Abstract
Introduction
The choice of weight estimation method to use during prehospital paediatric emergency care is important because it needs to be both accurate and easy to use. Accuracy is important to ensure optimum drug dosing while ease-of-use is important to minimise user errors and the cognitive load experienced by healthcare providers. Little is known about which weight estimation systems are used in the prehospital environment anywhere in the world. This knowledge is important because if the use of inappropriate weight estimation practices is identified, it could be remedied through education and institutional policies.
Methods
This was a prospective questionnaire study conducted in Johannesburg, South Africa, which obtained information on the knowledge, attitude and practice of weight estimation amongst advanced life support (ALS) paramedics.
Results
Forty participants were enrolled, from both the public and private sectors. The participants’ preferred method of weight estimation was visual estimation (7/40; 18%), age-based formulas (16/40; 40%), parental estimation (3/40; 8%), the Broselow tape (2/40; 5%) and the PAWPER tape (11/40; 28%). No participant was familiar with or used the Mercy method. All participants were very confident in the accuracy of their selected system.
Discussion
The knowledge and understanding of weight estimation systems by many advanced life support paramedics was poor and the use of inappropriate weight estimation systems was common. Further education and intervention is needed in order to change the sub-optimal weight estimation practices of ALS paramedics in Johannesburg.
Keywords: Weight estimation, Paediatrics, PAWPER tape, Broselow tape
African relevance
-
•
Weight estimation is as important in Africa as elsewhere in the world.
-
•
Prehospital systems in Africa should follow resource-appropriate, evidence-based guidelines.
-
•
The absence of reliable parental weights in resource-limited environments is problematic.
-
•
The best weight estimation systems are not expensive, but need to be disseminated.
Introduction
The nature of the prehospital emergency care environment and the presentation of acute emergency cases is such that healthcare providers have to rely on a method of estimating children’s weight in order to calculate emergency drug doses. Accurate weight estimate is important for calculating drug dosages, as inaccurate doses can be harmful [1].
The weight estimation systems most commonly researched and taught (particularly in paediatric advanced life support short courses) are the age-based formulas and the Broselow tape [2]. Age-based formulas, together with healthcare provider guesses of weight have been found to be amongst the least accurate of all the weight estimation systems, however, while the Broselow tape has also been shown to lack sufficient accuracy both in high-income and low- and middle-income countries [3]. The most accurate systems currently described are the two-dimensional length- and habitus-based systems (such as the Mercy method and the PAWPER tape) and parental estimates of weight [3].
While it has been reasonably well established which weight estimation systems are the most accurate, there is very limited evidence on which weight estimation systems are actually being used in the prehospital environment. This information is important, as the failure to use the most appropriate weight estimation methodology could potentially affect patient outcomes adversely. This information would also allow decision-makers to create appropriate policies for weight estimation practices and education and allow intervention into current practices, if required.
The aim of our study was to investigate and describe the current paediatric weight estimation practices of ALS paramedics in the emergency medical care setting within Johannesburg, South Africa.
Methods
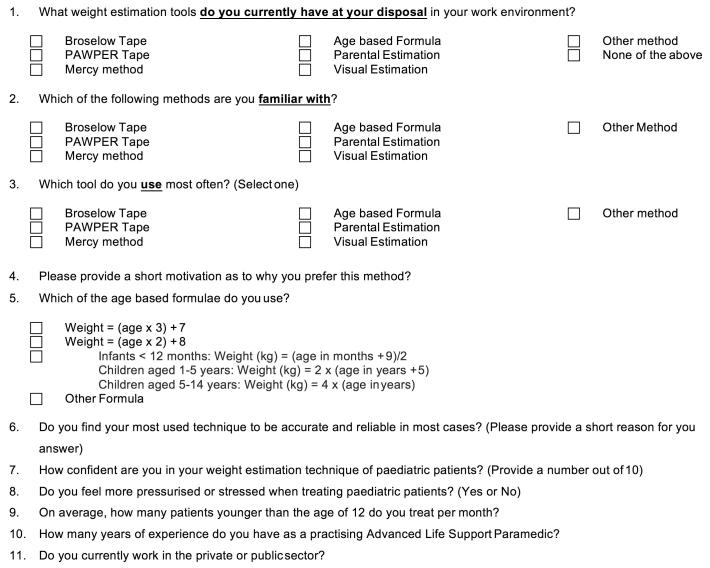
This was a qualitative questionnaire study. The questionnaire (Fig. 1) was designed to obtain basic information about the participants’ knowledge, attitude and practice with regards to emergency paediatric weight estimation. Full-time advanced life support (ALS) paramedics practising in Johannesburg, from either the private or the public sector, were invited to participate.
