Abstract
Despite being a relatively young nation, Singapore has established itself as a leading multifaceted medical hub, both regionally and globally. Although Singapore continues to pursue excellence in oncology care, cancer supportive care and survivorship care remain in the infancy stage. In an effort to advance this important aspect of oncology care in Singapore, the first cancer supportive and survivorship care forum was held in December 2016, involving 74 oncology practitioners. The primary goals of this forum were to raise awareness of the importance of cancer supportive and survivorship care and to provide a platform for oncology practitioners of diverse backgrounds to converge and address the challenges associated with the delivery of cancer supportive and survivorship care in Singapore. Key challenges identified during this forum included, but were not limited to, care fragmentation in an oncologist-centric model of care, poor integration of allied health and rehabilitation services, passive engagement of community partners, lack of specialized skill sets and knowledge in supportive and survivorship care, and patient-related barriers such as poor health literacy. The survivorship care model commonly used in Singapore places an imbalanced emphasis on surveillance for cancer recurrence and second primary cancers, with little attention given to the supportive and survivorship needs of the survivors. In summary, these challenges set the stage for the development and use of a more survivor-centric model, one that focuses not only on cancer surveillance, but also on the broad and unique physical and psychosocial needs of survivors of cancer in Singapore.
INTRODUCTION
Cancer is the leading cause of morbidity and mortality in Singapore. The number of new cancer diagnoses (for all cancer types) has increased from 45,799 in 2003 to 2007 to 61,522 in 2010 to 2014.1 The three most common cancer types in men are colorectal, lung, and prostate cancers, whereas the most common cancer types in women are breast, colorectal, and lung cancers.2 As a result of advancements in cancer therapeutics and early detection, the overall survival rates for all cancer types have improved significantly. The 5-year age-standardized observed survival rates for breast and colorectal cancers have increased from 67.5% and 45.9% during the period of 2005 to 2009 to 70.5% and 50.7% during the period of 2010 to 2014, respectively.1 However, survivors of cancer experience a myriad of health issues related directly to the cancer itself, pre-existing comorbidities, and anticancer therapies, all of which can potentially compromise their health-related quality of life and culminate in functional impairment at significant economic, emotional, and social costs.3-6
In view of the unique and unmet needs of survivors of cancer, the Institute of Medicine has emphasized how survivorship programs are essential to address the supportive and survivorship care needs of survivors of cancer.7 Although supportive care centers on the management of health problems related to cancer and its treatment, survivorship care focuses on helping survivors of cancer re-establish holistic normalcy after completion of cancer treatment. Survivorship care also encompasses management of the financial, psychological, and social impacts of cancer diagnoses and treatments on survivors of cancer and their family members and caregivers.6,8 Today, cancer supportive and survivorship care is recognized as one of the pillars of oncology care, and this is evident by the growing research efforts in this area, as well as the number of cancer institutes that have incorporated supportive and survivorship care programs and services.
In Singapore, cancer care is provided by both public tertiary institutes and private cancer centers. Within the public health system, health care is kept affordable through a financing system that relies heavily on individual responsibility and government subsidies, achieved through compulsory individual medical savings and insurance schemes. At present, the majority of cancer care is provided through publicly funded national cancer centers, and some of these centers have developed cancer survivorship care programs, although they are mostly small in scale and may only address specific health issues in niche populations. Examples would include speech therapy–led rehabilitation programs to address treatment-related speech and swallowing issues faced by patients with head and neck cancers and small-scale nurse-led patient navigation programs for patients with cancer with significant comorbidities and social challenges. Although commendable, these programs do not address the greater unmet survivorship care needs of all survivors of cancer. This is compounded by the fragmented and ad hoc nature of survivorship care as a result of the lack of awareness and integration of survivorship care into routine oncologic care and the shortage of health care professionals with supportive and survivorship care expertise. Change is desperately needed at both national and institutional levels to meet the survivorship care needs of the increasing numbers of survivors of cancer in Singapore.
