Abstract
Objective:
To compare images from early and delayed phases of contrast-enhanced thoracic CT for assessing pleural thickening or nodules in a series of patients with malignant pleural effusions.
Methods:
Blinded images from 36 patients with malignant pleural effusions showing pleural lesions in both early (35 s delayed) and delayed (70 s delayed) phases of thoracic and abdominal contrast-enhanced CT scan were retrospectively assessed by six observers. First, images were individually scored in a six-point scale grading the quality of visualization of pleural findings such as pleural thickening or nodules. This was followed by a paired analysis, where the readers had to choose the one showing the highest quality between two images presented together corresponding to both phases of the same patient showing the same pleural lesion. When possible, contrast attenuation of the abnormal pleura was measured. Statistical analysis was performed by using paired t-test and χ 2.
Results:
Mean attenuation of pleural lesions was significantly higher in the delayed phase (76.0 ± 25.1 vs 57.5 ± 20.7, p < 0.001). Mean score and score of individual images was statistically significant better for the delayed phase for all observers. In the paired analysis, all the readers preferred the delayed phase over the early phase in 77.8 to 91.7% of the cases.
Conclusion:
Delayed phase of contrast-enhanced CT is preferable to early phase for evaluating pleural findings.
Advances in knowledge:
Pleural attenuation is greater for the delayed phase compared with the early phase of contrast-enhanced chest CT. In the pairwise comparison, all the observers prefer the delayed phase over the early phase for pleural evaluation.
Introduction
Contrast-enhanced CT of the chest and abdomen has an important role in the workup of patients with suspected malignant pleural effusion and in the routine evaluation of patients with malignancies metastatizing the pleura.
Although with variable sensitivity and specificity, characterization of a pleural effusion as malignant on CT is supported by the presence of pleural thickening or nodules,1–7 but an adequate contrast enhancement is required for a better delineation of those abnormalities in the pleural surfaces.
The introduction of multidetector CT technology has dramatically decreased scan time, making it necessary to adjust contrast injection and scan parameters to the capabilities of these new technologies.8 When evaluating pleural effusion by CT, the role of iodinated contrast medium is to allow for an optimal enhancement of pleural thickening and tumoral lesions, for that purpose scan delay after contrast injection can greatly influence the degree of pleural thickening or nodule enhancement.
These lesions can be difficult to distinguish in the early phases of contrast-enhanced CT of the chest due to the lack of contrast enhancement, this is particularly true when comparing data from CT pulmonary angiography with thoracic CT performed at venous phase, as shown in a recent report evaluating diagnostic performance of routine CT in patients with suspected pleural malignancy.9
Aside from angiographic examinations, thoracic CT scans are routinely performed with a variety of protocols, with many institutions using early phases for scanning the chest and delayed phases for the abdomen.10 The British Thoracic Society (BTS) statement on malignant mesothelioma specifically recommends scanning at 60 s delay to achieve a better contrast of the tumoral lesions,11 while other guidelines12 specifically recommend an early (25–30 s delay) for the chest acquisition in cancer follow-up. There is lack of studies comparing routine non-angiographic early chest CT (25–35 s delay) with more delayed phases for the evaluation of pleural findings associated to malignancy.
In this setting, we performed this study to compare early and delayed phases of contrast-enhanced thoracic CT for assessing pleural thickening or nodules in a series of patients with malignant pleural effusions.
methods and materials
This study was accepted by the Institutional review board and informed consent was obtained from all the participants.
Patient population
From May 2015 to January 2017 all the patients with malignant pleural effusions who met the inclusion criteria were retrospectively included in the study.
To be included, the patients were required to have a malignant effusion diagnosed based on a cytological or histological confirmation, or in some patients based on clinical and radiological criteria supported by data from follow-up, when presented in a patient with known malignancy.
Inclusion criteria were the existence of a CT scan according to the protocol detailed below, a malignant effusion and CT findings such as pleural thickening or nodules visible on both the chest and abdominal phases of the scan.
All the patients had a chest and upper abdomen contrast- enhanced CT scan that included the chest in an early phase and the abdomen in a delayed phase. It was mandatory that the CT examinations showed any grade of visible pleural thickening or nodule on the sections of the abdominal phase covering the lower chest. In this way, we had an early (chest phase) and delayed (abdominal phase) of the same pleural lesion.
Patients were excluded if they weighted less than 50 kg or more than 100 kg, had an estimated glomerular filtration rate less than 60 ml min–1, iodinated contrast material allergy, or if the contrast injection protocol could not be achieved as required due to inadequate vein access, extravasation, or any other problem during contrast injection.
