Abstract
We introduce a low-fidelity, low-cost, reusable training model for the lateral canthotomy procedure. We believe that this trainer has the potential to improve clinicians’ knowledge and skill of the procedure, especially when cost or access to higher-fidelity trainers is prohibitive.
African Relevance
-
•
This article describes a novel low-cost medical education approach, appropriate to many African contexts.
-
•
It is an easily-reproducible solution for teaching a low occurrence, high risk procedure.
Introduction
Permanent vision loss is a rare but serious complication of orbital trauma. The most reversible cause of traumatic blindness is acute ocular compartment syndrome (AOCS), usually secondary to retrobulbar haemorrhage (RBH), intra-orbital oedema or more rarely orbital emphysema [1]. Timely diagnosis of AOCS and surgical decompression by lateral canthotomy of the ocular compartment has been shown to decrease the incidence of permanent blindness. Obtaining and maintaining procedural competency can be difficult due to the low incidence of RBH and AOCS, and the lack of access to trainers. This article discusses the construction and utilisation of a reusable non-cadaveric model, which simulates the orbital anatomy and can be used to teach and practice the lateral canthotomy procedure.
This low-fidelity eye model was invented to provide clinicians with hands on training in the lateral canthotomy procedure on a reproducible non-cadaveric model. Although cadaveric models have been shown to be effective, their use has limitations: the procedure can only be performed once or twice per cadaver, and at high cost. Porcine models and commercially available high-fidelity trainers share the same limitations. This is especially problematic in resource-limited areas where it may be cost prohibitive to obtain cadavers or commercial trainers. Our low-cost reproducible low-fidelity eye model is a potential solution to this problem and can be made from materials readily available in many countries.
Methods
Construction and utilisation of the low-fidelity eye model is demonstrated in the following figures and instructions. The items required are described in Box 1 and Fig. 1.
Box 1. The items required to construct the low-fidelity eye model.
-
•
1 standard size table tennis ball.
-
•
10 ml Ziploc recyclable container.
-
•
Pressure foam tape.
-
•
Scotch tape.
-
•
Transpore tape 3 M™.
-
•
Silk tape.
-
•
Tape roll.
-
•
Rubber band.
-
•
Scissors.
-
•
Scalpel.
Fig. 1.

Items needed.
Model assembly
Step 1: Cut out a rectangular-shaped hole on the base of the container with a scalpel, insert the ball into the container approximating to the rectangular hole made (Fig. 2A and B). Support the ball with tape.
Fig. 2.
A and B Step 1 of assembly.
Step 2: Cut the circular rubber band at one point so that you have a straight band. Then bisect the middle third of the rubber band lengthwise, to simulate the inferior and superior limbs of the lateral canthus tendon (Fig. 3).
Fig. 3.

Step 2 of assembly.
Step 3: Cut two pieces of Transpore 3 M™ tape, fold each and place at the 12 and 6o’clock positions of the rubber band bisections (Fig. 4).
Fig. 4.