SINGAPORE’S FIRST CANCER SUPPORTIVE AND SURVIVORSHIP CARE FORUM
On December 3, 2016, the first cancer supportive and survivorship care forum was held in Singapore; the forum involved 74 oncology practitioners, including oncologists, nurses, pharmacists, and other allied health care professionals. The primary goals of this forum were to raise awareness of the importance of cancer supportive and survivorship care and to provide a platform for oncology practitioners of diverse backgrounds to converge and address the challenges associated with the delivery of cancer supportive and survivorship care in Singapore. This article provides a summary of the forum and an outlook of Singapore’s future cancer supportive and survivorship care landscape.
CURRENT CHALLENGES IN SINGAPORE'S SUPPORTIVE AND SURVIVORSHIP CARE LANDSCAPE
Health Care System
In Singapore, the majority of survivors of cancer consult their oncologists, who may be based at various cancer centers, for their supportive and survivorship care needs, with cancer surveillance being the primary focus of survivorship care. With the increasing cancer incidence and survival rates, the existing infrastructure in Singapore cannot meet the increasing demand for cancer supportive and survivorship care services in a sustainable manner. The current oncologist-centric survivorship landscape is in stark contrast with survivorship care models in the developed countries of North America and Europe, where primary care providers are actively involved in a shared-care model of survivorship care delivery.9 Such a shared-care model is shown to improve survivors’ quality of life and care satisfaction, reduce costs, increase continuity of care, and reduce the burden on oncologists and tertiary health care institutes.10-14 Historically, cancer has always been a disease managed in tertiary health care settings in Singapore, and currently, there is a lack of training or robust professional development courses to allow primary health care providers to develop skill sets in cancer survivorship. Without the involvement of primary health care providers in cancer survivorship care, community care coordination for survivors of cancer, especially those with complex comorbidities, is lacking. In recent years, there have been increasing efforts to transition care from tertiary institutes to the community by empowering and engaging community-based family physicians; however, it must be emphasized that Singapore’s initiative for one family physician for every Singaporean is still in the infancy stage.15,16
Oncology Practitioners and Specialty Care Providers
Oncology practitioners often indicate that they are not equipped with the appropriate skills and knowledge to identify and manage some of the lesser known supportive and survivorship care issues.17 This problem is compounded by the lack of evidence-based management strategies for certain chronic and late adverse effects such as cognitive impairment and peripheral neuropathy. Although numerous guidelines have been published by the National Comprehensive Cancer Network, the Multinational Association of Supportive Care in Cancer, and ASCO to address management of survivorship issues, many recommendations in these guidelines are based on expert opinions and include therapies that are not readily available in Singapore.18-21
The provision of excellent supportive and survivorship care to patients with cancer and survivors requires a multidisciplinary approach that encompasses other health care disciplines, such as rehabilitation, nursing, and allied health. However, the involvement of these specialty care providers is largely ad hoc in nature and not integrated into routine oncologic care, resulting in fragmentation and suboptimal provision of supportive and survivorship care to survivors of cancer in Singapore, especially those with complex survivorship issues impacting quality of life.
