Abstract
Objectives:
Posttraumatic stress disorder (PTSD) and substance use disorders are highly comorbid. Effective treatments are largely lacking. This pilot study evaluated the safety and feasibility of a novel intervention, Concurrent Treatment of PTSD and Substance Use Disorders Using Prolonged Exposure (COPE), in preparation for a randomized controlled trial.
Methods:
Twenty-two treatment-seeking women with current DSM-IV-TR PTSD and alcohol dependence (AD) were recruited. Participants received COPE. Safety and feasibility were evaluated, as were efficacy-related outcomes: PTSD and depression symptom severity, alcohol use, craving, and dependence severity.
Results:
No adverse events occurred. COPE was implemented in routine clinical practice. Among the assessed women, 95.8% were eligible to participate. Treatment attendance and completion were higher than in previous studies. Post treatment, all efficacy-related outcomes, including PTSD and depression symptom severity, alcohol use, craving, and dependence severity, were significantly reduced.
Conclusions:
COPE was safe and feasible to use. Concerns that trauma-focused, exposure-based therapy might promote relapse in this population appear unwarranted. Our findings provide initial evidence suggestive of COPE efficacy for comorbid PTSD and AD in women. These results provide a strong rationale for investigating the efficacy of COPE for comorbid PTSD and AD in women in a randomized controlled trial.
Keywords: alcohol dependence, alcohol use disorder, integrated treatment, PTSD, women
Posttraumatic stress disorder (PTSD) is a debilitating condition characterized by re-experiencing a traumatic event, avoiding trauma-associated stimuli, numbing of general responsiveness and increased arousal, and post trauma (DSM-IV-TR) (American Psychiatric Association, 2000). Lifetime PTSD prevalence has been estimated to be 4.8% to 6.1% in the United States (Blanco et al., 2013; Goldstein et al., 2016), and 5.6% in Sweden (Frans et al., 2005). It is approximately twice as high in women as in men in both countries (Frans et al., 2005; Blanco et al., 2013; Goldstein et al., 2016).
Posttraumatic stress disorder and substance use disorder (SUD) frequently co-occur (Kessler et al., 1995). SUD is a condition where an individual continues to use a substance despite significant substance-related problems (American Psychiatric Association, 2000). SUD is characterized by tolerance, withdrawal, and greater substance use than intended, among other aspects (American Psychiatric Association, 2000).
Posttraumatic stress disorder is an established risk factor for alcohol use disorder (AUD) (Haller and Chassin, 2014; Kline et al., 2014; Walsh et al., 2014), and is highly comorbid with AUD (Blanco et al., 2013). The association between PTSD and alcohol dependence (AD) is stronger for women than for men (Berenz et al., 2016). There are currently no Swedish data on PTSD and AUD comorbidity. Among patients seeking treatment for SUD, from 30% to more than 60% also have PTSD (McCauley et al., 2012). Individuals with PTSD and SUD tend to have poorer treatment outcomes than those without the same comorbidity (Berenz and Coffey, 2012), whereas individuals with PTSD and AUD have more severe PTSD and AUD and a higher prevalence of suicide attempts than those with just 1 of the disorders (Blanco et al., 2013). Improvements in PTSD have been shown to have a greater impact on AUD than vice versa (Back et al., 2006).
Patients with PTSD and SUD are typically offered treatment for SUD first (van Dam et al., 2012). Swedish standard clinical practice mimics this: patients first receive treatment for their SUD. They are then required to achieve sobriety, before they are offered PTSD treatment, normally through referral to a different care provider. This strategy is not consistent with research, indicating that PTSD and SUD should be treated in an integrated manner (McCarthy and Petrakis, 2010; Roberts et al., 2015).
Few studies have evaluated pharmacological treatment of PTSD and comorbid SUD, and none of them have shown results supporting efficacy of the respective intervention (Berenz and Coffey, 2012). When it comes to psychological treatment, there is very little evidence to support the use of nontrauma-focused psychological interventions for PTSD and comorbid SUD (van Dam et al., 2012; Roberts et al., 2015). Reviews have found trauma-focused psychological treatment, with exposure-based interventions the most promising (Berenz and Coffey, 2012; van Dam et al., 2012), and integrated psychosocial treatments and combined psychosocial and pharmacological approaches encouraging (Flanagan et al., 2016). A recent meta-analysis found that traumafocused psychological treatment given alongside interventions for SUD reduced both PTSD symptom severity and substance use at 5 to 7 months of follow-up (Roberts et al., 2015). Yet, a common concern limiting the use of traumafocused psychological treatment in patients with PTSD and comorbid SUD is that exposure to trauma-associated stimuli might trigger relapse or result in increased substance use (Riggs et al., 2003; Becker et al., 2004).
