Abstract
Background
Readmission after ST‐segment–elevation myocardial infarction (STEMI) poses an enormous economic burden to the US healthcare system. Efforts to prevent readmissions should be based on understanding the timing and causes of these readmissions. This study aimed to investigate contemporary causes, timing, and cost of 30‐day readmissions after STEMI.
Methods and Results
All STEMI hospitalizations were selected in the Nationwide Readmissions Database (NRD) from 2010 to 2014. The 30‐day readmission rate as well as the primary cause and cost of readmission were examined. Multivariate regression analysis was performed to identify the predictors of 30‐day readmission and increased cumulative cost. From 2010 to 2014, the 30‐day readmission rate after STEMI was 12.3%. Within 7 days of discharge, 43.9% were readmitted, and 67.3% were readmitted within 14 days. The annual rate of 30‐day readmission decreased by 19% from 2010 to 2014 (P<0.001). Female sex, AIDS, anemia, chronic kidney disease, collagen vascular disease, diabetes mellitus, hypertension, pulmonary hypertension, congestive heart failure, atrial fibrillation, and increased length of stay were independent predictors of 30‐day readmission. A large proportion of patients (41.6%) were readmitted for noncardiac reasons. After multivariate adjustment, 30‐day readmission was associated with a 47.9% increase in cumulative cost (P<0.001).
Conclusions
Two thirds of patients were readmitted within the first 14 days after STEMI, and a large proportion of patients were readmitted for noncardiac reasons. Thirty‐day readmission was associated with an ≈50% increase in cumulative hospitalization costs. These findings highlight the importance of closer surveillance of both cardiac and general medical conditions in the first several weeks after STEMI discharge.
Keywords: causes, cost, readmission, ST‐segment elevation myocardial infarction
Subject Categories: Quality and Outcomes, Cardiovascular Disease, Percutaneous Coronary Intervention
Clinical Perspective
What is New?
Thirty‐day readmission rates after ST‐segment–elevation myocardial infarction have declined in recent years.
Nearly two thirds of patients were readmitted early, within the first 14 days after discharge.
A large proportion of patients were readmitted within 30 or 90 days for noncardiac reasons, particularly after coronary artery bypass grafting.
Thirty‐day readmission was associated with an ≈50% increase in the cumulative hospitalization cost.
What Are the Clinical Implications?
These data suggest that early readmissions could be prevented by closer surveillance and attention to both cardiac and general medical conditions before and within the early discharge period.
Further research is warranted to examine strategies to prevent 30‐day readmissions after ST‐segment–elevation myocardial infarction and to examine whether short‐term readmissions after ST‐segment–elevation myocardial infarction should serve as a quality metric of hospital performance and better outcomes.
Introduction
Recent advances in the treatment of ST‐segment–elevation myocardial infarction (STEMI) have resulted in improved outcomes over the past 2 decades.1, 2 However, STEMI remains a significant cause of morbidity and mortality in the United States. It is estimated that nearly $12.1 billion US dollars were spent in 2013 for hospital care of STEMI.3, 4 Despite efforts to provide prompt revascularization and optimal medical therapy for those presenting with STEMI, ≈20% of patients were readmitted within 30 days of hospitalization in earlier studies.5 Not surprisingly, 30‐day readmission is an enormous economic burden to the US healthcare system and impacts patient quality of life. Significant efforts have been spent on identifying factors associated with 30‐day readmissions.6
The Medicare Payment Advisory Commission has identified acute myocardial infarction as one of the 7 conditions that frequently result in costly readmission, and the Centers for Medicare & Medicaid Services have tried to address this issue through the Hospital Readmission Reduction Program.7 In July 2009, the Centers for Medicare & Medicaid Services began reporting 30‐day readmission for 3 common medical conditions, one of which was acute myocardial infarction.8 These measures have become part of a federal strategy to provide incentives to improve quality of care by reducing preventable readmissions.9 However, to achieve this goal, further understanding of the timing, underlying causes and cost of readmission is needed. Although value‐based medical care is becoming of greater emphasis and a measure of hospital performance, modifiable causes of readmissions remain elusive for the majority of these conditions. Identifying common and preventable etiologies of 30‐day all‐cause readmissions would allow institutions to focus already limited resources and prevent unnecessary readmissions. Using the National Readmission Database (NRD), we aimed to investigate contemporary causes, timing, and cost of 30‐day readmissions after STEMI from 2010 to 2014. The impact of percutaneous coronary intervention (PCI), coronary artery bypass grafting (CABG), or medical therapy (no revascularization) during the index STEMI admission on 30‐day readmissions was also examined.
Methods
Data Source and Study Population
The authors declare that all supporting data are available within the article and its online supplementary files. Data were obtained from the Agency for Healthcare Research and Quality, which administers the Healthcare Cost and Utilization Project. We used the NRD from 2010 to 2014. The NRD is an annual database constructed using 1 calendar year of discharge data and is drawn from the Healthcare Cost and Utilization Project State Inpatient Databases, with verified patient linkage numbers used to track the patients across hospitals within a state during a given year.10 The NRD is designed to support national readmission analyses and is a publicly available nationally representative healthcare database. In the year 2014, the NRD contained deidentified information for 14 894 613 discharges from 2048 hospitals in 22 states, representing 35 306 427 discharges. Each patient record in the NRD contains information on the patient's diagnoses and procedures performed during the hospitalization based on International Classification of Diseases, Ninth Revision–Clinical Modification (ICD‐9‐CM) codes as well as Clinical Classification Software (CCS) codes that groups multiple ICD‐9‐CM codes for facilitated statistical analyses. We identified study population, comorbidities, causes of readmissions and in‐hospital outcomes using a combination of ICD‐9‐CM codes and Clinical Classification Software codes. Institutional Review Board approval and informed consent were not required for current study because all data collection was derived from a deidentified administrative database.
Study Population and Variables
From 2010 to 2014, all hospitalizations for STEMI were selected by searching for ICD‐9‐CM codes for initial STEMI 410.x1 (n=303 127 representing 709 548 patients). Hospitalizations with ICD‐9 codes 410.7x (subendocardial MI) were excluded from analysis. ICD‐9‐CM procedure codes were used to identify patients who underwent lysis (99.10 and V45.88), PCI (00.66, 36.01, 36.02, 36.05, 36.06, and 36.07) or CABG (36.1x). Patients with a concomitant diagnosis of cardiogenic shock and cardiac arrest were identified using ICD‐9‐CM codes 785.51 and 427.5, respectively. Concurrent use of intra‐aortic balloon pump and percutaneous left ventricular support devices were identified with ICD‐9‐CM procedure codes 37.61 and 37.68, respectively. Patients discharged from January through November were included in the study to allow for completeness of data on 30 days of follow‐up after discharge. After analyzing the in‐hospital mortality rates stratified by revascularization method, we excluded patients who died during the index hospitalization. Furthermore, patients with missing data on length of hospital stay were excluded to properly capture interval until readmission. Patients discharged between October and December were additionally excluded during the analysis of 90‐day readmission.
Patient‐ and hospital‐level variables were included as baseline characteristics. NRD variables were used to identify age; sex; median household income quartiles; primary payer; and hospital teaching status, location, and bed size. The overall severity of comorbidities was defined by using the Elixhauser comorbidity score.11 Length of hospital stay was stratified to ≤3 days, 4 to 5 days, and ≥6 days.
Study End Points
The primary outcome of interest was 30‐day all‐cause readmission rate according to the methodology described by the Healthcare Cost and Utilization Project.12 Time to readmission was computed as the number of days from discharge date of index admission to readmission date. Only the first readmission within 30 days after discharge was included, and transfer to another hospital was not counted as a readmission. The primary cause of 30‐day readmission was identified based on Clinical Classification Software code in the first diagnosis field of each readmission record and dichotomized into noncardiac and cardiac causes.12 Noncardiac causes included respiratory, infectious, gastrointestinal, neuropsychiatric/substance, stroke/transient ischemic attack, endocrine/metabolic, genitourinary, hematologic/oncologic, peripheral vascular disease, trauma, complication of medical procedure, and other noncardiac causes. Cardiac causes included angina and chronic ischemic heart disease, heart failure, acute myocardial infarction, nonspecific chest pain, arrhythmia, and other cardiac causes. Furthermore, we identified most common diagnoses of 30‐day readmission using ICD‐9‐CM codes in the primary diagnosis field.13 Exploratory analysis was performed to identify the causes of 90‐day readmissions.
Statistical Analysis
All analyses were performed using SAS software, version 9.4 (SAS Institute, Cary, NC). Discharge weight provided by NRD was used for all analyses to obtain national estimates.10 Domain analysis was used for accurate variance calculations for subgroup analyses. All analyses accounted for hospital‐level clustering of patients and complex survey sampling design. For descriptive analyses, we compared baseline patient and hospital characteristics of patients with STEMI stratified by the occurrence of 30‐day readmission. Categorical variables are shown as frequencies, and continuous variables are presented as mean or median. For comparison, the Rao‐Scott χ2 test was used for categorical variables and either the Mann‐Whitney‐Wilcoxon nonparametric test or survey‐specific linear regression was used for continuous variables. To identify predictors of 30‐day readmission following discharge with STEMI, we created a multivariate Cox proportional hazards regression model for the outcome of 30‐day readmission by including covariates that had univariate significance with the outcome (P<0.1). For the cost analysis, the estimated cost for each hospitalization was calculated by merging NRD data with cost‐to‐charge ratio files provided by the Healthcare Cost and Utilization Project and then multiplying the charge for each hospitalization with the respective cost‐to‐charge ratio. Cumulative cost was defined as the cost of readmission plus the cost of the index admission. Cumulative cost for patients who did not experience readmission is equivalent to their cost of the index admission. Afterward, we examined the predictors of cumulative cost by performing survey‐specific multivariate linear regression and log‐transforming costs to achieve a normal distribution, as previously described.14 All tests were 2‐sided, with P<0.05 indicating statistical significance.
