Abstract
Introduction
The effect of patient position and patient cooperation on the accuracy of emergency weight estimation systems has not been evaluated previously. The objective of this study was to evaluate weight estimation accuracy of the Broselow tape, the PAWPER XL tape, the Mercy method, and a custom-designed mobile phone App in a variety of realistic simulated paediatric emergencies.
Methods
This was a prospective study in which 32 emergency medicine volunteers participated in eight simulations of common paediatric emergency conditions, using children models. The participants used each of the four methods to estimate the children’s weight. The accuracy of and time taken for the weight estimations were evaluated for each method. A regression analysis determined the effects of patient position and cooperation on weight estimation accuracy. Evaluation of subgroups of best-performers and worst-performers among the participants provided information on the effects of human user-error on weight estimation accuracy.
Results
The Broselow tape, Mercy method, App and the PAWPER XL tape achieved percentages of weight estimation within 10% of actual weight in 47.7, 57.3, 68.1, and 73.0% of estimations, respectively. Patient position and cooperation strongly impacted the accuracy of the Broselow tape, had a minimal effect on the Mercy method and the App, and had no effect on the PAWPER XL tape. The best performing participants achieved very high accuracy with all methods except the Broselow tape.
Discussion
The Mercy method, the App, and the PAWPER XL tape achieved exceptionally high accuracy even in uncooperative and sub-optimally positioned children when used by the best-performing participants. Human error, from inexperience and inadequate training, had the most significant impact on accuracy. The Mercy method was the most subject to human error, and the PAWPER XL tape, the least. Adequate training in using weight estimation systems is essential for paediatric patient safety.
Keywords: Body weight, Resuscitation, Paediatric weight estimation, Broselow tape, PAWPER tape, Mercy method
African relevance
-
•
Children in Africa and other low- and middle-income countries are vulnerable to inaccurate weight estimation in emergencies.
-
•
The effect of paediatric patient position on emergency weight estimation is unknown.
-
•
The effect of paediatric patient cooperation on emergency weight estimation is unknown.
-
•
Accurate weight estimation in children in emergencies is feasible with economical equipment options.
Introduction
During the management of paediatric emergencies, errors in drug dosing arising from inaccurate estimations of weight can potentially lead to poor outcomes [1], [2], [3]. It is therefore imperative that weight-estimation errors be minimised, so that optimum treatment can be delivered during emergency care. Weight estimation systems that have been proven to be accurate should be used and healthcare providers should be well-trained in their use [4], [5]. An accurate weight estimation system, however, may not necessarily lead to accurate weight determination as there are other potential sources of errors that must be considered [6], [7], [8]. Health care providers must account for the complexity of the weight estimation system, the experience of the users in weight estimation, and patient factors. These include: inherent limitations of the weight estimation system itself (e.g., age-based weight estimation is not accurate) [9], incorrect use of the device or system [10], [11] (even simple systems are susceptible to error when used by under-trained individuals [12], [13], [14]), or there may be difficulty in using the device or system because of suboptimal patient positioning or uncooperative patients (e.g., the use of a length-based tape in a sitting patient or in a combative, hypoxic child).
Two-dimensional weight estimation systems, which make use of length and habitus to estimate a weight, such as the Mercy method and the PAWPER XL tape, are the most accurate of all the existing weight estimation methodologies [2], [15]. However, they have never been evaluated under real or simulated resuscitation conditions. These systems are slightly more complex than simple length-based methods and so, may be more vulnerable to human errors during the stress of emergency care. A weight estimation system that is accurate, but unusable during emergencies, would be of little value.
Advances in technology can also be applied in this setting to reduce errors and cognitive load in emergencies. A mobile-phone App that could rapidly provide accurate point-of-care estimations of weight could be extremely useful. The Emergency Drug Dosing 4 Children App was designed to generate estimations of weight, but it has not previously been formally evaluated for patient and human factors [16].
The aim of this study was primarily to evaluate the accuracy of the four weight estimation systems, the Broselow tape, the Mercy method, the PAWPER XL tape, and a weight estimation App, under realistic simulated resuscitation scenarios. We also aimed to establish whether patient factors, including patient positioning and patient cooperation, and participant human error factors, including individual variations in competency, had a substantial impact on the accuracy of the weight estimation.
Methods
This study was a prospective, simulation study conducted in the Emergency Centre of a tertiary, academic hospital in Johannesburg, South Africa. Emergency medicine registrars, emergency medicine consultants, and senior advanced life support paramedics invited to participate in the study. All participants had at least five years’ postgraduate experience. Permission to conduct the study was obtained from the Human Research Ethics Committee of the University of the Witwatersrand. All participants signed an informed consent form. An estimated sample size of 30 participants was required to detect a 10% difference in accuracy between the methods based on the McNemar test, powered to 80% at a 0.05 significance level and assuming a baseline accuracy of 70%.
Eight simulation stations were prepared, each recreating a commonplace emergency scenario, with a child volunteer who simulated the medical condition, patient position, and degree of cooperation specified for the scenario (Table 1). The scenarios were chosen to recreate a spectrum of common realistic medical circumstances in which children might not be supine and not cooperative. Some children were fully cooperative, some simulated actively uncooperative patients, such as with a seizure, and some were passively uncooperative, such as during a cardiac arrest. The children were positioned in clinically realistic positions, for example, a supine position for a child in cardiac arrest and a sitting position for a child in respiratory distress.
Table 1.
