Abstract
African immigrant women survivors of cumulative trauma are at high risk for HIV infection. This study aims to identify survivors’ perceptions of (a) contextual (i.e., community, and relationship) and individual-level risk and protective factors for HIV among African immigrant women in the United States and (b) areas and strategies of HIV prevention intervention at contextual and individual levels. Qualitative data for this study were collected from African-born women (n = 39) in Maryland, Virginia, and Washington, DC, from February 2017 to March 2018. Seventeen in-depth interviews and five focus groups were conducted with African immigrant survivors of cumulative trauma. Results revealed HIV prevention intervention needs and risk and protective factors for HIV at the community (e.g., community education), relationship (e.g., intimate partner violence, family), and individual (e.g., women’s empowerment) levels. These findings can inform the development of culturally tailored multilevel HIV prevention interventions for African immigrant women.
Keywords: African immigrant, cumulative trauma, HIV, women
African immigrants (AI) are a fast-growing population in the United States (U.S.). In 2015, there were 2.1 million AI in the U.S., a substantial increase from 80,000 in 1970 (Anderson, 2017). In the HIV surveillance data from multiple regions in the U.S. (California, Georgia, King County [Washington State], Massachusetts, Minnesota, New Jersey, New York City, and Virginia), AI accounted for 3.8% of HIV diagnoses, though they constituted only 0.6% of the population (Kerani et al., 2008; Koku et al., 2016). Studies point to a disproportionate burden of human immunodeficiency virus (HIV) among AI women (AIW) in the U.S. (Blanas et al., 2013; Kerani et al., 2008; Okoro & Whitson, 2017). Approximately 41% of HIV diagnoses in the eight US regions occurred among AIW (Blanas et al., 2013; Kerani et al., 2008; Koku et al., 2016). HIV prevalence among AIW was found to be two to three times higher than among U.S.-born White women, U.S.-born Black women, and other foreign-born Black women (Blanas et al., 2013; Koku et al., 2016; Prosser, Tang, & Hall, 2012).
AIW are a high-risk group for HIV transmission through heterosexual contact (Johnson, Hu, & Dean, 2010), due to norms against use of condoms (Ahmed, 2013), cultural/religious beliefs such as “condom use is against religion” (DeJesus, 2007) and a general lack of knowledge of HIV-related risks, or existing resources for care (Foley, 2005; Rosenthal et al., 2003). In a study of practitioners serving AI in Minnesota, factors increasing HIV risk among AI included intimate partner violence (IPV), gender-based stigma, cultural beliefs, unprotected sex with husbands who have sex with other men and sexual/reproductive health illiteracy (Okoro & Whitson, 2017). AIW are likely to have experienced trauma pre-migration (Andersson et al., 2008; Small, Nikolova, & Narendorf, 2013) as well as post-migration (Akinsulure-Smith, Chu, Keatley, & Rasmussen, 2013; Mose & Gillum, 2016; West, 2016). A history of trauma has been associated with risk for HIV infection among women, irrespective of race or ethnicity (Wyatt et al., 2002). Factors placing abused women at risk for HIV infection may include psychological consequences of abuse on sexual decision making and inability to negotiate safer sex with an abusive partner. Moreover, financial dependence on sexual partners can limit women’s person control over HIV risk practices (Wyatt et al., 2002).
Despite their experiences of trauma or violence and need for care, AIW are less likely to seek services due to general barriers to health care access faced by AIs in the U.S. The barriers may include stigma of HIV, fear of deportation and isolation, cost of health care, lack of insurance and limited ability to navigate the U.S. health care system (Wafula & Snipes, 2014). A study on HIV positive AIs (n = 2714) found that AIs were more likely to present with AIDS diagnosis (45%) than both U.S.-born non-Blacks (25%) and U.S.-born Blacks (35%). AIs were also found to initiate care with more advanced HIV disease than the other two groups (Page, Goldbaum, Kent, & Buskin, 2009). In another study (n = 104), HIV infected AIs were less likely than non-immigrants to initiate antiretroviral therapy (ART; Beckwith et al., 2009). Barriers to care often included lack of knowledge of HIV care services in the community, financial concerns, lack of English language skills, and undocumented status contributing to fear of accessing the health care system (Akinsulure-Smith, 2013; Foley, 2005; Rosenthal et al., 2003). AIW may face more barriers to care than men because of their low status in family and community and unique challenges (e.g., financial dependence on partner). Thus, research is needed to better understand risk and protective factors for health issues such as HIV affecting AI populations and to inform prevention and intervention programs.