Concurrent Treatment of PTSD and SUDs using Prolonged Exposure (COPE) is a manual-based form of traumafocused cognitive behavioral therapy (CBT) with exposure to concurrently address PTSD and SUD (Killeen et al., 2011; Mills et al., 2012; Back et al., 2015). COPE is based on evidence-based treatments for the disorders it targets: prolonged exposure (PE) for PTSD (Foa et al., 2013); and relapse prevention for SUD (Carroll, 1998). COPE includes 3 key elements: psychoeducation on PTSD and SUD, and how they interact; prolonged imaginal exposure and in vivo exposure to trauma-associated stimuli for PTSD; and relapse prevention for SUD. All COPE sessions address both PTSD and SUD in an integrated fashion. Invivo exposure is typically included in sessions 3 to 11, and imaginal exposure in sessions 4 to 11. COPE consists of 12 sessions (Back et al., 2015). Treatment goals pertaining to both PTSD and SUD are defined in collaboration with the patient. Abstinence is recommended throughout the treatment, but goals can also be reductions in substance use.
Concurrent Treatment of PTSD and SUDs using Prolonged Exposure has been shown to reduce PTSD symptom severity without increasing substance use in an Australian population where most participants were polysubstance drug users and unemployed (Mills et al., 2012).
Here, we introduced COPE in Sweden, and conducted a pilot study to evaluate its safety and feasibility in a sample of women with current DSM-IV-TR PTSD and AD, but without current illicit drug abuse or dependence (American Psychiatric Association, 2000), where most participants were employed. This is warranted as: AUD is highly prevalent (Grant et al., 2015); more research on the treatment of comorbid PTSD and AUD is needed (Ralevski et al., 2014); and apart from a case report (Back et al., 2012), there are no prior data on how COPE will perform in this group. COPE has not previously been tested in the Swedish healthcare system. We hypothesized that COPE would be safe and its implementation feasible in regular Swedish clinical practice. Reductions in PTSD and depression symptom severity, and alcohol consumption were hypothesized to follow treatment completion, as in the earlier case report (Back et al., 2012), as were reductions in alcohol craving and dependence severity.
METHODS
The study was approved by the Stockholm Regional Ethics Review Board, and conducted at a Karolinska Institute affiliated outpatient unit providing treatment for women with AUD. Patients seeking treatment at the unit were offered evaluation using the Structured Clinical Interview for DSM Diagnosis (SCID-I) (First et al., 1996) and the Life Events Checklist (LEC) (Gray et al., 2004; Paunovic and Ost, 2005), administered by a psychiatrist or clinical psychologist. Approximately 50% of those seeking treatment at the unit have current PTSD. Participants were recruited among treatment-seeking patients. Inclusion criteria were DSM-IV-TR current diagnoses of PTSD and AD (American Psychiatric Association, 2000). Exclusion criteria were current suicidal ideation with a high risk of self-harm or suicide, current psychotic disorder, insufficient memory of the index trauma, dissociation which affected the patient more than her PTSD, living under threat of violence or currently in a violent relationship, and a current SUD other than alcohol or nicotine. Eligible subjects were given verbal and written information about the study and provided written informed consent. After inclusion, demographic data were collected and participants underwent additional assessment.
The Clinician-Administered PTSD Scale—Diagnostic Version (CAPS-DX), a structured interview that corresponds to the DSM-IV-TR criteria for PTSD, was used to assess PTSD symptom severity (range 0–136, higher scores indicate more severe PTSD) (Weathers et al., 2001; Paunovic and Ost, 2005). CAPS-DX was administered at baseline and 1 week after COPE session 12. The Alcohol Use Disorder Identification Test (AUDIT) (Saunders et al., 1993) can be used to assess the severity of AD (Donovan et al., 2006), and was so at baseline and 1 week after COPE session 12. The Drug Use Disorder Identification Test (DUDIT) was used at baseline to assess drug use (Berman et al., 2005). The suicidality section of the MINI International Neuropsychiatric Interview (MINI) was used at baseline and 1 week after COPE session 12 (Sheehan et al., 1998). Four instruments were administered at baseline, before each COPE session, 1 week, and 1 month after COPE session 12: the PTSD Checklist—Civilian Version (PCL-C) (Blanchard et al., 1996); the Time-Line Follow-Back (TLFB) (Sobell et al., 1979); the Penn Alcohol Craving Scale (PACS) (Flannery et al., 1999); and the Beck Depression Inventory—Second Edition (BDI-II) (Beck et al., 1996). The PTSD Checklist—Civilian Version (PCL-C) is a standardized self-report rating scale comprising 17 items that correspond to diagnostic criteria for PTSD (range 17–85, higher scores indicate more severe symptoms) (Blanchard et al., 1996). Time-Line Follow-Back (TLFB) was used to obtain quantitative drinking measures (Sobell et al., 1979). TLFB uses self-report to obtain estimates of daily drinking. Grams of alcohol consumed per week and percent heavy drinking days during the assessed time frame (at baseline: the preceding 90 days, and at each session and follow-up: the time since the last visit) were derived from the TLFB. Heavy drinking days were defined as days when a female consumes more alcohol than that in 3 standard drinks, each containing 14grams of alcohol. The Penn Alcohol Craving Scale (PACS) is a 5-item self-report scale to assess alcohol craving in the preceding week (range 0–30, higher scores indicate more severe craving) (Flannery et al., 1999). The Beck Depression Inventory—Second Edition (BDI-II) is a rating scale for severity of depressive symptoms (range 0–63, higher scores indicate more severe depression) (Beck et al., 1996). At follow-up 1 week after COPE session 12, participants were asked whether they had been exposed to any additional trauma. Participants who did not complete all 12 COPE sessions were not asked to follow-ups.
