Abstract
Study Objectives:
Sleep is critical to a child's health and well-being, but children are likely to sleep less and be awakened more often during the night in the hospital than at home. To date no studies have compared caregiver, nurse, and physician perspectives of nighttime sleep disruptions in the pediatric general medicine setting. Our aim was to assess caregiver, nurse, and physician perspectives on the most frequent in-hospital disruptors of sleep for pediatric patients. Additionally, we evaluated the degree of agreement of those opinions between the caregivers and medical team.
Methods:
Caregivers, nurses, and physicians were surveyed using the Potential Hospital Sleep Disruption and Noises Questionnaire (PHSDNQ) regarding their opinions on factors that disrupt sleep. Caregiver responses were collected via a convenience sample of patients hospitalized from February to August 2017 and hospital staff was surveyed once regarding overall perception. The perceived percentage of patients disrupted by each factor was calculated and compared among groups using chi-square tests. Using caregiver rank order based on mean response as the reference gold standard, the absolute differences of nurse and physician rank orders were summed and analyzed using a two-sample test of proportion. In addition, staff was asked knowledge and empowerment questions about how to maximize patient sleep in the hospital and responses were compared using chi-square tests.
Results:
A total of 162 caregivers, 77 nurses (84% response rate), and 81 physicians (90% response rate) completed surveys. Checking vital signs (50%), nurse/physician interruption (49%), and continuous pulse oximetry (38%) were the three most prevalent disruptors of pediatric inpatient sleep as reported by caregivers. Significant differences were observed between caregiver, nurse, and physician responses for pain, anxiety, alarms, noise, and tests (P ≤ .001 for all). Both nurse and physician rank orders were discordant when compared to caregivers; there was no significant difference between the two staff groups. When compared to physicians, nurses reported doing more to help children sleep in the hospital (33% versus 94%, P < .001).
Conclusions:
Although caregivers report medical interventions such as checking vital signs, nurse/physician interruption, and continuous pulse oximetry as the most frequent disruptors of inpatient pediatric sleep, pediatric staff has poor insight into these disruptions.
Citation:
Peirce LB, Orlov NM, Erondu AI, Anderson SL, Chamberlain M, Gozal D, Arora VM. Caregiver and staff perceptions of disruptions to pediatric inpatient sleep. J Clin Sleep Med. 2018;14(11):1895–1902.
Keywords: health care quality, pediatric hospital medicine, pediatrics, sleep and arousal, sleep deprivation
BRIEF SUMMARY
Current Knowledge/Study Rationale: Although children experience disrupted sleep in the hospital, there is a paucity of studies examining the causes of sleep disruption in hospitalized children from the perspectives of both caregivers and hospital staff. This study extends previous findings on caregiver-reported in-hospital sleep disruptions by also examining the perspectives of nurses and physicians, important stakeholders in improving pediatric sleep in the hospital.
Study Impact: The findings from this study suggest that medical interventions are the most prevalent disruptors as reported by caregivers, revealing a possible target for future pediatric sleep improvement efforts. However, the perspectives of nurses and physicians varied drastically from those of caregivers, highlighting the need for education of staff regarding top disruptors to pediatric sleep in the hospital.
INTRODUCTION
Inadequate sleep is a problem experienced by approximately 15 million American children.1 According to the American Academy of Sleep Medicine's consensus statement on the recommended amount of sleep for pediatric populations, adequate sleep duration has been linked to improved physical and mental health, learning, memory, and emotional regulation in children.2 These recommendations also state that inadequate sleep duration can increase the risk of hypertension, diabetes, obesity, depression, and injuries in children and adolescents.2 Due to their effect on healing and daily functioning, these factors are of particular importance to hospitalized children and their families. Sleep disruption can also adversely affect hospitalization and posthospital outcomes; prior work in an adult population has demonstrated that sleep loss in the hospital is associated with higher morning blood pressure,3 increased risk of hyperglycemia,4 and increased recovery time.5 Although the literature contains several systematic reviews of sleep disruption in pediatric cancer patients6 and children in a pediatric intensive care unit,7 there is a paucity of data on the effect of sleep disruption on health outcomes in pediatric patients. In addition, a poor sleep environment can also negatively influence the patient and family experience in the hospital.8 For example, quietness of the hospital room is one of the parent-reported Hospital Consumer Assessment of Healthcare Providers and Systems measures for pediatric patients.9
Although sleep is essential for health, hospitalization can be extremely disruptive to sleep.10 Prior studies have found that children admitted to a general pediatric ward sleep significantly less and awaken more during the night compared to at home.11–14 Through surveys given to patient families, these studies identified a variety of factors contributing to in-hospital sleep disruption including noise from alarms, staff interruptions, and pain.11–14 In contrast, other studies have focused on the views of pediatric in-hospital sleep from the perspective of physicians and nurses.15,16 Promoting sleep in the hospital has historically been a priority of the nursing profession. In Florence Nightingale's Notes on Nursing, she asserted that preventing patients from being awakened is a core principle of good nursing.17 This idea is mirrored in the American Academy of Nursing's “Choosing Wisely” campaign, which instructs nurses not to wake patients for routine care unless required by their condition.18
The perspectives of all stakeholders, both patient families and providers, must be compared in order to ensure the maximal effectiveness of quality improvement interventions aimed at improving in-hospital pediatric sleep. Furthermore, comparison between these groups is essential for determining areas for improvement in provider knowledge regarding the patient and family experience of sleep in the hospital. The few studies focusing on the comparison between patient and staff perceptions of in-hospital sleep disruptions have either examined an adult population19 or a pediatric population in an intensive care setting.15 To date no study has compared patient, nurse, and physician perspectives of nighttime sleep disruptions in the pediatric general medicine setting.
