Abstract
To assess primary care providers' (PCPs) opinions related to recommending home blood pressure monitoring (HBPM) for their hypertensive patients, the authors analyzed a Web‐based 2010 DocStyles survey, which included PCPs' demographics, health‐related behaviors, recommendations on HBPM, views of patient knowledge, and use of continuing medical education. Of the 1254 PCPs who responded, 539 were family practitioners, 461 were internists, and 254 were nurse practitioners; 32% recommended HBPM to ≥90% of their patients and 26% recommended it to ≤40% of their patients. Nurse practitioners were significantly more likely to recommend HBPM than were internists (odds ratio, 0.55; 95% confidence interval, 0.40–0.78). The top reasons for not recommending HBPM were “patient can't afford it” and “patient doesn't need it.” A total of 20% of PCPs indicated that their patients were poor to lower middle class; these PCPs were less likely to recommend HBPM to their patients than were those PCPs with most patients in higher economic classes. Additional efforts are needed to provide education to providers, especially physicians, about the benefits of HBPM in improved and cost‐effective blood pressure control in the United States.
Hypertension is a well‐known risk factor for heart disease and stroke1, 2 and affects approximately 68 million people in the United States.3, 4 Although there have been improvements in antihypertensive medications during the past 2 decades, fewer than half of people with hypertension have their blood pressure (BP) under control.3, 4 During 2005 to 2008, just 45.8% of hypertensive adults had their BP under control.4 National guidelines for management of hypertension include using lifestyle and behavior modifications along with antihypertensive medication to reach recommended BP levels and reduce the risk of coronary heart disease and stroke.1, 2
Home BP monitoring (HBPM) can build on the benefits of traditional office‐based BP monitoring.1, 2, 3, 4 The Seventh Report of the Joint National Committee on Prevention, Detection, and Treatment of High Blood Pressure (JNC 7) recommends HBPM as an effective way to provide information on a patient's response to treatment, improve compliance with therapy, and evaluate white‐coat hypertension.1, 2 The report also states that HBPM can guide behavioral change and goal setting in the pursuit to empower patients and help them invest in their own care.1, 2 Furthermore, a meta‐analysis of clinical trials showed that HBPM led to a significant 2‐fold reduction in medication compared with clinical BP monitoring alone. HBPM use has been shown to improve adherence to medication, allowing for dosage reduction and stabilization of BP, and to reduce the so‐called white‐coat effect, thus improving cardiovascular and end‐stage renal outcomes.6 However, in clinical settings, HBPM is an underutilized tool for fighting hypertension, with only 55% of patients using HBPM in 2005.7 These differences in regular HBPM use among hypertensive adults were associated with sex, age, race/ethnicity, household income, and education.8
Most studies of HBPM have provided clinical data or information from the patient's perspective, but scant information regarding physicians' attitudes and reasons for recommending HBPM exist. Primary care providers (PCPs) are usually the first line of care for patients with hypertension.9, 10 The objective of this study was to use data from the DocStyles 2010 survey to examine PCPs' attitudes regarding HBPM. In cases where HBPM use was not recommended, we wanted to determine any association with that decision and the PCPs' characteristics such as demographics, self‐report of continuing medical education (CME), and views on patients' medical knowledge and financial situation.
Methods
DocStyles 2010, an Internet survey conducted by Porter Novelli (Atlanta, GA, www.porternovelli.com) in July 2010, was sent to PCPs to understand how their attitudes influenced responses to health‐related inquiries pertaining to their practice. Physicians surveyed were randomly sampled from the Epocrates Honor Panel, a verified opt‐in panel of more than 168,000 medical practitioners. At the time of registration, physician verification was performed by confirming the first name, last name, date of birth, medical school, and graduation date with the American Medical Association's master file. Nurse practitioners were drawn from the Epocrates Allied Health Panel, which includes 560,000 health professionals, including 51,785 nurse practitioners.
Porter Novelli set a quota of 1000 PCPs and 250 nurse practitioners. In total, 1877 physicians and 431 nurse practitioners were screened, including only those who had been actively seeing patients in the United States for ≥3 years and who worked in an individual, group, or hospital practice. Those selected were not required to start or finish the survey. The estimated time of completion was 30 to 60 minutes and each participant received an honorarium of $40 to $60 after completion. No personal identifiers were included in the data file obtained by the Centers for Disease Control and Prevention. One thousand PCPs completed the entire survey for a response rate of 45.2%, as calculated by Porter Novelli. Those who did not complete the survey included 774 who did not respond to the invitation or responded after the survey ended, 60 who did not complete the entire survey, 30 who did not meet screening criteria, and 13 who were terminated because of filled quotas. Of the 431 nurse practitioners who were invited to participate, 254 completed the survey, giving a participation rate of 52.6%. Nurse practitioners who did not complete the survey included 122 who had no response or who responded after the survey ended, 12 who did not complete the entire survey, 10 who did not meet screening criteria, and 33 who were terminated because of filled quotas.