After selecting eligible patients meeting the inclusion criteria, clinical charts were reviewed and patients were excluded if they had a previous pleural intervention such as thoracoscopy or pleurodesis prior to the CT scan. Seven patients were excluded for this reason. Only one scan was included per patient, choosing the earlier one showing any grade of pleural abnormality apart from the effusion. Finally, 36 patients were enrolled in the study. A subset of the patients (12 cases) came from a randomized prospective study evaluating two CT scanning protocols in patients with lung cancer.13 Final study population were 23 males and 13 females, mean age 66.2 years (range 46–81). 19 patients had malignant pleural effusion due to lung cancer (16 adenocarcinoma, and 1 each microcytic, squamous, and non-otherwise specified), 8 had pleural metastasis from breast origin, 7 malignant mesothelioma, 1 metastatic cholangiocarcinoma, and 1 metastatic adenocarcinoma of unknown origin.
CT examination
All CT scans were performed using a 16-detector row scanner (Siemens Somatom Emotion 16; Siemens Medical Solutions, Erlangen, Germany). Scanning protocol consisted of two different acquisitions, one of the chest including the whole lung ending at the lung bases, beginning 35 s after the initiation of contrast administration. This was followed by a 70 s delayed abdominal acquisition, starting at the dome of the diaphragm and extending inferiorly. In the subset of patients belonging to the referred randomized prospective study evaluating two CT scanning protocols in patients with lung cancer,13 the protocol was selected according to the corresponding randomization at the moment of the scan. In the rest of the patients, protocol was selected among our institutional protocols according to the criteria of the radiologist responsible for the examination.
Scan parameters were as follows: collimation, 16 × 1.5 mm; pitch 1.2; rotation time, 0.6 s; reference tube current-time products of 150 mAs for the chest and 200 mAs for the abdomen at a tube voltage of 110 kVp. Automatic tube current modulation (CARE Dose 4D, Siemens, Erlangen, Germany) was switched on for all examinations.
Image reconstruction was performed with a medium-smooth soft-tissue kernel (B30) at a slice thickness of 5 mm without overlapping and a mediastinum window settings [window level, 50 Hounsfield units (HU); window width, 400 HU] for the purpose of the study.
All patients received a standardized i.v. contrast injection with a power injector (Medrad, Indianola, PA) consisting of Iomeprol (Bracco, Milan, Italy) with either 350 or 400 mgI ml−1 at a dose of 0.5 g of iodine per kilogram of weight, a fix duration of injection of 40 s, and followed by 30 ml saline chaser at the same rate as the contrast media. Contrast medium concentration was not controlled and was subjected to availability at the time of the scan.
Image preparation
One author who was radiologist technician and medical student in her last year (CEF), was instructed to select the image showing the pleural abnormalities in both phases, with special attention to single out similar images from both phases. When necessary, this author hid all the vessels or viscera that could suggest the phase of the study as shown in Figure 1, and the same author arranged them together in a random order in a portable document format, with a single number as the only identifier for each image.
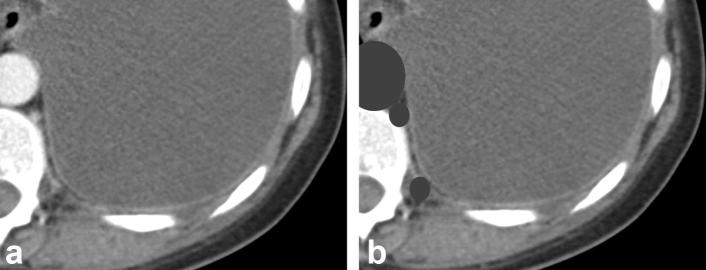
Figure 1.
Delayed phase CT of the chest showing subtle pleural enhancement. Aorta, azygos and intercostal vessels can be seen in A. Blinded image in B shows how all these structures have been hidden.
For a second analysis, a set of paired blinded images, corresponding to the same level of the chest from both phases of the examination, were prepared by the same author, who randomly ordered phases at right or left of the presentation, creating another portable document format with one number identifying each pair of images.
Image reading
Three radiologists (20, 10, and 4 years experienced) and three radiology residents (two in their fourth year and one in her third) read the images.
They first independently scored individual images for pleural thickening or nodules visualization. Readers were asked to grade each individual image by a six-point Likert's scale ranging from 1 (poor) to 5 (excellent visualization) and scored 0 when no pleural thickening or nodules were appreciated (Table 1).