The aims of this project were twofold. First, we aimed to determine the most frequent in-hospital sleep disruptors in patients admitted to a general pediatrics ward as perceived by caregivers (a parent or guardian). Based on prior work in the adult population,19 we hypothesized that at least 30% of care-givers would report staff interruptions as a disruptor of children's sleep in the hospital. Second, we aimed to evaluate the degree of agreement between pediatric patients, nurses, and physicians' perspective of the main factors influencing in-hospital sleep disruption in the general pediatric setting. Due to the emphasis on sleep within the nursing profession, we hypothesized that compared to physicians, nurses would be more likely to agree with caregivers regarding top disruptors.
METHODS
Study Design
A single-institution, survey-based study on pediatric patients and hospital staff was conducted at the University of Chicago Medicine to compare perceptions of in-hospital sleep disruptions among caregivers, nurses, and physicians. We took a convenience sample of patients age 30 days to 18 years admitted to the general pediatric unit at Comer Children's Hospital (floor 5). Patients admitted to the general pediatrics, gastroenterology, rheumatology, or neurology services whose parent or guardian spoke English and spent the previous night in the hospital room were surveyed. The caregiver was not approached if the patient had a gastrostomy tube, was dependent on tracheostomy, was monitored by continuous electroencephalogram, or had a diagnosis of cerebral palsy. In addition, we surveyed physicians and nurses employed by University of Chicago Medicine who work on the general pediatric units of Comer Children's Hospital. All staff surveyed work on the ward from which caregivers were surveyed. Most physicians surveyed were house staff. All staff involved with the design and administration of the surveys were asked not to complete a survey in order to avoid this source of bias. No protected health information was collected from any of the participants. The University of Chicago Institutional Review Board approved the study (protocol #12-1766).
Data Collection
Caregiver Report of Sleep Disruptions
In order to determine which factors are the most disruptive to pediatric patient sleep, a caregiver (parent or guardian) of children admitted to the general ward was approached every day (Monday-Friday) and asked to complete an age-specific Patient Sleep Assessment.20–22 The Patient Sleep Assessment is an intake assessment containing a bundle of tools, some of which are validated in pediatric populations and some that are not. The tools used in this study are the demographics section and the Potential Hospital Sleep Disruption and Noises Questionnaire (PHSDNQ). The Patient Sleep Assessment contains demographics questions such as sex, race, and level of education. Caregivers were also asked to complete a PHSDNQ, a survey asking the extent to which various factors disrupted their child's sleep the previous night (see Survey 1 in the supplemental material). These factors include medical interventions (checking vital signs, continuous pulse oximetry, medications, tests, nurse or physician interruption, and respiratory therapist), symptoms (pain and anxiety), and environmental factors (noise [all sources]), alarms on equipment, and room temperature).21,22 The PHSDNQ has been validated in adult patients,19 but has yet to be validated in pediatric patients. In order to modify the PHSDNQ for a pediatric population, we conducted focus groups with pediatric nurses and residents. As a result of this needs assessment, the PHSDNQ was modified in two ways. First, it was shortened in order to better reflect the common sleep disruptors in a pediatric setting and to reduce survey burden. Second, continuous pulse oximetry, respiratory therapist interruption, and nurse/physician interruption were added to the list of disruption factors questions as a result of specific comments from focus group participants regarding the high prevalence of these factors in the pediatric setting. Formal validation of the PHSDNQ in pediatric populations is ongoing. It is hospital policy for all patients admitted to floor 5 of Comer Children's Hospital to be monitored overnight with continuous pulse oximetry. All Patient Sleep Assessments were collected via convenience sampling and completed by a caregiver. All children younger than 18 years were required by the University of Chicago Institutional Review Board (protocol #12-1766) to have a parent present in the hospital room in order to participate in the survey. After permission was acquired from a parent, most adolescents either responded independently to the questions or in collaboration with a parent.