Step 3 of assembly.
Step 4: Begin construction of the soft tissue of the orbit by cutting two pieces of foam tape. Then cut out two small flaps near the lateral margins of the tape and fold them down. You are now left with three flaps: one large middle flap, and two small side flaps (Fig. 5A and B).
Fig. 5.
A and B Step 4 of assembly.
Step 5: Place the pieces of foam tape on the 6o’clock and 12o’ clock positions of the rubber band. Position the lateral edges of the small flaps in front of the point of rubber band bisection then fold the middle portion of the foam tape over the rubber band (Fig. 6A and B).
Fig. 6.
A and B Step 5 of assembly.
Step 6: Place the adjusted foam tape on the inferior edge of the tape, then repeat Step 7 for the foam tape placed on the superior edge. Take the tape hanging off the 6o’clock and 12o’clock positions and tape to the container. Place Transpore 3 M™ tape around the foam tape on the superior and inferior edges of the orbit (Fig. 7A and B).
Fig. 7.
A and B Step 6 of assembly.
Model demonstration
For the model demonstration, you will need a haemostat, a pickup, a pair of scissors and a syringe with a 25 gauge needle (+/−) containing saline solution.
Step 1: Inject the saline (simulated local anaesthetic) into the lateral crease of tape (Fig. 8A).
Fig. 8.
A and B Steps 1 and 2 of model demonstration.
Step 2: Clamp a haemostat over the foam tape at the same edge of the orbit where the saline was injected, and leave for one minute (Fig. 8B).
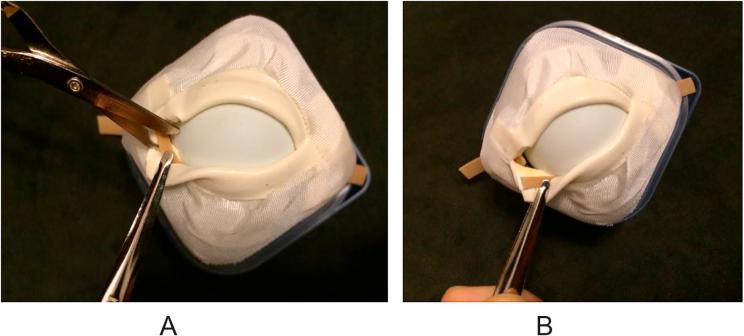
Step 3: Remove the haemostat and cut horizontally into the soft tissue then expose and cut the inferior crus of the canthus tendon (Fig. 9A and B).
Fig. 9.
A and B Step 3 of model demonstration.
Discussion
Trauma, while declining globally, is still a significant contributor to the Global Burden of Disease, which disproportionately affects low- and middle-income countries (LMICs) [2]. RBH is a rare complication of midface trauma, with an associated incident of blindness as high as 48% [4], [5], [6]. An accompanying AOCS, leading to retina and optic nerve compression, is believed to be the causative mechanism [7].
Timely orbital compartment decompression by performing a lateral canthotomy has been shown to preserve a patient’s vision. In an observational study by Fattahi et al, patients who received lateral canthotomy two or more hours after injury had an incomplete return of vision. Animal studies have demonstrated that irreversible optic nerve ischemic damage in monkeys can occur in 60–100 min [8]. To prevent irreversible orbital ischemia and blindness, AOCS requires prompt diagnosis and surgical decompression.
Lateral canthotomy is a time-sensitive, vision-saving, emergent procedure that requires regular practice for maintenance of skill. However, the incident of RBH is low, and not all require lateral canthotomy. In one American Level I trauma centre, the five-year incidence of traumatic RBH after orbital fracture or trauma was 3.6%. Of those, a little more than half received lateral canthotomy, averaging only about five such procedures per year [9]. This may overstate overall incidence somewhat, as other retrospective data suggest RBH after orbital fracture occurs at an even lower rate of <1% [3]. Given this low frequency of actual application, regular training on task trainers or biologic models is necessary to maintain procedural competency.
As previously stated, cadaveric and commercially available models are expensive and typically can only be used a limited number of times. For example, the SynDaver™ Labs Lateral Canthotomy Trainer, priced at USD750, is a high-fidelity trainer with many tactile, visual and structural details, but provides only two opportunities to perform lateral canthotomy per trainer, and cannot be “reset” for additional uses.
Our trainer was designed to be inexpensive, easy to set up, and reusable. We fabricated 32 trainers for approximately USD160, designed to allow two procedures per trainer, or a total of 64 uses for our initial production. Construction, resetting and maintenance of the trainer required only scissors, a craft knife, and a short primer on the design. In our institution, 24 learners simultaneously used the trainers during two different educational conferences over a two-year period. Each user performed the procedure twice on average, per conference. The body of the trainers remained in good repair. Rubber band and tape replacement costs were about USD35 over this period. Users uniformly stated they were more confident to perform the procedure, but this was not rigorously measured.
Our model provides just enough anatomical detail to serve as a platform to perform the basic steps of the procedure. This is appropriate for beginners – in order to learn and repeat the steps of the procedure – or for those who simply wish to focus on these steps. The trainer is not appropriate for use in high-fidelity simulation, where tactile, visual and functional verisimilitude is an essential part of the learning experience. Another limitation is the time needed to assemble the trainers. In our experience, it took the designer and an assistant about four hours to fabricate the initial production of 32 trainers (this included a brief construction primer for the assistant).
Each of the authors contributed to the study concept and design, analysis and interpretation of the data and drafting of the manuscript.
The study was approved by the Staten Island University Hospital IRB.
There was no financial support or conflict of interest of the investigation or manuscript development.
Conflicts of interest
The authors have no conflicts to declare.
Authors’ contributions
DK, RK, ECP, and JG all conceived, designed and conducted the work. All were involved in the drafting of the manuscript and all approve the final version.
Footnotes
Peer review under responsibility of African Federation for Emergency Medicine.
References
- 1.Soare S. Update on orbital decompression as emergency treatment of traumatic blindness. J Craniomaxillofac Surg. 2015;43(7):1000–1003. doi: 10.1016/j.jcms.2015.05.003. [DOI] [PubMed] [Google Scholar]
- 2.Haagsma J.A., Graetz N., Bolliger I., Naghavi M., Higashi H., Mullany E.C. The global burden of injury: incidence, mortality, disability-adjusted life years and time trends from the Global Burden of Disease study 2013. Inj Prev. 2016;22:3–18. doi: 10.1136/injuryprev-2015-041616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ballard S., Enzenauer R.W., O’Donnell T. Emergency lateral canthotomy and cantholysis: A simple procedure to preserve vision from sight threatening orbital hemorrhage. J Spec Oper Med. 2009;9:26. doi: 10.55460/1CLD-XJUV. [DOI] [PubMed] [Google Scholar]
- 4.Kloss B.T., Patel R. Orbital compartment syndrome from retrobulbar hemorrhage. Int J Emerg Med. 2010;3:521. doi: 10.1007/s12245-010-0245-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lee K.Y.C., Fong K. Visual recovery following emergent orbital decompression in traumatic retrobulbar haemorrhage. Ann Acad Med Singapore. 2006;35:831. [PubMed] [Google Scholar]
- 6.Ansari M.H. Blindness after facial fractures: a 19-year retrospective study. J Oral Maxillofac Surg. 2005;63:229–237. doi: 10.1016/j.joms.2004.05.221. [DOI] [PubMed] [Google Scholar]
- 7.Hayreh S.S., Weingeist T.A. Experimental occlusion of the central artery of the retina. IV: Retinal tolerance time to acute ischaemia. Br J Ophthalmol. 1980;64(11):818–825. doi: 10.1136/bjo.64.11.818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ferguson I.M.C. A human cadaveric workshop: One solution to competence in the face of rarity. Emerg Med Australas. 2016;28(6):752–754. doi: 10.1111/1742-6723.12601. [DOI] [PubMed] [Google Scholar]
- 9.Fattahi T. Incidence of retrobulbar hemorrhage in the emergency department. J Oral Maxillofac Surg. 2014;72:2500–2502. doi: 10.1016/j.joms.2014.06.457. [DOI] [PubMed] [Google Scholar]