Fig. 1.
The questionnaire used in this study.
At the time of the survey there were an estimated 80–100 practising ALS paramedics in the Johannesburg metropolitan area. A sample size of 40 participants was therefore selected for the pilot study to provide a ±10% margin of error with a 95% confidence level for the survey results. Ethical approval was granted from the University of Johannesburg Research Ethics Committee (REC 01-53-2016). Written informed consent was obtained from all participants.
The study took place during the second quarter of 2016. One of the researchers (LB) visited bases across Johannesburg and invited ALS paramedics to participate. Those that volunteered completed anonymous hard copies of the questionnaire. Responses were analysed and presented using basic descriptive statistics.
Results
Forty ALS paramedics participated in the survey. The details of the participants in terms of their sector of employment, their experience, the number of children they see per month and their self-perceived stress levels during paediatric emergencies is shown in Table 1. Nearly three-quarters of the participants (29/40; 72.5%) had more than two years’ postgraduate experience, so could be regarded as moderately experienced.
Table 1.
Demographic information from participants.
| Question | Outcome |
|---|---|
| Private sector, n (%) | 25/40 (62.5) |
| Experience as practising ALS paramedic in years, median (IQR) | 3.0 (1.9–5.3) |
| Number of children treated per month, median (IQR) | 4.0 (2.8–6.3) |
| Stress level high when treating children, n (%) | 27/40 (67.5) |
ALS, advanced life support; IQR, interquartile range.
A description of the weight estimation systems that the participants were familiar with, the systems they had available to them and the systems they used in practice are shown in Table 2. There was no significant difference in these outcomes between the private- and public-sector services. The reasons provided by the participants for their choice of system are also shown.
Table 2.
Participants’ knowledge and use of weight estimation systems.
| Participants familiar with method | Participants to whom method is available | Participants’ preferred method | Why do you prefer this method? | |
|---|---|---|---|---|
| Visual estimation | 8 (20%) | 40 (100%) | 7 (18%) | It is the quickest method; Normally parents do not know their children’s current weight; It is what I have available |
| Parental estimation | 11 (28%) | 40 (100%) | 3 (8%) | Parents should be the most accurate; Parents generally know the weight of their children |
| Age-based formulas | 37 (93%) | 40 (100%) | 16 (40%) | It is quickest, has been quite accurate to date; It works the fastest and is closest to the actual weight; In an emergency situation, it is the easiest to perform (4); It is the most accurate; It is what I am used to |
| PAWPER tape | 27 (68%) | 22 (55%) | 11 (28%) | It is easy to use and prevents confusion. I am bad at maths It is the most accurate and simple method (3); It is most accurate as it has been based on a South African population and I use it every day (3); Quick, accurate reference, drug calculations easily accessible (2); I have it readily available; Two-dimensional weight estimation method is the most accurate |
| Broselow tape | 15 (38%) | 7 (18%) | 2 (5%) | It is available and the quickest to use; It is the most accurate to estimate weight; |
| Mercy method | 0 | 0 | 0 | – |
Discussion
According to our search on Medline and Scopus, this is the first published study to have described which paediatric weight estimation systems are actually used in clinical practice in a particular prehospital environment, anywhere in the world.
The study population was made up of a group of moderately experienced ALS paramedics, representing both the private and public sector in Johannesburg. The small numbers of children treated were potentially one of the reasons that the majority of participants reported increased stress levels when dealing with paediatric emergencies. The low numbers of paediatric emergencies and the stress of these encounters amplify the need for an accurate, easy to use, appropriate weight estimation technique which would enhance rather than inhibit emergency care.
There were three major findings in this study: firstly, the level of the participants’ knowledge about the surveyed weight estimations methods was poor; secondly, the preferred methods of weight estimation used by many participants were methods known to be inaccurate and inappropriate for emergency care; and thirdly, not all ALS paramedics had access to the most accurate methods of weight estimation.
It was clear from the participants’ responses that their knowledge of weight estimation options and practices, as well as the science behind them, was relatively limited. This is probably the reason for the high level of selection of inappropriate systems for clinical usage. This is most likely because of the absence of a defined policy on and a protocol for paediatric weight estimation within the emergency care organisations. While the PAWPER tape is taught, advocated (and made available) for paediatric weight estimation in some public and private sector institutions and services, most ambulance training colleges and services still teach the use of age-based formulas. This has resulted in a delayed adoption of the newer and more accurate methods. The Mercy method is not currently taught by any institution.