The socio-ecological model can be used to identify areas of intervention at multiple levels within the social ecology as a way of addressing behavioral risks (McLeroy, Norton, Kegler, Burdine, & Sumava, 2003) such as risk for HIV infection. The model describes the complex interplay between community-, relationship-, and individual-level factors that have a cumulative effect on health (Golden & Earp, 2012). Using a socio-ecological model, this study identified risk and protective factors for HIV and areas of preventative interventions in a high-risk sample of AIW (i.e., AIW survivors of cumulative trauma). The existing literature on AI communities in the U.S. has not focused on identifying multilevel risk and protective factors or areas of HIV preventative intervention, specifically among AIW survivors of cumulative trauma.
Cumulative trauma, in this study, refers to multiple types of traumatic experiences such as childhood abuse and forced sex by a partner. Women exposed to cumulative trauma are at higher risk for poor health outcomes than those who are exposed to single type of trauma or no trauma (Sabri et al., 2016). Chronic stressors such as cumulative violence exposures pose health risks such as risk for HIV infection (Hillis, Anda, Felitti, & Marchbanks, 2001). Specifically, forced sex, rape, or dry sex with an HIV-infected partner increases the risk for HIV transmission by making it easy for the virus to enter the blood via friction, tears, and bleeding. Further, power differentials and fear of the abuser limit women’s ability to negotiate safe sex, placing them at risk for HIV infection. Traumatic life experiences including adverse childhood experiences increase the risk for HIV infection indirectly through engagement in high-risk behaviors (e.g., sharing needles to inject drugs as a coping strategy; Andersson, Cockcroft, & Shea, 2008), some of which may represent attempts to achieve intimate interpersonal connections (Hillis et al., 2001). However, compared to the general U.S. population, higher rates of HIV among AIWs have been attributed more to heterosexual transmission and less to injection drug use–associated transmission (Blanas et al., 2013). This suggests that violence or trauma and associated sexual risks for HIV infection or transmission may be significant in the overall expansion of the HIV epidemic and its disproportionate impact on AIW in the U.S. Studies are, therefore, needed to inform culturally specific HIV prevention interventions that incorporate needs of AIW cumulative trauma survivors. Even though studies have examined risk factors for HIV infection among AIs in the U.S., there is a dearth of research on risk factors for HIV infection among AIW survivors of cumulative trauma and factors to consider in their HIV prevention or intervention needs. This study fills this gap by investigating factors related to risk for HIV infection and needs for preventative interventions at multiple levels among AIW survivors of cumulative trauma.
METHODS
Participants (n = 39) were recruited using purposive and snowball sampling techniques with assistance from AI collaborators in Virginia, Washington, DC, and Maryland. The strategies included flyers, word of mouth and presentation of study at community meetings. The eligibility criteria were (a) African born, (b) over 18 years of age, (c) ability to speak English, and (d) experiences of cumulative trauma (exposures to two or more types of lifetime violence). The two or more types of violence were based on their reporting of the following two or more forms of abuse in childhood, adolescence, and/or adulthood (e.g., caregiver physical abuse, caregiver psychological abuse, sexual assault by known adult), exposure to random shootings or riots in real life, intimate partner violence (physical, sexual, or psychological) or non-intimate partner abuse (e.g., physical or sexual assault by someone other than the partner).