Results
Study Population and Trends of 30‐Day Readmission After STEMI
For each year from 2010 to 2014, the NRD data set included discharges from 1809 hospitals in 2010 to 2048 hospitals in 2014. Of 181 545 078 discharge records reviewed from 2010 to 2014, 709 548 patients presented with STEMI, resulting in in‐hospital mortality of 8.7% (95% confidence interval [CI], 8.6–8.8), 4.6% (95% CI, 4.5–4.7), 5.4% (95% CI, 5.2–5.7) and 25.1% (95% CI, 24.9–25.3) for overall cohort, PCI cohort, CABG cohort, and no revascularization cohort, respectively (P<0.001). Among those who survived the index admission with STEMI, 12.3% were readmitted within 30 days of discharge (Table 1). Specifically, 30‐day readmission rates were 11.1% (95% CI, 11.0–11.1), 14.9% (95% CI, 14.5–15.3) and 17.6% (95% CI, 17.4–17.9) for PCI cohort, CABG cohort, and no revascularization cohort, respectively. Of the total cohort, 17.8% of patients were readmitted more than once during the 30‐day period. During index hospitalizations for STEMI, 78.5% and 4.8% of patients underwent PCI and CABG, respectively, while 16.0% patients were medically treated (without revascularization). The median length of stay during the index hospitalization was 2.5 days (interquartile range [IQR], 1.6–4.4 days), 2.3 days (IQR, 1.5–3.6), 8.7 days (IQR, 6.2–13.1) and 3.0 days (IQR, 1.6–5.5) for the overall cohort, PCI cohort, CABG cohort, and no revascularization cohort, respectively (P<0.001).
Table 1.
Baseline Individual‐ and Hospital‐Level Characteristics for Patients Discharged Alive After Index Hospitalization With STEMI, 2010 to 2014
| Characteristics | Overall | 30‐Day Readmissiona | P Valueb | |
|---|---|---|---|---|
| No | Yes | |||
| Number of admissions | 709 548 | 622 134 (87.7) | 87 415 (12.3) | |
| Patient characteristics | ||||
| Age, mean (SE), y | 62.9 (0.1) | 62.4 (0.1) | 66.5 (0.1) | <0.001c |
| Age group, y | ||||
| <50 | 116 388 (16.4) | 105 717 (17.0) | 10 671 (12.2) | <0.001 |
| 50–64 | 122 866 (40.6) | 259 898 (41.8) | 28 234 (32.3) | |
| ≥65 | 305 028 (43.0) | 256 519 (41.2) | 48 509 (55.5) | |
| Female sex | 219 944 (31.0) | 185 441 (29.8) | 34 503 (39.5) | <0.001 |
| Smoking | 329 688 (46.5) | 293 514 (47.2) | 36 174 (41.4) | <0.001 |
| Hypertension | 461 566 (65.1) | 400 493 (64.4) | 61 073 (69.9) | <0.001 |
| Diabetes mellitus | 200 437 (28.2) | 169 009 (27.2) | 31 428 (36.0) | <0.001 |
| Dyslipidemia | 447 650 (63.1) | 395 267 (63.5) | 52 383 (59.9) | <0.001 |
| Known coronary artery disease | 602 522 (84.9) | 529 546 (85.1) | 72 976 (83.5) | <0.001 |
| Previous myocardial infarction | 59 615 (8.4) | 51 207 (8.2) | 8408 (9.6) | <0.001 |
| Previous PCI | 85 965 (12.1) | 74 762 (12.0) | 11 203 (12.8) | <0.001 |
| Previous CABG | 24 968 (3.5) | 20 986 (3.4) | 3982 (4.6) | <0.001 |
| Family history of coronary artery disease | 83 557 (11.8) | 75 771 (12.2) | 7786 (8.9) | <0.001 |
| History of CHF | 139 035 (19.6) | 110 408 (17.7) | 28 627 (32.7) | <0.001 |
| Peripheral vascular disease | 41 121 (5.8) | 33 318 (5.4) | 7803 (8.9) | <0.001 |
| Pulmonary hypertension | 15 542 (2.2) | 12 141 (2.0) | 3402 (3.9) | <0.001 |
| Chronic pulmonary disease | 80 588 (11.4) | 66 217 (10.6) | 14 372 (16.4) | <0.001 |
| Chronic kidney disease | 68 870 (9.7) | 53 443 (8.6) | 15 427 (17.6) | <0.001 |
| Liver disease | 7626 (1.1) | 6354 (1.0) | 1272 (1.5) | <0.001 |
| Anemia | 75 789 (10.7) | 60 060 (9.7) | 15 729 (18.0) | <0.001 |
| Atrial fibrillation | 83 800 (11.8) | 67 708 (10.9) | 16 092 (18.4) | <0.001 |
| Coagulopathy | 28 363 (4.0) | 23 477 (3.8) | 4887 (5.6) | <0.001 |
| AIDS | 1008 (0.1) | 828 (0.1) | 180 (0.2) | 0.002 |
| Collagen vascular disease | 14 629 (2.1) | 12 224 (2.0) | 2406 (2.8) | <0.001 |
| Drug abuse | 19 880 (2.8) | 17 277 (2.8) | 2604 (3.0) | 0.050 |
| Fluid/electrolyte disorders | 113 392 (16.0) | 93 036 (15.0) | 20 356 (23.3) | <0.001 |
| Obesity | 96 047 (13.5) | 84 428 (13.6) | 11 619 (13.3) | 0.235 |
| Other neurological disorders | 30 540 (4.3) | 25 273 (4.1) | 5267 (6.0) | <0.001 |
| Pulmonary circulation disorders | 642 (0.1) | 477 (0.1) | 165 (0.2) | <0.001 |
| Valvular heart disease | 1325 (0.2) | 1025 (0.2) | 300 (0.3) | <0.001 |
| Elixhauser comorbidity scores >4 | 145 051 (20.4) | 114 620 (18.4) | 30 432 (34.8) | <0.001 |
| Median household income | ||||
| First quartile | 220 748 (31.1) | 191 497 (30.8) | 29 251 (33.5) | <0.001 |
| Second quartile | 185 618 (26.2) | 162 855 (26.2) | 22 763 (26.0) | |
| Third quartile | 167 067 (23.5) | 147 394 (23.7) | 19 673 (22.5) | |
| Fourth quartile | 136 116 (19.2) | 120 388 (19.3) | 15 728 (18.0) | |
| Primary payer | ||||
| Medicare | 315 231 (44.4) | 264 153 (42.5) | 51 078 (58.4) | <0.001 |
| Medicaid | 52 020 (7.3) | 44 309 (7.1) | 7711 (8.8) | |
| Private including HMO | 241 624 (34.1) | 221 703 (35.6) | 19 922 (22.8) | |
| Self‐pay/no charge/other | 100 673 (14.2) | 91 970 (14.8) | 8703 (10.0) | |
| Index STEMI Presentation/Treatment | ||||
| Weekend admission | 199 681 (28.1) | 175 654 (28.2) | 24 026 (27.5) | 0.013 |
| Cardiogenic shock | 52 769 (7.4) | 42 734 (6.9) | 10 034 (11.5) | <0.001 |
| Cardiac arrest | 27 506 (3.9) | 23 368 (3.8) | 4138 (4.7) | <0.001 |
| Revascularization | ||||
| Thrombolytic therapy only | 3748 (0.5) | 3191 (0.5) | 557 (0.6) | <0.001 |
| All PCI | 556 825 (78.5) | 495 238 (79.6) | 61 587 (70.5) | |
| CABG only | 33 744 (4.8) | 28 723 (4.6) | 5022 (5.7) | |
| No revascularization | 113 642 (16.0) | 93 594 (15.0) | 20 048 (22.9) | |
| IABP | 52 471 (7.4) | 42 932 (6.9) | 9539 (10.9) | <0.001 |
| PLVAD | 1903 (0.3) | 1558 (0.3) | 345 (0.4) | <0.001 |
| Hospital characteristics | ||||
| Hospital teaching status | ||||
| Teaching | 368 248 (51.9) | 323 791 (52.0) | 44 457 (50.9) | 0.003 |
| Nonteaching | 341 301 (48.1) | 298 343 (48.0) | 42 958 (49.1) | |
| Hospital location | ||||
| Rural | 370 365 (52.2) | 326 957 (52.6) | 43 409 (49.7) | <0.001 |
| Urban | 339 183 (47.8) | 295 177 (47.4) | 44 006 (50.3) | |
| Hospital bed size | ||||
| Small | 57 054 (8.0) | 49 979 (8.0) | 7076 (8.1) | 0.966 |
| Medium | 156 249 (22.0) | 137 026 (22.0) | 19 222 (22.0) | |
| Large | 496 246 (69.9) | 435 129 (69.9) | 61 117 (69.9) | |
| Length of hospital stay, median (IQR), d | 2.5 (1.6–4.4) | 2.4 (1.5–4.0) | 3.5 (2.0–6.7) | <0.001d |
| Length of hospital stay, d | ||||
| ≤3 | 436 810 (61.6) | 398 204 (64.0) | 38 606 (44.2) | <0.001 |
| 4–5 | 124 906 (17.6) | 106 385 (17.1) | 18 521 (21.2) | |
| ≥6 | 147 832 (20.8) | 117 545 (18.9) | 30 288 (34.6) | |
| Disposition | ||||
| Home | 631 738 (89.0) | 561 403 (90.2) | 70 335 (80.5) | <0.001 |
| Facilitye | 71 660 (10.1) | 55 792 (9.0) | 15 868 (18.1) | |
| AMA/unknown | 6150 (0.9) | 4938 (0.8) | 1211 (1.4) | |
| Charge, median (IQR), $ | 63 363 (43 321–97 520) | 62 661 (43 189–95 453) | 69 679 (44 449–114 471) | <0.001d |
| Cost, median (IQR), $ | 18 316 (13 504–26 023) | 18 169 (13 498–25 548) | 19 515 (13 565–30 049) | <0.001d |
AMA indicates against medical advice; CABG, coronary artery bypass graft; CHF, congestive heart failure; HMO, health maintenance organization; IABP, intra‐aortic balloon pump; IQR, interquartile range; PCI, percutaneous coronary intervention; PLVAD, percutaneous left ventricular assist device; SE, standard error; STEMI, ST‐segment–elevation myocardial infarction.
