I Introduction
There is an emerging consensus that catastrophic health care costs are very important in developing countries, but the evidence on developed countries is less clear, with some estimates suggesting that as little as 0.5 percent of U.S. households are subject to high health care expenditures in any given year (Xu et al., 2003). With out-of-pocket spending as a fraction of total health care expenditures declining over time in the U.S. (World Bank, 2016), one might think that U.S. government and private health insurance are successfully insuring against such risks. Contrary to this view, we have found in previous work using the Health and Retirement Study (HRS) that out-of-pocket expenditure for health care represents a substantial financial burden for many elderly people, particularly for those near the end of life, or with dementia (Marshall, McGarry, and Skinner, 2011; Kelley et al., 2015).
In this paper, we take a new look at out-of-pocket expenditures, focusing on variations across demographic groups and with particular attention paid to such spending near the end-of-life. We are able to provide more detail on components of spending and cast a wider net on types of spending than previous studies. De Nardi et al. (2015a) recently used the Medicare Current Beneficiary Survey (MCBS) to document patterns of out-of-pocket health care expenditures in the United States, but these tabulations looked only at total spending and lacked detail about the components of out-of-pocket expenditures, for example expenses associated with making a home more accessible for disabled respondents. And unlike many other studies of out-of-pocket expenditures, the HRS “exit” interview data allows us to collect information about the substantial household medical expenses near death. Finally, by focusing on a common set of statistics comparable to those of the other studies in this volume, we are also able to put U.S. out-of-pocket spending in the context of other countries.
Measuring out-of-pocket expenditures in surveys is extremely difficult, and we have found that many responses to such questions are incomplete or confused. We therefore developed a detailed imputation approach to begin “filling in” the missing survey data and to capture the national distribution of out-of-pocket health care spending (Marshall, McGarry, and Skinner, 2011). This imputation approach, described in detail below, was motivated by a need to capture accurately out-of-pocket spending, and to distinguish rare but unusually high spending, from simple reporting error. Most empirical economic studies drop outliers, but in the case of out-of-pocket expenditures, it’s precisely the outliers that represent the uninsured spending risks most likely to affect savings behavior over the life cycle and especially during retirement
Briefly, we find that spending risk rises sharply at older ages and is greatest for individuals near the end-of-life, where the median individual spends $6,300 in their last year and five percent of those surveyed were reported to have spent over $62,000. We also find a remarkably wide distribution of out-of-pocket spending, particularly when aggregating over the final two years or final five years of life. Because most surveys do not include spending during the time elapsed since the last interview and death, estimates of the cost of care at the end of life will be downward biased. In contrast, the HRS conducts exit interviews of proxy-respondents following the death of a survey respondent and thus does capture these very high expenses near death.1 With these data, we show that out-of-pocket spending is highly concentrated both in terms of total expenditures—where the top 10 per cent of spenders account for 42 per cent of all spending—and even more so when broken down by spending category. This total spending displays relatively high persistence, even over long periods of time. We also find that mean out-of-pocket spending increases with both income and wealth, yet, while certain categories of spending are highly sensitive to the level of resources, spending itself turns out to be less concentrated in the upper income and wealth quintiles than one might expect. The results presented here are supportive of the view that U.S. households, in comparison to those in the U.K., are more likely to consume at higher rates during late retirement because of these very high out-of-pocket financial risks (Banks et al., 2015).
Finally, our results suggest that the fraction of households facing very high out-of-pocket spending is substantially greater in the U.S. than in other developed countries. For studies in this volume that do tabulate out-of-pocket expenses, the distribution of spending appears to be considerably less than what we find for the U.S.2 And while we cannot adjust across countries for quality of care or differences in tastes for medical care, the reality faced by elderly households in the U.S. is large and highly variable out-of-pocket expenditures, with potentially large effects on saving behavior and the well-being of elderly Americans. (Hubbard, Skinner, and Zeldes, 1995; De Nardi, French, and Jones, 2010).
II Data
The Health and Retirement Study (HRS) is a longitudinal survey of the U.S. population approximately ages 50 or older and their spouses or partners. The survey was begun in 1992 with a sample of 12,652 individuals who were born between 1931 and 1941 or who had a spouse or partner born in those years. In the case of couples, both parties were interviewed. These initial HRS respondents have been interviewed biennially ever since and will be followed until they die or attrit from the sample. A second cohort, individuals born in 1923 or earlier and their spouses and partners was interviewed in 1993 and again in 1995. These surveys were referred to as the Asset and Health Dynamics of the Oldest Old (AHEAD). In 1998, the AHEAD cohort was merged with the original HRS cohort. In addition, two new cohorts of individuals were added, those born between 1924 and 1930 (Children of the Depression Era) and those born between 1942 and 1947 (War Babies). These additions made the sample in the 1998 interview approximately representative of the population ages 51 or older. Refresher cohorts have since been added in 2004 and 2010 to keep the sample approximately population representative when properly weighted.
The HRS has several noteworthy attributes that facilitate the study of out-of-pocket medical expenditures. First, rather than a single measure of total expenditures, it collects detailed information on spending, utilisation, and insurance coverage for a variety of expenditure categories. Second, to deal with non-response, the HRS allows respondents who either do not know or refuse to disclose their actual expenditure to report a range for their spending. For instance, in lieu of reporting an exact dollar amount spent on a particular expenditure category—hospital stays, for example—an individual may instead report that she spent somewhere between $1,000 and $5,000 dollars. The particular range is arrived at through a series of unfolding bracket questions, an HRS innovation known as “random-entry bracketing.” Finally, in addition to the biennial interviewers—referred to hereafter as “core” interviews—when a respondent dies, the subsequent core interview is conducted with a knowledgeable survivor—typically the spouse if one is available, or a child, although neighbors and others have been interviewed. These “exit” interviews are critically important for obtaining an accurate measurement of medical spending at the end of life.
The categories available in the HRS vary both across survey years and between core and exit interviews, but they generally include spending on nursing homes, hospital in-patient stays, doctor visits, home care, special services and facilities, helpers, and insurance costs.3 Insurance costs include long-term care insurance premiums, private health care premiums, such as those for “Medigap” supplemental Medicare insurance policies, as well as premiums for Medicare Part B, Medicare Part C HMOs, and Medicare Part D prescription drug benefits.4 Beyond these categories, spending on out-patient surgery and dentist visits are available in core interviews in all survey years and exit interviews beginning in 2010. Exit interviews also contain data on spending on hospice care, non-medical expenditures—including, for example, home modification expenditures and housekeeping—and a catch-all “other” category for expenditures not covered by these categories.5
Within each category of spending, questioning generally follows a fairly standard pattern. Typically, respondents are first asked whether they used a particular service. For certain services—including visits to doctors, hospitals, nursing homes, and hospice—the number of visits or nights spent is also elicited. For those who do not use the particular service, or who are unaware of whether they used it, the strand of questioning stops here. However, if the use of a particular service is reported, the respondent is then asked whether they had to pay for the service, or whether their insurance covered all, some, or none of the expense. Those for whom insurance coverage was less than complete, for whom the extent of coverage was unknown, or who reported that the costs were not yet settled, are asked for the total amount spent. Spending is typically reported for the period between the end of the previous interview and the current interview, regardless of the length of that time period.6 We utilise all of this information in our imputation procedures.
Our imputation procedure has three broad steps. First, we cap outlier expenditure amounts at limits that reflect both the time elapsed since the previous interview and our knowledge of what might constitute a reasonable maximum expenditure over that period. Second, where a continuous report for spending is unavailable, we impute values using the elicited spending ranges obtained from the bracketing questions. Finally, where brackets are also unavailable, we impute remaining missing values using additional available information on utilisation and insurance coverage. All imputations are done separately for core and exit interview data. The following paragraphs elaborate on our imputation methodology.
The first problem that we confront in our imputation procedure is the handling of outliers. In doing so, we must be careful not to accept erroneous values of spending—a type II error—while also taking care not to wrongfully eliminate extreme, but correctly reported, amounts—a type I error. To deal with the outliers, we impose caps on maximum monthly expenditures in each spending category. These caps are reported in Table 1. The cap that we ultimately apply to an individual observation is adjusted for the amount of time elapsed between interviews. For instance, the monthly cap we use for nursing home spending is $15,000 (2010 dollars), so we assume that an individual with 24 months elapsed since the previous interview could have realistically spent at most $15,000 per month for 24 months, or $360,000. For further discussion of the rationales behind particular caps, see Marshall, McGarry, and Skinner (2011), pp. 110–1.
TABLE 1.
Monthly caps for out-of-pocket spending by category
| Category | Monthly Cap |
|---|---|
| Insurance Costs | $2,000 |
| Hospital, In-patient | $15,000 |
| Nursing Home | $15,000 |
| Doctor | $5,000 |
| Out-patient Surgery | $15,000 |
| Dental | $1,000 |
| Prescription Drugs | $5,000 |
| Hospice | $5,000 |
| Home Health Services | $15,000 |
| Special Services, Facilities | $15,000 |
| Non-Medical (includes Home Modification) | $5,000 |
| Helpers | $15,000 |
| Other | $15,000 |
Note: All caps are reported in 2010 dollars. Helper expenses are assumed to take place for a maximum of 4 months. Within the category of insurance costs, we assign a cap of $400 to Medicare HMO monthly premiums, $100 to Medicare Part D, $2,000 to long-term care, $400 to private Medigap policies (i.e. private insurance for individuals 65 and over), and $2,000 to private insurance premiums for individuals under 65.
When applying the caps to the expenditures in a particular year, we also convert the caps from the 2010 dollar amounts reported in Table 1 into the current dollars of the particular year (e.g., 2014) using the personal core expenditures chain-type price index. Therefore, while the value of the monthly cap for a given spending category is constant in real terms across interview years, the caps that we apply in particular interview years vary in nominal terms.
In the second step of our imputation procedure, we impute a continuous value for each bracketed response. To do so, we use the un-weighted mean of all continuous values within that bracket across all survey years.7 We use responses for all years in order to have a thicker sample. Were we to limit the set of continuous reports over which we calculate the within-bracket means to just a single year, certain categories of spending would have intervals with very few observations. We do this process separately for each survey wave because bracket endpoints are denominated in the currency of the survey wave. In cases of incomplete brackets wherein a respondent fails to report an upper limit, we use our capped value multiplied by the number of months elapsed between interviews as an upper limit. In addition, if the product of our monthly cap and the months elapsed between interviews is smaller than the reported upper bracket, we replace the bracket with our cap. If a lower bracket is not supplied, we use zero as the default lower bracket.