Staff Perceptions of Sleep Disruptions
To determine the health care providers' perspective on patient sleep disruption, a staff survey containing demographic information and a PHSDNQ was administered to physicians and nurses working on general pediatrics units (see Survey 2 in the supplemental material). The staff survey was modified from a survey used by Grossman et al. in a study examining staff perceptions of sleep in an adult population.19 In order to adapt this survey to a pediatric population, several questions were added regarding staff knowledge of pediatric sleep in the hospital and empowerment to help children sleep better in the hospital. The PHSDNQ on the staff survey asked about the same disruption factors as the patient PHSDNQ, but physicians and nurses were asked to rate how disruptive these factors are to patients in general. For example, the survey given to caregivers states, “Please rate the extent to which each of the following disrupted your child's sleep last night” and the factors are listed with Likert scale response options of 1 to 5. The survey given to staff states, “How disruptive do pediatric patients and their parents perceive the following factors to sleep in the hospital?” and the factors are listed with the same Likert scale response options of 1 to 5. Pediatric residents and hospitalists were asked to complete this survey at various meetings and over email. The survey was introduced to nurses at staff meetings and distribution continued daily. All paper survey data were entered and stored on the REDCap Database Version 6.14.0 (Vanderbilt University, 2017).
Data Analysis
Due to uncertainty regarding responsiveness of caregivers, we aimed to collect as many caregiver surveys as possible via a convenience sample from February to August 2017, with a goal of 100 caregivers for a stable estimate. The intended sample size for physicians (90) was determined by the number of pediatric and combined medicine and pediatric residents and pediatric hospitalists working on floors 5 and 6 of Comer Children's Hospital at the time of surveying. Intended sample size for nurses (92) was determined by the number of nurses working on the same two floors at the time of sampling as reported by the nurse manager of both floors.
The caregiver PHSDNQ response distribution was analyzed and the median responses were used to determine a cut point for dichotomization. In contrast to the data from previous work,19 PHSDNQ responses for each disruption factor were not normally distributed. Therefore, it was determined that the mean would not be a meaningful cutoff point for dichotomization. All caregiver PHSDNQ responses had a median of 1 (not disruptive at all), whereas the median for checking vital signs was 2 (somewhat disruptive). Therefore, 2 or higher was considered as a report of disruption by caregivers to best represent the variance in these data. The percentage of patients disrupted by each factor was calculated using the dichotomized data. In addition, the distribution of nurse and physician PHSDNQ responses was analyzed and the median responses were used to define a cutoff point for dichotomization. The median of nurse and physician PHSDNQ responses for each disruption factor ranged from 2 (somewhat disruptive) to 5 (extremely disruptive), with most items having a median of 3 (moderately disruptive). Therefore 4 (quite a bit disruptive) and higher was considered a report of disruption for both physicians and nurses to best represent the distribution of these data. Using the dichotomized data, the percentage of nurses and physicians reporting each factor as disruptive was calculated. The percentages of caregivers, nurses, and physicians reporting each factor as disruptive were compared across groups using chi-square tests.
Due to difference in the median values for parent/guardian responses and staff responses, the PHSDNQ responses were also analyzed by creating a rank order for each group using mean response. Using parent/guardian responses as the reference gold standard, the absolute difference of the ranking for each disruption factor was calculated for physicians and nurses.23 The absolute differences for all factors were then summed for both physicians and nurses. These sums were compared with a two-sample test of proportions using the total possible difference in caregiver and staff rank order as the denominator. Finally, the knowledge and empowerment questions on the staff survey were analyzed using chi-square tests. All tests were conducted in stata24 with a value of P ≤ .001 considered as achieving statistical significance after Bonferroni correction.