Patients received COPE (Killeen et al., 2011; Mills et al., 2012; Back et al., 2015), that is, twelve 90-minute sessions, typically delivered weekly, but with flexibility allowed to accommodate patient schedules or missed sessions. No limit for treatment duration, that is, how many weeks the sessions could be spread over, was set, as we had not noted such limits in previous studies (Mills et al., 2012; Foa et al., 2013), and this was a pilot study to test COPE in Swedish clinical practice. Patient goals pertaining to AD included abstinence and controlled drinking. A clinical psychologist trained in CBT, PE, and COPE delivered COPE. The psychologist received supervision for the duration of the study. Participants were also offered standard treatment for AD, that is, nonspecific psychosocial treatment for AUD, outpatient counseling, motivational interviewing (MI), relapse prevention, and biofeedback, at the unit, in parallel with COPE. In addition, participants could access any type of psychiatric and SUD treatment available, including outpatient counseling, inpatient or outpatient detoxification, residential rehabilitation, and pharmacotherapies.
Statistical analyses were conducted using repeated measures general linear models in Statistica Version 13 (Tulsa, OK). For the majority of outcomes (PCL-C, BDI-II, TLFB, and PACS), the within-subject factor included 4 time points: baseline (pretreatment), session 12, 1-week follow-up, and 1-month follow-up. For the CAPS-DX and AUDIT measures, the within-subject factor included the pretreatment and 1-week follow-up time points. Missing data were imputed (last observation carried backward for a single rating at baseline, last observation carried forward for all others), and intention-to-treat analyses were conducted. Significance was set at P<.05 for all models. Cohen dz was calculated by hand. Treatment completion was defined as completing all 12 COPE sessions, and noncompletion as completing fewer than 12 sessions. Baseline differences between completers and noncompleters were examined using t tests for continuous variables and chi-square-tests for categorical variables.
Safety and Feasibility
Safety was defined as no adverse events occurring during study participation. Adverse events were defined as increased reported suicidality and alcohol relapses, that is drinking equal or larger amounts of alcohol as when the AUD was most problematic, according to participant self-report.
Good feasibility was defined as COPE being provided in the Swedish healthcare system by existing staff, with adequate training and supervision (Back et al., 2015); a majority (>85%) of outpatients with PTSD and AUD being eligible for participation; and treatment attendance and completion rates similar to those previously reported (Mills et al., 2012; Roberts et al., 2015).
RESULTS
Sample Recruitment and Retention
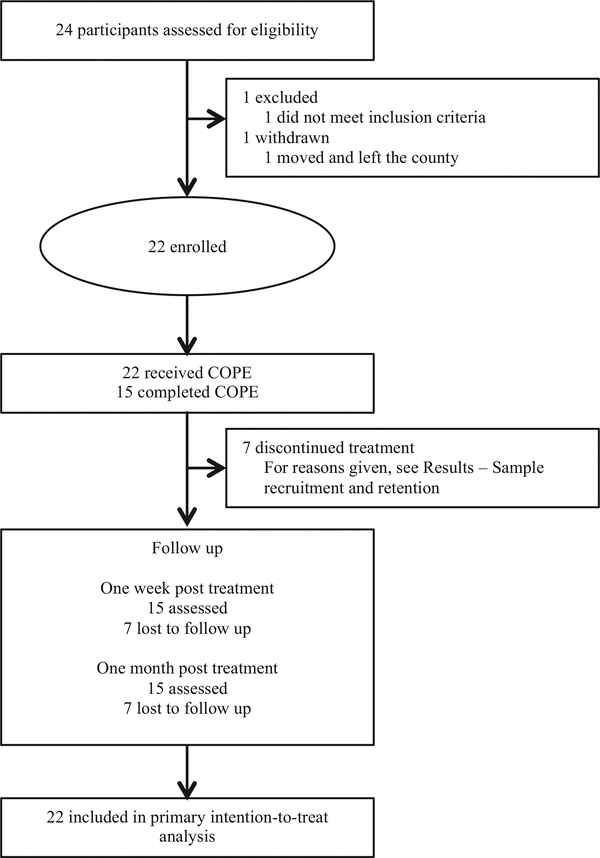
Twenty-four individuals were assessed, and 23 of these were eligible to participate (Fig. 1). An exclusion was due to not meeting diagnostic criteria for current PTSD and a withdrawal to a move to another part of the country. The remaining individuals (n=22) all chose to participate in the study. Of the participants included, 15 (68.2%) completed all 12 sessions ofCOPE. All 15 completers came to both follow-ups (Fig. 1).