The third and final step of the imputation procedure applies to cases where brackets are not supplied. In these situations, we first use information on the intensive margin of service utilisation. For spending on overnight stays in hospitals and nursing homes or visits to the doctor, we can obtain the number of nights spent or the number of visits. Using data from all survey waves from 2002–12, we compute average spending per night or visit, separately for each quartile of the number of nights or visits, and use these calculations to impute spending for an individual based on their utilisation.8
In cases where intensive margin utilisation data are not available, we impute missing values using a sequential procedure based on extensive margin utilisation data and insurance coverage. First, for individuals who report spending not fully covered by insurance, we impute the mean spending over all individuals in their survey year with positive expenditures. Second, to individuals whose expenses were covered we assign zeros. Third, to individuals unsure about their coverage, we impute the mean taken over all individuals in their survey year whose coverage information was known, including both those whose usage was fully covered and those whose usage was not. Fourth, we impute zeros to individuals who did not use the service in question. Finally, for individuals unsure of whether they used the service, we impute the mean taken over all individuals, including both those who used and those who did not use the service. Using this mean takes into account all of the various possibilities that these individuals may or may not have used the service, which may or may not have been covered by their insurance.
We limit our analyses in this paper to the core and exit interview data from 2008–12 survey waves to capture out-of-pocket spending patterns subject to Medicare Part D prescription drug coverage, which was implemented in 2006. Using data from the later years of the survey also mitigates the bias in the earlier survey years due to sampling from only the non-institutionalised population when the survey was initiated. Note, however, that the bracket imputations are done using means computed from the full range of the data from 1995–2012. We also restrict our sample to include only HRS respondents 55 years of age and older.
All expenditure amounts reported in this paper have been converted to 2014 dollars using the personal core expenditures chain-type price index and annualised by dividing spending by the number of months elapsed between interviews—or between the final core interview and the date of death—and multiplying by 12. Throughout this article, all means and quantiles are calculated using household sample weights provided by the HRS. Because decedents are assigned zero sample weights, we use weights from preceding core interviews.9 Finally, wherever the natural logarithm of a variable is used, observations are first bottom-coded at 10 per cent of the sample mean, taken in the particular survey wave in which the observation occurs.
III Data validation
Several studies have already thoroughly examined the validity of the HRS data through comparisons with alternative data sets. While Hurd and Rohwedder (2009) find that aggregate spending in the HRS is up to 60 per cent greater than aggregates based on the Medicare Expenditure Panel Survey (MEPS) and the Medicare Current Beneficiary Survey (MCBS), most researchers conclude that the HRS does not overstate out-of-pocket spending. French and Jones (2004) find that aggregate spending in the HRS is close to aggregates obtained from MCBS and MEPS after correcting for known under-reporting issues in those datasets. Goldman, Zissimopoulos, and Lu (2011) also compare the HRS with MEPS and MCBS and observe the measures of total out-of-pocket spending to be very similar across the three surveys. In fact, their results suggest that the HRS measures understate non-drug, non-nursing-home spending relative to MCBS. Consistent with the results from these studies, Marshall, McGarry, and Skinner (2011) conclude that aggregate estimates produced using the 2004 HRS data are very close to aggregate estimates based on the National Medical Expenditure Accounts (NMEA).
Most recently, De Nardi, French, and Jones (2013) compare means from the MCBS and the Asset and Health Dynamics of the Oldest Old (AHEAD) cohort of the HRS. In Appendix A, the authors report that conditional on income quintiles, average out-of-pocket spending among single elderly individuals in the AHEAD cohort is slightly lower across all income quintiles relative to the MCBS. Medicaid recipiency rates are also somewhat lower in AHEAD than in the MCBS, which in turn, are slightly lower than official enrollment numbers in the Medicaid Statistical Information System (MSIS). Taken together, the existing body of research on this topic provides us with little reason to doubt the validity of the out-of-pocket spending data in the HRS.
IV Spending over the life-cycle
We begin our analysis by examining the distribution of out-of-pocket medical expenditures over the life-cycle. As a first step, Table 2 presents the mean expenditures and various percentiles of spending for each of the spending categories reported in the HRS.10 The data in the table are for all individuals 55 or older in the survey waves 2008–12 and include data from both core and exit interviews. There are a total of 55,044 individual-interview observations, including 3,902 exit interviews (seven per cent) and 51,142 core interviews (93 per cent). Despite accounting for only seven per cent of the observations in the sample, the exit interviews contribute 21 per cent of the total out-of-pocket spending in the sample. Within particular categories, the influence of the exit interviews is even greater: the exit interviews contribute 46 per cent of spending on hospitals, 55 per cent of spending on nursing homes, 61 per cent of spending on home care, and 72 per cent of spending on helpers.11
TABLE 2.
Means and percentiles of spending by category, all interviews 2008–12
| Mean | 10th | 50th | 75th | 90th | 95th | 99th | |
|---|---|---|---|---|---|---|---|
| Hospital, In-patient | 306 | 0 | 0 | 0 | 233 | 1,005 | 5,564 |
| Nursing Home | 543 | 0 | 0 | 0 | 0 | 0 | 16,786 |
| Doctor | 289 | 0 | 50 | 209 | 625 | 1,294 | 3,883 |
| Out-Patient Surgery | 76 | 0 | 0 | 0 | 48 | 292 | 1,667 |
| Dental | 339 | 0 | 56 | 307 | 921 | 1,501 | 3,929 |
| Prescription Drugs | 761 | 0 | 307 | 835 | 1,842 | 2,825 | 6,446 |
| Home Health Services | 56 | 0 | 0 | 0 | 0 | 0 | 458 |
| Special Facility, Service | 35 | 0 | 0 | 0 | 0 | 46 | 562 |
| Helper | 129 | 0 | 0 | 0 | 0 | 0 | 2,730 |
| Non-Medical | 515 | 0 | 0 | 0 | 342 | 1,478 | 10,701 |
| Hospice | 159 | 0 | 0 | 0 | 0 | 0 | 3,917 |
| Insurance Costs | 2,663 | 0 | 1,916 | 3,852 | 6,086 | 7,595 | 13,505 |
| Other | 114 | 0 | 0 | 0 | 74 | 331 | 2,046 |
|
| |||||||
| Total | 5,289 | 349 | 3,504 | 6,228 | 10,088 | 14,535 | 37,254 |
| Total, Excluding NH | 4,765 | 345 | 3,462 | 6,071 | 9,456 | 12,855 | 25,642 |
Several insights are immediately evident from Table 2. First, there is considerable tail-risk in out-of-pocket medical spending. Though the median individual spends only $3,500 dollars out-of-pocket per year on health care, much larger expenditures are not uncommon. Ten per cent of individuals spend more than $10,000 per year out-of-pocket, and an unlucky one per cent spend over $37,000 in a single year. A major component of the expenditure risk is nursing home spending. Though over 95 per cent of individuals spend nothing on nursing homes, those who do pay a great deal. Excluding nursing home expenses reduced the 99th percentile of total out-of-pocket spending by over $11,000.
The outsized role nursing home spending risk in Table 2 and in the tables that follow owes to institutional characteristics of health care provision in the U.S. Medicare, the primary source of insurance coverage for the elderly, provides only very limited coverage of long-term care services. Medicaid, on the other hand, provides a wide range of long-term care services, but to be eligible, an individual is required to have exhausted nearly all of her income and assets. In addition, relatively few individuals in the U.S. hold private long-term care insurance. As a consequence, for the many individuals in the U.S. with non-negligible assets and without private long-term care insurance, long-term care spending risk is effectively uninsured, resulting in the very substantial out-of-pocket payments that we observe in the HRS. These features of the institutional setting in the U.S. also contribute to the sharp increase in out-of-pocket medical spending in old age, which we explore below, because long-term care services are disproportionately consumed by individuals at older ages.
A second conclusion from Table 2 is that the most sizable expenditure category is for health insurance. This category has the greatest spending at the mean and at all percentiles except for the 99th, where insurance costs are edged out of first place by nursing home expenses. While the median individual spends just about $2,000 out-of-pocket on annual insurance costs, 10 per cent of individuals spend $6,000 or more for insurance. We return to the issue of insurance in Section VIII.
While the majority of the results in this paper are based on the sample that appears in Table 2, it is illuminating to compute the same set of statistics separately for the core interviews and the exit interviews (for people who died). The results of this comparison appear in Tables 3 and 4. Table 3 presents the statistics computed with only the core interview data while Table 4 uses only data from the exit interviews. The striking differences between the tables highlight the importance of exit interview spending—the spending nearest to the end of life—as a share of spending over the life-cycle. They also illustrate how the influence of the exit interview data is greatly reduced when these observations are pooled with the core interview data. In fact, the results with the pooled data in Table 2 are very similar to the results using only the core interview data in Table 3.
TABLE 3.
Means and percentiles of spending by category, core interviews 2008–12
| Mean | 10th | 50th | 75th | 90th | 95th | 99th | |
|---|---|---|---|---|---|---|---|
| Hospital, In-patient | 195 | 0 | 0 | 0 | 134 | 828 | 3,612 |
| Nursing Home | 268 | 0 | 0 | 0 | 0 | 0 | 5,910 |
| Doctor | 254 | 0 | 52 | 205 | 576 | 1,195 | 3,314 |
| Out-Patient Surgery | 75 | 0 | 0 | 0 | 52 | 294 | 1,688 |
| Dental | 341 | 0 | 61 | 308 | 925 | 1,508 | 3,877 |
| Prescription Drugs | 720 | 0 | 282 | 798 | 1,753 | 2,589 | 6,421 |
| Home Health Services | 26 | 0 | 0 | 0 | 0 | 0 | 144 |
| Special Facility, Service | 30 | 0 | 0 | 0 | 0 | 40 | 474 |
| Helper | 42 | 0 | 0 | 0 | 0 | 0 | 828 |
| Non-Medical | . | . | . | . | . | . | . |
| Hospice | . | . | . | . | . | . | . |
| Insurance Costs | 2,691 | 0 | 1,926 | 3,883 | 6,139 | 7,705 | 13,676 |
| Other | 73 | 0 | 0 | 0 | 48 | 256 | 1,382 |
|
| |||||||
| Total | 4,674 | 348 | 3,420 | 5,986 | 9,310 | 12,682 | 25,963 |
| Total, Excluding NH | 4,425 | 348 | 3,397 | 5,892 | 9,036 | 11,806 | 21,705 |
TABLE 4.