RESULTS
Study Population: Patient Caregivers, Physicians, and Nurses
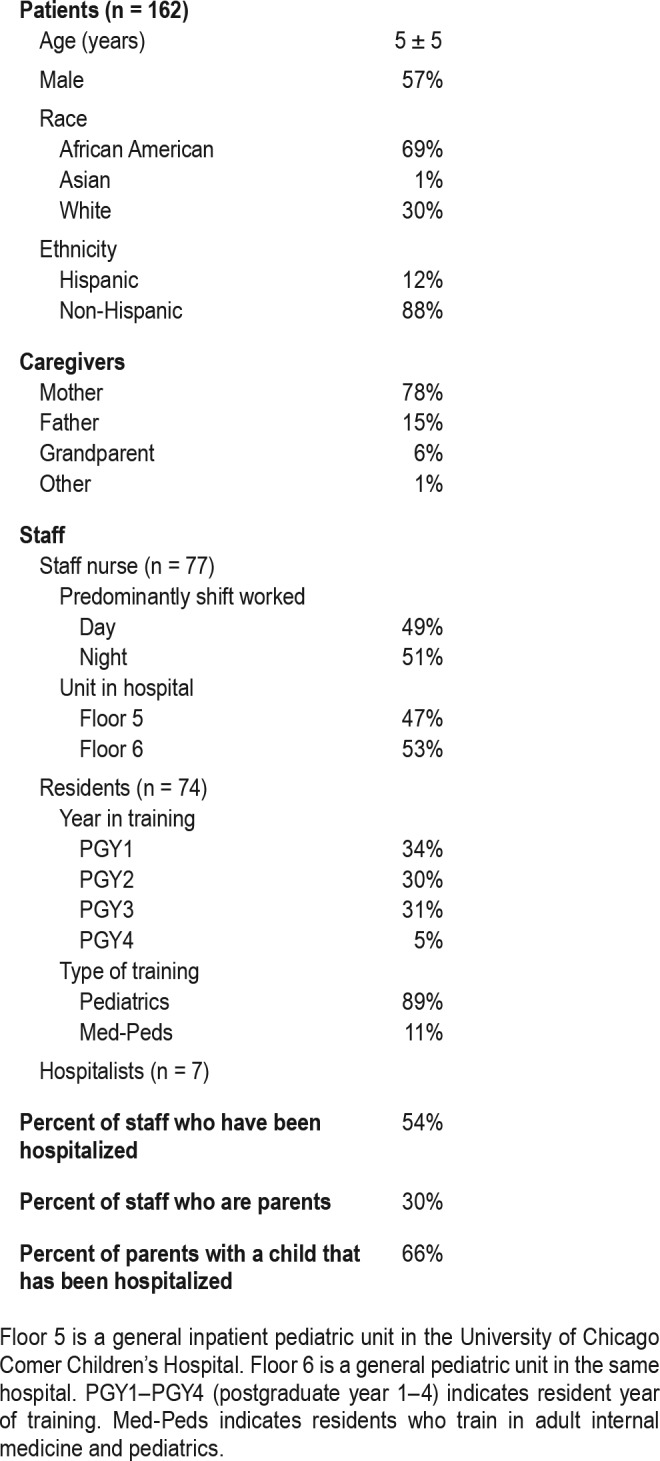
From February to August 2017, 162 caregivers completed the Patient Sleep Assessment, which included demographics and a PHSDNQ. Demographics from the Patient Sleep Assessment demonstrated that the mean age of patients was 5 ± 5 years old. The patient population was diverse in race and ethnicity, with 69% being African American and 12% being Hispanic. In addition, 81 physicians and 77 staff nurses who work on the ward from which caregivers were surveyed completed the staff survey, which included demographics and a PHSDNQ. Of the staff nurses who completed the PHSDNQ (84% response rate), there was a nearly equal split between nurses who work during the day versus the night and nurses who work on each of the two general pediatrics units studied. The physician population (90% response rate) included 7 hospitalists and 74 residents (Table 1).
Table 1.
Study population characteristics patients and caregivers.
Caregiver Report of Sleep Disruptions
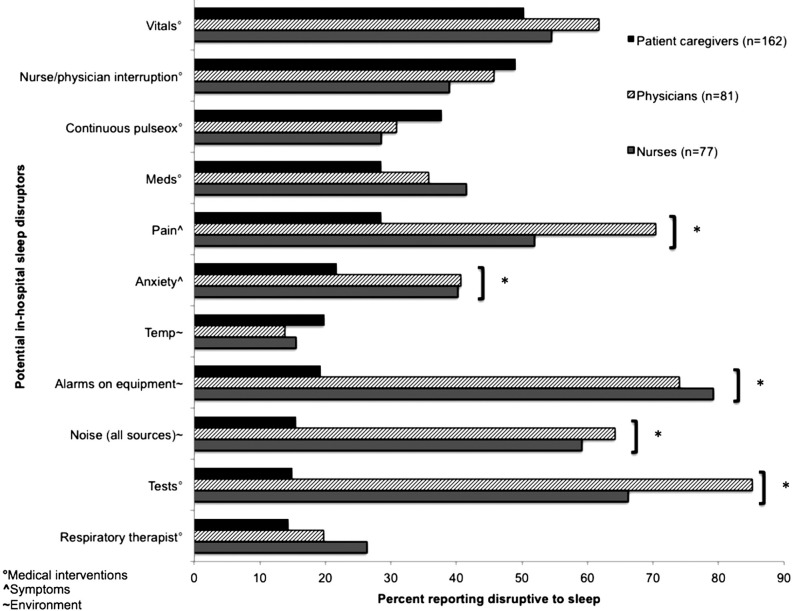
According to dichotomized caregiver responses from the PHSDNQ portion of the Patient Sleep Assessment, the five most frequent factors disrupting pediatric patient sleep in the hospital were checking vital signs (50%), nurse/physician interruption (49%), continuous pulse oximetry (38%), medications (29%), and pain (29%). The four most prevalent factors can all be classified as medical interventions. Environmental factors such as alarms on monitoring equipment (19%) and noise from all sources (16%) were less commonly reported by caregivers (Figure 1). Examining disruptions by age group did not yield any significant differences.