Values are presented as number (percentage) of patients unless otherwise indicated.
Rao‐Scott χ2 test was used for all statistical tests in Table 1 unless stated otherwise.
Survey‐specific linear regression was performed.
Mann‐Whitney‐Wilcoxon test was used.
Facility includes skilled nursing facility, intermediate care facility, and inpatient rehabilitation facility.
The annual rate of 30‐day readmission (Figure 1) decreased by 19% from 135 449 readmissions per million adults per year (13.5%) in 2010 to 108 526 readmission per million adults per year (10.9%) in 2014 (P<0.001). There was a 14% decrease in the annual rate of 30‐day readmission in the unrevascularized cohort, from 185 050 per million adults per year (18.5%) in 2010 to 159 194 per million adults per year (15.9%) in 2014 (P<0.001). Furthermore, the 30‐day readmission rate decreased by 20% for patients who underwent PCI for STEMI, from 122 625 per million adults per year (12.3%) in 2010 to 97 866 per million adults per year (9.8%) in 2014 (P<0.001). In contrast, the 30‐day readmission rate did not change over time for those who underwent CABG after presenting with STEMI. The median length of stay during the readmission was 2.6 days (IQR, 1.1–5.2), with in‐hospital mortality of 4.6% (95% CI, 4.4–4.7) for the overall cohort. The median length of stay was 2.3 days (IQR, 1.0–4.7), 3.8 days (IQR, 1.8–7.4) and 3.4 days (IQR, 1.7–6.2) for PCI cohort, CABG cohort, and no revascularization cohort, respectively (P<0.001). Furthermore, in‐hospital mortality during the readmission was 3.2% (95% CI, 3.1–3.4), 3.8% (95% CI, 3.3–4.4) and 8.8% (95% CI, 8.4–9.2) for PCI cohort, CABG cohort, and no revascularization cohort, respectively (P<0.001).
Figure 1.
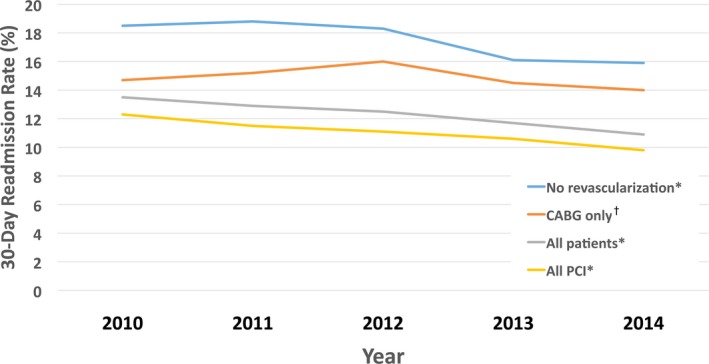
Temporal trends of 30‐day readmission rates after index admission for STEMI (ST‐segment–elevation myocardial infarction). * P for trend <0.001. † P for trend=0.472. CABG indicates coronary artery bypass graft; PCI, percutaneous coronary intervention.
Table 1 compares baseline characteristics for overall cohort as well as groups stratified by 30‐day readmission. Patients readmitted within the 30 days were older and more likely to be female and have hypertension, diabetes mellitus, previous myocardial infarction, previous coronary revascularization, congestive heart failure, peripheral vascular disease, chronic obstructive pulmonary disease, pulmonary hypertension, and chronic kidney disease. In addition, 34.8% of readmitted patients had an Elixhauser comorbidity score >4 versus 18.4% in the nonreadmitted cohort. Patients who presented with either cardiogenic shock or cardiac arrest or those who were not revascularized during the initial admission with STEMI were more likely to be readmitted within 30 days. Furthermore, 30‐day readmission was more frequent with >3 days of hospital stay during the index hospitalization, and particularly if the index length of stay was >6 days.
Predictors of 30‐Day Readmission After STEMI
Table 2 lists univariate and multivariate predictors of 30‐day readmission after initial hospitalization with STEMI. After adjusting for clinical and hospital characteristics, AIDS, anemia, chronic kidney disease, collagen vascular disease, diabetes mellitus, hypertension, pulmonary hypertension, congestive heart failure, and atrial fibrillation were found to be associated with an increased risk of 30‐day readmission. Although age was not associated with increased risk of readmission, female sex was a strong predictor of 30‐day readmission. More importantly, increased length of stay (LOS) during the index hospitalization was highly predictive of 30‐day readmission (62% increase in the group with LOS ≥6 days and 40% increase in the group with LOS 4 to 5 days versus the LOS ≤3 days group). In addition, private‐payer insurance and self‐pay status compared with Medicare were associated with fewer 30‐day readmissions. Unadjusted readmission rates were higher after CABG versus PCI, however, after multivariate adjustment, CABG was found to be predictive of fewer readmissions.
Table 2.
Independent Predictors of 30‐Day Readmission After Index Hospitalization With STEMI
| Predictors | Univariate Regressiona | Multivariate Regressionb | ||
|---|---|---|---|---|
| Unadjusted HR (95% CI) | P Value | Adjusted HR (95% CI) | P Value | |
| Female sex | 1.49 (1.46–1.53) | <0.001 | 1.18 (1.15–1.21) | <0.001 |
| Hypertension | 1.26 (1.23–1.30) | <0.001 | 1.08 (1.05–1.12) | <0.001 |
| Diabetes mellitus | 1.46 (1.43–1.50) | <0.001 | 1.21 (1.17–1.24) | <0.001 |
| Dyslipidemia | 0.87 (0.84–0.89) | <0.001 | 0.93 (0.91–0.96) | <0.001 |
| Family history of coronary artery disease | 0.72 (0.69–0.75) | <0.001 | 0.95 (0.91–0.99) | 0.030 |
| History of CHF | 2.11 (2.06–2.17) | <0.001 | 1.27 (1.23–1.31) | <0.001 |
| Peripheral vascular disease | 1.66 (1.59–1.73) | <0.001 | 1.16 (1.11–1.22) | <0.001 |
| Pulmonary hypertension | 1.90 (1.79–2.03) | <0.001 | 1.11 (1.04–1.19) | 0.002 |
| Chronic pulmonary disease | 1.59 (1.53–1.64) | <0.001 | 1.18 (1.14–1.22) | <0.001 |
| Chronic kidney disease | 2.12 (2.05–2.19) | <0.001 | 1.27 (1.23–1.32) | <0.001 |
| Liver disease | 1.40 (1.27–1.53) | <0.001 | 1.14 (1.04–1.25) | 0.007 |
| Anemia | 1.93 (1.87–2.00) | <0.001 | 1.12 (1.08–1.16) | <0.001 |
| Atrial fibrillation | 1.76 (1.70–1.81) | <0.001 | 1.17 (1.13–1.21) | <0.001 |
| AIDS | 1.48 (1.15–1.91) | 0.002 | 1.37 (1.06–1.76) | 0.017 |
| Collagen vascular disease | 1.38 (1.27–1.49) | <0.001 | 1.13 (1.04–1.22) | 0.002 |
| Fluid/electrolyte disorders | 1.65 (1.60–1.70) | <0.001 | 1.05 (1.02–1.09) | 0.005 |
| Median household income | ||||
| First quartile | 1 (reference) | 1 (reference) | ||
| Second quartile | 0.92 (0.89–0.95) | <0.001 | 0.95 (0.92–0.98) | 0.003 |
| Third quartile | 0.88 (0.85–0.92) | <0.001 | 0.91 (0.88–0.95) | <0.001 |
| Fourth quartile | 0.86 (0.83–0.90) | <0.001 | 0.90 (0.87–0.93) | <0.001 |
| Primary payer | ||||
| Medicare | 1 (reference) | 1 (reference) | ||
| Medicaid | 0.91 (0.87–0.95) | <0.001 | 1.06 (1.00–1.12) | 0.055 |
| Private including HMO | 0.49 (0.47–0.50) | <0.001 | 0.72 (0.69–0.75) | <0.001 |
| Self‐pay/no charge/other | 0.51 (0.49–0.53) | <0.001 | 0.73 (0.69–0.77) | <0.001 |
| Revascularization | ||||