FIGURE 1.
Study flow.
Those who discontinued treatment did so after 2 to 10 sessions (M=5.4 sessions, S=3.6). They did so for different reasons: 4 patients citing that they were happy with the results achieved and felt they did not need more treatment (4 of 7 [57.1%]), 1 because of a report to social services, in accordance with Swedish legislation (1 of 7 [14.3%]), 1 because COPE was felt to be too anxiety-provoking (1 of 7 [14.3%]), and 1 for unknown reasons, although COPE-related anxiety was denied (1 of 7 [14.3%]). They did not complete followup assessments.
There were no significant differences between completers and noncompleters on any of the baseline characteristics, including demographics, trauma history, psychiatric health, and AD (Table 1). However, the statistical analyses may have been underpowered to detect differences.
Table 1.
Baseline Characteristics
| All Participants | Completers (12 Sessions) | Noncompleters (<12 Sessions) | |
|---|---|---|---|
| Number (%) | |||
| Characteristics | (n = 22) | (n = 15) | (n = 7) |
| Demographic | |||
| Age, mean (SD) | 45.5 (10.4) | 45.8 (11.8) | 45.0 (7.3) |
| Secondary school completed | 22 (100) | 15 (100) | 7 (100) |
| Tertiary education completed | 13 (59.1) | 8 (53.3) | 5 (71.4) |
| Employed | 16 (72.7) | 9 (60.0) | 7 (100) |
| Single | 17 (77.3) | 12 (80.0) | 5 (71.4) |
| Trauma history | |||
| Type of index trauma | |||
| Physical assault | 3 (13.6) | 2 (13.3) | 1 (14.3) |
| Witnessed injury or death | 4 (18.2) | 2 (13.3) | 2 (28.6) |
| Sexual assault | 8 (36.4) | 5 (33.3) | 3 (42.9) |
| Accident or disaster | 2 (9.1) | 2 (13.3) | 0(0) |
| Other | 5 (22.7) | 4 (26.7) | 1 (14.3) |
| Number of trauma types experienced, mean (SD) | 7.3 (2.6) | 7.9 (2.7) | 6.0 (2.1) |
| Number of traumas experienced, mean (SD) | 10.5 (5.3) | 11.5 (5.7) | 8.3 (4.1) |
| Age at first trauma, mean (SD), yrs | 9.0 (5.7) | 9.2 (5.1) | 8.7 (7.1) |
| Time since index trauma, mean (SD), yrs | 22.0 (16.4) | 19.3 (16.0) | 28.0 (17.0) |
| Experienced trauma during childhood | 20 (90.9) | 14 (93.3) | 6 (85.7) |
| Experienced sexual abuse during childhood | 10 (45.5) | 7 (46.7) | 3 (42.9) |
| PTSD | |||
| Delayed onset | 10 (45.5) | 7 (46.7) | 3 (42.9) |
| Duration of trauma symptoms, mean (SD), yrs | 20.9 (15.8) | 22.2 (15.5) | 18.1 (17.2) |
| Other mental health history | |||
| Current psychiatric axis I comorbidity, in addition to PTSD and alcohol dependence Attempted suicide | 19 (86.4) | 13 (86.7) | 6 (85.7) |
| Attempted suicide | |||
| Lifetime | 10 (45.5) | 8 (53.3) | 2 (28.9) |
| Past year | 3 (13.6) | 1 (6.7) | 2 (28.9) |
Completers attended all 12 session; noncompleters attended fewer than 12 sessions. There were no significant differences between completers and noncompleters on any of the baseline characteristics. However, the statistical analyses may have been underpowered to detect differences
Treatment Exposure
All 22 participants attended at least 2 COPE sessions. The mean number of sessions attended was 9.9 (SD=3.4). Twenty-one participants (95.5%) attended sessions that included in vivo (21 [95.5%]) or imaginal exposure (21 [95.5%]), and 15 participants (68.2%) attended all 12 sessions. The 12 sessions of COPE were delivered over 14 to 44 weeks (M=23.1, median=20, SD=8.7).