Table 1.
Grading criteria for quality of visualization of pleural thickening or nodules
| Score | Grading criteria |
| 0 | Lack of pleural thickening or nodules |
| 1 | Poor visualization of the pleura |
| 2 | Acceptable but limited visualization |
| 3 | Adequate visualization |
| 4 | Very good visualization |
| 5 | Excellent visualization |
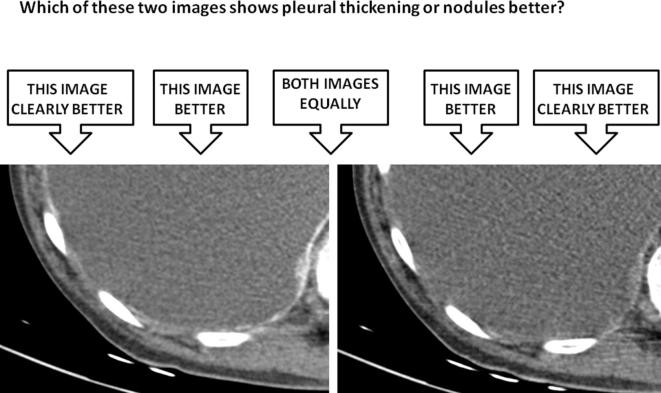
For the paired analysis readers were asked to select which, if any, of the two images showed pleural thickening or nodules better. They graded visualization as equal, better or clearly better than the opposite image as shown in Figure 2.
Figure 2.
Paired image presentation to the readers, showing the delayed phase at the left and early phase at the right. All the readers scored “clearly better” the image on the left. Attenuation of the paravertebral pleural nodule was 115 HU on the left and 40 HU on the right. HU, Hounsfield units.
Contrast enhancement
One author (JJAJ) measured attenuation values in HU of pleural lesions from the images previously selected by placing a circular or ovoid region of interest in the center of the lesion at the same level in both phases. Special attention was paid to avoid effusion, and when the lesion or pleural thickening was too thin to get and adequate measure it was discarded. Eight patients were excluded for this reason, and measurement was performed in the remaining 28.
Statistical analysis
Paired t-test was used to compare attenuation measurements between both phases of the examination.
The qualitative analyses results were compared between both protocols by using χ2 test and mean score by using student’s t-test.
Statistical analysis was performed using the software package SPSS statistics v. 21 (IBM, Somers, NY). Statistical significance was set at 0.05.
Results
Pleural enhancement
Pleural enhancement could be measured in 28 scans. Attenuation values ranged between 32–124 HU for early phase and 42–137 HU for delayed phase. Mean attenuation was significantly higher in the delayed phase (76.0 ± 25.1 vs 57.5 ± 20.7, p < 0.001).
Attenuation values were higher for the delayed phase in 22 out of 28 patients (78.6%) and of them, in all except one examination, measurements of attenuation of delayed phase exceeded in 10 HU or more to those of the early phase. Early phase measurements were higher in five examinations, but in only one case the difference between both values was over 10 HU. In the remaining case the HU values of the pleural thickening was exactly the same in both phases.
Single image scoring
Score of single images by observer is detailed in Table 2. When low quality scores (0,1,2) were grouped together and compared with adequate, good or excellent evaluation (scores 3 to 5), delayed phase was also significantly better than early phase for all the readers. Mean scores (Table 3) were statistically significant higher for delayed phases compared to early phase for all readers.
Table 2.
Single image scores of pleural thickening or nodules visualization by phase for each reader
| Score/Phase | 0 | 1 | 2 | 3 | 4 | 5 | pa | |
| Reader 1 | Early | 1 | 4 | 12 | 7 | 10 | 2 | 0.001 |
| Delayed | 0 | 3 | 1 | 7 | 12 | 13 | ||
| Reader 2 | Early | 1 | 5 | 15 | 8 | 6 | 1 | 0.000 |
| Delayed | 0 | 3 | 3 | 9 | 10 | 11 | ||
| Reader 3 | Early | 5 | 3 | 7 | 7 | 10 | 4 | 0.009 |
| Delayed | 2 | 1 | 2 | 7 | 10 | 14 | ||
| Reader 4 | Early | 2 | 11 | 7 | 10 | 6 | 0 | 0.008 |
| Delayed | 1 | 4 | 4 | 12 | 12 | 3 | ||
| Reader 5 | Early | 2 | 5 | 15 | 10 | 3 | 1 | 0.004 |
| Delayed | 0 | 4 | 6 | 14 | 7 | 5 | ||
| Reader 6 | Early | 3 | 7 | 9 | 8 | 5 | 4 | 0.031 |
| Delayed | 2 | 4 | 4 | 9 | 10 | 7 |
Statistical significance comparing frequency of scores 0, 1, and 2 grouped together vs 3, 4, and 5.