| All PCI | 1 (reference) | 1 (reference) | ||
| CABG only | 1.37 (1.30–1.44) | <0.001 | 0.79 (0.75–0.84) | <0.001 |
| No revascularization | 1.66 (1.60–1.71) | <0.001 | 1.05 (1.01–1.09) | 0.014 |
| IABP | 1.59 (1.53–1.65) | <0.001 | 1.16 (1.11–1.22) | <0.001 |
| Hospital teaching status | ||||
| Teaching | 0.96 (0.93–0.98) | 0.003 | 0.96 (0.93–0.99) | 0.007 |
| Hospital location | ||||
| Rural | 1 (reference) | 1 (reference) | ||
| Urban | 1.11 (1.08–1.15) | <0.001 | 1.09 (1.06–1.12) | <0.001 |
| Length of hospital stay, d | ||||
| ≤3 | 1 (reference) | 1 (reference) | ||
| 4 to 5 | 1.73 (1.68–1.78) | <0.001 | 1.40 (1.36–1.45) | <0.001 |
| ≥6 | 2.46 (2.39–2.53) | <0.001 | 1.62 (1.56–1.68) | <0.001 |
| Disposition | ||||
| Home | 1 (reference) | 1 (reference) | ||
| Facilityc | 2.12 (2.05–2.19) | <0.001 | 1.18 (1.13–1.22) | <0.001 |
| AMA/unknown | 1.89 (1.72–2.09) | <0.001 | 1.88 (1.70–2.06) | <0.001 |
| Age group, y | ||||
| <50 | 1 (reference) | 1 (reference) | ||
| 50 to 64 | 1.07 (1.03–1.12) | 0.001 | 0.98 (0.94–1.02) | 0.275 |
| ≥65 | 1.80 (1.73–1.87) | <0.001 | 1.02 (0.97–1.08) | 0.400 |
| Smoking | 0.80 (0.78–0.82) | <0.001 | 0.98 (0.95–1.01) | 0.100 |
| Known coronary artery disease | 0.89 (0.86–0.92) | <0.001 | 1.04 (1.00–1.08) | 0.051 |
| Previous myocardial infarction | 1.17 (1.13–1.22) | <0.001 | 1.03 (0.99–1.08) | 0.125 |
| Previous PCI | 1.07 (1.03–1.11) | 0.001 | 1.03 (0.99–1.07) | 0.162 |
| Previous CABG | 1.33 (1.26–1.42) | <0.001 | 1.02 (0.96–1.08) | 0.622 |
| Other neurological disorders | 1.46 (1.39–1.55) | <0.001 | 1.00 (0.95–1.06) | 0.945 |
| Pulmonary circulation disorders | 2.21 (1.62–3.02) | <0.001 | 0.96 (0.69–1.34) | 0.822 |
| Valvular heart disease | 1.92 (1.56–2.37) | <0.001 | 0.86 (0.69–1.08) | 0.186 |
| Elixhauser comorbidity scores >4 | 2.20 (2.14–2.26) | <0.001 | 1.01 (0.96–1.05) | 0.822 |
| Weekend admission | 0.97 (0.94–0.99) | 0.014 | 1.00 (0.98–1.03) | 0.754 |
| Cardiogenic shock | 1.68 (1.61–1.75) | <0.001 | 1.02 (0.97–1.07) | 0.382 |
| Cardiogenic arrest | 1.25 (1.18–1.33) | <0.001 | 0.95 (0.89–1.00) | 0.065 |
| PLVAD | 1.51 (1.27–1.81) | <0.001 | 0.98 (0.81–1.18) | 0.834 |
AMA indicates against medical advice; CABG, coronary artery bypass graft; CHF, congestive heart failure; CI, confidence interval; HMO, health maintenance organization; HR, hazard ratio; PCI, percutaneous coronary intervention; PLVAD, percutaneous left ventricular assist device; STEMI, ST‐segment‐elevation myocardial infarction.
Univariate Cox proportional hazards regression model was created with an outcome of 30‐day readmission for each covariate from Table 1 and the covariates with P<0.1 are listed.
Multivariate Cox proportional hazards regression model was created with an outcome of 30‐day readmission including all predictors with P<0.1 in the univariate analysis.
Facility includes skilled nursing facility, intermediate care facility, and inpatient rehabilitation facility.
Independent predictors of 30‐day readmission were identified for subgroups of patients who underwent PCI, CABG, or no revascularization at the time of index admission with STEMI (Tables S1 through S3). Chronic kidney disease, chronic obstructive pulmonary disease, diabetes mellitus, congestive heart failure, and increased LOS during the index hospitalization (LOS >4 days) were associated with increased 30‐day readmission regardless of revascularization status. Female sex was associated with a greater likelihood of readmission in the revascularized cohort only (adjusted hazard ratio, 1.23; 95% CI, 1.19–1.27 in PCI cohort; adjusted hazard ratio, 1.39; 95% CI, 1.24–1.55 in CABG cohort).
Timing and Causes of 30‐Day Readmission After STEMI
Figure 2 and Figure S1 demonstrate the timing of readmission for the overall cohort as well as for subgroups stratified by revascularization status during the index admission for STEMI. Importantly, 43.9% were readmitted within 7 days of discharge, and 67.3% were readmitted within 14 days in the overall cohort, with median time to readmission being 9 days (IQR, 3–17 days). The revascularization status did not impact the timing of readmissions. In the overall cohort, 41.6% of readmissions were attributable to noncardiac causes (Figure 3); this was also seen in PCI and no‐revascularization subgroups (Figure S2). In patients who underwent CABG, noncardiac causes accounted for a majority (65.1%) of 30‐day readmissions (Figure S2B). In the overall cohort, 24% of 30‐day readmissions were secondary to chest pain, angina, or ischemia. In addition, 11.3% of readmissions were attributable to recurrent myocardial infarction, while 13.9% and 4.2% were attributable to heart failure and arrhythmic causes, respectively. Among noncardiac causes, infectious etiology (pneumonia and sepsis), chronic obstructive pulmonary disease/respiratory failure, gastrointestinal bleeding, stroke, and acute renal failure were most prevalent. Figure 4 and Figure S3 demonstrate that there is a separation in the frequency of cardiac versus noncardiac causes of 30‐day readmission, particularly within the first 2 weeks after discharge. In fact, Figure S4 demonstrates that readmissions due to recurrent myocardial infarction (13.3% versus 7.2, P<0.001) or heart failure (14.7% versus 12.1%, P<0.001) are more common in the first 2 weeks after discharge compared with 15 to 30 days after discharge from index admission. By 90 days, 42.5% of patients were still readmitted for noncardiac causes in the overall cohort, 39.7% in the PCI cohort, 62.7% in the CABG cohort, and 46.7% in the nonrevascularized cohort (Figure S5).
Figure 2.
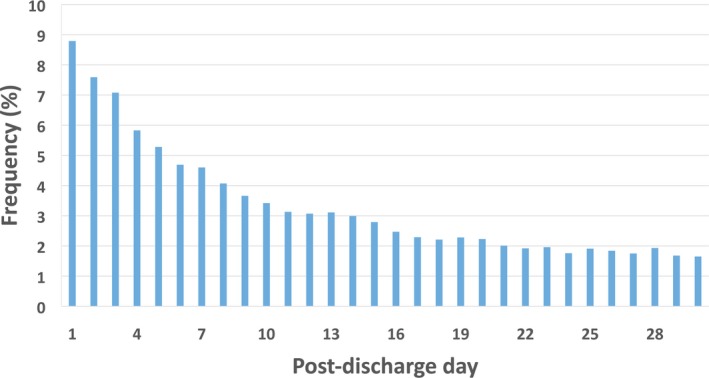
Timing of 30‐day readmission by postdischarge day in all patients after index admission for STEMI (ST‐segment–elevation myocardial infarction). *43.9% and 55.0% readmitted within 7 and 10 days, respectively. †Median time to readmission (IQR): 9 (3–17) days: 51.6% admitted within 9 days of discharge.
Figure 3.
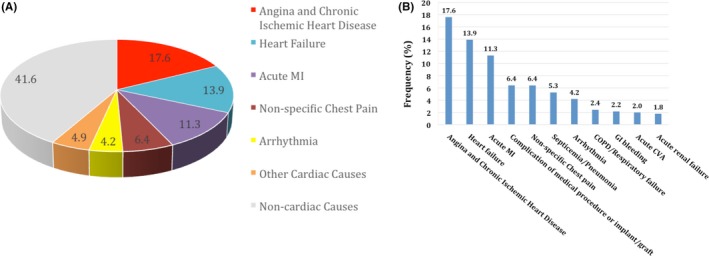
Common causes of 30‐day readmission in patients after index admission with STEMI. COPD indicates chronic obstructive pulmonary disease ; CVA, stroke; GI, gastro intestinal; MI, myocardial infarction; STEMI, ST‐segment‐elevation myocardial infarction.