Data was collected using demographic sheets, Adverse childhood experiences (ACE) questionnaire (Anda, Butchart, Felitti, & Brown, 2010; Ports et al., 2017), and semistructured focus group or in-depth interview guides. The demographic sheet was used to obtain information on participants’ characteristics such as age, education, marital status, employment, country of origin, length of time living in the U.S., and types of violence experienced. The 10-item ACE questionnaire asked participants to respond to a series of yes vs no questions on traumatic experiences in their first 18 years of life such as psychological, physical or sexual abuse, neglect, and household dysfunction (e.g., lived with household members who abused substances, were mentally ill or suicidal, or ever incarcerated, experienced parental divorce or separation, or witnessed domestic violence). The ACE score was calculated by summing the yes responses to each adverse experience.
The focus group guide explored post-migration experiences of participants or AIW in their networks, programs they participated in, their health concerns, stress management strategies, perspectives on HIV risks and needs for HIV prevention and other health issues. Focus groups can provide useful insight into people’s shared understanding of a phenomenon in a short time frame (Bloor, Frankland, Thomas, & Robson, 2001). The interview guide explored similar questions as the focus groups but probed more on personal trauma experiences which AIW would not have felt comfortable discussing in the group. In-depth interviews can provide useful information about personal experiences, feelings, perceptions, and opinions (Frechtling & Sharp, 1997), especially on sensitive topics such as traumatic life experiences, perpetrators of traumatic events and impact of traumatic life experiences on health. Both the interview and focus group sessions lasted from 60 to 90 minutes and were audio-recorded using digital recorders. Participants were compensated $35 for participation. The participants in the focus group were not the participants in the in-depth interviews. All study procedures were approved by Johns Hopkins University institutional review board.
Data were analyzed using a constructivist perspective and a thematic analysis procedure. Saturation was reached when no new themes were identified from the data. Thematic analysis with a constructivist perspective seeks to theorize the social and cultural contexts that drive the individual accounts shared with the researcher (Braun & Clark, 2006). The overarching codes and themes reflected contextual dimensions of AIW survivors’ experiences. Following the initial reading of transcripts, the principal investigator and a Masters student independently coded the focus groups and interview transcripts. The coding started with inductive coding to identify patterns in the data and identify themes. The codes with similar concepts were then collapsed into themes. These themes were then organized by domains of the socio-ecological framework, which present factors at multiple levels (e.g., individual, relationship community) as targets of interventions (McLeroy, Bibeau, Steckler, & Glanz, 1988). Participants perspectives on risk for HIV infection and interventions were described at the community, relationship, and individual levels. Inconsistencies in coding were addressed in meetings. To establish trustworthiness, an audit trail was maintained through detailed notes of research activities, recording of thoughts and experiences and regular debriefing sessions among the coders for reflexivity. Data from the interviews and focus groups were analyzed separately prior to triangulation. The findings were triangulated by comparing the perspectives of participants in the focus groups with those from the individual interviews.
RESULTS
The five focus groups (FG) primarily included 22 AIW from Ethiopia, Nigeria, Eritrea, Sudan, and Sierra Leone. The number of participants in each focus group ranged from four to five. The 17 in-depth interviews (IDI) were conducted with AIW from Ethiopia (n = 6), Eritrea (n = 2), Sudan (n = 2), Uganda (n = 4), Kenya (n = 1), Congo (n = 1), and Ghana (n = 1). Participants in the focus groups were different. Women were, on average, 39.9 years old (SD = 9.5). They had been in the U.S. for an average of 11.08 years (SD = 8.21). Approximately 77% (n = 30) of the AIW were employed. About 77% were married (n = 26), and 12% (n = 4) were divorced or separated. More than half of the AIW (73.5%, n = 25) had a bachelor’s or higher degree, with data on education missing for 5 participants. More than half of the AIW were exposed to war (51.3%, n = 20), were threatened physical harm (59%, n = 23), were made to feel unsafe (56.4%, n = 22), or experienced forced sex (53.8%, n = 21). Forty-six percent (46.2%, n = 18) reported experiencing physical violence. The average score on adverse childhood experiences was 2.31 (SD = 1.3), with most frequently reported childhood experiences being abuse by parents/caregiver (41–51.3%, n = 16–20) psychologically and physically, followed by sexual abuse by an adult 5 year or older (25.6%, n = 10).