Means and percentiles of spending by category, exit interviews 2008–12
| Mean | 10th | 50th | 75th | 90th | 95th | 99th | |
|---|---|---|---|---|---|---|---|
| Hospital, In-patient | 2,176 | 0 | 0 | 647 | 3,348 | 7,377 | 42,575 |
| Nursing Home | 5,162 | 0 | 0 | 0 | 12,330 | 34,067 | 91,372 |
| Doctor | 878 | 0 | 0 | 462 | 1,811 | 3,852 | 13,655 |
| Out-Patient Surgery | 84 | 0 | 0 | 0 | 0 | 92 | 1,027 |
| Dental | 285 | 0 | 0 | 161 | 680 | 1,444 | 5,564 |
| Prescription Drugs | 1,453 | 0 | 514 | 1,886 | 3,683 | 4,911 | 13,920 |
| Home Health Services | 629 | 0 | 0 | 0 | 275 | 2,046 | 13,783 |
| Special Facility, Service | 123 | 0 | 0 | 0 | 0 | 201 | 2,193 |
| Helper | 1,604 | 0 | 0 | 0 | 2,912 | 8,555 | 30,819 |
| Non-Medical | 515 | 0 | 0 | 0 | 342 | 1,478 | 10,701 |
| Hospice | 159 | 0 | 0 | 0 | 0 | 0 | 3,917 |
| Insurance Costs | 2,185 | 0 | 1,689 | 3,366 | 4,917 | 6,130 | 8,675 |
| Other | 588 | 0 | 0 | 0 | 767 | 1,926 | 9,444 |
|
| |||||||
| Total | 15,623 | 382 | 6,328 | 15,100 | 38,955 | 62,040 | 166,359 |
| Total, Excluding NH | 10,471 | 272 | 5,292 | 10,373 | 21,922 | 35,912 | 96,228 |
Furthermore, exposure to out-of-pocket risk in the core interview data in Table 3 pales in comparison to the risks found in the exit data, shown in Table 4. The median individual in the core interviews reports total spending of just around $3,400 out-of-pocket per year while 10 per cent spend more than $9,300 in a single year and five per cent spend over $12,600. By comparison, the annual out-of-pocket spending by the median individual in the exit interview data is $6,300. In the exit interviews, 10 cent of survey respondents spent $39,000 or more, and five per cent were reported to have spent over $62,000 out-of-pocket in their final year. The majority of this spending risk is due to nursing home spending, but considerable risk exists for many categories, including hospital and helper spending.
Table 5 compares the expenditure shares of each category for the core and exit interview data.12 Among those surveyed in the core interviews, insurance costs are by far the most significant category, accounting for 57 per cent of total out-of-pocket expenditure. This category is somewhat less important in the exit interview data but still accounts for 14 per cent of spending. Prescription drug costs are also a significant expenditure in both types of interviews, accounting for 15 and 9 per cent of total spending in core and exit interviews, respectively. Table 5 emphasises once again the importance of nursing home expenditure risk. While nursing home expenditures account for just six per cent of core interview spending, they represent 33 per cent of the spending in the exit interview data.
TABLE 5.
Expenditure shares by category and interview type
| Core | Exit | All | |
|---|---|---|---|
| Hospital, In-patient | 4.15 | 13.92 | 5.77 |
| Nursing Home | 5.70 | 33.02 | 10.23 |
| Doctor | 5.41 | 5.61 | 5.45 |
| Out-Patient Surgery | 1.60 | 0.35 | 1.39 |
| Dental | 7.26 | 1.21 | 6.23 |
| Prescription Drugs | 15.37 | 9.29 | 14.36 |
| Home Health Services | 0.55 | 3.51 | 1.04 |
| Special Facility, Service | 0.64 | 0.78 | 0.67 |
| Helper | 0.89 | 10.27 | 2.45 |
| Non-Medical | 0.00 | 3.27 | 0.68 |
| Hospice | 0.00 | 1.02 | 0.21 |
| Insurance Costs | 57.37 | 13.98 | 50.18 |
| Other | 1.07 | 3.76 | 1.52 |
|
| |||
| Total | 100.00 | 100.00 | 100.00 |
| Total, Excluding NH | 94.27 | 66.99 | 89.75 |
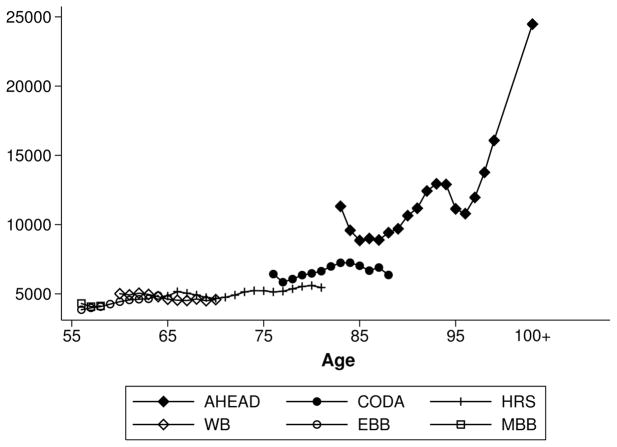
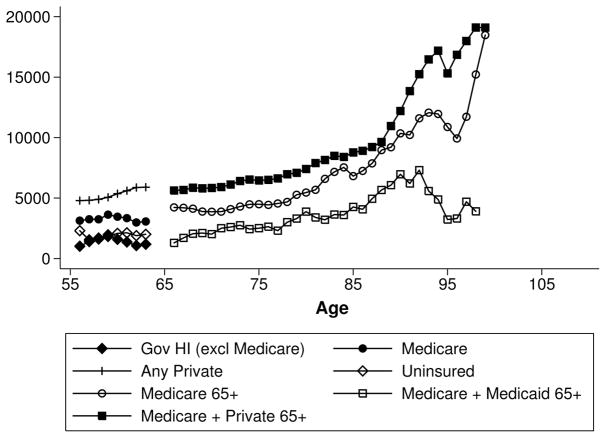
Returning to the analysis of life-cycle spending using the pooled core and exit interview data, Figure 1 depicts the evolution of mean total out-of-pocket expenditures with age. The figure plots three-year moving averages of total spending separately by the six distinct cohorts in the HRS. From the figure, the rise in out-of-pocket spending with age appears to be very gradual until individuals reach their mid-eighties, at which point spending rises sharply.
FIGURE 1.
Mean total spending by age and cohort
Note: Three-year moving average. A given cell is dropped when the number of observations in that cell and in the two adjacent cells combined is less than 50. This results in 2 observations being dropped.
Further details are provided in Tables 6 and 7, which depict the growth in spending for each expenditure category with age. Table 6 reports mean out-of-pocket spending by expenditure category while Table 7 records the share of total spending accounted for by each category. Both tables present figures for four age groups: 55–64, 65–74, 75–84, and 85+. As the tables indicate, much of the steep rise in spending at older ages is accounted for by nursing homes. Mean spending on nursing homes for individuals ages 85 or older is $3,538, which is 3.7 times larger than the mean among individuals ages 75–84 and 22 times larger than the mean among those ages 65–74. While spending on nursing homes accounts for only three per cent of spending for individuals ages 65–74, it represents over 15 per cent of spending for individuals ages 75–84 and more than 36 per cent for individuals 85 and older. Other categories of spending related to long-term care, such as home health services and helpers, also increase sharply for the oldest age group. While mean expenditures on prescription drugs and insurance costs are consistently large across all age groups, the share of total spending accounted for by these categories declines somewhat with age, especially for the 85+ age group.
TABLE 6.
Mean expenditure by category and age
| 55–64 | 65–74 | 75–84 | 85+ | Total | |
|---|---|---|---|---|---|
| Hospital, In-patient | 319 | 241 | 314 | 437 | 306 |
| Nursing Home | 32 | 159 | 946 | 3,538 | 543 |
| Doctor | 325 | 242 | 250 | 339 | 289 |
| Out-Patient Surgery | 104 | 54 | 56 | 38 | 76 |
| Dental | 329 | 361 | 344 | 304 | 339 |
| Prescription Drugs | 649 | 789 | 908 | 941 | 761 |
| Home Health Services | 18 | 19 | 86 | 323 | 56 |
| Special Facility, Service | 30 | 21 | 48 | 82 | 35 |
| Helper | 21 | 49 | 187 | 816 | 129 |
| Non-Medical | 354 | 426 | 478 | 649 | 515 |
| Hospice | 40 | 244 | 145 | 165 | 159 |
| Insurance Costs | 2,574 | 2,748 | 2,779 | 2,603 | 2,663 |
| Other | 75 | 83 | 169 | 284 | 114 |
|
| |||||
| Total | 4,430 | 4,757 | 6,071 | 9,755 | 5,289 |
| Total, Excluding NH | 4,425 | 4,607 | 5,135 | 6,239 | 4,765 |
TABLE 7.
Expenditure shares of total spending by category and age
| 55–64 | 65–74 | 75–84 | 85+ | Total | |
|---|---|---|---|---|---|
| Hospital, In-patient | 7.14 | 5.06 | 5.15 | 4.46 | 5.77 |
| Nursing Home | 0.71 | 3.34 | 15.55 | 36.19 | 10.23 |
| Doctor | 7.28 | 5.08 | 4.12 | 3.47 | 5.45 |
| Out-Patient Surgery | 2.32 | 1.12 | 0.89 | 0.36 | 1.39 |
| Dental | 7.34 | 7.45 | 5.47 | 2.84 | 6.23 |
| Prescription Drugs | 14.60 | 16.56 | 14.94 | 9.63 | 14.36 |
| Home Health Services | 0.40 | 0.39 | 1.38 | 3.09 | 1.04 |
| Special Facility, Service | 0.68 | 0.44 | 0.79 | 0.84 | 0.67 |
| Helper | 0.48 | 1.04 | 3.08 | 8.36 | 2.45 |
| Non-Medical | 0.13 | 0.43 | 0.73 | 1.63 | 0.68 |
| Hospice | 0.01 | 0.25 | 0.22 | 0.42 | 0.21 |
| Insurance Costs | 57.69 | 57.69 | 45.70 | 26.62 | 50.18 |
| Other | 1.25 | 1.13 | 1.97 | 2.17 | 1.52 |
|
| |||||
| Total | 100.00 | 100.00 | 100.00 | 100.00 | 100.00 |
| Total, Excluding NH | 99.18 | 96.61 | 84.39 | 63.82 | 89.75 |
Table 8 reports the variation in the distribution of total spending with age. The upper panel displays the distribution of annual total out-of-pocket spending from the 2008–12 interviews, and the bottom panel shows the distribution of cumulative spending over the same period. For comparability, in both panels, only individuals with non-missing spending data in all three years are included. In the lower panel, individuals are classified based on their age in 2008. Consistent with the results in the preceding tables, Table 8 displays a steep rise in the risk of large out-of-pocket spending shocks with age for the top age group, a result also found in De Nardi et al. (2015b). Ten per cent of individuals who were age 85 or older in 2008 reported more than $96,000 in out-of-pocket spending over the period covered by the 2008–12 interviews, and five per cent reportedly spent more than $132,000.13
TABLE 8.