Figure 4.
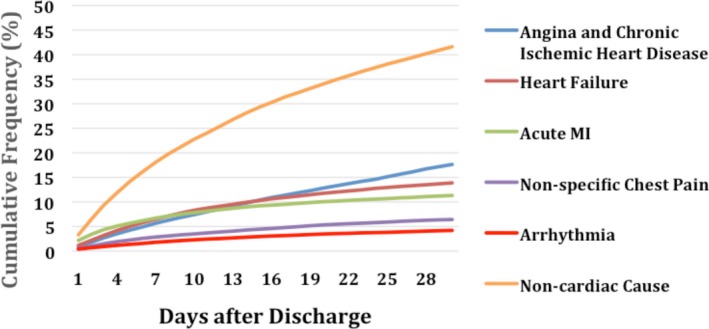
Cumulative frequency of 30‐day readmission for cardiac and noncardiac causes in post‐STEMI (ST‐segment‐elevation myocardial infarction) patients. MI indicates myocardial infarction.
Cost of Hospitalization and 30‐Day Readmission After STEMI
The median cumulative (index admission plus readmission) cost for those readmitted within 30 days was $31 072 (IQR, $21 374–47 321), whereas the cumulative cost for patients without 30‐day readmission was $18 169 (IQR, $13 498–25 548), P<0.001 (Table S4). The relative cost difference was particularly pronounced in medically treated patients, where the median cumulative cost for those readmitted within 30 days was $20 959 (IQR, $13 421–34 723), whereas the cumulative cost for patients without 30‐day readmission was $9273 (IQR, $6042–14 596), P<0.001. Table 3 demonstrates the association of 30‐day readmission and cumulative hospitalization cost. After multivariate adjustment, 30‐day readmission was associated with 47.9% increase in cumulative cost (95% CI, 0.47–0.49; P<0.001). Concomitant comorbidities including congestive heart failure, anemia, previously known coronary artery disease, obesity, peripheral vascular disease, valvular disease, and pulmonary circulation disorders also were independently associated with increased cumulative cost. In addition, cardiogenic shock (16% increase), cardiac arrest (18% increase), and the use of an intra‐aortic balloon pump (17% increase) or a percutaneous left ventricular assist device (66% increase) were associated with an increased cumulative cost. As expected, increased LOS (>4 days) was associated with higher cumulative cost, whereas lack of revascularization was associated with lower cumulative hospitalization cost.
Table 3.
Independent Predictors of Higher 30‐Day Total Cost of Hospitalization in Patients Treated After STEMI
| Predictors | Univariate Regressiona | Multivariate Regressionb | ||
|---|---|---|---|---|
| β (95% CI) | P Value | β (95% CI) | P Value | |
| 30‐day readmission | 0.556 (0.547–0.564) | <0.001 | 0.479 (0.472–0.486) | <0.001 |
| Age group, y | ||||
| <50 | 1 (reference) | 1 (reference) | ||
| 50–64 | 0.078 (0.071–0.085) | <0.001 | 0.019 (0.014–0.025) | <0.001 |
| ≥65 | 0.034 (0.025–0.043) | <0.001 | 0.004 (−0.005 to 0.012) | 0.381 |
| Female sex | −0.092 (−0.099 to −0.085) | <0.001 | −0.056 (−0.061 to −0.052) | <0.001 |
| Anemia | 0.250 (0.236–0.265) | <0.001 | 0.022 (0.014–0.030) | <0.001 |
| Obesity | 0.103 (0.093–0.113) | <0.001 | 0.044 (0.037–0.051) | <0.001 |
| Known coronary artery disease | 0.248 (0.234–0.261) | <0.001 | 0.060 (0.051–0.069) | <0.001 |
| Previous CABG | −0.162 (−0.181 to −0.142) | <0.001 | −0.030 (−0.043 to −0.018) | <0.001 |
| Coagulopathy | 0.604 (0.583–0.625) | <0.001 | 0.123 (0.111–0.136) | <0.001 |
| Diabetes mellitus | 0.088 (0.080–0.095) | <0.001 | 0.017 (0.013–0.022) | <0.001 |
| Peripheral vascular disease | 0.099 (0.084–0.113) | <0.001 | 0.020 (0.011–0.030) | <0.001 |
| Fluid/electrolyte disorders | 0.346 (0.332–0.359) | <0.001 | 0.069 (0.062–0.077) | <0.001 |
| History of CHF | 0.266 (0.254–0.278) | <0.001 | 0.029 (0.021–0.037) | <0.001 |
| Pulmonary hypertension | 0.189 (0.162–0.215) | <0.001 | 0.023 (0.008–0.038) | 0.003 |
| Pulmonary circulation disorders | 1.246 (1.120–1.371) | <0.001 | 0.487 (0.389–0.586) | <0.001 |
| Valvular heart disease | 1.184 (1.073–1.294) | <0.001 | 0.519 (0.448–0.590) | <0.001 |
| Elixhauser comorbidity scores >4 | 0.258 (0.246–0.271) | <0.001 | −0.016 (−0.024 to −0.008) | <0.001 |
| Median household income | ||||
| First quartile | 1 (reference) | 1 (reference) | ||
| Second quartile | 0.053 (0.040–0.066) | <0.001 | 0.053 (0.042–0.064) | <0.001 |
| Third quartile | 0.097 (0.081–0.112) | <0.001 | 0.090 (0.076–0.104) | <0.001 |
| Fourth quartile | 0.165 (0.146–0.185) | <0.001 | 0.157 (0.139–0.176) | <0.001 |
| Primary payer | ||||
| Medicare | 1 (reference) | 1 (reference) | ||
| Medicaid | 0.116 (0.102–0.131) | <0.001 | 0.056 (0.044–0.068) | <0.001 |
| Private including HMO | 0.036 (0.028–0.044) | <0.001 | 0.039 (0.031–0.046) | <0.001 |
| Self‐pay/no charge/other | −0.023 (−0.033 to −0.013) | <0.001 | 0.002 (−0.008 to 0.011) | 0.727 |
| Cardiogenic arrest | 0.630 (0.612–0.647) | <0.001 | 0.178 (0.166–0.191) | <0.001 |
| Cardiogenic shock | 0.761 (0.746–0.776) | <0.001 | 0.157 (0.146–0.168) | <0.001 |
| IABP | 0.829 (0.815–0.843) | <0.001 | 0.171 (0.160–0.182) | <0.001 |
| PVAD | 1.383 (1.320–1.445) | <0.001 | 0.660 (0.611–0.709) | <0.001 |
| Length of hospital stay, d | ||||
| ≤3 | 1 (reference) | 1 (reference) | ||
| 4 to 5 | 0.241 (0.232–0.250) | <0.001 | 0.230 (0.221–0.238) | <0.001 |
| ≥6 | 0.839 (0.830–0.850) | <0.001 | 0.674 (0.663–0.684) | <0.001 |
| Revascularization | ||||
| All PCI | 1 (reference) | 1 (reference) | ||
| CABG only | 0.791 (0.774–0.808) | <0.001 | 0.171 (0.155–0.187) | <0.001 |
| No revascularization | −0.640 (−0.653 to −0.626) | <0.001 | −0.730 (−0.743 to −0.717) | <0.001 |
| Weekend admission | 0.012 (0.005–0.018) | <0.001 | 0.020 (0.015–0.024) | <0.001 |
| Hospital bed size | ||||
| Small | 1 (reference) | 1 (reference) | ||
| Medium | 0.064 (0.010–0.118) | 0.021 | −0.021 (−0.070 to 0.028) | 0.393 |
| Large | 0.119 (0.067–0.172) | <0.001 | −0.021 (−0.068 to 0.027) | 0.393 |
| Hospital location | ||||
| Rural | 1 (reference) | 1 (reference) | ||
| Urban | 0.094 (0.072–0.115) | <0.001 | 0.008 (−0.012 to 0.028) | 0.448 |
| Hospital teaching status | ||||
| Teaching | 0.111 (0.089–0.133) | <0.001 | 0.033 (0.012–0.053) | 0.002 |
| Disposition | ||||
| Home | 1 (reference) | 1 (reference) | ||
| Facilityc | 0.087 (0.066–0.107) | <0.001 | −0.028 (−0.039 to −0.017) | <0.001 |
| AMA/unknown | −0.350 (−0.385 to −0.314) | <0.001 | −0.129 (−0.153 to −0.105) | <0.001 |
AMA indicates against medical advice; CABG, coronary artery bypass graft; CHF, congestive heart failure; CI, confidence interval; HMO, health maintenance organization; IABP, intra‐aortic balloon pump; PCI, percutaneous coronary intervention; PVAD, percutaneous ventricular assist device; STEMI, ST‐segment‐elevation myocardial infarction.
Survey‐specific univariate linear regression model was created with an outcome of log‐transformed cumulative cost for each covariate from Table 1 and the covariates with P<0.1 are listed.
Survey‐specific multivariate linear regression model was created with an outcome of log‐transformed cumulative cost including all predictors with P<0.1 in the univariate analysis.
Facility includes skilled nursing facility, intermediate care facility, and inpatient rehabilitation facility.