Details of simulation scenarios, simulated patients and the demographic characteristics of the participants.
| Station number | Characteristics of simulated patient | Clinical scenario including position of child and cooperation | Order of weight estimation methods |
|---|---|---|---|
| 1 | Age: 9 years Weight: 22.5 kg Length: 130 cm HS: 1 (very underweight) |
Cardiac arrest Supine on bed Floppy, no cooperation or resistance |
PTXL, APP, MM, BT |
| 2 | Age: 12 years Weight: 39.6 kg Length:151 cm HS: 4 (overweight) |
Status epilepticus Lateral position on bed Arms and legs jerking, no cooperation |
APP, MM, BT, PTXL |
| 3 | Age: 11 years Weight: 34.2 kg Length: 145 cm HS: 3 (average) |
Respiratory distress – severe asthma Sitting on bed. Will not lie down Anxious, semi-cooperative |
BT, PTXL, APP, MM |
| 4 | Age: 13 years Weight: 55.8 kg Length: 156 cm HS: 5 (obese) |
Major trauma with abdominal injuries Immobilised supine on stretcher Cooperative |
MM, PTXL, BT, APP |
| 5 | Age: 16 years Weight: 61.2 kg Length: 174 cm HS: 3 (average) |
Major trauma with head injury GCS 10/15 Supine on spine board Uncooperative, irritable |
MM, BT, PTXL, APP |
| 6 | Age: 1 year Weight: 11.7 kg Length: 80 cm HS: 4 (overweight) |
Severe gastroenteritis with hyperkalaemia Sitting on mom’s lap Not cooperative |
APP, MM, BT, PTXL |
| 7 | Age: 8 years Weight: 31.2 kg Length: 132 cm HS: 4 (overweight) |
Unstable supraventricular tachycardia Semi-recumbent on bed Fully cooperative |
PTXL, MM, APP, BT |
| 8 | Age: 7 years Weight: 26.4 kg Length: 131 cm HS: 2 (underweight) |
Severe pneumonia with hypoglycaemia Sitting down. Floppy. Semi-cooperative |
BT, APP, PTXL, MM |
| Characteristics of participants | ||||
| Qualification | N | Sex – male n (%) | Experience Years median (LQ, UQ) | Confidence with children score median (LQ, UQ) |
| All | 32 | 21 (65.6) | 5.5 (3.0, 11.5) | 6 (4, 7) |
| Emergency medicine registrars | 21 | 14 (66.7) | 5.0 (4.0, 6.8) | 6 (4, 7) |
| Emergency medicine consultants | 5 | 1 (20.0) | 9.0 (7.5, 9.8) | 7 (7, 7) |
| Senior advanced life support paramedics | 6 | 6 (100) | 12.5 (11.3, 15.3) | 7 (7, 8) |
HS, habitus score; PTXL, PAWPER XL tape; MM, Mercy method; BT, Broselow tape; LQ, lower quartile; UQ, upper quartile.
All participants attended a formal one-hour training session with the weight estimation methods and had an opportunity to practice to their satisfaction before starting the simulation. At each station, every participant used all four techniques to estimate weight. The sequence of methods used was different in each station, based on a randomised, pre-determined order. The participants were instructed to obtain each weight estimate independently, not taking the results of the other methods into account. They were informed that the estimations might not be the same between the different methods. They were blinded to the measured weight of the children and the weight estimates of other participants. The time taken to estimate the weights was recorded by a time-keeper.
Upon completion of the six minutes allocated for each station, the participants rotated to the next station until all eight stations were completed. The participants then completed a questionnaire on their experiences with the different systems. Finally, the investigators, experts in the use of the weight-estimation methods, used each system in each child model, now fully cooperative, to provide control data for weight estimation accuracy under ideal circumstances.
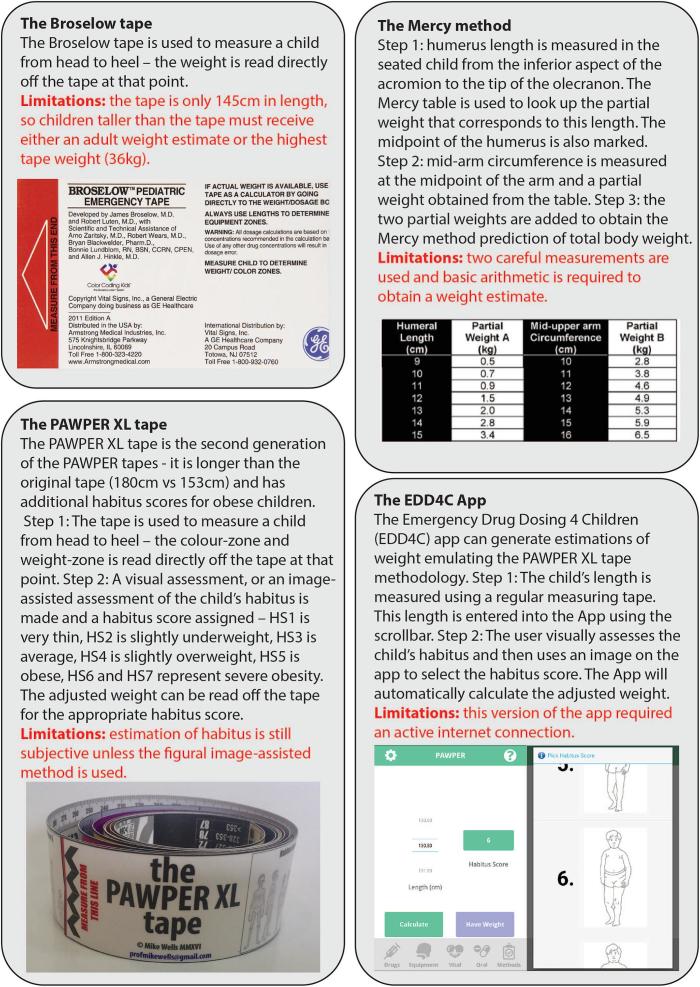
Four weight estimation methods were tested in this study (Fig. 1): the PAWPER XL tape [2], [17], the Broselow tape 2011 edition A, the Mercy method [15] and the Emergency Drug Dosing 4 Children mobile phone App.