The survey contained 113 items in all. Two questions were related to HBPM. First, PCPs were asked, “For what percentage of your hypertensive patients do you recommend a home blood pressure monitoring kit?” and were given a choice of responses (0%, 10%, 20%, 30%, 40%, 50%, 60%, 70%, 80%, 90%, and 100%). If they chose 100%, they skipped the next question. If they chose a value <100%, they were asked, “When you do not recommend home blood pressure monitoring kits, what is typically the main reason(s)? Select all that apply,” and were given the following choices: “patient won't use it,” “patient won't use it correctly,” “patient can't afford it,” “home kits not reliable,” “patient doesn't need it,” and “other reason.” We divided their responses according to the percentage of patients for whom they recommended HBPM: ≤40% (low), 50% to 80% (medium), and ≥90% (high).
Sociodemographic characteristics of the PCPs included their age, sex, and race/ethnicity. Height and weight were also recorded, which allowed calculation of their body mass index (BMI; kg/m2). BMI was categorized as underweight and normal weight (≤24), overweight (25.0–29.9), and obese (≥30) (http://www.ncbi.nlm.nih.gov/books/NBK2004/). The mean BMI was 25.7; two BMIs were excluded (one because of extremely low weight of 58 lb for a 5′11″ person [BMI=8.1] and one because of extremely high weight of 380 lb for a 5′5″ person [BMI=63.2]). Lifestyle behaviors such as number of days per week eating ≥5 cups of fruits and vegetables; smoking cigars, cigarettes, or pipes; and number of days exercising at an elevated heart rate for ≥30 minutes were also recorded. Characteristics related to PCPs' practices included specialty, financial situation of most of their patients, and main work setting.
The PCPs' self‐report of their CME was also a component of the survey. They were offered 5 choices ranging from “never” to “always” asking about how often they use certain sources for CME, including Internet, conferences, journals, government agencies, classes, CD‐ROMs, and medical podcasts. If they chose “always” as a response to a source, they were placed into the “always” group while the rest of the answers were placed into another group. The survey also asked how many hours per week they spent on the Internet for work‐related reasons. Two survey items revealed the providers' attitudes and opinions about their patients. First, they were asked to rate how much they agreed or disagreed with the following statement: “My patients are knowledgeable when it comes to health‐related issues.” Then, they were asked to rate this statement on the same scale: “I value the health‐related information from my patients.”
Statistical analysis was performed by using SAS software (version 9.2; SAS Institute, Inc, Cary, NC). Chi‐square tests were performed to determine differences among the groups according to the percent recommendation using a P value of <.05. Multivariate logistic regression was performed and variables with a P value <.1 in the univariate analyses were included in the model. We calculated odds ratios (ORs) and 95% confidence intervals (CIs) for likelihood of PCPs' recommending HBPM to ≥90% of their patients. Variables included in the model were sex, specialty, fruit and vegetable consumption, financial status of their patients, use of CME, whether they thought their patients were knowledgeable, and whether they valued their patients' health‐related information.
Results
Demographic and health‐related behavioral information for the 1254 PCPs who completed the survey is provided in Table 1. The mean age was 45.5 years and 56% of respondents were men. A majority of PCPs classified themselves as non‐Hispanic white (74%) followed by non‐Hispanic Asian (15%), other (4%), non‐Hispanic black (3%), and Hispanic (3%). A total of 48% of PCPs were underweight or of normal weight, 38% were overweight, and 14% were obese. Nearly all (96%) were nonsmokers. Regarding work setting, 42% had privileges at a teaching hospital and 61% worked in a group practice. Journals and the Internet were used most often as sources for CME. Of the PCPs, 16% “always” used journals, 16% “always” used the Internet, and 8% “always” attended conferences (Table 1).
Table 1.