Percentiles of total spending by age
| 55–64 | 65–74 | 75–84 | 85+ | Total | |
|---|---|---|---|---|---|
| 10th Percentile | 211 | 795 | 1,060 | 997 | 474 |
| 50th Percentile | 3,096 | 3,726 | 3,881 | 4,146 | 3,578 |
| 90th Percentile | 10,177 | 8,542 | 9,484 | 15,323 | 9,596 |
| 95th Percentile | 13,685 | 10,776 | 12,811 | 26,908 | 13,048 |
| 55–64 | 65–74 | 75–84 | 85+ | Total | |
|---|---|---|---|---|---|
| 10th Percentile | 3,733 | 7,737 | 8,388 | 9,287 | 5,579 |
| 50th Percentile | 21,875 | 24,180 | 25,662 | 28,960 | 23,706 |
| 90th Percentile | 55,877 | 50,308 | 58,738 | 96,981 | 55,835 |
| 95th Percentile | 73,477 | 61,017 | 81,211 | 132,915 | 74,005 |
Note: The spending measure in the upper panel is annual total out-of-pocket medical expenditure. The spending measure in the lower panel is cumulative out-of-pocket spending over the 2008–12 interviews. Cumulative spending is calculated from the non-annualised data. For comparability, both panels include only individuals with non-missing spending data in all three years. In the bottom panel, individuals are classified based on their age in 2008.
The results thus far demonstrate that out-of-pocket spending increases sharply at older ages. An interesting question is whether this pattern is driven primarily by the fact that the elderly are, on average, nearer to the end of life or whether it is simply a feature of old age itself. To explore this question further, the two panels of Table 9 show the age profile of total annual out-of-pocket medical spending separately for the core (upper panel) and exit (lower panel) interview data. The distinction is admittedly imperfect as we make no correction for the fact that individuals appearing in a core interview could have died shortly after the interview. Comparing the panels, it is once again evident that overall spending is much higher in the exit interview data, highlighting the importance of proximity to death. Yet, the risk of extreme expenditure does increase significantly with age in both the core and exit interview data, with the increase being particularly sharp for the oldest age group. These results suggest that aging itself is an important determinant of spending and, furthermore, that out-of-pocket medical spending risk associated with nearness to death may be significantly compounded by aging.14
TABLE 9.
Percentiles of total spending by age: core versus exit interviews
| 55–64 | 65–74 | 75–84 | 85+ | Total | |
|---|---|---|---|---|---|
| Mean | 4,300 | 4,459 | 5,221 | 6,665 | 4,674 |
| 50th Percentile | 2,993 | 3,644 | 3,846 | 4,042 | 3,420 |
| 90th Percentile | 9,765 | 8,481 | 9,197 | 13,448 | 9,310 |
| 95th Percentile | 13,326 | 10,554 | 12,266 | 23,389 | 12,682 |
| 55–64 | 65–74 | 75–84 | 85+ | Total | |
|---|---|---|---|---|---|
| Mean | 12,258 | 11,813 | 14,513 | 19,756 | 15,623 |
| 50th Percentile | 4,513 | 5,363 | 6,118 | 8,391 | 6,328 |
| 90th Percentile | 22,271 | 26,615 | 32,428 | 50,879 | 38,955 |
| 95th Percentile | 47,004 | 44,217 | 59,842 | 73,594 | 62,040 |
Note: The spending measure in both panels is annual total out-of-pocket medical expenditure. The upper panel includes data exclusively from core interviews while the bottom panel is derived solely from exit interview data.
Finally, Table 10 shows the evolution of mean total out-of-pocket spending by age and demographics. Rising exposure to spending risk with age occurs regardless of gender, race/ethnicity, or marital status. On average, across genders and races/ethnicities, mean spending at ages 85+ is more than twice as large as mean spending at ages 55–64. The ratios are somewhat larger for women and non-whites. The groups with the largest mean expenditures at advanced ages are whites, women, and single individuals. Because women tend to survive their husbands, it is single, elderly females who are at the greatest risk of needing to pay out-of-pocket for long-term care in old age.
TABLE 10.
Mean spending by selected demographics and age
| 55–64 | 65–74 | 75–84 | 85+ | Total | |
|---|---|---|---|---|---|
| Male | 4,337 | 4,761 | 5,913 | 8,857 | 5,044 |
| Female | 4,513 | 4,752 | 6,190 | 10,249 | 5,492 |
| Non-Hispanic White | 4,877 | 5,087 | 6,554 | 10,213 | 5,771 |
| Non-Hispanic Black | 2,895 | 3,448 | 3,749 | 6,978 | 3,423 |
| Hispanic | 2,739 | 2,989 | 3,179 | 6,165 | 3,050 |
| Married | 5,031 | 5,115 | 6,094 | 8,311 | 5,358 |
| Single | 3,242 | 4,106 | 6,030 | 10,372 | 5,323 |
V Concentration
Table 11 provides evidence on the very high degree of concentration in out-of-pocket spending, both overall and within each expenditure category. The upper panel reports mean expenditures across percentile ranges of the spending distribution, and the lower panel records the percentage of total spending on a given category that is accounted for by the spenders in each percentile range. For example, from the upper panel, the average, annual total out-of-pocket expenditure by individuals in the bottom half of the distribution was $1,515. Together, these individuals accounted for just 13.8 per cent of total out-of-pocket expenditure in the population. By contrast, the average individual in the top five percentiles of total expenditure spent $30,860 out-of-pocket annually. Individuals in the top five per cent of spending together accounted for 29.8 per cent of total out-of-pocket spending in the population. The top 10 per cent of spenders accounted for 42 per cent of total expenditure.
TABLE 11.
Means and concentration of spending by percentiles of spending and category
| 0–50% | 50–70% | 70–90% | 90–95% | 95–100% | Total | |
|---|---|---|---|---|---|---|
| Hospital, In-patient | 0 | 0 | 19 | 555 | 5,297 | 306 |
| Nursing Home | 0 | 0 | 0 | 0 | 12,838 | 543 |
| Doctor | 3 | 74 | 275 | 819 | 3,003 | 289 |
| Out-Patient Surgery | 0 | 0 | 0 | 87 | 1,166 | 76 |
| Dental | 1 | 110 | 429 | 1,103 | 3,053 | 339 |
| Prescription Drugs | 69 | 485 | 1,155 | 2,418 | 6,091 | 761 |
| Home Health Services | 0 | 0 | 0 | 0 | 1,220 | 56 |
| Special Facility, Service | 0 | 0 | 0 | 1 | 632 | 35 |
| Helper | 0 | 0 | 0 | 0 | 2,981 | 129 |
| Non-Medical | 0 | 0 | 59 | 848 | 9,725 | 515 |
| Hospice | 0 | 0 | 0 | 0 | 3,090 | 159 |
| Insurance Costs | 649 | 2,439 | 4,226 | 6,259 | 10,391 | 2,663 |
| Other | 0 | 0 | 6 | 176 | 2,095 | 114 |
|
| ||||||
| Total | 1,515 | 4,276 | 7,054 | 11,526 | 30,860 | 5,289 |
| Total, Excluding NH | 1,497 | 4,189 | 6,763 | 10,382 | 22,155 | 4,765 |
| 0–50% | 50–70% | 70–90% | 90–95% | 95–100% | Total | |
|---|---|---|---|---|---|---|
| Hospital, In-patient | 0.0 | 0.0 | 1.2 | 9.0 | 89.8 | 100.0 |
| Nursing Home | 0.0 | 0.0 | 0.0 | 0.0 | 100.0 | 100.0 |
| Doctor | 0.4 | 5.7 | 20.9 | 16.1 | 57.0 | 100.0 |
| Out-Patient Surgery | 0.0 | 0.0 | 0.0 | 6.0 | 94.0 | 100.0 |
| Dental | 0.1 | 7.0 | 27.2 | 17.8 | 47.8 | 100.0 |
| Prescription Drugs | 4.6 | 12.9 | 29.9 | 15.5 | 37.1 | 100.0 |
| Home Health Services | 0.0 | 0.0 | 0.0 | 0.0 | 100.0 | 100.0 |
| Special Facility, Service | 0.0 | 0.0 | 0.0 | 0.2 | 99.8 | 100.0 |
| Helper | 0.0 | 0.0 | 0.0 | 0.0 | 100.0 | 100.0 |
| Non-Medical | 0.0 | 0.0 | 2.3 | 8.1 | 89.6 | 100.0 |
| Hospice | 0.0 | 0.0 | 0.0 | 0.0 | 100.0 | 100.0 |
| Insurance Costs | 11.6 | 18.3 | 32.8 | 12.3 | 24.9 | 100.0 |
| Other | 0.0 | 0.0 | 1.0 | 7.8 | 91.3 | 100.0 |
|
| ||||||
| Total | 13.8 | 16.5 | 27.8 | 12.1 | 29.8 | 100.0 |
| Total, Excluding NH | 15.1 | 17.8 | 29.4 | 12.1 | 25.6 | 100.0 |
Note: Column headings indicate percentile ranges of spending for the categories which compose the rows. The upper panel records mean expenditures by category within each of these ranges. The lower panel reports the percentage of total population spending on a given category that is accounted for by the observations in each percentile range. For instance, individuals in the bottom half of total expenditure spend on average $1,515 and together account for 13.8 per cent of total out-of-pocket expenditure in the population.
Within particular spending categories, the degree of concentration is typically much higher. For instance, all nursing home, home care, and helper spending is concentrated in the top five per cent of spenders in those categories, reflecting the relative rarity of such services being paid for out-of-pocket in the general population. The top 10 per cent of spenders account for 100 per cent of spending on out-patient surgery, 97.8 per cent of hospital spending, 73.1 per cent of spending on doctor visits, 65.6 per cent of dental spending, and 52.6 per cent of prescription drug spending.15 The bottom 50 per cent of spenders only contribute significantly to expenditures on insurance premiums, where they account for 11.6 per cent of total spending. Indeed, spending on insurance premiums is the only category where the top 10 per cent account for less than 50 per cent of total spending. Even so, within this category, the top 10 per cent still account for 37.2 per cent of total spending.
