Abstract
Introduction
Purulent pericarditis poses diagnostic and therapeutic challenges, especially in resource-limited settings due to the unavailability of diagnostic tools, equipment, and expertise.
Case report
A three-year-old female presented to the emergency centre at Muhimbili National Hospital in Dar es Salaam, Tanzania with altered mental status, lethargy, intermittent fevers, worsening difficulty in breathing, and progressive lower extremity swelling over two months. The child was in shock upon arrival. Point-of-care ultrasound demonstrated cardiac tamponade secondary to purulent pericarditis. An ultrasound guided pericardiocentesis and lavage was successfully done in the emergency centre and antibiotics were started. Though definitive management (pericardiectomy) was delayed, the child survived to hospital discharge.
Conclusion
Pericardiocentesis, pericardial lavage, and the initiation of broad spectrum antibiotics are the mainstay of early treatment of purulent pericarditis. This treatment can be done safely in an emergency centre with little specialised equipment aside from point-of-care ultrasound.
Keywords: Emergency department, Pericarditis, Pediatrics, Tanzania
African relevance
-
•
Managing purulent pericarditis in resource-limited settings is challenging.
-
•
Bedside ultrasound in the emergency centre can help with early diagnosis.
-
•
Pericardiocentesis can be safely performed in the emergency centre with minimal equipment other than bedside ultrasound.
Introduction
Purulent pericarditis is a life-threatening condition that can compromise the haemodynamic status of a patient by causing cardiac tamponade. It has been associated with high mortality if treatment is delayed [1]. In resource-limited settings, purulent pericarditis can be challenging to diagnose and treat due to the lack of diagnostic tools, equipment, and expertise [2]. We present a case of purulent pericarditis in the Emergency Centre at Muhimbili National Hospital (EC-MNH) in Dar es Salaam, Tanzania.
Case report
A previously healthy, fully immunised, three-year-old female presented to the EC-MNH with altered mental status, lethargy, intermittent fevers, worsening difficulty in breathing, and progressive lower extremity swelling over the past two months.
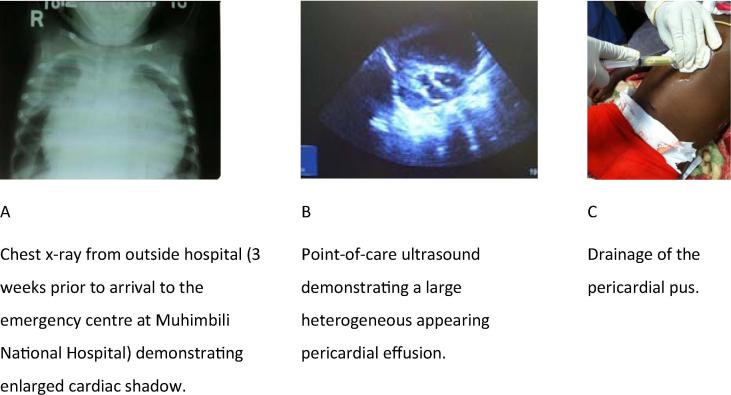
The patient had developed a high fever, fatigue, and generalised body malaise two months prior. She was treated at a local clinic with antibiotics and antimalarials, but her mother was never told a specific diagnosis. The patient improved, but did not return to baseline, and three weeks after her initial clinic visit, she began to have difficulty breathing. She was taken to multiple peripheral health centres during her fourth week of illness, and was given medications, but did not improve. Her mother then travelled to the nearest hospital, about 125 km from her village, where a chest X-ray was done. It showed cardiomegaly (Fig. 1a). The patient was diagnosed with heart failure of unknown origin, started on furosemide, digoxin, and benzylpenicillin, and sent home. Over the next three weeks, the patient worsened despite strict adherence to the medications. The patient’s mother was concerned, and, seeking a higher level of medical care, took a two-day train ride to Dar es Salaam with her sick child. She went directly from the train station to EC-MNH.
Fig. 1.
Images associated with emergency centre care.