Fig. 1.
Details of the weight-estimation systems used in this study. Descriptions of how the methods are used are provided. Abbreviations: EDD4C app (emergency drug dosing for children mobile application).
The performance of weight estimation of each system was evaluated for accuracy, bias and precision. Accuracy was represented by the percentage of estimations falling within 10% and 20% of actual weight (PW10 and PW20). The PW10 is a method of quantifying the overall accuracy of a weight estimation system and takes both bias and precision into account. An acceptable accuracy for a weight estimation system has been suggested to be a PW10 >70% [18]. The PW20 provides a measure of overall accuracy, but also provides an indication of the critical errors produced by a weight estimation system: those with a >20% error. An acceptable critical error rate for a weight estimation system has been suggested to be 5% (PW20 >95%) [19]. The bias was represented by the mean percentage error of estimations and the precision by the 95% limits of agreement of the percentage error; these were the Bland & Altman limits of agreement i.e., MPE ± 1.96 × standard deviation of percentage error. We determined the weight estimation accuracy achieved by each individual participant and calculated the accuracy data for the subgroups of best-performing and worst-performing participants. We then compared the systems based on overall accuracy (PW10 data) using the McNemar test for paired non-parametric data; we calculated odds ratios for the significant outcomes. We used the Mann-Whitney test to make comparisons between the times taken to complete the estimations.
In order to identify the effects of patient characteristics on the accuracy of weight estimation, we performed a multiple logistic regression analysis for each of the systems, with weight estimation accuracy, defined as estimates within 10% of actual weight, as the dependent variable and patient length, habitus score, position and cooperation as the independent variables. We quantified the effect sizes of statistically significant findings using crude and adjusted odds ratios. We used the R2 to measure how much variability was explained by each model.
The primary outcome measure was weight estimation accuracy (based on PW10 data). The secondary outcome measures were the time taken to complete weight estimation and feedback from the participants on the use of the systems.
A p < 0.05 was regarded significant for all statistical tests, including the predictors in the multivariate models. Statistical analysis was performed using Stata (StataCorp, 2015, Stata Statistical Software: Release 14, College Station, TX: StataCorp LP).
Results
Thirty-two participants were enrolled in the study with a variety of demographics (Table 1).
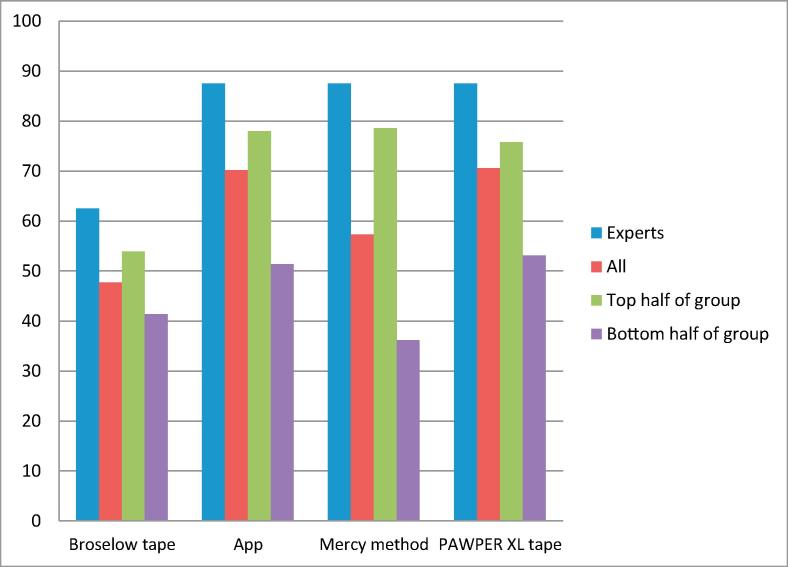
This study determined the accuracy of weight estimation for each method, the experts’ control data, and the times taken for weight estimation (Table 2). The PAWPER XL tape and the App had the highest accuracy, least bias, and best precision. The PAWPER XL tape and the App also had the lowest critical error rate, 4.8% and 5.0% respectively, and the Broselow tape the highest at 34.4%. This pattern was repeated with the experts’ weight estimation control data (Fig. 2).
Table 2.
Performance of the four weight estimation systems tested in the simulations.