All but 1 participant were enrolled in standard SUD treatment at the time of study enrollment. The majority continued to receive standard treatment in parallel with COPE, at least during part of the COPE treatment, with nonspecific psychosocial treatment for AUD being the most common intervention. Pharmacological treatment for psychiatric comorbidity was prescribed for some of the participants. Nine of the subjects (40.9%) received disulfiram or naltrexone prescriptions for part of their COPE treatment duration.
Safety and Feasibility
No adverse events were encountered during study participation. There were no reports of increased suicidality during treatment, or, for completers, the week after it. There were no reported relapses to drinking equal or larger amounts than when the AUD was most problematic, according to patient self-reports. All but 1 patient who discontinued COPE stayed in contact with the unit, and any adverse events postCOPE would have been captured, but none was noted.
Concurrent Treatment of PTSD and SUDs using Prolonged Exposure was provided in the Swedish healthcare system by existing staff, with adequate training and supervision (Back et al., 2015). Of the assessed patients with PTSD and AUD, 95.8% were eligible to participate. Treatment attendance was 1.98 times as high and treatment completion 3.79 times as high as in a previously reported trial (Mills et al., 2012). Furthermore, treatment attendance (mean number of sessions attended 9.9, and proportion of available sessions attended 82.6%) was higher, and the completion rate at the upper end of those reported in a recent meta-analysis of psychological interventions for PTSD and comorbid SUD, where varying definitions of treatment completion were used (Roberts et al., 2015).
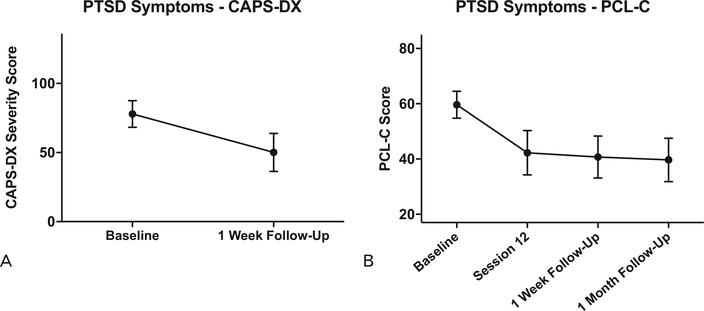
PTSD Outcomes
There was a significant reduction in PTSD symptom severity from baseline to follow-up. Clinician-rated PTSD symptom severity (CAPS-DX) was significantly reduced after treatment (F [1, 21]=29.6, P<0.001, Cohen dz=1.16; Fig. 2A), as was self-rated symptom severity (PCL-C) (F [3, 63]=23.9, P<0.001, Cohen dz=1.19; Fig. 2B.). Ten (66.7%) of the 15 completers no longer filled the diagnostic criteria for PTSD at the 1-week follow-up. Depression symptom severity (BDI-II) was also significantly reduced (F [3, 63]=14.2, P<0.001, Cohen dz=0.96).
FIGURE 2.
Group means and 95% confidence intervals for (A) clinician-rated PTSD symptom severity (CAPS-DX) and (B) participant self-rated PTSD symptom severity (PCL-C) (n=22).
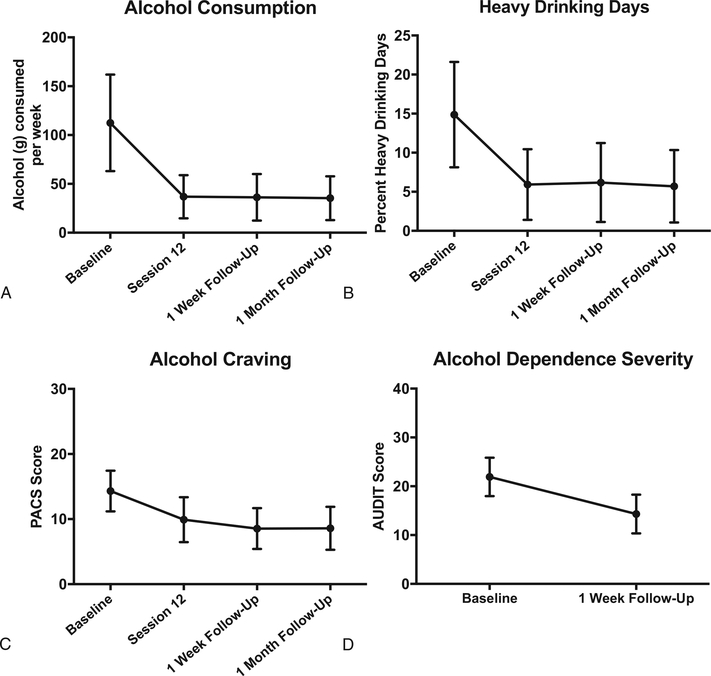
Alcohol Outcomes
Alcohol consumption (TLFB) was significantly reduced (F [3, 63]=12.2, P<0.001, Cohen dz=0.75; Fig. 3A), as was the percentage of heavy drinking days (F [3, 63]=7.4, P<0.001, Cohen dz=0.66; Fig. 3B). Alcohol craving (PACS) was also significantly reduced (F [3, 63]=6.7, P<0.001, Cohen dz=0.63; Fig. 3C). AD severity (AUDIT) was also markedly reduced (F [1, 21]=13.6, P<0.001, Cohen dz=0.79; Fig. 3D).