Table 3.
Mean score of single images for visualization of pleural thickening or nodules by phase for each reader
| Phase | Scorea | p | |
| Reader 1 | Early | 2,75 ± 1,23 | 0.000 |
| Delayed | 3,86 ± 1,20 | ||
| Reader 2 | Early | 2,44 ± 1,10 | 0.000 |
| Delayed | 3,64 ± 1,25 | ||
| Reader 3 | Early | 2,72 ± 1,58 | 0.004 |
| Delayed | 3,78 ± 1,40 | ||
| Reader 4 | Early | 2,19 ± 1,21 | 0.003 |
| Delayed | 3,08 ± 1,23 | ||
| Reader 5 | Early | 2,28 ± 1,08 | 0.004 |
| Delayed | 3,08 ± 1,18 | ||
| Reader 6 | Early | 2,47 ± 1,46 | 0.048 |
| Delayed | 3,17 ± 1,46 |
Figures are mean ± standard deviation.
Paired comparison
When pairwise comparison was achieved, delayed phase was considered to be better in 183 of 216 readings (84.7%), with this percentage ranging between 77.8 and 91.7 among the six observers (Table 4). In only 13 readings (6%) early phase was judged better and in 20 (9.3%) were equal. In 72 out of 183 readings (33% of all the readings) considering delayed phase better, it was considered “clearly better”.
Table 4.
Best phase selected in 36 pairs of images for each reader
| Phase/Reader | Reader 1 | Reader 2 | Reader 3 | Reader 4 | Reader 5 | Reader 6 |
| Early | 1 (2,8) | 1 (2,8) | 4 (11,1) | 2 (5,6) | 3 (8,3) | 2 (5,6) |
| Delayed | 33 (91,7) | 32 (88,9) | 28 (77,8) | 31 (86,1) | 31 (86,1) | 28 (77,8) |
| Equal | 2 (5,6) | 3 (8,3) | 4 (11,1) | 3 (8,3) | 2 (5,6) | 6 (16,7) |
Figures in parenthesis are percentages.
Discussion
Detecting pleural findings such as nodules and pleural thickening on CT scans has diagnostic value to characterize pleural effusions. For that purpose, adequate contrast enhancement of these lesions is of major importance. Contrast-enhanced chest CT scans are routinely performed for initial staging and follow-up of patients with neoplasms and in the diagnostic workup of pleural effusions with a variety of protocols. However, studies examining the optimal scanning and contrast injection protocols in this setting are scarce, and there is no consensus about which delay to use. Some publications from medical societies11, 12 and other review articles7, 14,15 include variable recommendations based on expert opinion. There is a trend to suggest delayed phase should be better by permitting a greater enhancement of pleural lesions, with most authors recommending between 45 s14 and more delayed 60–70 s,7, 11,14,15 but evidence for this recommendation is lacking. In this setting, comparison of early and delayed phases of chest CT scan should be of interest to help radiologists choose the optimal scanning protocol.
In a recent report,13 we have shown that a single acquisition thoracic and abdominal delayed phase CT scan has advantages over two independent phases for the chest and abdomen respectively, and that pleural findings are better evaluated at delayed single scan or delayed abdominal phase compared to early phase. In that study however, some interpretation bias due to knowledge of the phase when reading the examination could exist.
To avoid this bias, we designed this study that specifically compares early and delayed phases by blinding the images and making a blind pairwise comparison between both phases. The optimal study design for evaluating both phases should be an accuracy study, scanning the same patient by both protocols in a limited time period and blinding all images to avoid bias due to knowledge of the phase. However, the number of patients required and technical limitations for blinding all the images in a study precludes this design. In this setting, pairwise comparison has been shown to be a good method for image assessment.16
A recent report evaluating diagnostic performance for pleural malignancy of routine CT has shown the superiority of venous phase imaging acquired 60–70 s post-contrast compared to CT pulmonary angiography using bolus tracking in the pulmonary artery.9 However, accuracy in this study was retrospectively assessed based on the radiological report as part of the routine clinical activity. Moreover, the timing for CT pulmonary angiography in that study differs from that from routine early chest contrast-enhanced scan. What we call early delay in our series corresponds to that recommended for the chest by the Royal College of Radiology for cross-sectional imaging in cancer management11 and is routinely used in many radiology facilities, as reported in a Spanish radiologist's survey on the management of lung cancer.10 However, Hooper et al17 reported coexistence of both malignant effusion and pulmonary embolism in up to 9.8% in a series of patients presenting with unilateral pleural effusion and they suggest a combined CT pulmonary angiography and a pleural phase CT protocol in this setting.