| Weight-estimation accuracy data of participants | ||||
|---|---|---|---|---|
| Participants | Broselow tape | EDD4C app | Mercy method | PAWPER XL tape |
| n | 256 | 235 | 253 | 256 |
| Mean percentage error (%) | −10.0 | 2.8 | −6.8 | −1.8 |
| Limits of agreement (%) | −50.8, 30.8 | −25.4, 31.1 | −35.2, 21.5 | −23.6, 19.9 |
| PW10 (%) | 47.7ed,mm,pt | 68.1bt | 57.3bt,pt | 73.0bt,mm |
| PW20 (%) | 65.6ed,mm,pt | 95.0bt | 85.8bt,pt | 95.2bt,mm |
| Weight-estimation accuracy data of experts | ||||
| Experts | Broselow tape | EDD4C app | Mercy method | PAWPER XL tape |
| n | 24 | 24 | 24 | 24 |
| Mean percentage error (%) | −10.0 | 3.3 | −6.0 | −1.5 |
| Limits of agreement (%) | −50.8, 30.8 | −7.0, 13.5 | −18.4, 6.5 | −15.0, 12.0 |
| PW10 | 50.1ed,mm,pt | 87.5bt | 87.5bt | 87.5bt |
| PW20 | 62.6ed,mm,pt | 100bt | 95.8bt | 100bt |
| Stratified weight-estimation accuracy of participants – accuracy (PW10) data | ||||
| Participants | Broselow tape | EDD4C app | Mercy method | PAWPER XL tape |
| n | 32 | 32 | 32 | 32 |
| Top 10 (best in group) (%) | 56.4ed,mm,pt | 84.0bt | 82.3bt | 87.5bt |
| Bottom 10 (worst in group) (%) | 36.3ed,pt | 51.4bt,mm | 24.1ed,pt | 57.5bt,mm |
| Top half of group (%) | 53.9ed,mm,pt | 80.4bt | 78.6bt | 83.6bt |
| Bottom half of group (%) | 41.4ed,pt | 55.6bt,mm | 36.2ed,pt | 62.5bt,mm |
| Time to complete weight estimation | ||||
| Participants | Broselow tape | EDD4C app | Mercy method | PAWPER XL tape |
| n | 256 | 235 | 253 | 256 |
| Time (s)–median (LQ, UQ) | 20 (14, 26)ed,mm,pt | 44 (33, 60)bt,pt | 44 (37, 54)bt,pt | 23.5 (18, 29)bt,ed,mm |
| Time <30 s – n (%) | 218 (85.2)ed,mm | 43 (17.0)bt,mm,pt | 23 (9.0)bt,ed,pt | 203 (79.3)ed,mm |
| Time >60 s – n (%) | 2 (0.8)ed,mm | 66 (25.7)bt,pt | 36 (14.1)bt,pt | 2 (0.8)ed,mm |
bt, Broselow tape; ed, EDD4C app; mm, Mercy method; pt, PAWPER XL tape.
Fig. 2.
Accuracy of weight estimation of each of the systems. The histogram shows the weight estimation accuracy for each weight estimation system for the pooled participants, the experts, the best 16 participants and the worst 16 participants (top and bottom half of the group, respectively). Percentages of weight estimates within 10% of actual weight (PW10) are shown.
The data for the weight estimation accuracy by the participants and the expert “controls” were calculated with the groups of best and worst performers in each system (Table 2). A negative figure in the mean percentage error and percentage error limits of agreement indicates an underestimation of weight (Table 2). Statistical tests used for the comparisons were the McNemar test for paired outcome comparisons and the Mann-Whitney test for paired time-data. The superscripts designate significant differences in the comparisons between the weight estimation systems; for example, in the Broselow tape column, the PW10 data “47.7ed,mm,pt” indicates a significant difference in the comparisons between the PW10 of the Broselow tapebt, the EDD4C apped, the Mercy methodmm and the PAWPER XL tapept (Table 2). Statistical testing was not performed on the mean percentage error (MPE) data as statistically significant differences in bias provided limited information.
There was substantial variation between individual participants in the accuracy of weight estimation achieved. The highest-performers amongst the participants achieved exceptionally good accuracy with the Mercy method, the App and the PAWPER XL tape, achieving PW10s of 78.6%, 80.4% and 83.6% respectively. The worst-performers were least accurate with the Mercy method when compared with the App and the PAWPER XL tape, achieving PW10s 36.2%, 55.6% and 62.5% respectively.
The Broselow tape and PAWPER XL tape had significantly faster estimation times than the App and Mercy method, with about 80% of estimations completed within 30 s. Even with the slower methods, weight estimation was completed in less than one minute in more than 75% of scenarios.
Multiple regression analysis were also performed (Table 3). The accuracy of the PAWPER XL tape was unaffected by the children’s length, habitus, position or degree of cooperation, the Mercy method and the App were slightly affected, but the Broselow tape was significantly impacted by these factors. For the Broselow tape, habitus deviations from the average were associated with the largest impact on accuracy. Position and cooperation had no effect on the time to obtain weight estimates for any system, but taller and overweight children had slightly slower weight estimation times with the App.
Table 3.
The results of the multiple regression analyses for weight estimation accuracy and time to obtain a weight estimation.