Survivors
The multiracial and multicultural population in Singapore poses unique patient-specific challenges that must be addressed to allow for the delivery of successful cancer supportive and survivorship care. First, as a result of cultural and religious sensitivities, survivors have expressed discomfort and unwillingness to discuss sensitive survivorship health issues such as sexuality and fertility with their oncology practitioners, which hampers the provision of support and services for such issues. Second, despite a reasonably high level of general health literacy among Singaporeans, the adequacy of cancer-related health literacy is unknown, with oncology providers generally questioning the ability of survivors of cancer to be self-aware and self-manage their cancer survivorship issues.17 Third, survivors of cancer may turn to unorthodox alternative treatments to manage their health problems, particularly when the use of complementary and alternative medicines and traditional Chinese medicines is highly prevalent in Singapore.22 Although anecdotal benefits are occasionally reported, many of these therapies are not proven to be effective and may actually be harmful to survivors. Fourth, despite the benefits and importance of community care coordination through primary care providers, survivors are reluctant to involve them in their supportive and survivorship care journey, preferring to receive ongoing care at tertiary centers. Finally, the financial burden from treatment and consultation fees may deter patients from attending follow-up appointments or complying with recommended treatments.23
PROPOSED SURVIVORSHIP CARE MODEL IN SINGAPORE
The commonly used survivorship care model in Singapore places an imbalanced emphasis on surveillance for cancer recurrence and second primary cancers, with little attention given to the rehabilitative needs of survivors of cancer after diagnosis and treatment. The challenges laid out earlier set the stage for a shift toward a more survivor-centric model, one that focuses not only on cancer surveillance, but also on the broad and unique physical and psychosocial needs of survivors of cancer in Singapore.
Participants in the forum identified several principles as vital for the optimization of survivorship care in Singapore. The principles are briefly classified as follows: Survivorship care should be survivor centered, consist of integrated and coordinated care, promote wellness, be accessible and equitable, and be research driven and evidence based.
Survivor-centered care: The model needs to be relevant and individualized to the needs of survivors of cancer at all stages of their survivorship journeys. In addition, survivors of cancer should be engaged and empowered to be active partners in their individual survivorship journeys.
Integrated and coordinated care: Cancer supportive and survivorship care should be integrated into routine oncologic care. Patients and survivors should have access to cancer supportive and survivorship care services across both tertiary and community health care settings. The health care team should assume responsibility for planning, providing, and coordinating various clinical services across the continuum of survivorship care. This will facilitate efficient and effective communication between all tertiary and community health care professionals involved. Integrated and coordinated care would allow survivors of cancer to receive the right type of care at the right time and in the right environment.
Promotion of wellness: With mounting evidence demonstrating the health benefits of lifestyle interventions, cancer survivorship care must include measures to holistically improve the state of health of patients with cancer and survivors. Such examples include education and provision of community-based programs to encourage healthy lifestyle behaviors and self-monitoring and preventative care to maintain an optimal state of health.
Research-driven and evidence-based practices: To advance cancer supportive and survivorship care, a robust research infrastructure should be incorporated seamlessly into the survivorship model. This infrastructure should promote and facilitate research initiatives that address pertinent clinical problems, with an aim to develop evidence-based management strategies for cancer supportive and survivorship care.
Accessible and equitable care: Any survivor of cancer should be able to access supportive and survivorship care services at any point during his or her cancer journey. Increasing health care costs have resulted in an increased financial burden to survivors and their families. Thus, supportive and survivorship care should be subsidized through strategic partnerships with governmental, commercial, and philanthropic organizations.
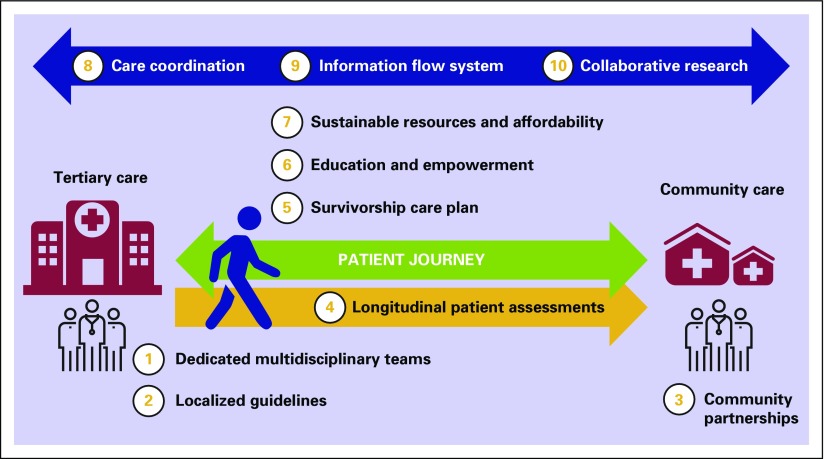
On the basis of the aforementioned recommendations, the proposed survivorship care model in Singapore should encompass the following elements (Fig 1).