When pleural enhancement measurement was feasible, we found attenuation values were higher in the delayed phase in most patients. Both the overall dose and the contrast infusion rate play a role in the final enhancement for the same delay,8 but they were maintained constant in all the examinations according to the patient’s weight. Raj et al18 using 60 s delayed CT scans, found greater enhancement of the pleura at higher contrast dose and rate, although the dose was fixed for all the patients in their study, independently of their weight. Mean attenuation values in our patients with delayed phase were between those of the high and low contrast dose groups in the study by Raj et al.18
Accordingly to these attenuation value differences, subjective score of individual images were also uniformly better in the delayed phase for all observers independently of their experience level, as demonstrated by both the mean scores and the comparison of ranked Likert’s scale.
Results of evaluation of paired images clearly also show the preferences of all the readers for the delayed phase over the early phase. As stated before, pairwise comparison is an acceptable method to assess subjective image quality16 when accuracy studies are not possible, or as in our case, blinding of part of the information of the images is required and manually performed. To our knowledge this is the first report using this methodology to show the superiority of one phase over the other in evaluation of pleural findings and the results favor the use of the delayed phase. Our findings come to confirm the assertion from the BTS statement on malignant mesothelioma11 that scan delay of 60 s allows for an optimal visualization of pleural disease and in our study increases the confidence of the readers to make a diagnosis of pleural thickening or nodule. The use of a single delayed phase or dual early and delayed phases should be advocated for CT scans evaluating patients with suspected malignant pleural effusions. When two different phases are performed for the chest and the abdomen, the delayed abdominal phase covering the lower pleura could be valuable to better detect pleural thickening and nodules.
Our study has some limitations. First, it is a retrospective study and scanning protocol was chosen according to a radiologist's preference, thus limiting the generalization of the results. That is the reason why there is a relatively small number of patients, since many eligible patients were scanned with other protocols, mainly a single acquisition delayed phase. However, despite the small sample, we think our results are significant enough to take into consideration. Second, restricting the reading to one single image per phase in each patient also decreases the power of the study, although as stated before, it is an acceptable way to compare qualitative characteristics for a given technique. Third, the tube current-time product was different between early and delayed phase and this could have a role in a worse perception of the findings due to more noisy images in the early phase, particularly in heavy patients.
In conclusion, our results are an evidence supporting that the delayed phase should be preferable to early phase for evaluating pleural thickening or nodules associated to malignant pleural effusions.
Contributor Information
Juan José Arenas-Jiménez, Email: j.arenasjimenez@gmail.com.
Elena García-Garrigós, Email: piolelena@hotmail.com.
Carmen Escudero-Fresneda, Email: carmen.escudero@goumh.umh.es.
Marina Sirera-Matilla, Email: marinasirera@gmail.com.
Irene García-Pastor, Email: irene.garciapastor@gmail.com.
Alberto Quirce-Vázquez, Email: aquirce89@gmail.com.
Mariana Planells-Alduvin, Email: mcplanells@gmail.com.