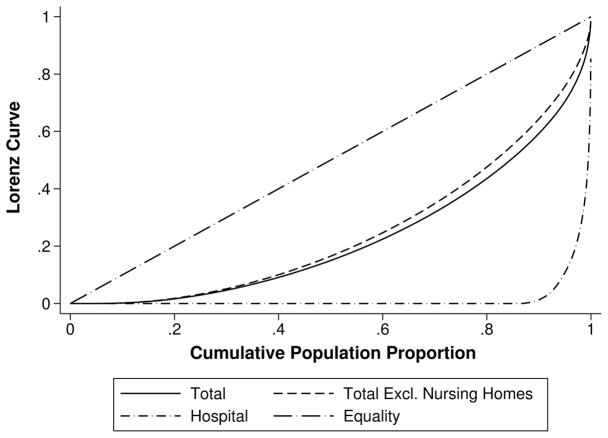
Another way to view this information is through the lens of techniques typically used to study inequality, such as the Lorenz curve and Gini coefficient. Figure 2 presents three Lorenz curves: for total spending, total spending excluding spending on nursing homes, and hospital spending.16 The respective Gini coefficients for these categories are 0.55, 0.51, and 0.97. The high Gini coefficient for hospital spending and the deep bend in its Lorenz curve confirm the highly concentrated distribution of out-of-pocket hospital spending. The high concentration of nursing home spending is suggested by the lower Gini coefficient of total spending when nursing home expenditures are excluded.
FIGURE 2.
Lorenz curves for selected expenditure categories
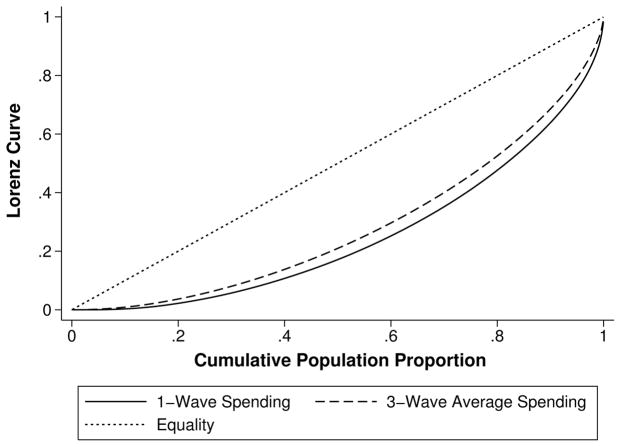
The evidence to this point has indicated that annual out-of-pocket spending tends to be highly concentrated. One interesting question is whether the distribution of spending becomes less concentrated when examined over a longer horizon. To address this question, Figure 3 depicts two Lorenz curves for total spending: one for the pooled interview data from 2008–12 and another for average spending over this period. For comparability, only individuals present in all three waves are included in the construction of both curves. The Gini coefficient for the pooled 1-wave expenditures is 0.50, and the coefficient for the 3-wave average is 0.44. While it is true that concentration is reduced when one averages across a 3-interview—a roughly 6-year—period, the reduction is rather small. As will be shown in Section VI, this fact likely owes to the high degree of persistence in out-of-pocket spending over time.
FIGURE 3.
Lorenz curves for 1-wave spending (2008–12) versus 3-wave average
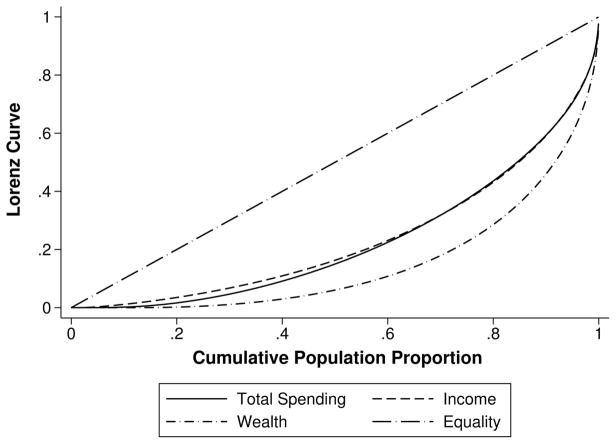
Finally, we compare the concentration of total out-of-pocket spending in our sample to the concentration of income and wealth in the same population.17 This comparison is depicted in Figure 4, which plots Lorenz curves for total out-of-pocket spending, income, and wealth. The distribution of spending in the population turns out to be strikingly similar to the distribution of income, and both of these are relatively more evenly distributed than net wealth. The Gini coefficients for spending, income, and wealth are, respectively, 0.55, 0.52, and 0.70.
FIGURE 4.
Lorenz curves for spending versus income and wealth
VI Persistence
A chief advantage of the HRS relative to other surveys with information on out-of-pocket medical spending is the length of the HRS panel. To capitalise on that important dimension of the HRS, in this section we use data from the survey years 1998–2012. We select 1998 because it is the wave in which the HRS becomes approximately representative of the American population. Over the period 1998–2012, the HRS provides a fairly consistent measure of total out-of-pocket spending covering roughly 16 years. By comparison, the MCBS has panels on medical spending only up to three years long.
Table 12 reports the correlation coefficients for three categories of out-of-pocket spending in both levels and logs across many survey years of the HRS. The left two columns display the correlation in total out-of-pocket spending over 1998–2012, the middle two columns contain the correlations for total spending excluding nursing home spending, and the rightmost two columns record the results for hospital spending alone. The latter four columns use data only from 2002–12 because hospital and nursing home spending were not measured separately in the HRS prior to 2002. Recall that before taking logs, we bottom-code spending for each category in each wave at 10 per cent of its mean in that wave.
TABLE 12.
Correlation of out-of-pocket spending across time
| Correlation of Year t with: | Total | Total Ex. NH | Hospital | |||
|---|---|---|---|---|---|---|
|
| ||||||
| Levels | Logs | Levels | Logs | Levels | Logs | |
| Year t – 2 | 0.374 | 0.606 | 0.306 | 0.634 | 0.0988 | 0.228 |
| Year t – 4 | 0.239 | 0.500 | 0.217 | 0.549 | 0.0183 | 0.139 |
| Year t – 6 | 0.177 | 0.442 | 0.192 | 0.494 | 0.0208 | 0.110 |
| Year t – 8 | 0.140 | 0.392 | 0.177 | 0.444 | 0.0458 | 0.0964 |
| Year t – 10 | 0.119 | 0.343 | 0.146 | 0.409 | 0.0204 | 0.0800 |
| Year t – 12 | 0.100 | 0.295 | ||||
| Year t – 14 | 0.0747 | 0.275 | ||||
Note: The three categories are total out-of-pocket medical expenditures (left two columns), total expenditures minus nursing home expenditures (middle two columns), and hospital expenditures (right two columns). We use data from all core and exit interviews from the 1998–2012 surveys to calculate correlations for total spending, but we use only data from 2002–12 to calculate correlations for total spending excluding nursing homes and for hospital spending. The reason is that nursing home and hospital spending are reported in the HRS as a single combined amount prior to the 2002 survey wave and are not easily disentangled. Before taking logs, expenditures were bottom-coded at 10 per cent of mean spending on that category. This was done wave-by-wave, so for example, observations for hospital spending from the 1998 interview data are bottom-coded at 10 per cent of the mean hospital expenditure taken over all observations in 1998.
The reported correlation coefficients demonstrate the relatively high persistence over time for total out-of-pocket spending in both levels and logs. The correlation in expenditures between two adjacent survey waves—that is, between year t and year t – 2—is 0.374 in levels and 0.606 in logs. Serial correlation declines over time, but correlation persists even several years apart. For instance, the correlation in reported spending at interviews 6 years apart is 0.177 in levels and 0.442 in logs. Results are similar for total spending excluding expenditures on nursing homes. By contrast, hospital spending displays almost no serial correlation.18
The three panels of Table 13 report three transition matrices for five quintiles of total out-of-pocket spending between survey waves of the HRS. The top panel presents a one-wave—approximately two-year—transition matrix. Each (i, j) cell in this panel represents that probability of transitioning from quintile i at survey wave t – 1 to quintile j at survey wave t. The middle and lower panels report the analogous three-wave and five-wave transition matrices, respectively.
TABLE 13.
Transition matrices between quintiles of total spending
| Spending Quintile (t-1) | Spending Quintile (t) | |||||
|---|---|---|---|---|---|---|
| Bottom | 2nd | 3rd | 4th | Top | Total | |
| Bottom | 58.1 | 21.9 | 9.7 | 5.4 | 4.8 | 100.0 |
| 2nd | 18.0 | 37.7 | 23.5 | 12.1 | 8.6 | 100.0 |
| 3rd | 8.3 | 20.8 | 33.5 | 24.0 | 13.3 | 100.0 |
| 4th | 4.6 | 10.7 | 21.8 | 37.0 | 25.9 | 100.0 |
| Top | 4.0 | 6.4 | 11.8 | 24.5 | 53.2 | 100.0 |
|
| ||||||
| Total | 18.8 | 19.8 | 20.3 | 20.6 | 20.5 | 100.0 |
| Spending Quintile (t-3) | Spending Quintile (t) | |||||
|---|---|---|---|---|---|---|
| Bottom | 2nd | 3rd | 4th | Top | Total | |
| Bottom | 43.1 | 24.8 | 14.5 | 9.7 | 8.0 | 100.0 |
| 2nd | 15.3 | 30.3 | 24.0 | 16.5 | 13.9 | 100.0 |
| 3rd | 9.4 | 19.7 | 26.6 | 25.4 | 19.0 | 100.0 |
| 4th | 5.9 | 12.4 | 22.0 | 31.2 | 28.5 | 100.0 |
| Top | 5.3 | 9.0 | 15.6 | 26.2 | 43.8 | 100.0 |
|
| ||||||
| Total | 16.1 | 19.6 | 20.8 | 21.6 | 21.9 | 100.0 |
| Spending Quintile (t-5) | Spending Quintile (t) | |||||
|---|---|---|---|---|---|---|
| Bottom | 2nd | 3rd | 4th | Top | Total | |
| Bottom | 31.7 | 25.9 | 17.9 | 13.6 | 10.8 | 100.0 |
| 2nd | 14.4 | 24.4 | 24.6 | 19.4 | 17.3 | 100.0 |
| 3rd | 8.9 | 19.0 | 25.5 | 25.0 | 21.6 | 100.0 |
| 4th | 6.5 | 13.3 | 21.4 | 29.2 | 29.5 | 100.0 |
| Top | 5.5 | 10.8 | 18.1 | 26.2 | 39.4 | 100.0 |
|
| ||||||
| Total | 13.9 | 19.1 | 21.7 | 22.5 | 22.9 | 100.0 |
Note: The three panels display transition matrices for five quintiles of total out-of-pocket spending between waves of the HRS. The panels include all observations from core and exit interviews from the 1998–2012 waves. The top panel displays the 2-year (1-interview-wave) transition matrix. In the top panel, each (i, j) cell represents the probability of transitioning from quintile i at survey wave t – 1 to quintile j at survey wave t. The middle and bottom panels display the analogous 6-year (3-interview-wave) and 10-year (5-interview-wave) matrices.