Figure 1. Caregiver, physician, and nurse frequency of reporting of potential disruptors to inpatient pediatric sleep, n = 320.
Dichotomized survey data of physicians and nurses were compared to patient responses using chi-square tests. This figure suggests that the top disruptors of pediatric sleep in the hospital as reported by patient caregivers are checking vital signs, nurse/physician interruption, and continuous pulse oximetry and illustrates the diversity within caregiver, physician, and nurse perspectives of sleep in the hospital. Symbols indicate: ° = factors categorized as medical interventions, ∧ = factors categorized as symptoms, ∼ = environment factors, and * = P ≤ .001. All P values were calculated using chi-square tests.
Caregiver, Physician, and Nurse Perceptions of Sleep Disruption
Comparing the percentages of caregivers, physicians, and nurses who reported each factor as disruptive demonstrated similarity in frequency of reporting among all three groups for the top three caregiver-reported sleep disruptors (checking vital signs, nurse/physician interruption, and continuous pulse oximetry). In addition, similarity in frequency of reporting was observed among physicians and nurses for most disruption factors. However, statistically significant differences in frequency of reporting emerged between the three groups for the following factors: pain (29% caregivers versus 70% physicians versus 52% nurses, P < .001), anxiety (22% versus 41% versus 40%, P = .001), alarms on monitoring equipment (19% versus 74% versus 79%, P < .001), noise all sources (16% versus 64% versus 59%, P < .001), and tests such as drawing blood (15% versus 85% versus 66%, P < .001) (Figure 1). Examining disruptions by physician type (hospitalist versus resident) and year of residency (postgraduate years 1–4) did not yield any significant differences.
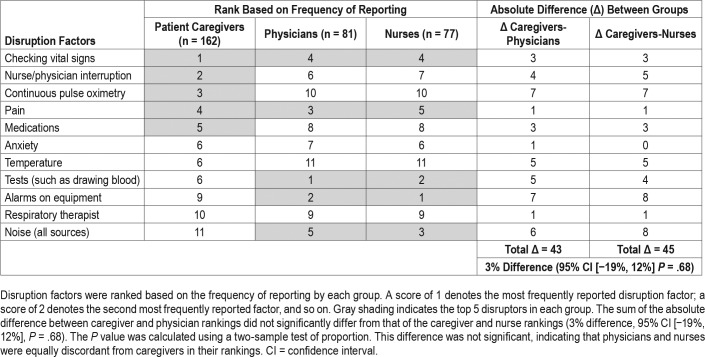
Caregiver, physician, and nurse responses to PHSDNQ disruption questions show lower mean responses by caregivers (1.37 for noise to 2.42 for checking vital signs) than by physicians (2.40 for temperature to 4.38 for tests) and nurses (2.48 for temperature to 4.13 for alarms on equipment) (see Table S1 in the supplemental material). There were several discrepancies among the disruption factor rank order based on mean response between staff (physicians and nurses) and caregivers. Of the top five factors reported by patients, only two (checking vital signs and pain) were also reflected in the top five factors perceived to be disruptive by staff. The other three factors in the caregiver top five ranking (nurse/physician interruption, continuous pulse oximetry, and medications) were ranked much lower by staff. For example, the second most disruptive factor as reported by caregivers, nurse-physician interruption, was not present in the top five factors for either physicians or nurses. Furthermore, continuous pulse oximetry was rated third by patients but was rated 10th by both physicians and nurses. Last, physicians and nurses rated tests such as drawing blood as the first and second most disruptive factor (respectively), but caregivers rated tests as the sixth most disruptive factor.
The sum of the absolute difference between caregiver and physician rankings did not significantly differ from that of the caregiver and nurse rankings (3% difference, 95% confidence interval −19%, 12%, P = .68). This indicates that physicians and nurses were equally discordant from caregivers in their rankings (Table 2).
Table 2.
Absolute differences between the rank of disruption factors based on mean response among pediatric patient caregivers, physicians, and nurses, n = 320.
Physician and Nurse Knowledge and Empowerment
When staff members were surveyed regarding their opinions of pediatric sleep in the hospital, almost all staff agreed that maximizing pediatric patients' sleep in the hospital was important in helping them recover (physicians = 99%, nurses = 97%). However, only 40% of physicians stated that they knew how to help patients sleep better in the hospital and even fewer physicians (33%) reported that they were doing what they can to assist with this process. Nurses were significantly more confident in their knowledge of how to improve pediatric inpatient sleep than physicians (77% versus 40%, P < .001) and reported doing more to help children sleep in the hospital (94% versus 33%, P < .001).