REFERENCES
- 1.Leung AN, Müller NL, Miller RR. CT in differential diagnosis of diffuse pleural disease. AJR Am J Roentgenol 1990; 154: 487–92. doi: 10.2214/ajr.154.3.2106209 [DOI] [PubMed] [Google Scholar]
- 2.Arenas-Jiménez J, Alonso-Charterina S, Sánchez-Payá J, Fernández-Latorre F, Gil-Sánchez S, Lloret-Llorens M. Evaluation of CT findings for diagnosis of pleural effusions. Eur Radiol 2000; 10: 681–90. doi: 10.1007/s003300050984 [DOI] [PubMed] [Google Scholar]
- 3.Hierholzer J, Luo L, Bittner RC, Stroszczynski C, Schröder RJ, Schoenfeld N, et al. MRI and CT in the differential diagnosis of pleural disease. Chest 2000; 118: 604–9. doi: 10.1378/chest.118.3.604 [DOI] [PubMed] [Google Scholar]
- 4.Traill ZC, Davies RJ, Gleeson FV. Thoracic computed tomography in patients with suspected malignant pleural effusions. Clin Radiol 2001; 56: 193–6. doi: 10.1053/crad.2000.0573 [DOI] [PubMed] [Google Scholar]
- 5.Hallifax RJ, Haris M, Corcoran JP, Leyakathalikhan S, Brown E, Srikantharaja D, et al. Role of CT in assessing pleural malignancy prior to thoracoscopy. Thorax 2015; 70: 192–3. doi: 10.1136/thoraxjnl-2014-206054 [DOI] [PubMed] [Google Scholar]
- 6.Porcel JM, Pardina M, Bielsa S, González A, Light RW. Derivation and validation of a CT scan scoring system for discriminating malignant from benign pleural effusions. Chest 2015; 147: 513–9. doi: 10.1378/chest.14-0013 [DOI] [PubMed] [Google Scholar]
- 7.Cardinale L, Ardissone F, Gned D, Sverzellati N, Piacibello E, Veltri A. Diagnostic Imaging and workup of Malignant Pleural Mesothelioma. Acta Biomed 2017; 88: 134–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bae KT. Intravenous contrast medium administration and scan timing at CT: considerations and approaches. Radiology 2010; 256: 32–61. doi: 10.1148/radiol.10090908 [DOI] [PubMed] [Google Scholar]
- 9.Tsim S, Stobo DB, Alexander L, Kelly C, Blyth KG. The diagnostic performance of routinely acquired and reported computed tomography imaging in patients presenting with suspected pleural malignancy. Lung Cancer 2017; 103: 38–43. doi: 10.1016/j.lungcan.2016.11.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.García Garrigós E, Arenas Jiménez JJ, Sánchez Payá J, Sirera Matilla M, Gayete Cara À. Computed tomography protocols used in staging bronchopulmonary carcinoma: results of a national survey. Radiologia 2016; 58: 460–7. doi: 10.1016/j.rxeng.2016.11.002 [DOI] [PubMed] [Google Scholar]
- 11.British Thoracic Society Standards of Care Committee BTS statement on malignant mesothelioma in the UK, 2007. Thorax 2007; 62(Suppl 2): ii1–ii19. doi: 10.1136/thx.2007.087619 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.William S. General techniques for examinations discussing CT, biopsy and MRI: Nicholson T (ed) : Recommendations for cross-sectional imaging in cancer management. Second edition London: The British Institute of Radiology.; 2014. [Google Scholar]
- 13.García-Garrigós E, Arenas-Jiménez JJ, Sánchez-Payá J. Best protocol for combined contrast-enhanced thoracic and abdominal CT for lung cancer: A single-institution randomized crossover clinical trial. AJR Am J Roentgenol 2018; 210: 1226–34. doi: 10.2214/AJR.17.19185 [DOI] [PubMed] [Google Scholar]
- 14.Benamore RE, O'Doherty MJ, Entwisle JJ. Use of imaging in the management of malignant pleural mesothelioma. Clin Radiol 2005; 60: 1237–47. doi: 10.1016/j.crad.2005.05.015 [DOI] [PubMed] [Google Scholar]
- 15.Evans AL, Gleeson FV. Radiology in pleural disease: state of the art. Respirology 2004; 9: 300–12. doi: 10.1111/j.1440-1843.2004.00599.x [DOI] [PubMed] [Google Scholar]
- 16.Phelps AS, Naeger DM, Courtier JL, Lambert JW, Marcovici PA, Villanueva-Meyer JE, et al. Pairwise comparison versus Likert scale for biomedical image assessment. AJR Am J Roentgenol 2015; 204: 8–14. doi: 10.2214/AJR.14.13022 [DOI] [PubMed] [Google Scholar]
- 17.Hooper C, Laurence I, Harvey J, Morley A, Darby M, Edey A, et al. The role of CT pulmonary angiography in the investigation of unilateral pleural effusions. Respiration 2014; 87: 26–31. doi: 10.1159/000347003 [DOI] [PubMed] [Google Scholar]
- 18.Raj V, Kirke R, Bankart MJ, Entwisle JJ. Multidetector CT imaging of pleura: comparison of two contrast infusion protocols. Br J Radiol 2011; 84: 796–9. doi: 10.1259/bjr/55980445 [DOI] [PMC free article] [PubMed] [Google Scholar]