The results in Table 13 confirm the strong persistence in total spending over time. The top panel indicates that 53.2 per cent of individuals in the top quintile of spending in the previous wave will be in the top quintile in the current wave. Among individuals who were in the bottom quintile in the last wave, 58.1 per cent will remain there in the current wave. This finding persists over a longer horizon. Among individuals in the top quintile six years—or three survey waves—earlier, 43.8 remain in the top quintile in the current wave (middle panel). Over 10 years, the analogous figure is 39.4 per cent (bottom panel).
In results not shown, among individuals in the top quintile of total out-of-pocket spending excluding nursing home costs in the previous interview, 54.0 per cent remain in the top quintile in the current wave. Comparable figures for hospital spending could not be presented because the degree of concentration in that category is so great that constructing hospital spending quintiles is not possible.
VII Income and wealth gradients
Another benefit of working with the HRS relative to other datasets with information on out-of-pocket medical spending is that the HRS has excellent measures of both household wealth and income. In this paper, wealth refers to total household net worth including equity from a secondary residence, and income refers to household income including both asset and non-asset income. These measures have been converted from household- to individual-level measures using the procedure in Michael and Citro (1995)—that is, by dividing the reported amounts by the number of adults in the household raised to the power 0.7. As income and wealth are not measured in the exit interviews, these variables are drawn from preceding core interviews. If these data are missing from the core interview immediately preceding the exit interview, data from earlier core interviews is used.19
Table 14 shows the gradients of mean total out-of-pocket spending and the degree of spending concentration by income and wealth quintiles. While neither concentration nor mean spending appears very responsive to income above the bottom income quintile, both increase monotonically with wealth. However, even for wealth, the increase in mean spending across the quintiles is not particularly sharp. Moreover, the degree of concentration, while much greater for wealth than income, is also perhaps lower than one might expect. Individuals in the top wealth quintile account for 27.2 per cent of total out-of-pocket medical spending while those in the top income quintile account for 22.9 per cent. These numbers are not all that far from income and wealth neutrality, which would imply that spending is 20 per cent in each of the quintiles.
TABLE 14.
Mean total spending and concentration by income and wealth quintiles
| Quintile | Income | Wealth | ||
|---|---|---|---|---|
|
| ||||
| Mean Expenditure | Percent of Total | Mean Expenditure | Percent of Total | |
| Bottom | 3,974 | 15 | 4,089 | 15.5 |
| Second | 5,503 | 20.8 | 4,404 | 16.7 |
| Third | 5,700 | 21.6 | 5,125 | 19.4 |
| Fourth | 5,234 | 19.8 | 5,601 | 21.2 |
| Top | 6,031 | 22.8 | 7,225 | 27.3 |
Table 15 provides the breakdown of the income gradient in mean spending by the various expenditure categories available in the HRS. The mean total spending of those in the highest quintile is 1.54 times greater than those in the lowest quintile. Excluding nursing home expenses, the ratio is 1.73. For the individual spending categories, few patterns are discernible. On the one hand, individuals in top quintile spend 0.53 times as much on hospitals and 0.41 times as much on nursing homes. On the other hand, those in the top quintile spend 2.4 times more on insurance, 3 times more on dental expenses, and 3.2 times more on non-medical health expenses. The results are quite similar for wealth quintiles.20
TABLE 15.
Mean spending by category and income quintile
| Category | Income Quintile
|
||||
|---|---|---|---|---|---|
| Bottom | Second | Third | Fourth | Top | |
| Hospital, In-patient | 363 | 314 | 430 | 236 | 189 |
| Nursing Home | 641 | 811 | 657 | 380 | 229 |
| Doctor | 241 | 279 | 303 | 291 | 331 |
| Out-Patient Surgery | 48 | 71 | 74 | 76 | 108 |
| Dental | 176 | 272 | 338 | 379 | 521 |
| Prescription Drugs | 680 | 866 | 874 | 715 | 669 |
| Home Health Services | 71 | 91 | 55 | 35 | 29 |
| Special Facility, Service | 32 | 36 | 23 | 31 | 55 |
| Helper | 125 | 186 | 140 | 87 | 109 |
| Non-Medical | 307 | 515 | 616 | 733 | 731 |
| Hospice | 160 | 199 | 110 | 199 | 68 |
| Insurance Costs | 1,522 | 2,452 | 2,727 | 2,909 | 3,694 |
| Other | 115 | 138 | 88 | 107 | 122 |
|
| |||||
| Total | 3,974 | 5,503 | 5,700 | 5,234 | 6,031 |
| Total, Excluding NH | 3,371 | 4,714 | 5,057 | 4,864 | 5,806 |
The interpretation of these results is subject to at least two important caveats. First, the relationship in our data between medical spending and income or wealth should not be understood as representing an elasticity. Our results are based on out-of-pocket medical expenditure data rather than data on total expenditures or the quantity of health care services consumed. This feature of the data is problematic because individuals face different prices for medical services, and furthermore, these prices are both unobservable to us and likely to be correlated with income and wealth. Low-income individuals, for example, are more likely to have their costs covered by Medicaid. Conversely, wealthy individuals may have more comprehensive health insurance coverage.
A second caveat about the results is that they may be biased somewhat by systematic differences in health status across the different income quintiles. To partially control for the influence of health status, Table 16 replicates the income gradients by expenditure category exclusively using the data from the exit interviews. As all individuals in these interviews are near death, their health statuses should be more similar. Comparing the two sets of results, the influence of health is readily apparent. In the exit interview data, those in the top income quintile spend more than those in the lowest quintile for all categories save for hospital expenditures, where they spend just 0.93 times as much. There are strong gradients with income in most categories (ratio of means, highest-to-lowest quintile, in parentheses): examples include nursing homes (1.4), prescription drugs (2.6), helper (2.8), and insurance costs (2.9). Total spending is 1.9 times larger for those in the highest income quintile relative to those in the lowest quintile.
TABLE 16.
Mean spending by category and income quintile, exit interviews 2008–12
| Category | Income Quintile
|
||||
|---|---|---|---|---|---|
| Bottom | Second | Third | Fourth | Top | |
| Hospital, In-patient | 1,683 | 1,749 | 4,346 | 1,568 | 1,243 |
| Nursing Home | 3,828 | 5,780 | 6,161 | 5,919 | 4,558 |
| Doctor | 684 | 839 | 1,192 | 933 | 898 |
| Out-Patient Surgery | 36 | 159 | 96 | 36 | 43 |
| Dental | 147 | 255 | 323 | 339 | 682 |
| Prescription Drugs | 912 | 1,463 | 1,846 | 1,621 | 2,315 |
| Home Health Services | 447 | 832 | 720 | 468 | 661 |
| Special Facility, Service | 72 | 109 | 100 | 160 | 376 |
| Helper | 990 | 1,801 | 1,660 | 1,587 | 3,250 |
| Non-Medical | 307 | 515 | 616 | 733 | 731 |
| Hospice | 160 | 199 | 110 | 199 | 68 |
| Insurance Costs | 1,305 | 2,231 | 2,552 | 2,889 | 3,465 |
| Other | 479 | 611 | 421 | 778 | 1,061 |
|
| |||||
| Total | 10,908 | 16,251 | 19,927 | 17,057 | 19,102 |
| Total, Excluding NH | 7,080 | 10,508 | 13,766 | 11,137 | 14,544 |
Table 17 shows how the income and wealth gradients of mean total out-of-pocket spending vary across four age groups: 55–64, 65–74, 75–84, and 85+. The results demonstrate that gradients of spending with income and wealth exist across all age groups. If anything, the influence of income seems to grow with age: the ratio of mean spending by those in the top income quintile to those in the bottom at ages 55–64 is 1.83, and the same ratio is 2.0 for those ages 85+. Interestingly, the opposite pattern seems to hold for the gradient of mean total spending with wealth.
TABLE 17.
Mean total spending by income and wealth quintiles and age
| 55–64 | 65–74 | 75–84 | 85+ | Total | |
|---|---|---|---|---|---|
| Income Q1 | 2,892 | 3,406 | 4,315 | 7,444 | 3,974 |
| Income Q2 | 3,826 | 4,561 | 6,141 | 9,900 | 5,503 |
| Income Q3 | 4,634 | 4,917 | 6,747 | 10,790 | 5,700 |
| Income Q4 | 4,562 | 4,794 | 6,457 | 11,494 | 5,234 |
| Income Q5 | 5,325 | 6,262 | 8,659 | 13,761 | 6,031 |
| Wealth Q1 | 3,255 | 3,318 | 4,715 | 8,679 | 4,089 |
| Wealth Q2 | 3,746 | 3,927 | 5,070 | 8,527 | 4,404 |
| Wealth Q3 | 4,209 | 4,722 | 5,735 | 9,671 | 5,125 |
| Wealth Q4 | 4,791 | 4,956 | 6,319 | 10,242 | 5,601 |
| Wealth Q5 | 6,539 | 6,361 | 8,139 | 12,104 | 7,225 |
VIII Insurance costs
Due to the particular importance of insurance premiums as an expenditure category and the high quality of the measures of such spending in the HRS relative to other surveys, we devote a separate section to the role of insurance. As was discussed above, insurance costs are a persistently large component of out-of-pocket spending across age groups, accounting for 50 per cent of all out-of-pocket spending in our sample (Table 5). Though somewhat less concentrated than other categories, insurance costs display a significant gradient with both income and wealth. In this section, we disaggregate insurance costs into its five components—Medicare Part B; Medicare Advantage (HMO); Medicare Part D prescription drug coverage; private insurance, including Medigap; and long-term care insurance—and analyze their distribution, variation with age, and sensitivity to income.21
Table 18 summarises the distribution of expenditures on insurance, reporting the means and various percentiles of spending for each of the five insurance categories available in the HRS. The largest mean insurance expense is for private insurance. For individuals younger than 65, this category typically represents employee contributions to employer-provided health insurance. For older individuals, these are Medigap supplemental coverage plans. Private insurance is also the most variable category: though the median individual spends just $437 on private coverage, 10 per cent of individuals spend $4,666 or more, and five per cent spend $5,920 or more annually on private coverage. This is likely the consequence of differences in how much their current or past employer pays for their health insurance plan, rather than variations in the cost of the plan per se. As can also be seen in the table, few individuals hold long-term care insurance though the expenses of those who do hold such policies can be large.22
TABLE 18.