Proportion of Primary Care Providers Who Recommend HBPM, by Demographic and Health Characteristics—DocStyles, 2010
| No. (%) | Proportion (%) of Patients Given HBPM Recommendation | ||||
|---|---|---|---|---|---|
| ≤40% | 50–80% | ≥90% | P Value | ||
| (n=327) | (n=521) | (n=40) | |||
| Total | 1254 | 26 | 42 | 32 | |
| Age, y | .9463 | ||||
| <40 | 404 (32) | 32 | 32 | 33 | |
| 40–50 | 459 (37) | 38 | 36 | 36 | |
| >50 | 391 (31) | 30 | 32 | 31 | |
| Sex | .0527 | ||||
| Male | 705 (56) | 56 | 60 | 52 | |
| Female | 549 (44) | 44 | 40 | 48 | |
| Race/ethnicity | .2051 | ||||
| Non‐Hispanic white | 933 (74) | 71 | 76 | 75 | |
| Non‐Hispanic black | 43 (3) | 6 | 2 | 3 | |
| Hispanic | 42 (3) | 3 | 4 | 3 | |
| Asian/Pacific Islander | 191 (15) | 17 | 15 | 15 | |
| Other race | 45 (4) | 4 | 3 | 4 | |
| Body mass index, kg/m2 | .3724 | ||||
| Underweight or normal weight (≤24.9) | 599 (48) | 46 | 49 | 50 | |
| Overweight (25.0–29.9) | 472 (38) | 36 | 38 | 36 | |
| Obese (≥30) | 181 (14) | 17 | 13 | 14 | |
| Days per week eat ≥5 cups fruit or vegetables | .0035 | ||||
| 0 | 109 (9) | 11 | 7 | 10 | |
| 1–3 | 457 (36) | 40 | 40 | 30 | |
| 4–6 | 490 (39) | 33 | 40 | 43 | |
| 7 | 198 (16) | 16 | 14 | 18 | |
| Days per week smoke cigarettes, cigars, or pipes | .8677 | ||||
| 0 | 1199 (96) | 95 | 95 | 96 | |
| 1 or more | 55 (4) | 5 | 5 | 4 | |
| Days per week exercise or keep heart rate up ≥30 minutes | .2810 | ||||
| 0 | 113 (9) | 10 | 7 | 11 | |
| 1–3 | 585 (47) | 50 | 47 | 44 | |
| 4–6 | 462 (37) | 32 | 39 | 37 | |
| 7 | 94 (7) | 8 | 7 | 8 | |
| Main work setting,% | .0066 | ||||
| Individual practice | 216 (17) | 16 | 17 | 19 | |
| Group practice | 765 (61) | 55 | 63 | 63 | |
| Hospital or clinic | 273 (22) | 29 | 20 | 19 | |
| Years practicing medicine | .7498 | ||||
| <10 | 406 (32) | 35 | 31 | 32 | |
| 10–20 | 567 (45) | 43 | 47 | 45 | |
| Patients' financial status | .0012 | ||||
| Very poor–poor | 68 (5) | 9 | 5 | 3 | |
| Poor–lower middle class | 190 (15) | 19 | 15 | 13 | |
| Lower middle class–middle class | 529 (42) | 42 | 42 | 42 | |
| Middle class–upper middle class | 413 (33) | 28 | 34 | 36 | |
| Upper middle class–affluent | 54 (4) | 3 | 4 | 6 | |
| Continuing medical education | |||||
| Internet | .1434 | ||||
| Always | 197 (16) | 12 | 16 | 18 | |
| Conferences | .0991 | ||||
| Always | 97 (8) | 6 | 6 | 11 | |
| Journals | .0011 | ||||
| Always | 201 (16) | 14 | 15 | 19 | |
| Government agencies | .0089 | ||||
| Always | 61 (5) | 4 | 4 | 7 | |
| Classes | .0089 | ||||
| Always | 31 (2) | 2 | 2 | 4 | |
| CD‐ROM | .1757 | ||||
| Always | 20 (2) | 1 | 1 | 3 | |
| Medical podcast | .0009 | ||||
| Always | 25 (2) | 0 | 2 | 4 | |
Abbreviation: HBPM, home blood pressure monitoring.
We found that 26% of PCPs recommended HBPM to ≤40% of their hypertensive patients, 42% recommended it to 50% to 80% of patients, and 32% recommended it to ≥90% of patients. Of those who recommended HBPM to ≥90% of their patients, 45% were family physicians, 31% were internists, and 25% were nurse practitioners (data not shown).
Approximately 20% of PCPs ranked their patients' financial status as very poor to lower middle class. PCPs working in hospital‐ or clinic‐based practices were less likely to recommend HBPM to their patients than were those in individual or group practices. We did not find that the number of years practicing medicine was associated with recommending HBPM.