DISCUSSION
To the best of our knowledge, this is the first study to compare caregiver, physician, and nurse perceptions of disruptions of inpatient pediatric sleep. Unlike other studies comparing staff and patient perceptions in the adult setting19 or the pediatric intensive care setting,15 this study examines perceptions of sleep disruption in the pediatric general medicine setting. The most frequent disruptors to pediatric inpatient sleep as reported by caregivers were medical interventions such as checking vital signs, nurse or physician interruption, and continuous pulse oximetry. As hypothesized, more than 30% of patient caregivers reported nurse or physician interruption as being disruptive to patient sleep (48.7%). However, contrary to our second hypothesis, nurses were not more likely than physicians to agree with patients regarding the top disruptors of pediatric inpatient sleep in the hospital. In fact, nurses and physicians largely concurred, with both professional groups disagreeing with caregivers about the factors disrupting pediatric sleep. This finding is surprising in light of the nursing profession's focus on avoiding sleep disruption as emphasized in the American Academy of Nursing's “Choosing Wisely” campaign.18
Based on the results of this study, the factors that disrupted most patients during the night (as reported by caregivers) were checking vital signs, nurse/physician interruption, and continuous pulse oximetry. These results align with other studies that reported nursing disruptions such as checking vital signs and nurse interruption12–14 as the top disruptors of pediatric sleep. A similar study in an adult population found that patients, physicians and nurses agreed that pain, checking vital signs, and tests were the top three disruptors to patient sleep.19 The finding that checking vital signs are a top disruptor aligns with our study, but pain and tests seemed to be less disruptive to the pediatric population. Furthermore, there seemed to be agreement on which factors were ranked as most disruptive among all three groups in an adult medicine setting,19 which is not the case in our study. In addition, a prior study in a pediatric intensive care unit compared staff and caregiver perceptions of sleep disruption and found medical alarms to be the most common cause of disruptive noise,15 a factor that was not one of the top disruptors among patients admitted to the general pediatrics unit.
In contrast to caregivers, when physicians and nurses were asked about what disrupts their patients' sleep, they considered factors such as tests and alarms on equipment to be more disruptive. This discrepancy could be because in general, people tend to report the things they experience as issues. For example, physicians and nurses often hear alarms when they enter rooms and are sensitive to these disruptions. They also could have been exposed to the idea of alarm fatigue in the literature, an area of focus for the Joint Commission Hospital Accreditation program.25 One possible explanation for staff ranking tests and alarms as the top disruption factors is that they could have had a specific group of patients in mind while filling out the survey, such as severely ill patients who require extensive tests and alarms for their care. Caregivers could consider alarms to be less disruptive because hearing alarms reassures them that someone is watching over their child. Last, staff ranked nurse/physician interruption as the fifth or sixth most disruptive factor in the disruption factor rank order. Neither nurses nor physicians had the insight to implicate themselves in the sleep disruptive process.
In general, caregivers reported lower mean and median PHSDNQ response values than staff. However, this could be because caregivers and staff were using the scale differently; caregivers were rating disruption factors from the previous night while staff were considering disruptions for all the patients they have ever cared for. Similarly, caregivers may perceive some disruptions as essential to their child's care and may worry about how a complaint about sleep disruption might be perceived or may affect the care their child receives. Last, literature on patient satisfaction surveys shows that a skew toward positive evaluation of services is common,26 which may explain why caregivers were hesitant to report more intensive disruptions.
This study has important implications for clinicians designing quality improvement (QI) interventions targeted at ameliorating pediatric sleep. The top factors disrupting patient sleep in this study (checking vital signs, nurse/physician interruption, and continuous pulse oximetry) are all medical interventions. The similarity in percentage reporting the top three factors as disruptive to sleep among caregivers and staff reinforces our conclusion that these factors are the most important to target in future QI interventions aimed at improving sleep of hospitalized children. Therefore, in order to maximally benefit patients, future QI initiatives targeting sleep in the hospital should focus on ensuring that only necessary medical interventions are ordered for patients (ie, limiting pulse oximetry and checking vital signs throughout the night when not necessary). The data in this study do not differentiate between medically necessary versus unnecessary interventions. However, “medical necessity” depends on clinical status and disease process, which varies by patient. We cannot determine what is medically necessary for all patients. Looking forward, we hypothesize that the most efficient and realistic way to reduce total disruptions is to focus on decreasing interventions deemed clinically unnecessary by physicians for specific patients, therefore decreasing the likelihood of potential harm to patients.
The discrepancy in perceptions of disruptions among care-givers, nurses, and physicians revealed in the study highlights the need for education of providers, especially considering that the top disruptors discovered in this study are potentially actionable medical interventions. Furthermore, when surveyed regarding their opinions about sleep in the hospital, only 40% of physicians said that they knew how to help patients sleep better and only 33% stated that they were doing what they can to help. These results highlight the need for education of physicians and nurses about sleep disruption in the hospital, and for providing staff with simple interventional measures that result in reduced sleep disruption and improved quantity and quality of sleep. The need for sleep education is not unique to this institution; the Institute of Medicine Committee on Sleep Medicine and Research asserts that awareness of sleep deprivation and sleep disorders is low among health care professionals in the United States.27 Furthermore, a 2005 consensus of pediatric sleep medicine practitioners found that education on healthy pediatric sleep and common pediatric sleep disorders is severely lacking among the medical community.28 Our project presents a vital opportunity to increase awareness about the importance of sleep to the pediatric general medicine population.