| Accuracy of weight estimation | |||||||
|---|---|---|---|---|---|---|---|
| Broselow tape | Mercy method | App | PAWPER XL tape | ||||
| Position | Crude OR Adjusted OR Crude R2 Adjusted R2 |
6.5 (3.0, 10) 5.9 (1.9, 26) 0.21 0.65 |
Crude OR Adjusted OR Crude R2 Adjusted R2 |
0.4 (0.4, 0.5) 0.6 (0.5, 0.7) 0.35 0.40 |
Crude OR Adjusted OR Crude R2 Adjusted R2 |
2.5 (1.4, 4.4) 3.8 (1.4, 10) 0.25 0.32 |
NS |
| Interpretation: BT more accurate in supine children | Interpretation: MM more accurate in sitting children | Interpretation: MM more accurate in supine children | |||||
| Cooperation | Crude OR Adjusted OR Crude R2 Adjusted R2 |
4.9 (2.9, 8.3) 1.6 (1.2, 2.7) 0.26 0.65 |
Crude OR Adjusted OR Crude R2 Adjusted R2 |
2.7 (2.2, 3.2) 3.6 (1.6, 8.2) 0.25 0.40 |
NS | NS | |
| Interpretation: BT more accurate in cooperative children | Interpretation: MM more accurate in cooperative children | ||||||
| Length | Crude OR Adjusted OR Crude R2 Adjusted R2 |
5.8 (4.0, 7.6) 4.8 (3.2, 7.4) 0.19 0.65 |
Crude OR Adjusted OR Crude R2 Adjusted R2 |
1.1 (1.0, 1.3) 1.2 (1.0, 1.4) 0.15 0.40 |
Crude OR Adjusted OR Crude R2 Adjusted R2 |
1.1 (1.0, 1.8) 1.3 (1.1, 2.5) 0.14 0.32 |
NS |
| Interpretation: BT less accurate in taller children | Interpretation: MM less accurate in taller children | Interpretation: EDD4C less accurate in taller children | |||||
| Habitus | Crude OR Adjusted OR Crude R2 Adjusted R2 |
28 (19, 37) 18 (14, 22) 0.46 0.65 |
Crude OR Adjusted OR Crude R2 Adjusted R2 |
1.1 (1.0, 1.4) 1.1 (1.0, 1.3) 0.10 0.40 |
Crude OR Adjusted OR Crude R2 Adjusted R2 |
1.4 (1.1, 1.8) 1.4 (1.0, 1.8) 0.12 0.32 |
NS |
| Interpretation: BT less accurate in underweight, overweight and obese children | Interpretation: MM less accurate in obese children | Interpretation: BT less accurate in underweight children | |||||
| Time to obtain weight estimate | |||||
| Broselow tape | Mercy method | App | PAWPER XL tape | ||
| Position | NS | NS | NS | NS | |
| Cooperation | NS | NS | NS | NS | |
| Length | NS | NS | Crude OR Adjusted OR Crude R2 Adjusted R2 |
1.2 (1.1, 1.3) 1.3 (1.1, 1.5) 0.23 0.19 |
NS |
| Interpretation: EDD4C slower in taller children | |||||
| Habitus | NS | NS | Crude OR Adjusted OR Crude R2 Adjusted R2 |
(1.0, 1.3) (1.1, 1.4) 0.17 0.19 |
NS |
OR, odds ratios; PTXL, PAWPER XL tape; EDD4C; Emergency Drug Dosing 4 Children mobile application; MM, Mercy method; BT, Broselow tape.
Discussion
This is the first study to have evaluated the Mercy method and the PAWPER XL tape in a simulated resuscitation setting. It is also the first to have evaluated a weight-estimation App and the first study to have evaluated the effects of suboptimal patient positions and behaviour on weight estimation accuracy.
When considering the accuracy of the systems, the Broselow tape was not ideal according to the results of this study. Its performance was similar to that reported in many previous articles with PW10s between 45% and 60%, however its accuracy was better than its performance in very underweight populations with PW10s between 10% and 30% [20], [21], [22], [23]. Both its poor accuracy and high critical error rate continue to raise doubts about its safety when used to guide drug dose calculations in many populations. The Mercy method has previously been shown to be very accurate in populations from both high-income and low- and middle-income countries across the world with PW10 70–80% [2], [24], [25], [26], [27], [28]. In this study, its accuracy was substantially lower with a PW10 of 57%, but it was comparable to the accuracy reported when the method was used by non-experts with PW10 46–53% [11], [24]. The PAWPER XL tape performed very well in this study with a PW10 73.0%, similar to the results from the only other previous study on the PAWPER XL tape [17]. The App achieved a moderate degree of weight estimation accuracy, but was slightly less accurate than the PAWPER XL tape-system on which it is based. This data was encouraging, however, and supports the value of further research into weight estimating point-of-care mobile phone apps, in addition to the tape-based PAWPER XL system. The use of an App that could provide an accurate estimate of weight as well as comprehensive information on drug dosing would be enormously useful.
The accuracy data from the experts illustrated the excellent levels of accuracy the two-dimensional weight estimation systems could achieve in an ideal scenario. The difference in accuracy between the experts and the participants was a strong indication that patient-induced errors, such as from patient positioning or lack of cooperation, or user-induced errors impact weight estimation accuracy, more than an inaccuracy of the methodology itself [11], [29].
The effects of length and habitus were important for the Broselow tape: the tape was significantly and substantially less accurate in underweight and overweight children, a major disadvantage common to all length-based weight estimation systems [9], [30]. It is also the reason that the Broselow tape has been repeatedly shown to be inaccurate in populations with a high prevalence of underweight or obese children, or both [31]. Length plus a measure of habitus is required for an accurate weight estimation [32]. Taller children also had a reduced accuracy of weight estimation with the Broselow tape. Since the length limitations of the tape are quite restrictive at 145 cm, children as young as nine or ten years of age may not receive accurate weight estimations [33]. While children “too tall for the tape” are often excluded during research studies, this is not possible in the real world. In this study, two children were too tall for the tape and had substantial underestimation of their weight, despite the participants following the manufacturers’ guidelines for this scenario to use an adult weight.
Length and habitus had a far smaller impact on the accuracy of the Mercy method and the App, and none at all on the PAWPER XL tape, because the two-dimensional systems take both length and habitus into account in the estimation methodology [2], [15]. The observed associations were unlikely to significantly impact on overall accuracy. Previous studies on the original PAWPER tape showed a high accuracy in populations with a low prevalence of obesity with a PW10 >80%, but a lower accuracy in populations with a high incidence of obesity with a PW10 60–70% [2], [24], [34], [35]. The lack of association with habitus in this study provided preliminary evidence that the PAWPER XL tape may have addressed this problem.
Suboptimal patient positioning and lack of patient cooperation negatively influenced the performance of the Broselow tape considerably, which was far more evident than in the other weight estimation systems. The tentative explanation for this is that the width of the tape at 95 mm may have made it cumbersome and difficult to manipulate in sitting or uncooperative children.