Fig 1.
Proposed survivorship care model and required elements.
Dedicated and integrated multidisciplinary survivorship care teams: The survivorship team is multidisciplinary in nature, purposefully developed, and integrated into routine oncologic care. It involves both medical and paramedical staff with expertise to not only manage the myriad of health and psychosocial issues faced by survivors of cancer, but also develop educational and research initiatives and drive institutional and governmental changes to advance the field of cancer supportive and survivorship care in Singapore. Examples of disciplines involved in such a team include, but are not limited to, oncology, rehabilitative medicine, nursing, physical therapy, pharmacy, dietetics, and psychosocial oncology. These teams should also be present across both tertiary and community care settings to deliver survivorship care throughout the survivorship continuum.
Localized cancer survivorship guidelines: Although international cancer survivorship guidelines have been developed by major organizations, these have to be localized to the health care and sociocultural needs and subtleties of an Asian nation such as Singapore. Guidelines can be translated to care pathways that can equip health care providers to provide evidence-based and cost-effective cancer survivorship care. An example is the standardization of care pathways for common treatment-related toxicities, such as fatigue, cognitive impairment, peripheral neuropathy, endocrine therapy–specific toxicities (eg, hot flashes), and musculoskeletal symptoms.
Community partnerships: The community environment is beneficial for survivors for several reasons. First, it is beneficial for survivors to recuperate and receive care in familiar environments, which in turn may promote psychological recovery as they transition from institution-based acute care. Second, community-based survivorship care provides an excellent conduit for health and wellness promotion. Finally, the transition of survivors to community-based care will substantially reduce the workload of oncology health care providers in tertiary institutions, allowing for more efficient and effective use of health care resources. Community health care providers, such as general practitioners or family medicine physicians, nurses, pharmacists, and physical therapists, should collaborate with tertiary oncology health care providers and community partner organizations to optimize supportive and survivorship care. An example of a community partner organization is the Singapore Cancer Society, which not only provides means-based financial support to patients with cancer, but also has recently taken major steps toward expanding cancer survivorship care through the establishment of a community cancer rehabilitation center to address the needs of survivors of cancer and their caregivers.
Robust adaptive patient assessment program: This would entail detailed initial assessments, including health literacy, treatments (planned or completed), existing unmet or possible future supportive care or survivorship needs, and psychosocial backgrounds, to guide survivorship care planning. This would be followed by longitudinal assessments throughout the survivor’s journey, allowing for the detection of new or ongoing health issues to be addressed. In addition, such assessments would also allow the provision of interventions and resources to survivors of cancer that are stratified to the complexity and severity of their health issues.
Mandatory survivorship care plan: Every survivor of cancer must be given a survivorship care plan at the completion of their acute cancer care, and this plan should be compatible with the individual’s health literacy and accessible to all health care professionals and caregivers. The survivorship care plan empowers survivors and their caregivers to take charge of their survivorship care needs and facilitates the transfer of crucial information to other health care providers involved in their survivorship journey. This care plan should include information such as treatment history, planned future treatments and follow-ups, any current or future supportive and survivorship care needs, respective management plans, recommended lifestyle changes, and other information related to the care of the survivor.
Education and empowerment of survivors of cancer: Survivors of cancer must be regarded as active partners in survivorship care and be provided access to survivorship care resources adapted to their spoken language and health literacy levels.
Sustainable resources and affordability: Because of the increasing health care costs and constantly evolving health care resource allocations, survivorship care in Singapore needs to be financially sustainable for survivors, health care institutions, and providers. Survivorship care teams can assist survivors in navigating and optimizing their access to the complex array of governmental and volunteer welfare organization financial subsidies and benefits. In addition, collaboration between health care institutions and providers, governmental bodies, and volunteer welfare organizations is required to ensure adequate resources (such as manpower allocation and governmental subventions) are allocated to cancer survivorship care in a sustainable manner.