Discussion
There are several important and novel findings in this large, contemporary, all‐payer observational study of the National Readmission Database in the years 2010 to 2014. First, in this overall cohort of >700 000 STEMI patients, the 30‐day readmission rate was 12.3%, lower than the previously reported rate of ≈20%.8 The median length of index hospitalization was short (2.5 days) and median length of readmission stay was 2.6 days, while index admission in‐hospital mortality was 8.7% and readmission in‐hospital mortality was 4.6%. Second, over the 5‐year period, the 30‐day readmission rates after STEMI have declined, particularly in those undergoing PCI and in medically treated patients. Third, of patients readmitted, two thirds were readmitted early (within the first 14 days after discharge). Fourth, a large proportion of patients (≈40%) were readmitted within 30 or 90 days for noncardiac reasons, whereas in the post‐CABG population, two thirds of 30‐ and 90‐day readmissions were for noncardiac reasons. Finally, 30‐day readmission was associated with a 47.9% increase in the cumulative hospitalization cost, with the cumulative cost increase of $12 903 in those with 30‐day readmission.
This study has extended prior literature by revealing that the rate of 30‐day readmissions after STEMI declined between 2010 and 2014. In the 2007–2009 Medicare fee‐for‐service claims data, the rate of 30‐day readmission after STEMI hospitalization was 19.9%.5 Our data suggest that the 30‐day readmission rate declined to 13.5% in 2010 and to 10.9% in 2014. This decline in 30‐day readmissions after STEMI has been also seen in the fee‐for‐service Medicare and Veterans Health Administration beneficiaries between 2009 and 2012.15 The decline in readmissions following STEMI may be due to widespread use of primary PCI (≈80% in our study), adherence to improved antiplatelet and medical therapy, and greater national focus by the Centers for Medicare & Medicaid Services on reducing 30‐day readmissions. Angina and ischemic heart disease have been identified as the primary reason for cardiac readmissions in our study. A minority of these readmissions are due to planned PCI, given that a proportion of patients in the United States are readmitted within 30 days after STEMI for planned elective PCI or, less commonly, CABG.16
Similar to previous work, we have demonstrated that a large proportion of patients are readmitted early after STEMI, with 67.3% of patients being readmitted within 14 days. The median time to readmission of 9 days in our cohort was similar to the published data in the Medicare population, where median time to readmission was 10 days after STEMI.5 Given that one third of 30‐day readmissions occur during days 15 through 30 after hospitalization, meticulous attention should be paid to the period beyond the initial follow‐up visit within 1 to 2 weeks of hospitalization. This may partly explain why outpatient interventions have been ineffective in reducing 30‐day readmissions when close outpatient follow‐up was lacking.17 The timing of 30‐day readmissions highlights the importance of both early outpatient care and longitudinal surveillance strategies within 30 to 90 days following hospitalization.18 Measures focusing on supportive discharge interventions have been shown to enhance patient capacity for self‐care and have helped to avoid readmissions.19 Comprehensive programs that focus on both inpatient and outpatient interventions and utilize tools that facilitate cross‐site communication can lead to a decrease in early readmissions.20, 21 Programs focusing on reducing 30‐day readmissions should take into account that over one third of all readmissions occur for noncardiac reasons, with two thirds of post‐CABG patients being readmitted for medical conditions within 30 days. Therefore, continuity of care with primary care providers from the inpatient setting to strategic follow‐up after discharge should be of great importance. This is particularly important in the post‐CABG population, where many patients may benefit from earlier and closer medical surveillance (especially in the setting of the global surgical fee). Furthermore, institutions with poorer patient safety performance have been associated with greater unplanned readmissions.22 Additional follow‐up measures, including provider‐initiated telephone or videophone communication, the use of remote telemonitoring, provider home visits, and patient‐directed rehabilitation efforts, should be considered and intensified.19
Thirty‐day hospital readmissions are common and costly, particularly in the elderly and high‐risk patients with STEMI.23 Similar to our data, prior studies have also indicated that the risk of readmission was higher in women compared with men, particularly in younger patients.24, 25 The analysis of the 2013 National Readmissions Database confirmed an unequal burden of readmissions on women, particularly in younger women.25 This may be partly explained by the fact that women have atypical presentation symptoms and different risk factors and receive suboptimal care because of being underdiagnosed with STEMI.26 Therefore, reperfusion in women is often delayed, which may lead to higher rates of adverse events and more rehospitalizations.26 Women are also at a higher risk for bleeding and vascular complications after PCI, with lower adoption of radial PCI, which can also lead to more readmissions.27 Importantly, age was not found to be an independent predictor of 30‐day readmissions. Other studies have indicated that patients >65 years of age had higher risk‐adjusted odds for readmission.24 However, despite conflicting data regarding the association of 30‐day readmission with advanced age, the burden of readmission among younger patients still remains substantial. Thus, it is important to continue monitoring for differences in the quality of STEMI care and adherence to process measures based on age, sex, and other sociodemographic characteristics.
Our study further confirms the relationship between LOS and readmission rates. The LOS after STEMI has dramatically declined in the United States during the past quarter century.28 The median LOS for the index admission with STEMI was only 2.5 days. The United States has one of the lowest lengths of stay compared with other countries.29 This trend is likely driven by financial factors within a healthcare system that rewards early discharge. Concerns have been raised that very early discharge (<48 hours) may result in suboptimal outcomes.30 Nevertheless, this analysis suggests that early discharge (≤3 days) was associated with fewer readmissions compared with longer LOS of 4–5 days or ≥6 days. As one might predict, patients with a prolonged index hospitalization of ≥6 days because of complexity of the clinical presentation and adverse in‐hospital post–myocardial infarction events, are much more likely to be readmitted within 30 days. Our findings indicate that hospitals and clinicians (both cardiologists and primary care providers) should intensify their focus and postdischarge surveillance of patients with prolonged LOS given the high risk of subsequent events.
There is a growing interest in examining costs associated with post‐STEMI readmissions.4, 23, 31, 32 Recent data on post‐PCI readmissions in 2013 indicate that the mean cumulative costs are higher for those with readmissions ($39 634 versus $22 058; P<0.001), with multivariable analysis showing that readmission accounted for a 45% increase in cumulative costs.14 Our cost analysis data extend these findings to the STEMI population ($31 072 versus $18 169; P<0.001). After the multivariable adjustment, the 30‐day readmission after STEMI substantially increased the cumulative costs by nearly 50%. This is of particular importance, given the Medicare Access and CHIP Reauthorization Act of 2015, which penalizes hospitals with higher risk‐adjusted 30‐day readmission rates regardless of the cause for readmission.33 Such reimbursement policies are designed to encourage hospitals to develop better strategies to prevent expensive 30‐day readmissions. Currently, voluntary payment bundles for STEMI care (that extend to 90 days) are being introduced. However, hospitals may be discouraged to participate in such bundles given that ≈40% of 90‐day readmissions occur for noncardiac reasons, and thus the hospitals would be forced to absorb the high cost of noncardiac readmissions. Several important questions remain: whether the bundled payment structure will result in better post‐STEMI outcomes and whether hospitals should be penalized for noncardiac readmissions after STEMI. Furthermore, policymakers need to ensure that 30‐day readmission rates after STEMI is a good‐quality metric that leads to better outcomes, which recently has been questioned in the heart failure literature.34 Further research is needed to examine the preventability of 30‐day readmissions after STEMI and to explore whether short‐term readmissions after STEMI should serve as a reliable quality metric of hospital performance and better clinical outcomes.
The results of this study should be interpreted in the context of several limitations. First, this is a retrospective study based on data from the NRD, with the sample designed to approximate the national distribution of key hospital characteristics. Our estimates were derived from a 50% sample of US hospitals, and it is possible that the readmission cohort was either underrepresented or overrepresented by this sample. However, the NRD has been used extensively to examine national healthcare trends, and its sampling design has been validated in numerous publications.14, 24, 25 Second, miscoded and missing data can occur in large administrative data sets; however, Healthcare Cost and Utilization Project quality control procedures are routinely performed to confirm that NRD data values are valid, consistent, and reliable.35, 36 Third, the NRD does not include detailed information about patient clinical characteristics, such as coronary anatomy, heart failure class, left ventricular function, or admission/discharge medications. Data on discharge medications or long‐term compliance with medications were not available. Fourth, we have reported mortality during the 30‐day readmission (although not the main focus of our analysis), since the NRD does not have data regarding out‐of‐hospital mortality in patients discharged after STEMI. Therefore, our post‐STEMI mortality estimates could be lower than the actual 30‐day post‐STEMI mortality. Also, we were not able to define readmissions because of planned staged PCI. Nonetheless, inclusion of planned staged PCI as readmission is important for estimation of total costs.37 Furthermore, we used ICD‐9 codes for defining clinical scenarios and procedures, which may lead to misclassification bias. Noncardiac causes of readmission may have been underestimated by not including readmissions due to the revascularization strategy (eg, bleeding or vascular complications from transfemoral access, acute renal failure from contrast‐induced nephropathy, pneumonia after intubation, infection from central line placement, or sternotomy). Finally, the NRD includes discharge information from 22 states across the United States and represents a national population; however, our results cannot be considered completely generalizable.