FIGURE 3.
Group means and 95% confidence intervals for (A) grams of alcohol consumed per week (TLFB), (B) percent heavy drinking days, (C) alcohol craving (PACS), and (D) alcohol dependence severity (AUDIT) (n=22).
DISCUSSION
Posttraumatic stress disorder comorbidity is highly prevalent among individuals seeking treatment for SUD (McCauley et al., 2012). More research on treatment for comorbid PTSD and SUD is needed (Berenz and Coffey, 2012; van Dam et al., 2012; Ralevski et al., 2014; Roberts et al., 2015). Here, we gave COPE, a manual-based type of integrated trauma-focused CBT for PTSD and SUD (Back et al., 2015), at an outpatient unit for women with AUD in Sweden, and evaluated its safety and feasibility. Our data support the safety of COPE in women with comorbid PTSD and AD, as no adverse events (ie, increased suicidality or alcohol relapses, which means drinking equal or larger amounts of alcohol as when the AUD was most problematic) were observed throughout the duration of the study. Such adverse events were also absent among those who discontinued COPE, but remained in contact with the unit, where any adverse events would have been captured. These observations are in agreement with previously published findings (Killeen et al., 2011; Mills et al., 2012). Together with a recent review (Flanagan et al., 2016), these data should allay concerns that trauma-focused psychological treatment with exposure for PTSD promotes substance use and relapse (Riggs et al., 2003; Becker et al., 2004). Thus, these observations pave theway for research on, and implementation of, integrated exposurebased treatment for comorbid PTSD and SUD.
Providing COPE in the Swedish public healthcare system was deemed feasible. COPE was provided by existing staff, with adequate training and supervision (Back et al., 2015). The vast majority of patients with PTSD and AUD (95.8%) were eligible to participate in the study. Treatment attendance and completion were higher than in a previous trial (Mills et al., 2012), probably due to a higher level of functioning among the patients in this pilot study. Furthermore, treatment attendance was higher, and completion rates at the upper end of the range reported in a recent meta-analysis of psychological interventions for PTSD and comorbid SUD (Roberts et al., 2015), even when strict criteria of treatment completion, that is, attending all 12 COPE sessions, were applied. The completion rate was around 70%. Attrition did not appear to be systematic, as dropouts did not differ from completers on a wide range of baseline characteristics. However, due to the small sample size, the statistical power to detect differences is limited and undetected differences may exist.
Limitations
Because our study was primarily designed to evaluate safety and feasibility, it had no control arm, and we can therefore not make definitive claims of efficacy or effectiveness. Despite its obvious limitations, our data provide suggestive initial evidence that COPE may improve PTSD and depression symptom severity, and also alcohol craving, consumption, and dependence severity in this clinical population, which has more severe PTSD and AUD (Blanco et al., 2013) and tends to have poorer treatment outcomes than those without the same comorbidity (Berenz and Coffey, 2012).
All patients took more than 12 weeks to complete treatment and no limit was set on over how long a period the treatment could stretch. The timeframe for treatment was likely longer than in a previously reported study, where 40% of patients were still receiving COPE after 3 months (Mills et al., 2012). Impairments associated with PTSD-SUD comorbidity may require a longer duration of time for treatment completion. Yet, in future studies, we will use a time limit.
The TLFB has been shown to be reliable in alcohol abusers (Sobell et al., 1979), and also psychiatric outpatients with severe mental illness (Carey et al., 2004). Using biomarkers of alcohol consumption, in addition to the TLFB, could, however, have strengthened this pilot study. The study could also have been strengthened by a longer followup period.
CONCLUSIONS
Concurrent Treatment of PTSD and SUDs using Prolonged Exposure is a safe and feasible treatment for treatmentseeking women with PTSD and AD in outpatient care. Our findings provide initial evidence suggestive of efficacy of this treatment for both PTSD and AD symptoms. Randomized controlled trials (RCTs) will be needed to conclusively establish efficacy and effectiveness. More research is warranted based on the present findings and the current literature on PTSD and comorbid SUD, highlighting the need for welldesigned studies and replication of those already conducted (van Dam et al., 2012; Ralevski et al., 2014; Roberts et al., 2015; Flanagan et al., 2016). Based on the data reported here, an RCT is underway.