Care coordination through patient navigators: Successful survivorship care cannot be achieved without a dedicated care coordination service for survivors. It is well known that cancer care is becoming increasingly complex and multidisciplinary in nature, and when combined with a complex health care and funding system, as exists in Singapore, cancer care can be confusing, resulting in suboptimal care among survivors. Patient navigators could guide patients and survivors through their treatment and survivorship journeys by coordinating various aspects of care such as appointments, optimizing resources available to the patients and survivors, and providing oncology-specific care advice. Such a service also ensures that care needs are met and no survivor is lost in transition. The need for care coordination is equally important in tertiary and community care settings because care needs do not decrease, but will change over time as survivors move through the survivorship continuum.
Information flow system: For coordinated care to be achieved, a continuous and efficient information flow system between community providers and specialists is needed. The information flow system could be in the form of a portal that allows remote access to patients’ health care data, communication among various health care providers across the health care system, and scheduling of patient appointments.
Research: A survivorship care model should be combined with a robust research infrastructure to provide cutting-edge therapies in supportive and survivorship care. With a research infrastructure in place, clinical trials and research can be conducted to advance understanding and develop new interventions and programs. In addition, robust and high-quality data should be collected seamlessly to evaluate the effectiveness of current and new interventions and programs. A key area of focus would be on the development of interventions to manage poorly understood supportive and survivorship issues, such as chemotherapy-associated neuropathy, cancer-related fatigue, and cognitive impairment.
CONCLUSION AND FUTURE DIRECTIONS
Cancer survivorship care is still in its infancy in Singapore. With an aging population, increasing cancer survival rates, and increasingly unmet cancer supportive and survivorship care needs, the need for effective cancer supportive and survivorship care services has never been more urgent. These services cannot exist in isolation, but should be framed within a model of care that complements both the unique needs of Singapore’s survivors of cancer as well as Singapore’s health care infrastructure. Singapore’s ongoing shift toward developing a community-based health care system is a necessary step in the provision of future community-based cancer survivorship services. Core working groups across tertiary and community health care providers and institutions, as well as collaboration with governmental and volunteer welfare organizations, are necessary to advance the field of supportive and survivorship care for the benefit of survivors of cancer and their families. These working groups and collaborations can in turn lead to the development of evidence-based cancer supportive and survivorship care best practices for Singapore, improved access to clinical services, and the formation of collaborative research networks to advance cancer supportive and survivorship care locally, regionally, and internationally.
Through this forum, we have taken initial steps to raise awareness, discuss challenges, and unite various stakeholders in cancer supportive and survivorship care in Singapore. In response, we have developed a supportive and survivorship care model and a set of guiding principles that will serve as the blueprint for Singapore’s future cancer supportive and survivorship care paradigm. This is the start of a nationwide movement to ultimately provide holistic and integrated care for survivors of cancer and to transform Singapore into a regional and international center of excellence in cancer supportive and survivorship care.
ACKNOWLEDGMENT
We thank the participants for their contribution to this study.
AUTHOR CONTRIBUTIONS
Conception and design: Kiley Wei-Jen Loh, Terence Ng, Hay Mar Saw, Rathi Mahendran, Celia Tan, Yew Jin Ong, Alethea Chung Pheng Yee, Alexandre Chan, Khee Chee Soo
Administrative support: Hay Mar Saw
Provision of study material or patients: Su Pin Choo, Gail Chia Yang Chang
Collection and assembly of data: Kiley Wei-Jen Loh, Gail Chia Yang Chang, Alexandre Chan, Khee Chee Soo
Data analysis and interpretation: Kiley Wei-Jen Loh, Su Pin Choo, Celia Tan, Khee Chee Soo
Manuscript writing: All authors
Final approval of manuscript: All authors
Accountable for all aspects of the work: All authors
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
The following represents disclosure information provided by authors of this manuscript. All relationships are considered compensated. Relationships are self-held unless noted. I = Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For more information about ASCO's conflict of interest policy, please refer to www.asco.org/rwc or ascopubs.org/jco/site/ifc.