More than half the surveyed ALS practitioners (58%) made use of visual estimation or age-based formulas to estimate weight, while only 36% used methods known to be accurate (parental estimates or the PAWPER tape) [3]. Visual estimation of weight (a guess by the healthcare provider) is highly inaccurate and has been discredited [4]. Weight estimation formulas are not only inaccurate in estimating weight, but the calculations required may add to already elevated levels of stress experienced by the user [5]. The ability to remember the formulas may also be impaired in emergencies, further aggravating stress levels and increasing the risk of errors [6]. It would, therefore, be considered unacceptable for an ALS practitioner to rely on this technique [7]. Few practitioners used the Broselow tape. While this tape is definitely more accurate than age-formulas and visual estimation of weight, it also is not sufficiently accurate to avoid medication errors [8]. It underestimates the weight of children in well-nourished populations to such a degree that it may result in the “under-resuscitation of children” [9]. In under-nourished populations, on the other hand, it may overestimate weight to such a degree that it causes dangerous overdoses of medication [10]. Given its high cost and low accuracy, the Broselow tape is also not an appropriate option.
There are only two studies on the accuracy of parental estimates of weight in low- and middle-income countries, both from urban areas, which showed parental estimates to be reasonably accurate [11], [12]. Parental estimates would, therefore, probably be a valid method to use in urban areas and would certainly be preferable to the use of visual estimation or age-formulas. The best choices for accurate weight estimation would have been the Mercy method and the PAWPER tape, with the PAWPER tape more suited to the prehospital environment [3]. The Mercy method was not familiar to any of the participants, although it is a low-cost method with proven accuracy across the world.
The majority of participants, other than those who favoured the PAWPER tape, provided anecdotal reasons for their choices of method, rather than a response based on evidence. The correlates with the low-level of knowledge and familiarity with weight estimation systems. It was a further indicator of the need for education amongst emergency care providers in Johannesburg. It is also possible that emergency care practitioners are not exposed to weight estimation methods such as the PAWPER tape and Mercy method in the emergency centres to which they transport patients. This is a potential intervention point for education and upskilling of ALS paramedics.
The lack of perceived availability of appropriate weight estimation methods to the ALS practitioners was also of concern. This suggests that appropriate protocols should be developed within prehospital emergency care provider organisations and that ALS providers should be educated on the availability and use of modern weight estimation systems. While both the PAWPER tape and the Mercy method are readily available in Johannesburg, the PAWPER tape is simpler, quicker and easier to use, even under the stressful conditions of a paediatric resuscitation [13]. It is also more accurate than the Mercy method [8]. The PAWPER tape would, therefore, be the method that we would recommend for prehospital use.
One author has previously suggested that length-based weight estimation might be difficult in immobilised children in the prehospital environment, but length-based weight estimation is generally regarded as the standard of care in most mature emergency medical systems [14], [15]. A recent study evaluating the weight estimation accuracy of the PAWPER tape in simulated paediatric emergencies with children in realistic clinical positions (e.g. spinal immobilisation) and with various degrees of cooperation (e.g. a convulsing child), showed no difference in accuracy between optimum and sub-optimum conditions [13]. In the same study, the Mercy method was slightly more affected by adverse conditions, but still functioned well. We can speculate that these methods are, therefore, probably well-suited to and appropriate for the prehospital environment.
The main limitation of this study was the small number of participants. Although the sample size was appropriate for the estimated number of potential participants, the results might not be generalisable. However, even at the extreme margins of error the findings of the study raise significant issues.
The current knowledge and use of paediatric weight estimation techniques by advanced life support (ALS) practitioners in Johannesburg was not of an appropriate standard. It is of concern that the proportion of participants using inaccurate methods was so high. The Mercy method and the PAWPER tape have several advantages for use in emergency medical scenarios, most notably that they are the most accurate weight estimation systems and they are inexpensive, which would allow them to be used in resource-limited settings.
We recommend that more emphasis be placed on the use of the PAWPER tape and the Mercy method in emergency medical care training institutions and emergency medical service provider organisations and also that access to these methods be improved. In choosing between the PAWPER tape and the Mercy method, we would recommend the use of the PAWPER tape because of superior accuracy and ease-of-use.
It would be useful to expand this research to other regions, rural areas and even the emergency centres of hospitals, where weight estimation practices may not be optimum. A similar follow-up study would be useful in the future, after an education program has been conducted for ALS providers in Johannesburg.