There was a similar, although smaller, association with the Mercy method: it was slightly less accurate in uncooperative children, but it was more accurate in sitting children, while the opposite was true for the App. Since the best performers amongst the participants demonstrated little difference in accuracy to that of the experts using the systems under ideal circumstances, the net adverse effects of position and cooperation were likely to be a decrease in accuracy of only a few percentage points at most.
There was no association between patient position or behaviour and the performance of the PAWPER XL tape. The negligible difference between the best participants’ accuracy and the experts’ accuracy under ideal circumstances confirmed the resilience of this method in this respect. The smaller width of the tape of 40 mm, when compared with the Broselow tape, may have made it easier to manipulate in uncooperative or sitting patients.
When considering the effects of human factor errors, the results achieved by the experts proved that it was possible to achieve a high level of weight estimation accuracy in these children with the Mercy method, the PAWPER XL tape, and the App. Furthermore, the subgroup of best-performers amongst the participants proved that it was possible to achieve a high degree of accuracy despite the adverse patient factors. Human error factors were therefore far more significant and important: it is likely that training, experience and inherent skill played the major role in determining the final accuracy of weight estimation. This has been shown previously in a human factor errors analysis on the Mercy method, which showed very poor accuracies in 80 minimally-trained users [11]. In this study, the largest disparity between the accuracy of the best-performing and worst-performing participants was seen with the Mercy method, which suggests that this more complex technique was the most vulnerable to human error. This gap, while still present, was not as marked with PAWPER XL tape and the App. Differences in accuracy between experienced and inexperienced users have been shown in other studies with the PAWPER tape, although even brief formal training sessions with users eliminated these errors [2], [35], [36].
Even the Broselow tape, which appears to be simple to use, has been found to be dependent on training: errors are extremely common unless users have been formally trained with the tape [10], [37].
The very positive aspect of these findings is that appropriate training is likely to enable high levels of accuracy to be consistently reproduced in real-life practice with the PAWPER XL tape and the Mercy method [38]. Proper training in weight estimation for use in emergencies should not be ignored and should probably be included as part of paediatric advanced life support courses as well as routine paediatric simulation training.
The Broselow tape and the PAWPER XL tape were both successful at providing a rapid estimate of weight. While this finding was expected for the Broselow tape, in the case of the PAWPER XL tape, it confirmed that habitus assessment was a quick process and therefore probably added minimal cognitive stress. The Mercy method, however, was significantly slower. The multiple measurements and calculations required were the cause of this delay. The use of the App was relatively slow because it was hindered by a scrollbar data-entry system that was very time-consuming to use. Despite the relative slowness of these two systems, however, they did not take longer than 60 s to complete. Although there is no published benchmark for weight estimation times, these systems were all satisfactorily efficient.
One of the most interesting findings of the study was that many of the participants realised that they required more training and practice in weight estimation than they had expected. Although they had considered themselves to be well-trained, they discovered during the simulations that they did not have enough practice.
The Mercy method was found to be complex and too difficult to use in an emergency but, despite its limitations, the App was well-liked. The PAWPER XL tape was regarded by most participants as the most appropriate of the methods for clinical emergency usage.
There were technical problems with fluctuating Wi-Fi access for the Emergency Drug Dosing 4 Children App within the hospital precincts on the day of the study. This slowed its functioning and may have skewed data against the App.
Performing sequential weight estimations could potentially have introduced bias, but this was addressed by rotating the order of estimations. A previous study using a similar protocol, however, did not demonstrate any bias from sequential weight estimations [11].
We did not evaluate the participants’ previous experience with weight estimation methods. Since some methods are commonly used in South Africa, such as the Broselow tape, these methods may have been more familiar to the participants.
The sample of children in this study was skewed to an older age-group, so the weight estimation accuracy findings might not be generalizable to a younger population. The findings with regards to patient-induced errors and user-induced errors might not remain true and relevant in all age-groups, however. Most weight estimation systems are more accurate in younger children, which may also have biased the results towards those systems, such as the PAWPER XL tape, which are accurate across a broad range of age-groups.
The Broselow tape performed poorly in this study, as in many others before, and it is difficult to see an ongoing future role for the tape when compared to other, newer weight estimation systems. It was the method most affected by suboptimal patient positioning and behaviour. The accuracy of the Mercy method was only slightly impacted by adverse patient positioning and behaviour, but was the system most affected by human factor errors. The App achieved reasonable accuracy, but was the slowest of the methods evaluated because of design limitations. It was only slightly affected by patient factors, but was impacted by differences in ability between participants. The App was popular with the participants but needs further research. The PAWPER XL tape was completely unaffected by patient factors and was the most resilient and least vulnerable to human factor errors, although these still had a significant impact on its overall performance.
While patient factors frequently cannot be safely changed to improve weight estimation accuracy, human factor errors can be reduced through training. Paediatric weight estimation training should become an integral part of resuscitation simulation teaching.
Conflicts of interest
MW designed and created the PAWPER tape that is reviewed in this manuscript. MW is also an editor of this journal. He was, however, not involved in the peer review, decision or editing process of this paper. There are no further conflicts of interest.
Authors’ contributions
MW conceived the original idea. MW and LG designed the scenarios and collected the data. MW carried out the analysis of data. MW drafted the manuscript; LG and AB revised it. MW, LG and AB approved the final version that was submitted.
Footnotes
Peer review under responsibility of African Federation for Emergency Medicine.
Supplementary data associated with this article can be found, in the online version, at https://doi.org/10.1016/j.afjem.2017.12.003.
Appendix A. Supplementary data
Representative responses and key themes obtained from the post-participation survey. The number of multiple similar comments is indicated in parentheses. The approval rating of each method is also shown.