Kiley Wei-Jen Loh
Consulting or Advisory Role: AstraZeneca, Novartis
Terence Ng
Employment: Roche Pharma AG
Su Pin Choo
Honoraria: Bayer, Bristol-Myers Squibb
Consulting or Advisory Role: Celgene, Novartis, Eisai, Bristol-Myers Squibb, Shire, Sirtex Medical
Research Funding: Bristol-Myers Squibb
Travel, Accommodations, Expenses: Amgen, Bristol-Myers Squibb, Merck, Bayer
Hay Mar Saw
No relationship to disclose
Rathi Mahendran
No relationship to disclose
Celia Tan
No relationship to disclose
Gail Chia Yang Chang
No relationship to disclose
Yew Jin Ong
No relationship to disclose
Alethea Chung Pheng Yee
No relationship to disclose
Alexandre Chan
Honoraria: GlaxoSmithKline, Merck Sharp & Dohme, Mundipharma
Consulting or Advisory Role: GlaxoSmithKline, Merck Sharp & Dohme, Mundipharma
Speakers' Bureau: GlaxoSmithKline, Merck Sharp & Dohme
Khee Chee Soo
No relationship to disclose
REFERENCES
- 1. Singapore Cancer Registry: Interim Annual Registry Report: Trends in Cancer Incidence in Singapore, 2010-2014. https://www.nrdo.gov.sg/docs/librariesprovider3/default-document-library/cancer-trends-2010-2014_interim-annual-report_final-(public).pdf?sfvrsn=0.
- 2. Singapore Cancer Registry: Annual Registry Report. https://www.nrdo.gov.sg/docs/librariesprovider3/Publications-Cancer/cancer-registry-annual-report-2015_web.pdf?sfvrsn=10.
- 3.Miller KD, Siegel RL, Lin CC, et al. Cancer treatment and survivorship statistics, 2016. CA Cancer J Clin. 2016;66:271–289. doi: 10.3322/caac.21349. [DOI] [PubMed] [Google Scholar]
- 4.Rowland JH, Bellizzi KM. Cancer survivorship issues: Life after treatment and implications for an aging population. J Clin Oncol. 2014;32:2662–2668. doi: 10.1200/JCO.2014.55.8361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Weaver KE, Forsythe LP, Reeve BB, et al. Mental and physical health-related quality of life among U.S. cancer survivors: Population estimates from the 2010 National Health Interview Survey. Cancer Epidemiol Biomarkers Prev. 2012;21:2108–2117. doi: 10.1158/1055-9965.EPI-12-0740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schumacher KL, Stewart BJ, Archbold PG, et al. Effects of caregiving demand, mutuality, and preparedness on family caregiver outcomes during cancer treatment. Oncol Nurs Forum. 2008;35:49–56. doi: 10.1188/08.ONF.49-56. [DOI] [PubMed] [Google Scholar]
- 7.Hewitt M, Greenfield S, Stovall E. From Cancer Patient to Cancer Survivor: Lost in Transition. Washington, DC: The National Academies Press; 2005. [Google Scholar]
- 8.Hudson PL, Aranda S, Kristjanson LJ. Meeting the supportive needs of family caregivers in palliative care: Challenges for health professionals. J Palliat Med. 2004;7:19–25. doi: 10.1089/109662104322737214. [DOI] [PubMed] [Google Scholar]
- 9.McCabe MS, Bhatia S, Oeffinger KC, et al. American Society of Clinical Oncology statement: Achieving high-quality cancer survivorship care. J Clin Oncol. 2013;31:631–640. doi: 10.1200/JCO.2012.46.6854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Brennan M, Butow P, Spillane AJ, et al. Follow up after breast cancer: Views of Australian women. Aust Fam Physician. 2011;40:311–316. [PubMed] [Google Scholar]