Figure 1 shows the proportion of PCPs recommending HBPM by specialty. The largest percentages of family (41%) and internal medicine (44%) physicians recommended HBPM to 50% to 80% of their patients. The largest percentage of nurse practitioners (40%) recommended HBPM to ≥90% of their patients.
Figure 1.
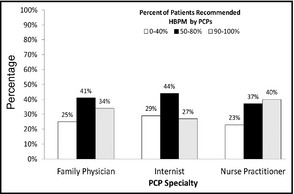
Primary care providers recommending home blood pressure monitoring (HBPM) for their hypertensive patients, by specialty—DocStyles, 2010. aBased on primary care provider (PCP) response to DocStyles 2010 survey question, “For what percentage of hypertensive patients do you recommend HBPM use?”
A total of 32% of PCPs recommended HBPM to 100% of their patients, leaving about two thirds of PCPs to choose reasons why they did not (Figure 2). Among PCPs who recommended HBPM 0% to 40% of the time, the two reasons chosen most often were “patient can't afford it” (43%) and “patient doesn't need it” (36%), significantly different from PCPs who recommended HBPM 50% to 80% and ≥90% of the time (P=.042 and .002, respectively). Other reasons why PCPs did not recommend HBPM were “patient won't use,” “home kits are not reliable,” and “other” (P=.011, .001, and .007, respectively).
Figure 2.
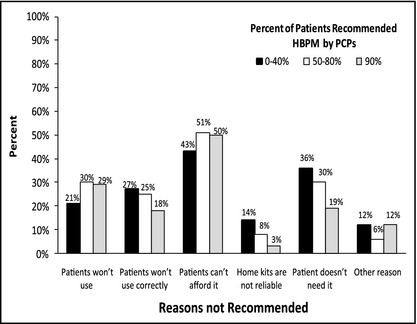
Reasons primary care providers (PCPs) did not recommend home blood pressure monitoring (HBPM)—DocStyles, 2010. aBased on PCP response to DocStyles 2010 survey question, “When you do not recommend home blood pressure monitoring kits, what is typically the main reason(s)? Select all that apply.”
Figure 3 shows the ORs of PCPs recommending HBPM to ≥90% of patients compared with those who recommended it less often, from 0% to 80%. Internists were significantly less likely to recommend HBPM to ≥90% of their patients than were nurse practitioners (OR, 0.55; 95% CI, 0.40–0.78). PCPs who ate 5 cups of fruits and vegetables from 1 to 3 days a week were significantly less likely to recommend HBPM (OR, 0.60; 95% CI, 0.38–0.95) than were those who did not eat this amount any day of the week. Compared with PCPs whose patients were in the very poor to poor category economically, those who stated that most of their patients were in the lower middle class to the middle class (OR, 2.14; 95% CI, 1.12–4.06), middle class to upper middle class (OR, 2.58; 95% CI, 1.35–4.93), and upper middle class to affluent (OR, 3.89; 95% CI, 1.70–8.88) were 2 to 3 times more likely to recommend HBPM to ≥90% of their patients. PCPs who selected “always” for one of the categories of CME sources were more likely to recommend HBPM to ≥90% of their patients than were those who did not. However, this did not reach significance in our model (OR, 1.28; 95% CI, 0.99–1.66).
Figure 3.
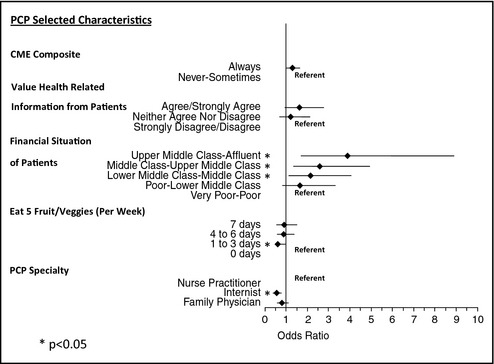
Odds ratios (95% confidence interval) of recommending home blood pressure monitoring, by selected characteristics of primary care providers (PCPs)—DocStyles, 2010. *P<.05. Continuing medical education (CME) is the continuing medical education through various ways such as conferences, online courses, seminars, etc.
Discussion
DocStyles 2010 is a nationwide survey used to collect information about the behavior and attitudes of PCPs. We used the data to understand the characteristics of PCPs related to their attitudes and advice regarding frequency of recommending HBPM. Our results showed that only about one third of PCPs recommended HBPM to ≥90% of their patients. Internists and PCPs with patients who were poor to very poor were less likely to recommend HBPM.