ACKNOWLEDGMENTS
The authors thank The Swedish Society of Addiction Medicine, Systembolaget’s Alcohol Research Council, and the Söderström-Königska Foundation for grants funding this study.
Funding: The work summarized herein was funded by grants from The Swedish Society of Addiction Medicine, Systembolaget’s Alcohol Research Council, and the Söderström-Königska Foundation. The above had no involvement in study design, collection, analysis or interpretation of data, the writing of the report, or the decision to submit the article for publication.
Footnotes
Conflicts of interest: Professors Back, Killeen, and Brady are authors of the manual describing the intervention used in this study, and may receive royalties from its further sales. For the remaining authors none were declared.
REFERENCES
- American Psychiatric Association Diagnostic and statistical manual of mental disorders, 4th ed. Text rev. Washington DC: American Psychiatric Association Publishing; 2000. [Google Scholar]
- Back SE, Brady KT, Sonne SC, et al. Symptom improvement in co-occurring PTSD and alcohol dependence. J Nerv Ment Dis 2006;194:690–696. [DOI] [PubMed] [Google Scholar]
- Back SE, Killeen T, Foa EB, et al. Use of an integrated therapy with prolonged exposure to treat PTSD and comorbid alcohol dependence in an Iraq veteran. Am J Psychiatry 2012;169:688–691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Back SE, Foa EB, Killeen TK, et al. Concurrent Treatment of PTSD and Substance Use Disorders Using Prolonged Exposure (COPE) Therapist Guide. New York: Oxford University Press; 2015. [Google Scholar]
- Beck AT, Steer RA, Brown GK. Manual for the Beck Depression Inventory-II. San Antonio: Psychological Corporation; 1996. [Google Scholar]
- Becker CB, Zayfert C, Anderson E. A survey of psychologists’ attitudes towards and utilization of exposure therapy for PTSD. Behav Res Ther 2004;42:277–292. [DOI] [PubMed] [Google Scholar]
- Berenz EC, Coffey SF. Treatment of co-occurring posttraumatic stress disorder and substance use disorders. Curr Psychiatry Rep 2012;14:469–477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berenz EC, Roberson-Nay R, Latendresse SJ, et al. Posttraumatic stress disorder and alcohol dependence: epidemiology and order of onset. Psychol Trauma 2016. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berman AH, Bergman H, Palmstierna T, et al. Evaluation of the Drug Use Disorders Identification Test (DUDIT) in criminal justice and detoxification settings and in a Swedish population sample. Eur Addict Res 2005;11:22–31. [DOI] [PubMed] [Google Scholar]
- Blanchard EB, Jones-Alexander J, Buckley TC, et al. Psychometric properties of the PTSD checklist (PCL). Behav Res Ther 1996;34:669–673. [DOI] [PubMed] [Google Scholar]
- Blanco C, Xu Y, Brady K, et al. Comorbidity of posttraumatic stress disorder with alcohol dependence among US adults: results from National Epidemiological Survey on Alcohol and Related Conditions. Drug Alcohol Depend 2013;132:630–638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carey KB, Carey MP, Maisto SA, et al. Temporal stability of the timeline followback interview for alcohol and drug use with psychiatric outpatients. J Stud Alcohol 2004;65:774–781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carroll KM. A Cognitive-Behavioral Approach: Treating Cocaine Addiction. Rockville: National Institute on Drug Abuse; 1998. [Google Scholar]
- Donovan DM, Kivlahan DR, Doyle SR, et al. Concurrent validity of the Alcohol Use Disorders Identification Test (AUDIT) and AUDIT zones in defining levels of severity among out-patients with alcohol dependence in the COMBINE study. Addiction 2006;101:1696–1704. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, et al. Structured Clinical Interview for DSM-IVAxis I Disorders, Clinician Version (SCID-CV). Washington DC: American Psychiatric Press Inc; 1996. [Google Scholar]
- Flanagan JC, Korte KJ, Killeen TK, et al. Concurrent treatment of substance use and PTSD. Curr Psychiatry Rep 2016;18:70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flannery BA, Volpicelli JR, Pettinati HM. Psychometric properties of the Penn Alcohol Craving Scale. Alcohol Clin Exp Res 1999;23:1289–1295. [PubMed] [Google Scholar]
- Foa EB, Yusko DA, McLean CP, et al. Concurrent naltrexone and prolonged exposure therapy for patients with comorbid alcohol dependence and PTSD: a randomized clinical trial. JAMA 2013;310:488–495. [DOI] [PubMed] [Google Scholar]