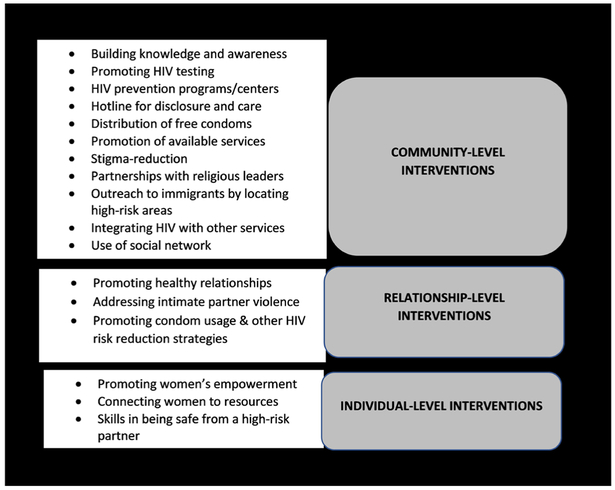
Analysis of qualitative data revealed risk and protective factors for HIV as well as needs for interventions (Figure 1) at the: (a) community level, (b) relationship level, and (c) individual level. The community-level risks for HIV infection were identified as lack of knowledge and awareness in the community, culture of polygamy, immigration-related changes, and stigma for HIV that related to barriers to disclosure and treatment. The protective factors for HIV identified at the community level were HIV prevention programs for AIs, building education and knowledge in the community, addressing stigma of HIV, promoting community norms of HIV testing before marriage, distributing free condoms, and partnering with churches for HIV prevention programming. Factors at the relationship level that increased risk for HIV infection included lack of decision-making power, IPV, inability to negotiate condom use with a partner, having a high-risk sexual partner, and partner’s nondisclosure of HIV positive status. Family was protective when it provided support to women who were at risk from their partners. Family-level interventions that promote healthy relationships and address IPV were discussed as protective against HIV infection. The individual-level risks for HIV infection were reported to be poverty and other needs driving sexual risk, traumatic life experiences, and use of alcohol and drugs. Protective factors identified were abstinence from sex before marriage, use of self-protection strategies, and women’s independence and education. In the sections below, pseudonyms are used as identifiers instead of real names to protect the identity of the participants.
FIGURE 1.
Multilevel interventions for HIV prevention among African immigrants.
COMMUNITY-LEVEL FACTORS AND NEEDS FOR INTERVENTIONS
COMMUNITY-LEVEL FACTORS RELATED TO RISK FOR HIV INFECTION
(a) Lack of Knowledge and Awareness. Many AIW (n = 8; FG and IDI) attributed the risk for HIV infection to lack of knowledge and awareness in the community. Maryam, for instance, shared: “I think there is a lack of awareness, people don’t know about how to prevent HIV and how to use condoms.” (Maryam, Sudan, age 47; IDI). Abeni described how lack of awareness in the community can impact testing or disclosure of HIV positive status:
There’s no awareness in the community. If there’s no awareness and there’s no form of support, and I’m going to be stigmatized, I don’t want to know my HIV status. If I know my status, I’m not going to tell anybody.
(Abeni, Nigeria, age 49; FG)
According to Aynalem, immigrant children may receive HIV education in schools, but that information may not reach their parents:
I hope children will get much HIV information from schools, but I don’t think they will share it with their parents. I see a huge cultural and language gap between the children that are born and brought up here and their parents.