Conclusions
This study examined post‐STEMI readmission rates, causes, timing, and the association of readmissions on overall 30‐day costs after STEMI. Thirty‐day readmission rates after STEMI have declined, particularly in those undergoing PCI and in medically treated patients. Nearly two thirds of patients were readmitted early, within the first 14 days after discharge. A large proportion of patients were readmitted within 30 or 90 days for noncardiac reasons, particularly after CABG. Thirty‐day readmission was associated with an ≈50% increase in the cumulative hospitalization cost. These data suggest that early readmissions could be prevented by closer surveillance and attention to both cardiac and general medical conditions before and within the early discharge period. Further research is warranted to examine strategies to prevent 30‐day readmissions after STEMI and to examine whether short‐term readmissions after STEMI should serve as a quality metric of hospital performance and better outcomes.
Sources of Funding
This work was supported by grants from the Michael Wolk Heart Foundation and the New York Cardiac Center, Inc (New York, NY). The Michael Wolk Heart Foundation and the New York Cardiac Center, Inc had no role in the design and conduct of the study; in the collection, analysis, and interpretation of the data; or in the preparation, review, or approval of the manuscript.
Disclosures
None.
Supporting information
Table S1. Independent Predictors of 30‐Day Readmission after Index Hospitalization With STEMI in Patients Treated With PCI
Table S2. Independent Predictors of 30‐Day Readmission After Index Hospitalization With STEMI in Patients Treated With CABG
Table S3. Independent Predictors of 30‐Day Readmission After Index Hospitalization With STEMI in Medically Treated (Nonrevascularized) Patients
Table S4. Cumulative 30‐Day Charges and Costs
Figure S1. A, Timing of 30‐day readmission by postdischarge day in patients treated with PCI during index admission for STEMI. *43.8% and 54.8% admitted within 7 and 10 days, respectively. †Median time to readmission (IQR): 9 (3–17) days: 51.4% admitted within 9 days of discharge. B, Timing of 30‐day readmission by post‐discharge day in patients treated with CABG only during index admission for STEMI. *42.0% admitted within 7 days, 50.6% within 9 days and 54.0% within 10 days of discharge. †Median time to readmission (IQR): 9 (4–17) days. C, Timing of 30‐day readmission by post‐discharge day in patients without revascularization during index admission for STEMI. *44.5% and 55.7% admitted within 7 and 10 days, respectively. †Median time to readmission (IQR): 8 (3–17) days: 48.5% and 52.1% admitted within 8 and 9 days, respectively.
Figure S2. Common causes of 30‐day readmission after index admission with STEMI in the (A) PCI cohort, (B) CABG cohort, and (C) nonrevascularization cohort.
Figure S3. Cumulative frequency of 30‐day readmission for (A) cardiac versus noncardiac causes in post‐PCI patients, (B) cardiac versus noncardiac causes in post‐CABG patients, and (C) cardiac versus noncardiac causes in patients without revascularization.
Figure S4. Common causes of 30‐day readmission in patients readmitted within 14 days versus 15 to 30 days of discharge after index admission with STEMI. Values are presented as percentage. P value for *<0.001, P value for nonspecific chest pain=0.26, P value for arrhythmia=0.65, P value for noncardiac causes=0.32.
Figure S5. Cumulative frequency of 90‐day readmission for (A) cardiac and noncardiac causes in the overall cohort, (B) cardiac and noncardiac causes in post‐PCI patients, (C) cardiac and noncardiac causes in post‐CABG patients, and (D) cardiac and noncardiac causes in medically treated (nonrevascularized) patients.
(J Am Heart Assoc. 2018;7:e009863. DOI: 10.1161/JAHA.118.009863.)30371187
References
- 1. Reed GW, Rossi JE, Cannon CP. Acute myocardial infarction. Lancet. 2017;389:197–210. [DOI] [PubMed] [Google Scholar]
- 2. Yeh RW, Sidney S, Chandra M, Sorel M, Selby JV, Go AS. Population trends in the incidence and outcomes of acute myocardial infarction. N Engl J Med. 2010;362:2155–2165. [DOI] [PubMed] [Google Scholar]
- 3. Benjamin EJ, Virani SS, Callaway CW, Chamberlain AM, Chang AR, Cheng S, Chiuve SE, Cushman M, Delling FN, Deo R, de Ferranti SD, Ferguson JF, Fornage M, Gillespie C, Isasi CR, Jiménez MC, Jordan LC, Judd SE, Lackland D, Lichtman JH, Lisabeth L, Liu S, Longenecker CT, Lutsey PL, Mackey JS, Matchar DB, Matsushita K, Mussolino ME, Nasir K, O'Flaherty M, Palaniappan LP, Pandey A, Pandey DK, Reeves MJ, Ritchey MD, Rodriguez CJ, Roth GA, Rosamond WD, Sampson UKA, Satou GM, Shah SH, Spartano NL, Tirschwell DL, Tsao CW, Voeks JH, Willey JZ, Wilkins JT, Wu JH, Alger HM, Wong SS, Muntner P; American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee . Heart disease and stroke statistics‐2018 update: a report from the American Heart Association. Circulation. 2018;137:e67–e492. [DOI] [PubMed] [Google Scholar]
- 4. Torio CM, Moore BJ. National Inpatient Hospital Costs: The Most Expensive Conditions by Payer, 2013. HCUP Statistical Brief # 204. Available at: http://www.hcup-us.ahrq.gov/reports/statbriefs/sb204-Most-Expensive-Hospital-Conditions.pdf. Published May 2016. Accessed March 23, 2018.
- 5. Dharmarajan K, Hsieh AF, Lin Z, Bueno H, Ross JS, Horwitz LI, Barreto‐Filho JA, Kim N, Bernheim SM, Suter LG, Drye EE, Krumholz HM. Diagnoses and timing of 30‐day readmissions after hospitalization for heart failure, acute myocardial infarction, or pneumonia. JAMA. 2013;309:355–363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Fingar K, Washington R. Trends in Hospital Readmissions for Four High‐Volume Conditions, 2009–2013. HCUP Statistical Brief # 196. Available at: http://www.hcup-us.ahrq.gov/reports/statbriefs/sb196-Readmissions-Trends-High-Volume-Conditions.pdf. Published November 2015. Accessed March 26, 2018.
- 7. Medicare Payment Advisory Commission . Report to the Congress promoting greater efficiency in Medicare. 2007. Available at: http://purl.access.gpo.gov/GPO/LPS106668. Accessed March 28, 2018.
- 8. Krumholz HM, Merrill AR, Schone EM, Schreiner GC, Chen J, Bradley EH, Wang Y, Wang Y, Lin Z, Straube BM, Rapp MT, Normand SL, Drye EE. Patterns of hospital performance in acute myocardial infarction and heart failure 30‐day mortality and readmission. Circ Cardiovasc Qual Outcomes. 2009;2:407–413. [DOI] [PubMed] [Google Scholar]
- 9. Kocher RP, Adashi EY. Hospital readmissions and the Affordable Care Act: paying for coordinated quality care. JAMA. 2011;306:1794–1795. [DOI] [PubMed] [Google Scholar]
- 10. Agency for Healthcare Research and Quality . Introduction to the HCUP Nationwide Readmissions Database (NRD). Available at: https://www.hcupus.ahrq.gov/db/nation/nrd/Introduction_NRD_2010-2014.pdf.. Accessed March 14, 2018.
- 11. Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36:8–27. [DOI] [PubMed] [Google Scholar]
- 12. Agency for Healthcare Research and Quality . Introduction to the HCUP Nationwide Readmissions Database (NRD). Available at: https://www.hcup-us.ahrq.gov/db/nation/nrd/Introduction_NRD_2010-2014.pdf. Accessed March 14, 2018.
- 13. Fingar KR, Barrett ML, Jiang HJ. A Comparison of All‐Cause 7‐Day and 30‐Day Readmissions, 2014. HCUP Statistical Brief # 230. Available at: https://www.hcup-us.ahrq.gov/reports/statbriefs/sb230-7-Day-Versus-30-Day-Readmissions.pdf. Published October 2017. Accessed March 21, 2018.