HBPM, as part of a hypertension management protocol, has been found to help improve BP control among patients for whom previous treatment had not achieved control.6 Additionally, since BP control is inadequate in the United States, with only half of patients' with well‐controlled BP,4, 5 it is important for PCPs to incorporate HBPM into the management of hypertension in their patients, which could improve control. Understandably, this is no small task for a busy PCP practice.
HBPM has been found to be beneficial in both diagnosing and treating patients with hypertension. A recent meta‐analysis has shown statistically significant drops in both systolic and diastolic BP as well as reduction in medications and better BP control in patients using HBPM compared with office BP monitoring.6 The many BP readings available from HBPM have been shown to be more reproducible than office‐based BP measurements. BP readings taken by patients at home tend to be lower than those taken at the doctor's office and are closer to the average BP recorded by 24‐hour ambulatory monitors; such frequent readings best predict cardiovascular risk.7 Perhaps most importantly, regular HBPM use can enhance evaluation of how well BP is being controlled in patients who are taking antihypertensive medications.6, 11, 12, 13, 14, 15
Our study shows many reasons why PCPs did not recommend HBPM, including cost of the devices and problems associated with their use. Cost is a barrier. Patients pay from $20 to $100 for a monitor with a regular‐sized cuff.16 About half of all users (those who are overweight or obese) would need to purchase a large‐sized cuff.12 PCPs would also have to provide adequate patient education on the proper use of the device to ensure accurate measurements, including regular use and appropriate timing.6, 7, 11, 12, 13, 14, 15 Patients should submit readings to PCPs every 3 months so that an average BP can be determined.12 Fortunately, in one study, HBPM led to less intensive antihypertensive drug treatment based on lowered diastolic BP measurements.13 The cost of medication for hypertension management ranges from $1700 to $3000 over 5 years, so lowering prescription costs by using home monitors in addition to visits to the doctor's office can save a great deal of money over the same period.7
Examining the reasons why PCPs choose not to recommend HBPM gives insight as to the barriers currently present. “Patient can't afford it” was the most frequently chosen reason and presents an opportunity for public health interventions and policy recommendations. Furthermore, recommendations in the Call to Action on Use and Reimbursement for Home Blood Pressure Monitoring for rebates or insurance reimbursements for HBPM equipment, although important, have not been widely followed.7 The second most frequently chosen reason PCPs did not recommend HBPM was, “patient doesn't need it.” Perhaps a high proportion of those PCPs' patients have well‐controlled hypertension. However, use of HBPM may still be helpful because HBPM has a stronger predictive value for both future cardiovascular events and total mortality than do office BP measurements.5
We found that CME, thinking that patients were knowledgeable about health‐related issues, and positively valuing health information from patients are important factors that might increase the likelihood of PCPs' recommending HBPM; however, these findings are not statistically significant. Evidence points to directly involving patients in their care as part of lifestyle interventions and HBPM provides evidence‐based care that informs both the provider and patient about the course of treatment.7
Limitations
This study has some limitations. First, the DocStyles PCP panel and data may not accurately represent PCPs in the United States, since participation in the survey was voluntary and PCPs who completed the survey were given an honorarium of $40 to $60. Thus, self‐selection bias is likely. Second, quotas were set for the types of PCPs included (eg, specialty, race/ethnicity, and age), which excluded some respondents. Third, the survey was Internet‐based, which requires Internet access and might bias respondent selection toward younger providers with greater technologic skills. Fourth, the survey contains self‐reported data, which are subject to overestimation of behaviors by respondents thought to be desirable. Fifth, PCPs were asked to choose from a certain set of values to whom they recommended HBPM use, which did not allow them to choose an exact percentage for their answer. Lastly, DocStyles 2010 has not been tested for reliability or validity; however, DocStyles 2010 has a large sample size and provides recent information pertaining to both viewpoints and activities of PCPs.
Conclusions
To our knowledge, there are no published reports on perceived attitudes of PCPs regarding HBPM recommendation. Although JNC 7 recommends that HBPM be used in the evaluation and treatment of patients with hypertension,1 a significant proportion of PCPs are not recommending its use to the majority of their patients. Knowledge of the attitudes of PCPs regarding HBPM can play an important role in the effort to control hypertension in Americans. Use of product rebates or insurance reimbursement for the cost of monitors are viable options in the future and likely would increase recommendations. Additional efforts are needed to provide education to providers, especially to internists and family physicians, about the benefits of HBPM in improved and cost‐effective BP control in the United States.