- 11.Hall SJ, Samuel LM, Murchie P. Toward shared care for people with cancer: Developing the model with patients and GPs. Fam Pract. 2011;28:554–564. doi: 10.1093/fampra/cmr012. [DOI] [PubMed] [Google Scholar]
- 12.Grunfeld E, Levine MN, Julian JA, et al. Randomized trial of long-term follow-up for early-stage breast cancer: A comparison of family physician versus specialist care. J Clin Oncol. 2006;24:848–855. doi: 10.1200/JCO.2005.03.2235. [DOI] [PubMed] [Google Scholar]
- 13.Grunfeld E, Gray A, Mant D, et al. Follow-up of breast cancer in primary care vs specialist care: Results of an economic evaluation. Br J Cancer. 1999;79:1227–1233. doi: 10.1038/sj.bjc.6690197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Grunfeld E, Fitzpatrick R, Mant D, et al. Comparison of breast cancer patient satisfaction with follow-up in primary care versus specialist care: Results from a randomized controlled trial. Br J Gen Pract. 1999;49:705–710. [PMC free article] [PubMed] [Google Scholar]
- 15.Ministry of Health Singapore https://www.moh.gov.sg/content/moh_web/home/pressRoom/speeches_d/2016/speech-by-minister-fo-health–mr-gan-kim-yong–at-the-moh-commit.html Speech by Minister for Health, Mr Gan Kim Yong, at the MOH Committee of Supply Debate 2016.
- 16.Ministry of Health Singapore https://www.moh.gov.sg/content/moh_web/home/pressRoom/highlights/2016/2020-healthcare-manpower-plan.html 2020 Healthcare Manpower Plan.
- 17.Ng T, Toh MR, Cheung YT, et al. Follow-up care practices and barriers to breast cancer survivorship: Perspectives from Asian oncology practitioners. Support Care Cancer. 2015;23:3193–3200. doi: 10.1007/s00520-015-2700-2. [DOI] [PubMed] [Google Scholar]
- 18.National Comprehensive Cancer Network Survivorship. Version 2. https://www.nccn.org/store/login/login.aspx?ReturnURL=https://www.nccn.org/professionals/physician_gls/pdf/survivorship.pdf.
- 19.Resnick MJ, Lacchetti C, Bergman J, et al. Prostate cancer survivorship care guideline: American Society of Clinical Oncology Clinical Practice Guideline endorsement. J Clin Oncol. 2015;33:1078–1085. doi: 10.1200/JCO.2014.60.2557. [DOI] [PubMed] [Google Scholar]
- 20.Nekhlyudov L, Lacchetti C, Davis NB, et al. Head and neck cancer survivorship care guideline: American Society of Clinical Oncology Clinical Practice Guideline endorsement of the American Cancer Society Guideline. J Clin Oncol. 2017;35:1606–1621. doi: 10.1200/JCO.2016.71.8478. [DOI] [PubMed] [Google Scholar]
- 21.Runowicz CD, Leach CR, Henry NL, et al. American Cancer Society/American Society of Clinical Oncology breast cancer survivorship care guideline. J Clin Oncol. 2016;34:611–635. doi: 10.1200/JCO.2015.64.3809. [DOI] [PubMed] [Google Scholar]
- 22.Shih V, Chiang JY, Chan A. Complementary and alternative medicine (CAM) usage in Singaporean adult cancer patients. Ann Oncol. 2009;20:752–757. doi: 10.1093/annonc/mdn659. [DOI] [PubMed] [Google Scholar]
- 23.Chan A, Chiang YY, Low XH, et al. Affordability of cancer treatment for aging cancer patients in Singapore: An analysis of health, lifestyle, and financial burden. Support Care Cancer. 2013;21:3509–3517. doi: 10.1007/s00520-013-1930-4. [DOI] [PubMed] [Google Scholar]