- Frans Ö, Rimmo P-A, Åberg L, et al. Trauma exposure and post-traumatic stress disorder in the general population. Acta Psychiatr Scand 2005;111:291–299. [DOI] [PubMed] [Google Scholar]
- Goldstein RB, Smith SM, Chou SP, et al. The epidemiology of DSM-5 posttraumatic stress disorder in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions-III. Soc Psychiatry Psychiatr Epidemiol 2016;51:1137–1148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant BF, Goldstein RB, Saha TD, et al. Epidemiology of DSM-5 alcohol use disorder: results from the National Epidemiologic Survey on Alcohol and Related Conditions III. JAMA Psychiatry 2015;72:757–766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gray MJ, Litz BT, Hsu JL, et al. Psychometric properties of the life events checklist. Assessment 2004;11:330–341. [DOI] [PubMed] [Google Scholar]
- Haller M, Chassin L. Risk pathways among traumatic stress, posttraumatic stress disorder symptoms, and alcohol and drug problems: a test of four hypotheses. Psychol Addict Behav 2014;28:841–851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Sonnega A, Bromet E, et al. Posttraumatic stress disorder in the national comorbidity survey. Arch Gen Psychiatry 1995;52:1048–1060. [DOI] [PubMed] [Google Scholar]
- Killeen TK, Back SE, Brady KT. The use of exposure-based treatment among individuals with PTSD and co-occurring substance use disorders: clinical considerations. J Dual Diagn 2011;7:194–206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kline A, Weiner MD, Ciccone DS, et al. Increased risk of alcohol dependency in a cohort of National Guard troops with PTSD: a longitudinal study. J Psychiatr Res 2014;50:18–25. [DOI] [PubMed] [Google Scholar]
- McCarthy E, Petrakis I. Epidemiology and management of alcohol dependence in individuals with post-traumatic stress disorder. CNS Drugs 2010;24:997–1007. [DOI] [PubMed] [Google Scholar]
- McCauley JL, Killeen T, Gros DF, et al. Posttraumatic stress disorder and cooccurring substance use disorders: advances in assessment and treatment. Clin Psychol (New York) 2012;19 DOI: 10.1111/cpsp.12006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mills KL, Teesson M, Back SE, et al. Integrated exposure-based therapy for co-occurring posttraumatic stress disorder and substance dependence. A randomized controlled trial. JAMA 2012;308:690–699. [DOI] [PubMed] [Google Scholar]
- Paunovic N, Ost LG. Psychometric properties of a Swedish translation of the Clinician-Administered PTSD Scale-Diagnostic Version. J TraumaStress 2005;18:161–164. [DOI] [PubMed] [Google Scholar]
- Ralevski E, Olivera-Figueroa LA, Petrakis I. PTSD and comorbid AUD: a review of pharmacological and alternative treatment options. Subst Abuse Rehabil 2014;5:25–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riggs DS, Rukstalis M, Volpicelli JR, et al. Demographic and social adjustment characteristics of patients with comorbid posttraumatic stress disorder and alcohol dependence: potential pitfalls to PTSD treatment. Addict Behav 2003;28:1717–1730. [DOI] [PubMed] [Google Scholar]
- Roberts NP, Roberts PA, Jones N, et al. Psychological interventions for posttraumatic stress disorder and comorbid substance use disorder: a systematic review and meta-analysis. Clin Psychol Rev 2015;38:25–38. [DOI] [PubMed] [Google Scholar]
- Saunders JB, Aasland OG, Babor TF, et al. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO Collaborative Project on Early Detection of Persons with Harmful Alcohol Consumption: II. Addiction 1993;88:791–804. [DOI] [PubMed] [Google Scholar]
- Sheehan DV, Lecrubier Y, Sheehan KH, et al. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry 1998;59:22–33. quiz 34–57. [PubMed] [Google Scholar]
- Sobell LC, Maisto SA, Sobell MB, et al. Reliability of alcohol abusers’ selfreports of drinking behavior. BehavRes Ther 1979;17:157–160. [DOI] [PubMed] [Google Scholar]
- van Dam D, Vedel E, Ehring T, et al. Psychological treatments for concurrent posttraumatic stress disorder and substance use disorder: a systematic review. Clin Psychol Rev 2012;32:202–214. [DOI] [PubMed] [Google Scholar]
- Walsh K, Elliott JC, Shmulewitz D, et al. Trauma exposure, posttraumatic stress disorder and risk for alcohol, nicotine, and marijuana dependence in Israel. Compr Psychiatry 2014;55:621–630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weathers FW, Keane TM, Davidson JRT. Clinician-Administered PTSD scale: a review of the first ten years of research. Depress Anxiety 2001;13:132–156. [DOI] [PubMed] [Google Scholar]