Several limitations could have affected the results of this study. First, this was a single-institution study conducted on the pediatric general medicine wards at an academic medical center, which potentially limits the generalizability of study results. In addition, because the patients in this study are minors, parent or guardian response to surveys was required; therefore, the data collected were secondhand perceptions of factors that disrupt sleep rather than firsthand from patients. Furthermore, caregiver data were collected via a convenience sample, which may have led to sampling bias. Several factors that may affect a hospitalized child's sleep patterns were not accounted for, including medications being taken by the patient, post intensive care unit status, and timing of survey collection during hospital stay. An additional limitation is the absence of data regarding patient length of stay and acute versus chronic disease state. In addition, recall bias may have affected the data collection in that staff and caregivers had different perspectives while responding to surveys. Caregivers were asked to report disruptions affecting their child's previous nights' sleep, whereas physicians and nurses were surveyed once regarding the factors that affect their patients' sleep in general. Although the providers surveyed work on the unit where the study was conducted, surveys were not patient specific. In addition, the PHSDNQ has been validated in adult but not pediatric patient populations. Last, no objective measurements of sleep disruption were included in this study. Our group plans to collect objective data using actigraphy in the future.
In summary, this study shows that the most frequent disruptors of inpatient pediatric sleep are medical interventions. In addition, this study suggests that medical professionals have little insight into these disruptors. In order to design an effective patient centered QI intervention, medical interventions should be targeted and staff should be educated about sleep in the hospital.
DISCLOSURE STATEMENT
Work for this study was performed at the University of Chicago. All authors have seen and approved this manuscript. Financial support was provided by NHLBI 5R25HL116372 and 1K24HL136859. REDcap access was provided by the Center for Research Informatics and funded by the Biological Sciences Division and by the Institute for Translational Medicine, CTSA grant number UL1 TR000430 from the National Institutes of Health. The authors report no conflicts of interest.
ACKNOWLEDGMENTS
The authors thank the Pritzker School of Medicine Summer Research Program and the National Heart, Lung and Blood Institute (5R25HL116372, 1K24HL136859) for its generous funding.
ABBREVIATIONS
- PHSDNQ
Potential Hospital Sleep Disruption and Noises Questionnaire
- QI
quality improvement
REFERENCES
- 1.Smaldone A, Honig JC, Byrne MW. Sleepless in America: Inadequate sleep and relationships to health and well-being of our nation's children. Pediatrics. 2007;119(Supplement 1):S29–S37. doi: 10.1542/peds.2006-2089F. [DOI] [PubMed] [Google Scholar]
- 2.Paruthi S, Brooks LJ, D'Ambrosio C, et al. Recommended amount of sleep for pediatric populations: a consensus statement of the American Academy of Sleep Medicine. J Clin Sleep Med. 2016;12(6):785–786. doi: 10.5664/jcsm.5866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Arora VM, Chang KL, Fazal AZ, et al. Objective sleep duration and quality in hospitalized older adults: associations with blood pressure and mood. J Am Geriatr Soc. 2011;59(11):2185–2186. doi: 10.1111/j.1532-5415.2011.03644.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.DePietro RH, Knutson KL, Spampinato L, et al. Association between inpatient sleep loss and hyperglycemia of hospitalization. Diabetes Care. 2017;40(2):188–193. doi: 10.2337/dc16-1683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Delaney LJ, Van Haren F, Lopez V. Sleeping on a problem: the impact of sleep disturbance on intensive care patients - a clinical review. Ann Intensive Care. 2015;5:3. doi: 10.1186/s13613-015-0043-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lee S, Narendran G, Tomfohr-Madsen L, Schulte F. A systematic review of sleep in hospitalized pediatric cancer patients. Psychooncology. 2017;26(8):1059–1069. doi: 10.1002/pon.4149. [DOI] [PubMed] [Google Scholar]
- 7.Kudchadkar S, Aljohani O, Punjabi NM. Sleep of critically ill children in the pediatric intensive care unit: a systematic review. Sleep Med Rev. 2014;18(2):103. doi: 10.1016/j.smrv.2013.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.McCann D. Sleep deprivation is an additional stress for parents staying in hospital. J Spec Pediatr Nurs. 2008;13(2):111–122. doi: 10.1111/j.1744-6155.2008.00142.x. [DOI] [PubMed] [Google Scholar]
- 9.Agency for Healthcare Research and Quality. The CAHPS Child Hospital Survey. [Accessed June 28, 2017]. https://www.ahrq.gov/cahps/surveys-guidance/hospital/about/child_hp_survey.html.