Disclosures
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
J Clin Hypertens (Greenwich). 2013;00:00–00© 2013 Wiley Periodicals, Inc.
References
- 1. Chobanian AV, Bakris GL, Black HR, et al. The Seventh Report of the Joint National Committee on Prevention, Detection, and Treatment of High Blood Pressure. Hypertension. 2003;42:1206–1252. [DOI] [PubMed] [Google Scholar]
- 2. US Department of Health and Human Services . Seventh Report of the Joint National Committee on Prevention, Detection, and Treatment of High Blood Pressure. Bethesda, MD: National Institutes of Health; 2004. NIH Publication No. 04‐5230. [Google Scholar]
- 3. Egan BM, Zhao Y, Axon RN. US trends in prevalence, awareness, treatment and control of hypertension, 1998–2008. JAMA. 2010;303:2043–2050. [DOI] [PubMed] [Google Scholar]
- 4. Gillespie C, Kuklina EV, Briss PA, et al. Vital signs: prevalence, treatment and control of hypertension – United States, 1999–2002 and 2005–2008. MMWR Morb Mortal Wkly Rep. 2011;60:103–108. [PubMed] [Google Scholar]
- 5. Niiranen TJ, Hanninen MR, Johansson J, et al. Home‐measured blood pressure is a stronger predictor of cardiovascular risk than office blood pressure: the Finn‐Home study. Hypertension. 2010;55:1346–1351. [DOI] [PubMed] [Google Scholar]
- 6. Agarwal R, Bills JE, Hecht TJW, Light RP. Role of home blood pressure monitoring in overcoming therapeutic inertia and improving hypertension control: a systemic review and meta‐analysis. Hypertension. 2011;57:29–38. [DOI] [PubMed] [Google Scholar]
- 7. Pickering TG, Miller NH, Ogedegbe G, et al. Call to action on use and reimbursement for home blood pressure monitoring: executive summary: a joint scientific statement from the American Heart Association, American Society of Hypertension, and Preventative Cardiovascular Nurses Association. Hypertension. 2008;52:1–9. [DOI] [PubMed] [Google Scholar]
- 8. Ayala C, Tong X, Keenan NL. Regular use of home blood pressure monitors by hypertensive adults – healthstyles, 2005 and 2008. J Clin Hypertens. 2012;14:172–177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Viera AJ, Cohen LW, Mitchell CM, Sloane PD. High blood pressure knowledge among primary care patients with known hypertension: a North Carolina family medicine research network (NC‐FM‐RN) study. J Am Board Fam Med. 2008;21:300–308. [DOI] [PubMed] [Google Scholar]
- 10. Kreuter MW, Chedda SG, Bull FG. How does physician advice influence patient behavior? Evidence for a priming effect. Arch Fam Med. 2000;9:426–433. [DOI] [PubMed] [Google Scholar]
- 11. Pickering TG, White WB. When and how to use self (home) and ambulatory blood pressure monitoring. J Am Soc Hypertens. 2010;4:56–61. [DOI] [PubMed] [Google Scholar]
- 12. NHLBI Obesity Education Initiative Expert Panel on the Identification, Evaluation, and Treatment of Obesity in Adults (US). Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults: The Evidence Report. Bethesda (MD): National Heart, Lung, and Blood Institute; 1998. Sep. Chapter 4, Treatment Guidelines. http://www.ncbi.nlm.nih.gov/books/NBK2004/. Accessed October 15, 2011. [Google Scholar]
- 13. Staessen JA, Hond ED, Celis H, et al. Antihypertensive treatment based on blood pressure measurement at home or in the physician's office: a randomized controlled trial. JAMA. 2004;291:955–964. [DOI] [PubMed] [Google Scholar]
- 14. Mancia G, Parati G. Home blood pressure monitoring: a tool for better hypertension control. Hypertension. 2011;57:21–23. [DOI] [PubMed] [Google Scholar]
- 15. Parati G, Stergiou GS, Asmar R, et al. European Society of Hypertension practice guidelines for home blood pressure monitoring. J Hum Hypertens. 2010;24:779–85. [DOI] [PubMed] [Google Scholar]
- 16. Mayo Clinic . Get the most out of home blood pressure monitoring. http://www.mayoclinic.com/health/high-blood-pressure/HI00016/NSECTIONGROUP=2/. Accessed February 12, 2012.