(Aynalem, Ethiopia, age 39; IDI)
It was considered important to specifically educate women because of lack of acceptance of HIV as a problem by men in the community. “I think our women need to be educated on STDs because men don’t care. Some of them don’t even believe HIV exists. They’re like, ‘It’s a lie. White people invented this.’” (Fatu, Sierra Leone, age 34; FG).
(b) Culture of Polygamy. Although having multiple sexual partners was identified as a risk factor for HIV infection by majority of AIW, a small number of AIW (n = 2; FG) attributed the risk for HIV infection to legitimization of multiple sexual relationships via a culture of polygamy among African immigrants:
Many women get infected, because men can have multiple partners. Then they just spread the viruses and the STDs. Even in America they have polygamy here. The country has laws here, but they can’t leave their wives due to cultural and religious reasons.
(Marie, Sierra Leone, age 28; FG)
Family support of polygamy and pressure to stay in a polygamous marriage further place woman at risk for HIV infection: “Families are so used to polygamy, family will say- All men play. You have that player. … The pressure will make you stay with that person.” (Fatu, Sierra Leone, age 34; FG).
(c) Factors Related to Migration to the U.S. Some AIW (n = 3; FG and IDI) related risk for HIV infection to immigration related factors such as length of immigration and lack of community ties in the US. For example, Adera explained:
If Ethiopian immigrants are coming before 8 years, they don’t have any knowledge about HIV. When you say it’s about the HIV, they don’t want to listen. We don’t have any center to give them the information. If they are coming now, they have good knowledge about HIV. Ethiopia is working hard on HIV.
(Adera, Ethiopia, age 33; IDI)
Lack of community ties in the U.S. was associated with risk for HIV infection by two AIW:
Here you don’t have the community watching you. If you are back home, everybody knows you are husband of this family. That’s holding them. Here men are going out with multiple women and women don’t have control. I don’t believe they would say, Oh, I don’t trust you. You should use condom.
(Aynalem, Ethiopia, age 39; IDI)
Abioye shared: “Back home you cannot just go out and sleep with anybody. Here, who cares. You get husbands angry, they go and have sex with a prostitute. It’s easier for them.” (Abioye, Nigeria, age unknown; FG).
(d) Stigma of HIV: Barriers to Testing and Disclosure. Some AIW (n = 7; FG and IDI) described HIV-related stigma and shame as barriers to HIV testing and care. HIV infected women were more likely than men to not disclose their HIV status due to embarrassment and shame: “When you are infected by a husband, then you are not at fault. If you a girl and you acquire HIV, you are a shame to your family and to the public” (Namazzi, Uganda, age 67; IDI).
Akifa shared her thoughts about perceptions of HIV in the community:
If a woman gets infected, she would die. She cannot talk about it. We don’t think HIV is a normal disease … stigma comes with it. How you get HIV, that’s the number one question. No one thinks that you’re innocent. … You did something wrong to get it.
(Akifa, Sudan, age 35; FG)
A few AIW (n = 4; FG) believed that limited knowledge of modes of HIV transmission can be a barrier to disclosure of HIV status:
The only way to get HIV in Sudan is having an extramarital affair. People don’t know you can get HIV through a blood transfusion or whatever. A lot of people think if you have HIV, that means you sleep with a man.
(Akifa, Sudan, age 35; FG)
Fear of repercussion by the community was a barrier to disclosure (n = 15; FG and IDI):
Once you say it, people won’t come close to you because there’s not enough awareness that you’re not going to catch HIV by sitting close to somebody. People think if I touch someone with HIV, I’m going to get it.
(Abioye, Nigeria, age unknown; FG)
Interestingly, Abbo mentioned that ostracizing an HIV positive person is protective against HIV. “The community decreases the risk for HIV—because they try to shun away from the person who has HIV” (Abbo, Uganda, age 60; IDI). Zoya believed that HIV-related stigma is more prevalent among immigrants in the US than Africans in her home country. “HIV is a big taboo. I have three friends who were teaching the public in Ethiopia. They disclosed their status there. When they came here, they are silent because of the stigma. It’s no more taboo there, but it’s still taboo here in USA” (Zoya, Ethiopia, age 41; FG).