Summary of expenditure on insurance premiums by type of insurance
| Mean | 10th | 50th | 75th | 90th | 95th | 99th | |
|---|---|---|---|---|---|---|---|
| Medicare Part B | 587 | 0 | 0 | 1,248 | 1,417 | 1,417 | 2,832 |
| Medicare HMO | 121 | 0 | 0 | 0 | 257 | 848 | 2,395 |
| Medicare Part D | 102 | 0 | 0 | 0 | 475 | 663 | 1,284 |
| Private, Medigap | 1,664 | 0 | 437 | 2,617 | 4,666 | 5,920 | 12,841 |
| Long-term Care | 226 | 0 | 0 | 0 | 189 | 1,930 | 4,280 |
|
| |||||||
| Insurance Costs | 2,663 | 0 | 1,916 | 3,852 | 6,086 | 7,595 | 13,505 |
The age profiles of mean spending by insurance category appear in Table 19. Interestingly, mean total insurance costs are roughly constant with age. Though private insurance spending falls at Medicare eligibility—from a mean of $2,320 for individuals aged 55–64 to just $1,249 for individuals aged 65–74—this decline is offset by a rise in other categories, notably Medicare Part B premiums.
TABLE 19.
Spending on insurance premiums by age
| 55–64 | 65–74 | 75–84 | 85+ | Total | |
|---|---|---|---|---|---|
| Medicare Part B | 79 | 952 | 1,135 | 1,074 | 587 |
| Medicare HMO | 20 | 184 | 219 | 224 | 121 |
| Medicare Part D | 18 | 171 | 184 | 182 | 102 |
| Private, Medigap | 2,320 | 1,249 | 1,024 | 1,000 | 1,664 |
| Long-term Care | 140 | 273 | 338 | 281 | 226 |
|
| |||||
| Insurance Costs | 2,574 | 2,748 | 2,779 | 2,603 | 2,663 |
Table 20 reports the gradient of insurance spending across income quintiles. In general, no components of Medicare spending appear to be correlated with income.23 In contrast, both private insurance and long-term care insurance premiums seem to be highly sensitive to income. On the basis of the means in Table 20, those in the highest income quintile spend 3.9 times more on private insurance and 5.7 times more on long-term care insurance.
TABLE 20.
Spending on insurance premiums by income quintiles
| Category | Income Quintile
|
||||
|---|---|---|---|---|---|
| Bottom | Second | Third | Fourth | Top | |
| Medicare Part B | 522 | 829 | 710 | 468 | 412 |
| Medicare HMO | 154 | 170 | 139 | 83 | 59 |
| Medicare Part D | 116 | 150 | 116 | 72 | 61 |
| Private, Medigap | 697 | 1,198 | 1,593 | 2,064 | 2,761 |
| Long-term Care | 68 | 160 | 225 | 254 | 421 |
|
| |||||
| Insurance Costs | 1,522 | 2,452 | 2,727 | 2,909 | 3,694 |
Figure 5 compares mean spending over the life-cycle among those with different types of insurance. This figure captures both the direct effect of insurance on spending as well as the influence of other covariates—such as income—that are systematically related to both spending and the choice of insurance coverage. The figure plots three-year moving averages of total out-of-pocket medical spending by age for each of seven different insurance/age categories. Across all ages, those with private insurance (under 65) or private insurance in addition to Medicare (65 and older) have the highest average spending. Individuals with non-Medicare government insurance (under 65) or with both Medicare and Medicaid (65 and older) have the lowest spending. Spending rises gradually from age 65 through one’s early eighties after which it increases steeply. The increases are largest for individuals with Medicare or Medicare in addition to private insurance. In comparison, the increase in spending is muted for individuals who report receiving Medicaid coverage at any point between interviews, consistent with Medicaid coverage of long-term care needs, which rise with age.
FIGURE 5.
Mean total spending by insurance status and age
Note: Three-year moving average. A given cell is dropped when the number of observations in that cell and in the two adjacent cells combined is less than 50. This results in 14 observations being dropped.
IX Spending at the very end of life
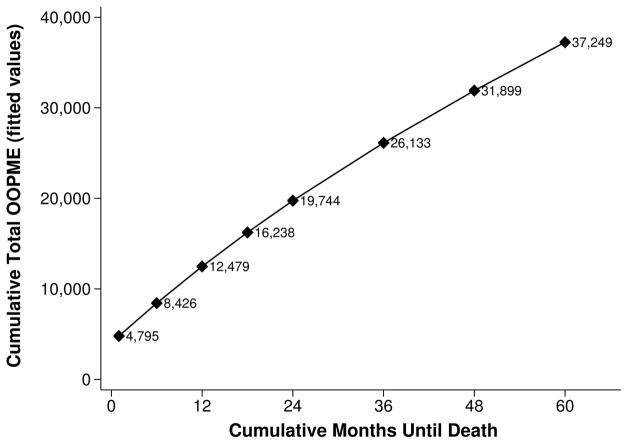
The final set of results in this paper attempt to capture the extent to which spending near the end of life is dominated by spending over the final months or year of life. To this end, Figure 6 plots the fitted values from a regression of cumulative total out-of-pocket spending until death on a constant plus a quartic in the number of months until death. Only decedents whose survivors provided an exit interview are included in the analysis. The figure uses data from all interviews from 1998–2012. The figure indicates that on average decedents spent $8,426 out-of-pocket on medical expenses over their last six months of life and $12,479 over their final year. Yet, the curve for mean cumulative spending is surprisingly linear with the number of months until death. Spending over the last year of life constitutes 63 per cent of average expenditures over one’s final two years of life, and it represents just 34 per cent of spending over the final five years. While the contribution of the final year of life is quite significant, considerable out-of-pocket expenditures also occur further from death.
FIGURE 6.
Spending by months until death
Note: Figure plots the fitted values from a (weighted least squares) regression of cumulative (not annualised) total out-of-pocket spending until death on a constant and a 4th order polynomial of the cumulative number of months until death. No other covariates are included. Data from core and exit interviews from the 1998–2012 waves are used, and only respondents whose survivors provided an exit interview are included in the estimation.
X Discussion and conclusion
In this paper, we have documented patterns of out-of-pocket medical expenditures in the United States, with a particular focus on end-of-life expenditures. We used an imputation approach that seeks to avoid the biases inherent in either counting outlandish responses as real, or that shrinks the economically important but rare outliers reflecting extremely high costs. While other studies have examined the magnitude of such spending (e.g., De Nardi et al. 2015b; De Nardi, French, and Jones 2013; Goldman, Zissimopoulos, and Lu 2011; Hurd and Rohwedder 2009), here we consider both levels and the distribution of out-of-pocket spending over time in far greater detail, and in a way that can be compared internationally.
How do these spending measures compare with other countries? An early study showed U.S. residents paying a higher fraction of health care costs out-of-pocket (Wagstaff and Van Doorslaer, 1992), which, coupled with the much higher level of health care spending, implies out-of-pocket spending in dollar terms far in excess of other countries. A more recent 2011 OECD study comparing out-of-pocket expenditures, however, shows average out-of-pocket spending in 2009 to be just 3.1 percent of total consumption in the U.S., below the average of 3.2 in the OECD. (OECD, 2011). Yet in this same study, micro-level data showed the distribution of medical expenses in the U.S. appeared to have a larger variance. For example, 45 per cent of high-income and 29 per cent of low-income households in 2010 experienced an out-of-pocket medical expense in excess of $1000 in the U.S. Comparable estimates for the Netherlands were 11 per cent and seven per cent; for Germany, 10 per cent and five per cent; and for the U.K., zero per cent for both income groups (OECD, 2011). Of course, per capita GDP is somewhat higher in the U.S., but not so much higher to explain these sharp differences across countries. Switzerland is one potential exception to this rule: the corresponding percentage of individuals spending more than $1000 is still lower than the U.S. (34 per cent and 20 per cent for high and low income households, respectively), but the study also reports out-of-pocket spending as a percentage of final consumption to be higher in Switzerland (6.2 per cent) than the U.S. (3.1 per cent) (OECD, 2011).
With respect to the studies in this issue, estimates of out-of-pocket expenditures are typically available only for aggregate measures of health spending. In the Netherlands, for example, per-capita expenditures (including home health care) are about the same as in the U.S. Yet the low overall percentage of out-of-pocket spending (4.6 per cent) implies average out-of-pocket expenditures less than half that in the U.S. (Bakx et al., 2015). Christensen, Gortz, and Kallestrup-Lamb (2015) provide considerable detail about out-of-pocket spending in Denmark, and while the estimates do not include nursing and home health care, out-of-pocket expenditures near the end of life are very modest for the elderly: just $385 for males and $429 for females. By contrast, out-of-pocket spending near the end of life in the U.S. is considerably larger for hospitals ($2,176), prescription drugs ($1,453), and physician payments ($878); see Table 4.24
One recent study that might appear to contradict these results compares spending in the last six months across cancer patients in several developed countries (Bekelman et al., 2016). Their estimate of inpatient hospital spending in the last six months in the U.S. ($18,500) is higher than the Netherlands ($10,936) and the U.K. ($9,342) but less than Canada ($21,840) and Norway ($19,783). However, their results do not report out-of-pocket spending separately and are limited to utilization in the hospital setting. More importantly, the dollar amounts are adjusted using an OECD price index that adjusts away the much higher prices of health care in the U.S. (for both inpatient and outpatient care). From their results, it is thus difficult to measure how, for example, the loss of a spouse might affect a widow or widower’s financial security.25
In sum, there is remarkably little evidence on the distribution and characteristics of out-of-pocket spending in other countries, but what little evidence there is suggests that the U.S. is an outlier with regard to the extent to which it exposes its citizens to the risk of out-of-pocket expenditures. Additional studies of the microeconomics of out-of-pocket expenditures would be valuable for assessing equity in these health care systems.
Footnotes
Proxy respondents are most likely to be a spouse or child. If neither is available, other knowledgeable individuals may provide answers.
As we discuss in the conclusion, OECD statistics on aggregate out-of-pocket expenditures across countries show the U.S. near the median, but spending in the U.S. appears to exhibit far more variability, potentially placing more households at serious financial risk.
Note that throughout this document the label “hospital” is used in reference to in-patient hospital spending only and excludes out-patient expenditures.
Spending on Medicare Part B is not recorded in the HRS. We impute spending on the basis of whether the respondent was reported to have been covered by Part B, and we adjust premiums using information on household income and marital status and whether the respondent was covered by Medicaid.
In 2010, the question regarding “other” spending category was added to the core interviews while the question on “non-medical” expenditures was eliminated from the exit interviews and replaced with a more specific—but not entirely identical—question on home modifications. Throughout this paper, we combine the non-medical (2008 and earlier) and home modification (2010 and later) categories into a single expenditure category which we label “Non-Medical.”
There are a few important exceptions. For new interviewees, the survey requests spending over the previous two years. For the “helpers” category, core interviews ask for spending in the “last month” while exit interviews ask for a “typical month.” We assume that helper expenditures take place for 4 months or the time elapsed between interviews, whichever is shorter. In addition, insurance payments may be reported at various frequencies—e.g. monthly, quarterly—and respondents are asked to report average monthly prescription drug expenditures.