On arrival, the patient was ill appearing and in severe respiratory distress with pallor and diaphoresis. Her vital signs were: temperature 37 °C, blood pressure 60/40, pulse 138, respiration rate 40, oxygen saturation 86% (on 15L non-rebreather mask). Her weight was 8.2 kg. The remainder of her exam revealed muffled heart sounds, cold extremities with absent peripheral pulses in both the upper and lower extremities, distended neck veins, and 2+ pitting oedema in her lower extremities and dependent areas. Her lungs had bilateral lower lobe crackles with significant accessory muscle use. She was minimally interactive and only made purposeful movements to painful stimuli.
She was placed on oxygen and given a normal saline bolus. An electrocardiogram showed sinus tachycardia with low voltage QRS complexes. Point-of-care ultrasound demonstrated a large, heterogeneous-appearing pericardial effusion with tamponade physiology including complete collapse of the right ventricle during diastole (Fig. 1b). The ultrasound also revealed bilateral pleural effusions and free fluid in the abdomen that we interpreted as ascites.
Due to cardiac tamponade, an emergent pericardiocentesis was performed. The patient underwent moderate sedation with ketamine. The area was prepped in the usual sterile manner, and under ultrasound guidance using the subxiphoid approach, an 18-gauge cannula attached to a 20 mL syringe was used to aspirate the pericardial pus.
The pericardiocentesis drained 350mls of pus (Fig. 1c), after which the patient’), aemodynamics improved: her blood pressure increased to 80/52, distal pulses were palpable, and the patient began to speak. The pericardium was flushed three times with normal saline, and the patient was given ceftriaxone and metronidazole. Attempts to place a pericardial catheter for continued drainage were unsuccessful due to thick pus that could not be aspirated via the thin catheters available. HIV testing was negative.
The patient was admitted to the paediatric ward with the diagnoses of purulent pericarditis causing tamponade, shock, and severe acute malnutrition. The cardiology service was consulted on admission and they reviewed the patient, but the patient was unstable, malnourished, and they had concern for disseminated tuberculosis (TB). Therefore, they decided that the patient was not fit for a cardiac procedure and she remained in the paediatric ward. Her pericardial cultures grew E. coli.
An echocardiogram performed on hospital day three showed small loculations remaining in the pericardium. Cardiology then decided to perform a pericardial window or pericardiectomy; however, they wished for the patient to be medically optimised before surgery. She remained in the ward with supportive care, antibiotics tailored to culture growth, empiric anti-TB medication, and a nutritional program consisting of F75 milk and Plumpy’Nut.
After two months in the ward, the patient had no further signs of infection, multiple TB tests were negative, she had only minimal peripheral oedema, no respiratory symptoms, and good weight gain. She was cleared for surgery. Intraoperatively, they found a fibrotic pericardium completely adherent to the heart with multiple tissue growths, and a pericardectomy was performed. The patient was discharged home in good condition one week after the procedure.
Discussion
In resource-limited settings, early diagnosis and treatment of purulent pericarditis may be difficult because of limited equipment, diagnostic tools, and expertise [3]. We were able to diagnose this condition with ultrasound; however, our EC is the only full-capacity EC in Tanzania, and one of the few with ultrasound [4]. In many areas of Tanzania, like most low- and middle-income countries, emergency care facilities are limited, scattered, and not adequately equipped, resulting in a delayed diagnosis despite the patient seeking healthcare in multiple facilities prior to arrival at our EC [5]. We believe that this case illustrates the difficulties of seeking emergency care in developing healthcare systems, but highlights the role that emergency care can take in these settings.
In our EC, ultrasound revealed cardiac tamponade and we performed an immediate ultrasound guided pericardiocentesis and lavage, which was lifesaving. As well as removal of the pus, and lavage, we started the patient on broad-spectrum antibiotics.
Purulent pericarditis is most often caused by Streptococcus pneumoniae and Staphylococcus aureus [6], [7], [8], [9]. However, there is limited data about the incidence and causative agents in resource-limited settings. Published case reports from Africa have identified co-infection with TB and other atypical organisms more commonly than reports from high-income countries [8], [10]. In our case, the patient had E. coli as a causative agent. E.coli is a rare etiological agent in cases of purulent pericarditis, mostly associated with bacteraemia from genitourinary system [10]. It can be associated with immunosuppression [11]. We believe that our patient was susceptible to this condition because of immunosuppression from malnutrition, as no other risk factors for infection were identified.