- 10.Young JS, Bougeois JA, Hilty DM, Hardin KA. Sleep in hospitalized medical patients, part 1: factors affecting sleep. J Hosp Med. 2008;3(6):473–482. doi: 10.1002/jhm.372. [DOI] [PubMed] [Google Scholar]
- 11.Oliveira L, Gomes C, Bacelar Nicolau L, Ferreira L, Ferreira R. Environment in pediatric wards: light, sound, and temperature. Sleep Med. 2015;16(9):1041–1048. doi: 10.1016/j.sleep.2015.03.015. [DOI] [PubMed] [Google Scholar]
- 12.Bisogni S, Chiarini I, Giusti F, Ciofi D, Poggi GM, Festini F. Impact of hospitalization on the sleep patterns of newborns, infants and toddlers admitted to a pediatric ward: a cross-sectional study. Minerva Pediatr. 2015;67(3):209–217. [PubMed] [Google Scholar]
- 13.Herbert AR, de Lima J, Fitzgerald DA, Seton C, Waters KA, Collins JJ. Exploratory study of sleeping patterns in children admitted to hospital. J Paediatr Child Health. 2014;50(8):632–638. doi: 10.1111/jpc.12617. [DOI] [PubMed] [Google Scholar]
- 14.Meltzer LJ, Davis KF, Mindell JA. Patient and parent sleep in a children's hospital. Pediatr Nurs. 2012;38(2):64–71. [PubMed] [Google Scholar]
- 15.Kaur H, Rohlik GM, Nemergut ME, Tripathi S. Comparison of staff and family perceptions of causes of noise pollution in the Pediatric Intensive Care Unit and suggested intervention strategies. Noise Health. 2016;18(81):78. doi: 10.4103/1463-1741.178480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Stremler R, Adams S, Dryden-Palmer K. Nurses' views of factors affecting sleep for hospitalized children and their families: a focus group study. Res Nurs Health. 2015;38(4):311–322. doi: 10.1002/nur.21664. [DOI] [PubMed] [Google Scholar]
- 17.Nightingale F. Notes on Nursing: What It Is, and What It Is Not. 1st ed. New York, NY: D. Appleton and Company; 1860. [Google Scholar]
- 18.American Academy of Nursing. Choosing Wisely: Sleep - Twenty Things Nurses and Patients Should Question. [Accessed July 5, 2017]. http://www.aannet.org/initiatives/choosing-wisely/sleep.
- 19.Grossman MN, Anderson SL, Worku A, et al. Awakenings? Patient and hospital staff perceptions of nighttime disruptions and their effect on patient sleep. J Clin Sleep Med. 2017;13(2):301–306. doi: 10.5664/jcsm.6468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sadeh A, Mindell JA, Luedtke K, Wiegand B. Sleep and sleep ecology in the first 3 years: a web-based study. J Sleep Res. 2009;18(1):60–73. doi: 10.1111/j.1365-2869.2008.00699.x. [DOI] [PubMed] [Google Scholar]
- 21.Gabor JY, Cooper AB, Crombach SA, et al. Contribution of the intensive care unit environment to sleep disruption in mechanically ventilated patients and healthy subjects. Am J Respir Crit Care Med. 2003;167(5):708–715. doi: 10.1164/rccm.2201090. [DOI] [PubMed] [Google Scholar]
- 22.Topf M. Personal and environmental predictors of patient disturbance due to hospital noise. J Appl Psychol. 1985;70(1):22–28. [PubMed] [Google Scholar]
- 23.Dunbar B. Exploration: Then and Now - Survival! Lesson. NASA. [Accessed June 5, 2018]. https://www.nasa.gov/audience/foreducators/topnav/materials/listbytype/Survival_Lesson.html. Published July 17, 2009.
- 24.StataCorp. Stata Statistical Software: Release 15. College Station, TX: StataCorp LLC; 2017. [Google Scholar]
- 25.Joint Commission. 2017 Hospital National Patient Safety Goals. [Accessed August 18, 2017]. https://www.jointcommission.org/assets/1/6/2017_NPSG_HAP_ER.pdf.
- 26.Crow R, Gage H, Hampson S, et al. The measurement of satisfaction with healthcare: implications for practice from a systematic review of the literature. Health Technol Assess. 2002;6(32):1–244. doi: 10.3310/hta6320. [DOI] [PubMed] [Google Scholar]
- 27.Colten HR, Altebogt BM. Sleep Disorders and Sleep Deprivation: an Unmet Public Health Problem. Washington, DC: Institute of Medicine (US) Committee on Sleep Medicine and Research, National Academies Press (US); 2006. [PubMed] [Google Scholar]
- 28.Owens JA, Mindell JA. Pediatric sleep medicine: priorities for research, patient care, policy and education. A report from the conference held February 19-20, 2005, Amelia Island, Florida. J Clin Sleep Med. 2006;2(1):77–88. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.