These bracket imputations are not conditioned on any other covariates. Exceptions occur for helpers, where bracket imputations taken into account the number of helpers, and for insurance premiums, where the imputations distinguish between individuals with a single plan versus those with multiple plans.
The survey years 2002–12 are used because it is only beginning in 2002 that hospital, nursing home, and doctor spending are each reported individually. Prior to 2002, hospital and nursing home spending are reported as a single amount, as are doctor, out-patient surgery, and dental spending.
Nursing home residents are also assigned zero weight. In these cases, as well, we use the most recent non-zero weight from the previous core interviews.
Recall from the preceding discussion that two categories—non-medical spending (2008 and earlier) and home modification spending (2010 and later)—have been combined into a single category, labeled “Non-Medical” in the tables.
These figures do not appear in the tables. They were calculated from the annualised spending data without using sample weights.
These expenditure shares were computed by summing out-of-pocket expenditures in each category across observations and dividing by the sum of total out-of-pocket spending.
On average, the number of months elapsed between core interviews is 24, and the number between the final core interview and the exit interview is 15. Therefore, for individuals who were still alive in 2012, cumulative spending took place on average over 6 years. For those who died between the 2010 and 2012 interviews, the average duration was 5 years and 3 months. Note, however, that spending is reported for the period since the previous interview for re-interviewees. As a result, for individuals who missed one or more interviews leading up to the 2008 interview, cumulative spending may reflect expenditure over a period longer than 6 years. On the other hand, for individuals who died shortly after their 2010 core interview, the reporting period will be closer to 4 years.
To analyze more formally how the age gradient of out-of-pocket medical spending is affected by controlling for proximity to death, for our sample of decedents, we regressed total spending on a constant, the set of age category dummies (ages 65–74, 75–84, and 85+), and a quartic in the number of months until death, and we compared these results to a specification that excluded the controls for nearness to death. Both regressions were weighted using household weights. (Results are not shown.) We found that the inclusion of the additional controls flattens the gradient of spending with age. The coefficient on the 85+ age category decreases significantly from $6,451 to $4,604, and the coefficient on the 75–84 age category falls insignificantly from $1,877 to $1,423. The coefficient estimates on these two categories are significant at the 1% level in both specifications. The results support the conclusion that both aging and time to death have independent and significant effects on out-of-pocket spending.
The high degree of concentration in particular categories also owes to the fact that certain services are infrequently used. For example, nursing home use was reported in only 7% of our observations, and home health care was reported in just over 10%. In each case, an even smaller subset of those using the service actually paid for out-of-pocket: just 3.4% paid for nursing homes and 2.3% paid for home health care. On the other hand, high concentration of spending does not necessarily mean that the use of the service is highly concentrated. For instance, despite the fact that out-of-pocket spending on hospital stays is almost entirely concentrated in the top 10% of spenders, hospital utilisation is reported in nearly 30% of our observations.
Each (x, y) coordinate along the curve represents the cumulative proportion of total spending (on the y-axis) accounted for by the cumulative proportion of the population on the x-axis. The 45 degree line represents perfect equality. Curves closer to the 45 degree line are more equal, and those that bend further toward the south-east corner are less equal.
For more information on the definition of the income and wealth variables used in this paper, refer to the discussion in Section VII.
That the correlations are higher in logs than in levels is not the result of bottom-coding. Rather, it arises from the log transformation. We are measuring correlation using Pearson’s correlation, which posits a linear relationship between current and lagged out-of-pocket spending. Non-linear transformations, such as taking logs, will generally alter this measure of correlation. The higher correlations in logs than in levels suggests that the relationship between current and lagged spending is non-linear. In addition, the distribution of medical spending is highly skewed by large outliers. Taking logs squashes the distribution, which reduces the influence of outliers and may also increase the correlations.
The exit interviews do include a measure of the total value of the decedent’s estate. However, unlike our core income and wealth measures, which we take from the RAND HRS data, imputations are not yet available for the exit interview data. A second concern is that, for married couples, the estate data are likely to measure only a portion of the household’s wealth over the interval. For these reasons, and to maintain consistency with our income measure that is not available in the exit interviews, we opt to use the core wealth measure from the earlier core interviews.
Mean total spending by those in the top wealth quintile is 1.74 times greater than those in the lowest quintile. Excluding nursing home spending, it is twice as large. Insurance spending is 2.9 times larger, and non-medical spending is 3.2 times greater.
Recall that spending on Medicare Part B is not recorded in the HRS and must be imputed. See footnote 4 for details. In addition, bear in mind that the interpretation of the results in this section may be affected by the fact that the majority of individuals younger than 65 will have zero expenditures on the Medicare insurance categories.
In our data, roughly 11 per cent of individuals hold long-term care insurance. The median spending among these individuals is approximately $1,750 though 10 per cent spend over $4,000.
Although Medicare Part B premiums vary programmatically with income, this relationship is offset by the age composition of the sample, which includes many individuals who are not yet age-eligible for Medicare. In particular, individuals in the higher income quintiles are younger on average and thus less likely to be eligible for (and hence, to pay premiums for) Medicare, meaning that the upper quintiles contain more instances of zero expenditure on Medicare.
The Danish data are for the last 12 months of life whereas the HRS exit interview is for deaths that occurred since the last survey, which averages around 15 months.
One might argue that the higher levels of U.S. out-of-pocket spending could be justified by the greater health benefits they provide. For patients with very advanced cancers, most patients express a preference for dying at home. Indeed, one randomized trial found patients with metastatic cancer treated with early palliative care lived longer than the control group treated more intensively (Temel et al., 2010). Bekelman et al. (2016) showed that fewer cancer patients in the U.S. died in hospital, but more were admitted during their last 6 months to an ICU, suggesting mixed evidence on U.S. end-of-life care relative to that in other countries.
Contributor Information
Sean Fahle, SUNY Buffalo.
Kathleen McGarry, UCLA.
Jonathan Skinner, Dartmouth.
References
- Bakx Pieter, Douven Rudy, O’Donnell Owen, van Doorslaer Eddy. Spending on Health Care in the Netherlands: Not Going So Dutch? 2015 [Google Scholar]
- Banks James, Blundell Richard, Levell Peter, Smith James P. Tech rep, RAND Working Paper WR-1100. 2015. Life-cycle Consumption Patterns at Older Ages in the U.S. and the U.K. [Google Scholar]
- Bekelman Justin E, Halpern Scott D, Blankart Carl Rudolf, Bynum Julie P, Cohen Joachim, Fowler Robert, Kaasa Stein, Kwietniewski Lukas, Melberg Hans Olav, Onwuteaka-Philipsen Bregje, et al. Comparison of Site of Death, Health Care Utilization, and Hospital Expenditures for Patients Dying with Cancer in 7 Developed Countries. JAMA. 2016;315(3):272–283. doi: 10.1001/jama.2015.18603. [DOI] [PubMed] [Google Scholar]
- Christensen Bent Jesper, Gortz Mette, Kallestrup-Lamb Malene. Medical Spending in Denmark 2015 [Google Scholar]
- De Nardi M, French Eric, Jones JB. Medicaid Insurance in Old Age. 2013 doi: 10.1257/aer.20140015. [DOI] [PubMed] [Google Scholar]
- De Nardi Mariacristina, French Eric, Jones John Bailey. Why Do the Elderly Save? The Role of Medical Expenses. Journal of Political Economy. 2010;118(1):39–75. [Google Scholar]
- De Nardi Mariacristina, French Eric, Jones John Bailey, McCauley Jeremy. Medical Spending of the U.S. Elderly. 2015a doi: 10.1111/j.1475-5890.2016.12106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Nardi Mariacristina, French Eric, Jones John Bailey, McCauley Jeremy. Tech rep, National Bureau of Economic Research. 2015b. Medical Spending of the U.S. Elderly. [Google Scholar]
- French Eric, Jones John Bailey. On the Distribution and Dynamics of Health Care Costs. Journal of Applied Econometrics. 2004;19(6):705–721. [Google Scholar]
- Goldman D, Zissimopoulos J, Lu Y. Medical Expenditure Measures in the Health and Retirement Study. Forum Health Econ Policy. 2011;14(3) doi: 10.2202/1558-9544.1267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hubbard R Glenn, Skinner Jonathan, Zeldes Stephen P. Precautionary Saving and Social Insurance. Journal of Political Economy. 1995;103(2):360–99. [Google Scholar]
- Hurd Michael D, Rohwedder Susann. The Level and Risk of Out-of-Pocket Health Care Spending. University of Michigan Retirement Research Center, Working Paper. 2009;(218) [Google Scholar]
- Kelley Amy S, McGarry Kathleen, Gorges Rebecca, Skinner Jonathan S. The Burden of Health Care Costs for Patients With Dementia in the Last 5 Years of Life. Annals of internal medicine. 2015;163(10):729–736. doi: 10.7326/M15-0381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marshall Samuel, McGarry Kathleen, Skinner Jonathan S. The Risk of Out-of-Pocket Health Care Expenditure at the End of Life. Explorations in the Economics of Aging. 2011 Mar;:101–128. [Google Scholar]
- Michael Robert T, Citro Constance F. Measuring Poverty: A New Approach. National Academies Press; 1995. [Google Scholar]
- OECD. Burden of Out of Pocket Medical Expenditures 2011 [Google Scholar]
- Temel Jennifer S, Greer Joseph A, Muzikansky Alona, Gallagher Emily R, Admane Sonal, Jackson Vicki A, Dahlin Constance M, Blinderman Craig D, Jacobsen Juliet, Pirl William F, et al. Early palliative care for patients with metastatic non–small-cell lung cancer. New England Journal of Medicine. 2010;363(8):733–742. doi: 10.1056/NEJMoa1000678. [DOI] [PubMed] [Google Scholar]
- Wagstaff Adam, Van Doorslaer Eddy. Journal of Health Economics. Equity in the Finance of Health Care: Some International Comparisons. 1992;11(4):361–387. doi: 10.1016/0167-6296(92)90012-p. [DOI] [PubMed] [Google Scholar]
- World Bank. Out-of-Pocket Health Expenditure. Data retrieved from World Development Indicators. 2016 http://data.worldbank.org/indicator/SH.XPD.OOPC.ZS.
- Xu Ke, Evans David B, Kawabata Kei, Zeramdini Riadh, Klavus Jan, Murray Christopher JL. Household Catastrophic Health Expenditure: A Multicountry Analysis. The Lancet. 2003;362(9378):111–117. doi: 10.1016/S0140-6736(03)13861-5. [DOI] [PubMed] [Google Scholar]