References
- 1.Cattermole G.N., Graham C.A., Rainer T.H. Paediatric weight estimation. Emerg Med J. 2012;29(1):82–83. doi: 10.1136/emermed-2011-200690. [DOI] [PubMed] [Google Scholar]
- 2.Wells M., Coovadia A., Kramer E., Goldstein L. The PAWPER tape: a new concept tape-based device that increases the accuracy of weight estimation in children through the inclusion of a modifier based on body habitus. Resuscitation. 2013;84(2):227–232. doi: 10.1016/j.resuscitation.2012.05.028. [DOI] [PubMed] [Google Scholar]
- 3.Srinivasan V., Nadkarni V.M., Helfaer M.A., Carey S.M., Berg R.A. American Heart Association National Registry of Cardiopulmonary Resuscitation I. Childhood obesity and survival after in-hospital pediatric cardiopulmonary resuscitation. Pediatrics. 2010;125(3):e481–e488. doi: 10.1542/peds.2009-1324. [DOI] [PubMed] [Google Scholar]
- 4.Luscombe M. “Kid's aren't what they used to be”: a study of paediatric patients' weights and their relationship to current weight estimation formulae. Br J Anaesth. 2005;95(4):578. [Google Scholar]
- 5.Lerner C., Gaca A.M., Frush D.P., Hohenhaus S., Ancarana A., Seelinger T.A. Enhancing pediatric safety: assessing and improving resident competency in life-threatening events with a computer-based interactive resuscitation tool. Pediatr Radiol. 2009;39(7):703–709. doi: 10.1007/s00247-009-1265-y. [DOI] [PubMed] [Google Scholar]
- 6.Luten R., Wears R.L., Broselow J., Croskerry P., Joseph M.M., Frush K. Managing the unique size-related issues of pediatric resuscitation: reducing cognitive load with resuscitation aids. Acad Emerg Med. 2002;9(8):840–847. doi: 10.1111/j.1553-2712.2002.tb02175.x. [DOI] [PubMed] [Google Scholar]
- 7.Porter E., Barcega B., Kim T.Y. Analysis of medication errors in simulated pediatric resuscitation by residents. West J Emerg Med. 2014;15(4):486–490. doi: 10.5811/westjem.2014.2.17922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kaufmann J., Laschat M., Wappler F. Medication errors in pediatric emergencies: a systematic analysis. Deutsches Ärzteblatt International. 2012;109(38):609–616. doi: 10.3238/arztebl.2012.0609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wells M., Goldstein L., Bentley A. It is time to abandon age-based emergency weight estimation in children! A failed validation of 20 different age-based formulas. Resuscitation. 2017;116(7):73–83. doi: 10.1016/j.resuscitation.2017.05.018. [DOI] [PubMed] [Google Scholar]
- 10.Hohenhaus S.M., Frush K.S. Pediatric patient safety: common problems in the use of resuscitative aids for simplifying pediatric emergency care. J Emerg Nurs. 2004;30(1):49–51. doi: 10.1016/j.jen.2003.11.011. [DOI] [PubMed] [Google Scholar]
- 11.Abdel-Rahman A., Jacobsen R., Watts J., Doyle S., O’Malley D., Hefner T. Comparative performance of pediatric weight estimation techniques: a human factor errors analysis. Pediatr Emerg Care. 2015 doi: 10.1097/PEC.0000000000000543. [DOI] [PubMed] [Google Scholar]
- 12.Hohenhaus S.M. Assessing competency: the Broselow-Luten resuscitation tape. J Emerg Nurs. 2002;28(1):70–72. doi: 10.1067/men.2002.121815. [DOI] [PubMed] [Google Scholar]
- 13.Shah A.N., Frush K., Luo X., Wears R.L. Effect of an intervention standardization system on pediatric dosing and equipment size determination: a crossover trial involving simulated resuscitation events. Arch Pediatr Adolesc Med. 2003;157(3):229–236. doi: 10.1001/archpedi.157.3.229. [DOI] [PubMed] [Google Scholar]
- 14.Lammers R., Willoughby-Byrwa M., Fales W. Medication errors in prehospital management of simulated pediatric anaphylaxis. Prehosp Emerg Care. 2014;18(2):295–304. doi: 10.3109/10903127.2013.856501. [DOI] [PubMed] [Google Scholar]
- 15.Abdel-Rahman S.M., Ridge A.L. An improved pediatric weight estimation strategy. Open Med Devices J. 2012;4:87–97. [Google Scholar]
- 16.Emergency drug dosing 4 children [Internet]. 2014. Available from: https://play.google.com/store/apps/details?id=emergencyapp.emergencyapp.