- 14. Tripathi A, Abbott JD, Fonarow GC, Khan AR, Barry NG IV, Ikram S, Coram R, Mathew V, Kirtane AJ, Nallamothu BK, Hirsch GA, Bhatt DL. Thirty‐day readmission rate and costs after percutaneous coronary intervention in the United States: a national readmission database analysis. Circ Cardiovasc Interv. 2017;10:e005925. [DOI] [PubMed] [Google Scholar]
- 15. Suter LG, Li SX, Grady JN, Lin Z, Wang Y, Bhat KR, Turkmani D, Spivack SB, Lindenauer PK, Merrill AR, Drye EE, Krumholz HM, Bernheim SM. National patterns of risk‐standardized mortality and readmission after hospitalization for acute myocardial infarction, heart failure, and pneumonia: update on publicly reported outcomes measures based on the 2013 release. J Gen Intern Med. 2014;29:1333–1340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Kociol RD, Lopes RD, Clare R, Thomas L, Mehta RH, Kaul P, Pieper KS, Hochman JS, Weaver WD, Armstrong PW, Granger CB, Patel MR. International variation in and factors associated with hospital readmission after myocardial infarction. JAMA. 2012;307:66–74. [DOI] [PubMed] [Google Scholar]
- 17. Wong FK, Chow S, Chung L, Chang K, Chan T, Lee WM, Lee R. Can home visits help reduce hospital readmissions? Randomized controlled trial J Adv Nurs. 2008;62:585–595. [DOI] [PubMed] [Google Scholar]
- 18. Khot UN, Johnson MJ, Lowry AM, Rajeswaran J, Kapadia S, Shishehbor MH, Menon V, Ellis SG, Goepfarth P, Blackstone EH. The time‐varying risk of cardiovascular and noncardiovascular readmissions early after acute myocardial infarction. J Am Coll Cardiol. 2017;70:1101–1103. [DOI] [PubMed] [Google Scholar]
- 19. Leppin AL, Gionfriddo MR, Kessler M, Brito JP, Mair FS, Gallacher K, Wang Z, Erwin PJ, Sylvester T, Boehmer K, Ting HH, Murad MH, Shippee ND, Montori VM. Preventing 30‐day hospital readmissions: a systematic review and meta‐analysis of randomized trials. JAMA Intern Med. 2014;174:1095–1107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Coleman EA, Parry C, Chalmers S, Min SJ. The care transitions intervention: results of a randomized controlled trial. Arch Intern Med. 2006;166:1822–1828. [DOI] [PubMed] [Google Scholar]
- 21. Naylor M, Brooten D, Jones R, Lavizzo‐Mourey R, Mezey M, Pauly M. Comprehensive discharge planning for the hospitalized elderly: a randomized clinical trial. Ann Intern Med. 1994;120:999–1006. [DOI] [PubMed] [Google Scholar]
- 22. Wang Y, Eldridge N, Metersky ML, Sonnenfeld N, Fine JM, Pandolfi MM, Eckenrode S, Bakullari A, Galusha DH, Jaser L, Verzier NR, Nuti SV, Hunt D, Normand SL, Krumholz HM. Association between hospital performance on patient safety and 30‐day mortality and unplanned readmission for Medicare fee‐for service patients with acute myocardial infarction. J Am Heart Assoc. 2016;5:e003731 DOI: 10.1161/JAHA.116.003731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee‐for‐service program. N Engl J Med. 2009;360:1418–1428. [DOI] [PubMed] [Google Scholar]
- 24. Khera R, Jain S, Pandey A, Agusala V, Kumbhani DJ, Das SR, Berry JD, de Lemos JA, Girotra S. Comparison of readmission rates after acute myocardial infarction in 3 patient age groups (18 to 44, 45 to 64, and ≥65 years) in the United States. Am J Cardiol. 2017;120:1761–1767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. O'Brien C, Valsdottir L, Wasfy JH, Strom JB, Secemsky EA, Wang Y, Yeh RW. Comparison of 30‐day readmission rates after hospitalization for acute myocardial infarction in men versus women. Am J Cardiol. 2017;120:1070–1076. [DOI] [PubMed] [Google Scholar]
- 26. Mehta LS, Beckie TM, DeVon HA, Grines CL, Krumholz HM, Johnson MN, Lindley KJ, Vaccarino V, Wang TY, Watson KE, Wenger NK; American Heart Association Cardiovascular Disease in Women and Special Populations Committee of the Council on Clinical Cardiology, Council on Epidemiology and Prevention, Council on Cardiovascular and Stroke Nursing, and Council on Quality of Care and Outcomes Research . Acute myocardial infarction in women: a scientific statement from the American Heart Association. Circulation. 2016;133:916–947. [DOI] [PubMed] [Google Scholar]
- 27. Feldman DN, Swaminathan RV, Kaltenbach LA, Baklanov DV, Kim LK, Wong SC, Minutello RM, Messenger JC, Moussa I, Garratt KN, Piana RN, Hillegass WB, Cohen MG, Gilchrist IC, Rao SV. Adoption of radial access and comparison of outcomes to femoral access in percutaneous coronary intervention: an updated report from the national cardiovascular data registry (2007–2012). Circulation. 2013;127:2295–2306. [DOI] [PubMed] [Google Scholar]
- 28. Baker DW, Einstadter D, Husak SS, Cebul RD. Trends in postdischarge mortality and readmissions: has length of stay declined too far? Arch Intern Med. 2004;164:538–544. [DOI] [PubMed] [Google Scholar]
- 29. Kaul P, Newby LK, Fu Y, Mark DB, Califf RM, Topol EJ, Aylward P, Granger CB, Van de Werf F, Armstrong PW. International differences in evolution of early discharge after acute myocardial infarction. Lancet. 2004;363:511–517. [DOI] [PubMed] [Google Scholar]
- 30. Swaminathan RV, Rao SV, McCoy LA, Kim LK, Minutello RM, Wong SC, Yang DC, Saha‐Chaudhuri P, Singh HS, Bergman G, Feldman DN. Hospital length of stay and clinical outcomes in older STEMI patients after primary PCI: a report from the National Cardiovascular Data Registry. J Am Coll Cardiol. 2015;65:1161–1171. [DOI] [PubMed] [Google Scholar]
- 31. Huckfeldt PJ, Mehrotra A, Hussey PS. The relative importance of post‐acute care and readmissions for post‐discharge spending. Health Serv Res. 2016;51:1919–1938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Bradley EH, Curry L, Horwitz LI, Sipsma H, Thompson JW, Elma M, Walsh MN, Krumholz HM. Contemporary evidence about hospital strategies for reducing 30‐day readmissions: a national study. J Am Coll Cardiol. 2012;60:607–614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Centers for Medicare & Medicaid Services (CMS), HHS . Medicare Program; Merit‐Based Incentive Payment System (MIPS) and Alternative Payment Model (APM) Incentive Under the Physician Fee Schedule, and Criteria for Physician‐Focused Payment Models. Final rule with comment period. Fed Regist. 2016;81:77008–77831. [PubMed] [Google Scholar]
- 34. Pandey A, Golwala H, Xu H, DeVore AD, Matsouaka R, Pencina M, Kumbhani DJ, Hernandez AF, Bhatt DL, Heidenreich PA, Yancy CW, de Lemos JA, Fonarow GC. Association of 30‐day readmission metric for heart failure under the hospital readmissions reduction program with quality of care and outcomes. JACC Heart Fail. 2016;4:935–946. [DOI] [PubMed] [Google Scholar]
- 35. Barrett ML, Ross DN. HCUP Quality Control Procedures Deliverable #1707.05. Available at: https://www.hcup-us.ahrq.gov/db/quality.pdf. Published February 20, 2017. Accessed March 26, 2018.
- 36. Yoon F, Sheng M, Jiang HJ, Steiner CA, Barrett ML. Calculating Nationwide Readmissions Database (NRD) Variances. HCUP Methods Series Report No. 2017‐01. Available at: https://www.hcup-us.ahrq.gov/reports/methods/2017-01.pdf. Published January 24, 2017. Accessed March 2, 2018.
- 37. Hannan EL, Zhong Y, Krumholz H, Walford G, Holmes DR Jr, Stamato NJ, Jacobs AK, Venditti FJ, Sharma S, King SB III. 30‐day readmission for patients undergoing percutaneous coronary interventions in New York State. JACC Cardiovasc Interv. 2011;4:1335–1342. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Independent Predictors of 30‐Day Readmission after Index Hospitalization With STEMI in Patients Treated With PCI
Table S2. Independent Predictors of 30‐Day Readmission After Index Hospitalization With STEMI in Patients Treated With CABG
Table S3. Independent Predictors of 30‐Day Readmission After Index Hospitalization With STEMI in Medically Treated (Nonrevascularized) Patients
Table S4. Cumulative 30‐Day Charges and Costs
Figure S1. A, Timing of 30‐day readmission by postdischarge day in patients treated with PCI during index admission for STEMI. *43.8% and 54.8% admitted within 7 and 10 days, respectively. †Median time to readmission (IQR): 9 (3–17) days: 51.4% admitted within 9 days of discharge. B, Timing of 30‐day readmission by post‐discharge day in patients treated with CABG only during index admission for STEMI. *42.0% admitted within 7 days, 50.6% within 9 days and 54.0% within 10 days of discharge. †Median time to readmission (IQR): 9 (4–17) days. C, Timing of 30‐day readmission by post‐discharge day in patients without revascularization during index admission for STEMI. *44.5% and 55.7% admitted within 7 and 10 days, respectively. †Median time to readmission (IQR): 8 (3–17) days: 48.5% and 52.1% admitted within 8 and 9 days, respectively.
Figure S2. Common causes of 30‐day readmission after index admission with STEMI in the (A) PCI cohort, (B) CABG cohort, and (C) nonrevascularization cohort.
Figure S3. Cumulative frequency of 30‐day readmission for (A) cardiac versus noncardiac causes in post‐PCI patients, (B) cardiac versus noncardiac causes in post‐CABG patients, and (C) cardiac versus noncardiac causes in patients without revascularization.
Figure S4. Common causes of 30‐day readmission in patients readmitted within 14 days versus 15 to 30 days of discharge after index admission with STEMI. Values are presented as percentage. P value for *<0.001, P value for nonspecific chest pain=0.26, P value for arrhythmia=0.65, P value for noncardiac causes=0.32.
Figure S5. Cumulative frequency of 90‐day readmission for (A) cardiac and noncardiac causes in the overall cohort, (B) cardiac and noncardiac causes in post‐PCI patients, (C) cardiac and noncardiac causes in post‐CABG patients, and (D) cardiac and noncardiac causes in medically treated (nonrevascularized) patients.


