in South West Nigeria. West Afr J Med. 2002;21:87–90. [PubMed] [Google Scholar]
- Omokhodion FO. Low back pain in an urban population in Southwest Nigeria. Trop Doct. 2004;34:17–20. doi: 10.1177/004947550403400107. [DOI] [PubMed] [Google Scholar]
- Rabin A, Shashua A, Pizem K, Dickstein R, Dar G. A clinical prediction rule to identify patients with low back pain who are likely to experience short-term success following lumbar stabilization exercises: a randomized controlled validation study. J Orthop Sports Phys Ther. 2014;44:6–B13. doi: 10.2519/jospt.2014.4888. [DOI] [PubMed] [Google Scholar]
- Ramond A, Bouton C, Richard I, Roquelaure Y, Baufreton C, Legrand E, Huez JF. Psychosocial risk factors for chronic low back pain in primary care: a systematic review. Fam Pract. 2011;28:12–21. doi: 10.1093/fampra/cmq072. [DOI] [PubMed] [Google Scholar]
- Ryan CG, Gray HG, Newton M, Granat MH. Pain biology education and exercise classes compared to pain biology education alone for individuals with chronic low back pain: a pilot randomised controlled trial. Man Ther. 2010;15:382–387. doi: 10.1016/j.math.2010.03.003. [DOI] [PubMed] [Google Scholar]
- Sokunbi G, Gambo HB, Blasu C. Effects of group-based versus individual-based spinal stability exercises (SSE) on physical health and mental wellbeing of patients with chronic low back pain (LBP): a randomized controlled trial (RCT) J Pain Relief. 2015;4:203. [Google Scholar]
- Sorensen PH, Bendix T, Manniche C, Korsholm L, Lemvigh D, Indahl A. An educational approach based on a non-injury model compared with individual symptom-based physical training in chronic LBP. A pragmatic, randomised trial with a one-year follow-up. BMC Musculoskelet Disord. 2010;11:212. doi: 10.1186/1471-2474-11-212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tella BA, Akinbo SR, Asafa SA, Gbiri CA. Prevalence and impacts of low back pain among peasant farmers in south-west Nigeria. Int J Occup Med Environ Health. 2013;26:621–627. doi: 10.2478/s13382-013-0135-x. [DOI] [PubMed] [Google Scholar]
- Thabane L, Ma J, Chu R, Cheng J, Ismaila A, Rios LP, Robson R, Thabane M, Giangregorio L, Goldsmith CH. A tutorial on pilot studies: the what, why and how. BMC Med Res Methodol. 2010;6:1. doi: 10.1186/1471-2288-10-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Middelkoop M, Rubinstein SM, Verhagen AP, Ostelo RW, Koes BW, van Tulder MW. Exercise therapy for chronic nonspecific low-back pain. Best Pract Res Clin Rheumatol. 2010;24:193–204. doi: 10.1016/j.berh.2010.01.002. [DOI] [PubMed] [Google Scholar]
- Waddell G, Newton M, Henderson I, Somerville D, Main CJ. A Fear-Avoidance Beliefs Questionnaire (FABQ) and the role of fear-avoidance beliefs in chronic low back pain and disability. Pain. 1993;52:157–168. doi: 10.1016/0304-3959(93)90127-B. [DOI] [PubMed] [Google Scholar]
- Wong JJ, Côté P, Sutton DA, Randhawa K, Yu H, Varatharajan S, Goldgrub R, Nordin M, Gross DP, Shearer HM, Carroll LJ, Stern PJ, Ameis A, Southerst D, Mior S, Stupar M, Varatharajan T, Taylor-Vaisey A. Clinical practice guidelines for the noninvasive management of low back pain: a systematic review by the Ontario Protocol for Traffic Injury Management (OPTIMa) Collaboration. Eur J Pain. 2017;21:201–216. doi: 10.1002/ejp.931. [DOI] [PubMed] [Google Scholar]
- Wood L, Hendrick P, Quraishi N. A systematic review of pain and disability outcomes of pain neuroscience education (PNE) in the management of chronic low back pain. Spine J. 2016;16(4 Suppl):S51. [Google Scholar]