Footnotes
Peer review under responsibility of African Federation for Emergency Medicine.
Supplementary data associated with this article can be found, in the online version, at https://doi.org/10.1016/j.afjem.2018.01.003.
Appendix A. Supplementary data
References
- 1.Srinivasan V., Nadkarni V.M., Helfaer M.A., Carey S.M., Berg R.A., American Heart Association National Registry of Cardiopulmonary Resuscitation I Childhood obesity and survival after in-hospital pediatric cardiopulmonary resuscitation. Pediatrics. 2010;125(3):e481–e488. doi: 10.1542/peds.2009-1324. [DOI] [PubMed] [Google Scholar]
- 2.de Caen A.R., Berg M.D., Chameides L., Gooden C.K., Hickey R.W., Scott H.F. Part 12: Pediatric Advanced Life Support: 2015 American Heart Association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care (Reprint) Pediatrics. 2015;136(Suppl 2):S176–S195. doi: 10.1542/peds.2015-3373F. [DOI] [PubMed] [Google Scholar]
- 3.Wells M., Goldstein L., Bentley A. The accuracy of emergency weight estimation systems in children - a systematic review and meta-analysis. Int J Emerg Med. 2017;10(29):1–43. doi: 10.1186/s12245-017-0156-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Anglemyer B.L., Hernandez C., Brice J.H., Zou B. The accuracy of visual estimation of body weight in the ED. Am J Emerg Med. 2004;22(7):526–529. doi: 10.1016/j.ajem.2004.09.002. [DOI] [PubMed] [Google Scholar]
- 5.Lammers R., Byrwa M., Fales W. Root causes of errors in a simulated prehospital pediatric emergency. Acad Emerg Med. 2012;19(1):37–47. doi: 10.1111/j.1553-2712.2011.01252.x. [DOI] [PubMed] [Google Scholar]
- 6.Lancaster L. Mission impossible – minimising the terror of paediatric resuscitation for staff in the ED. Austr Emerg Nurs J. 2002;5(3):16–20. doi: 10.1016/j.aaen.2004.11.003. [DOI] [PubMed] [Google Scholar]
- 7.Wells M., Goldstein L., Bentley A. It is time to abandon age-based emergency weight estimation in children! A failed validation of 20 different age-based formulas. Resuscitation. 2017;116(7):73–83. doi: 10.1016/j.resuscitation.2017.05.018. [DOI] [PubMed] [Google Scholar]
- 8.Wells M., Goldstein L., Bentley A. A systematic review and meta-analysis of the accuracy of weight estimation systems used in paediatric emergency care in developing countries. Afr J Emerg Med. 2017 doi: 10.1016/j.afjem.2017.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nieman C.T., Manacci C.F., Super D.M., Mancuso C., Fallon W.F., Jr. Use of the Broselow tape may result in the underresuscitation of children. Acad Emerg Med. 2006;13(10):1011–1019. doi: 10.1197/j.aem.2006.06.042. [DOI] [PubMed] [Google Scholar]
- 10.Dicko A., Alhousseini M.L., Sidibé B., Traoré M., Abdel-Rahman S.M. Evaluation of the Mercy weight estimation method in Ouelessebougou, Mali. BMC Public Health. 2014;14:270. doi: 10.1186/1471-2458-14-270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Akabarian S., Vahedparast H., Ravanipour M., Mirzaei K. Comparison of Broselow tape measurements versus mother estimations of pediatric weights. Iran South Med J. 2013;16(2):138–143. [Google Scholar]
- 12.Trakulsrichai S., Boonsri C., Chatchaipun P., Chunharas A. Accuracy of three methods used for Thai children's body weight estimation. J Med Assoc Thai. 2012;95(9):1194–1199. [PubMed] [Google Scholar]
- 13.Wells M., Goldstein L., Bentley A. The accuracy of paediatric weight estimation during simulated emergencies: the effects of patient position, patient cooperation and human errors. Afr J Emerg Med. 2017 doi: 10.1016/j.afjem.2017.12.003. [in press] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sandell J.M., Charman S.C. Can age-based estimates of weight be safely used when resuscitating children? Emerg Med J. 2009;26(1):43–47. doi: 10.1136/emj.2008.061119. [DOI] [PubMed] [Google Scholar]
- 15.Bernius M., Thibodeau B., Jones A., Clothier B., Witting M. Prevention of pediatric drug calculation errors by prehospital care providers. Prehosp Emerg Care. 2008;12(4):486–494. doi: 10.1080/10903120802290752. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.