- 17.Wells M., Goldstein L., Bentley A. A validation study of the PAWPER XL tape: accurate estimation of both total and ideal body weight in children up to 16 years of age. Trauma Emerg Care. 2017;2(4):1–8. [Google Scholar]
- 18.Wells M., Goldstein L., Bentley A. High-tech adjuncts to emergency weight estimation: Point-of-care ultrasound and point-of-care bioelectrical impedance measurements can increase the accuracy of length-based weight estimation in children. Trauma Emerg Care. 2017;2(3):1–8. [Google Scholar]
- 19.Stewart D. University of Sydney; 2009. Accuracy of the Broselow tape for estimating paediatric weight in two Australian Emergency Departments. [Google Scholar]
- 20.Graves L., Chayen G., Peat J., O'Leary F. A comparison of actual to estimated weights in Australian children attending a tertiary children’s hospital, using the original and updated APLS, Luscombe and Owens, Best Guess formulae and the Broselow tape. Resuscitation. 2014;85(3):392–396. doi: 10.1016/j.resuscitation.2013.11.024. [DOI] [PubMed] [Google Scholar]
- 21.Suh D., Kwak Y., Kim D., Jeong J. Estimating weights using the Broselow tape in Korea: comparison of old and new versions of the Broselow tape use. Ann Emerg Med. 2013;62(4):S109. [Google Scholar]
- 22.Geduld H., Hodkinson P.W., Wallis L.A. Validation of weight estimation by age and length based methods in the Western Cape, South Africa population. Emerg Med J. 2011;28(10):856–860. doi: 10.1136/emj.2010.098640. [DOI] [PubMed] [Google Scholar]
- 23.Clark M.C., Lewis R.J., Fleischman R.J., Ogunniyi A.A., Patel D.S., Donaldson R.I. Accuracy of the Broselow Tape in South Sudan, “The Hungriest Place on Earth”. Acad Emerg Med. 2016;23(1):21–28. doi: 10.1111/acem.12854. [DOI] [PubMed] [Google Scholar]
- 24.Georgoulas V., Wells M. The PAWPER tape and the Mercy Method outperform other methods of weight estimation in children in South Africa. S Afr Med J. 2016;106(9):933–939. doi: 10.7196/SAMJ.2016.v106i9.10572. [DOI] [PubMed] [Google Scholar]
- 25.Batmanabane G., Kumar Jena P., Dikshit R., Abdel-Rahman S.M. Using the Mercy Method for weight estimation in Indian children. Global Pediatr Health. 2015:1–7. doi: 10.1177/2333794X14566625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dicko A., Alhousseini M.L., Sidibé B., Traoré M., Abdel-Rahman S.M. Evaluation of the Mercy weight estimation method in Ouelessebougou, Mali. BMC Public Health. 2014;14:270. doi: 10.1186/1471-2458-14-270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Abdel-Rahman S.M., Paul I.M., James L.P., Lewandowski A. Evaluation of the Mercy TAPE: performance against the standard for pediatric weight estimation. Ann Emerg Med. 2013;62(4) doi: 10.1016/j.annemergmed.2013.02.021. 332–339.e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Abdel-Rahman S.M., Ahlers N., Holmes A., Wright K., Harris A., Weigel J. Validation of an improved pediatric weight estimation strategy. J Pediatr Pharmacol Ther. 2013;18(2):112–121. doi: 10.5863/1551-6776-18.2.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hunt E.A., Hohenhaus S.M., Luo X., Frush K.S. Simulation of pediatric trauma stabilization in 35 North Carolina emergency departments: identification of targets for performance improvement. Pediatrics. 2006;117(3):641–648. doi: 10.1542/peds.2004-2702. [DOI] [PubMed] [Google Scholar]
- 30.Yamamoto L.G., Inaba A.S., Young L.L., Anderson K.M. Improving length-based weight estimates by adding a body habitus (obesity) icon. Am J Emerg Med. 2009;27(7):810–815. doi: 10.1016/j.ajem.2008.06.023. [DOI] [PubMed] [Google Scholar]
- 31.Young K.D., Korotzer N.C. Weight estimation methods in children: a systematic review. Ann Emerg Med. 2016;68(4) doi: 10.1016/j.annemergmed.2016.02.043. 441–451.e10. [DOI] [PubMed] [Google Scholar]
- 32.Losek J.D., Garland J., Nelson D.B. Body habitus + height = accurate weight estimate. Ann Emerg Med. 1989;18(6):709. doi: 10.1016/s0196-0644(89)80539-6. [DOI] [PubMed] [Google Scholar]
- 33.Cattermole G.N., Leung P.Y., Graham C.A., Rainer T.H. Too tall for the tape: the weight of schoolchildren who do not fit the Broselow tape. Emerg Med J. 2013 doi: 10.1136/emermed-2012-202325. [epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 34.Chavez H., Peterson R., Lo K., Arel M. Weight estimation in an inner city Pediatric Emergency Department: the effect of obesity. Am J Emerg Med. 2015;33(10):1364–1367. doi: 10.1016/j.ajem.2015.07.040. [DOI] [PubMed] [Google Scholar]
- 35.Garcia C.M., Meltzer J.A., Chan K.N., Cunningham S.J. A validation study of the PAWPER (Pediatric Advanced Weight Prediction in the Emergency Room) tape-a new weight estimation tool. J Pediatr. 2015;167(1) doi: 10.1016/j.jpeds.2015.04.006. 173–177.e1. [DOI] [PubMed] [Google Scholar]
- 36.O'Leary F., John-Denny B., McGarvey K., Hann A., Pegiazoglou I., Peat J. Estimating the weight of ethnically diverse children attending an Australian emergency department: a prospective, blinded, comparison of age-based and length-based tools including Mercy, PAWPER and Broselow. Arch Dis Child. 2017;102(1):46–52. doi: 10.1136/archdischild-2016-310917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hohenhaus S.M., Frush K.S. Pediatric patient safety in resuscitation simulations: lessons learned from studying clinician behavior. Pediatr Emerg Care. 2005;21(1):71–75. doi: 10.1097/01.pec.0000150992.49722.60. [DOI] [PubMed] [Google Scholar]
- 38.Frush K., Hohenhaus S., Luo X., Gerardi M., Wiebe R.A. Evaluation of a Web-based education program on reducing medication dosing error: a multicenter, randomized controlled trial. Pediatr Emerg Care. 2006;22(1):62–70. doi: 10.1097/01.pec.0000195760.97199.7e. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Representative responses and key themes obtained from the post-participation survey. The number of multiple similar comments is indicated in parentheses. The approval rating of each method is also shown.