In the case of purulent pericarditis causing tamponade, early pericardiocentesis, lavage, and initiation of broad-spectrum antibiotics can be performed in the EC, and can lead to good clinical outcomes even if further care is delayed. Strengthening emergency care systems throughout Tanzania will strengthen the overall health system.
Conflicts of interest
The authors declare no conflicts of interest.
Dissemination of results
This case was shared with staff members of Muhimbili National Hospital’s emergency centre through an informal presentation followed by discussion.
Authors’ contributions
CR and BM received and managed the case including follow up and writing of the case report. KD corrected grammar, HS revised the report and gave cultural advise on the case. CR, BM, KD and HS approved the final version that was submitted.
Sources
The compilation of this case report used no specific funding.
Footnotes
Peer review under responsibility of African Federation for Emergency Medicine.
Supplementary data associated (An author-translated French version) with this article can be found, in the online version, at https://doi.org/10.1016/j.afjem.2017.12.002.
Appendix A. Supplementary data
References
- 1.Pankuweit S., Ristić A.D., Seferović P.M. Bacterial pericarditis: diagnosis and management. Am J Cardiovasc Drugs Drugs Devices Interv. 2005;5(2):103–112. doi: 10.2165/00129784-200505020-00004. [DOI] [PubMed] [Google Scholar]
- 2.Simonÿ C.F.B., Malham M., Kanstrup J. Lifesaving pericardiocentesis due to purulent pericarditis with growth of Gram-negative rods in an immune-competent Inuit male. Int J Emerg Med. 2014;7:21. doi: 10.1186/s12245-014-0021-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.dos Santos L.F., Moreira D., Ribeiro P. Purulent pericarditis: a rare diagnosis. Rev Port Cardiol. 2013 Jan 9;32(09):721–727. doi: 10.1016/j.repc.2013.07.003. [DOI] [PubMed] [Google Scholar]
- 4.Latyshev Y., Mathew A., Jacobson J.M. Purulent pericarditis caused by haemophilus parainfluenzae. Tex Heart Inst J. 2013;40(5):608–611. [PMC free article] [PubMed] [Google Scholar]
- 5.Reynolds T.A., Mfinanga J.A., Sawe H.R. Emergency care capacity in Africa: a clinical and educational initiative in Tanzania. J Public Health Policy. 2012 Dec;33(S1):S126–37. doi: 10.1057/jphp.2012.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tokuyasu H., Saitoh Y., Harada T. Purulent pericarditis caused by the Streptococcus milleri group: a case report and review of the literature. Int Med Tokyo Jpn. 2009;48(12):1073–1078. doi: 10.2169/internalmedicine.48.2109. [DOI] [PubMed] [Google Scholar]
- 7.Petcu C.P., Dilof R., Bătăiosu C., Petcu P.D. Purulent pericardial effusions with pericardial tamponade – diagnosis and treatment issues. Curr Health Sci J. 2013;39(1):53–56. [PMC free article] [PubMed] [Google Scholar]
- 8.Tomkowski W.Z., Kuca P., Gralec R. Management of purulent pericarditis. Monaldi Arch Chest Dis Arch Monaldi Mal Torace Fondazione Clin Lav IRCCS Ist Clin Tisiol E Mal Appar Respir Univ Napoli Secondo Ateneo. 2003 Dec;59(4):308–309. [PubMed] [Google Scholar]
- 9.Kabbani M.S., Najm H., Godman M. Five children with purulent pericarditis and review of the literature. Ann Trop Paediatr. 2004 Mar;24(1):95–101. doi: 10.1179/027249304225013277. [DOI] [PubMed] [Google Scholar]
- 10.Megged O., Argaman Z., Kleid D. Purulent pericarditis in children: is pericardiotomy needed? Pediatr Emerg Care. 2011 Dec;27(12):1185–1187. doi: 10.1097/PEC.0b013e31823b44af. [DOI] [PubMed] [Google Scholar]
- 11.Rallidis L.S., Thomaidis K.P., Vlasseros I.N. Successful treatment of staphylococcal pericarditis with early catheter drainage and antibiotics. Acta Cardiol. 1997;52(5):437–443. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.