NEEDS FOR COMMUNITY-LEVEL HIV PREVENTION INTERVENTIONS
Many AIW (n = 18; FG and IDI) highlighted the need for HIV prevention education programs for African immigrants in the US. According to Aynalem: “I have never seen any program on HIV for women. I don’t think there is anything for the community” (Aynalem, Ethiopia, age 39; IDI). Neela, an Ethiopian participant, stated: “It’s better to show [the community] how to prevent HIV. It’s not about they don’t know about HIV/AIDS. They know, but it’s more to train them how to prevent from getting that thing” (Neela, Ethiopia, age 36; IDI). Alia, a survivor from Sudan, said: “We need orientation … we need to let everybody know about HIV risk and how to prevent themselves from infection” (Alia, Sudan, age 47; IDI). For some AIW (n = 3; FG and IDI), women’s education was more important than men:
Education and awareness for women is important because men know how they can get HIV but still they go outside. I don’t think there is hope, say, if you educate men for 100 years, nothing will come. We have to educate women to protect themselves because they are the victims.
(Akifa, Sudan, age 35; FG)
Others expressed the need to focus efforts on educating men (n = 4; FG and IDI):
I think that men are the ones who should be informed, should be educated. They just know what their culture teaches them. They don’t want to learn about what is supposed to happen. It’s just the way they’ve been doing stuff.
(Fatu, Sierra Leone, age 34; FG)
Other suggested components of HIV prevention interventions at the community level (n = 5, FG and IDI) included distributing free condoms, promoting norms of HIV testing before marriage, addressing stigma of HIV, and providing an anonymous hotline for HIV care to preserve privacy and confidentiality:
There must be a hotline that a woman can call and get advice in her language. That’s what we were doing back home in Ethiopia. The volunteers who just disclosed their HIV positive status and using medication, they leave their number if someone wants to call them and ask. That’s how they are teaching the public. … hotline to call and to contact someone in their own language … because they don’t want to go physically to the service with the letters “HIV.”
(Zoya, Ethiopia, age 41; FG)
One survivor highlighted the need for stigma-reduction community interventions:
I think once you remove the stigma about HIV in the African community, a lot of lives will be saved. I even believe strongly in removing the stigma than the medications, because at least if they know early, they are willing to accept it, then they’ll get treated. You can have all the medicines in the world, but if the person doesn’t want to even know if they have it, then the medicines are pointless. Then they keep infecting others … removing that stigma, just because I have HIV doesn’t mean you cannot hang out with me. I’m still the same person. I just have something in my blood. It doesn’t contaminate you. Just making it okay. It’s not their fault that they have this disease, so don’t make them feel so bad.
(Marie, Sierra Leone, age 28, FG)
Some AIW survivors (n = 6; FG and IDI) discussed the role of religious institutions in HIV prevention and the need for including religiosity in HIV prevention interventions: “The word of God can help them to refuse sin. Sleeping with another man outside your marriage is a sin. Then you would respect yourself, and you’d respect God.” (Namazzi, Uganda, age 67; IDI). Nyala mentioned:
Get partnership with the local churches and the priests-especially with the most senior churches that have been here in the service for a long time may have really well-developed systems in there. Start there, in all religions.
(Nyala, Ethiopia, age 38; IDI)
However, Eshe did not believe church could help:
I don’t think church is the place. If you say HIV, they will say, “You are trying to destroy a family” … condom … HIV … is not an easy thing to bring into church. They still associate HIV with sin, so that’s certainly victimization for them to be there and the pastor teaching the audience that HIV comes because of the sin, because of your bad activities.
(Eshe, Ethiopia, age 42, FG)
In the end, however, Eshe mentioned:
We don’t want to block the church because that’s where people gather, but it has to be contextualized in what the church believes—if the media works heartily, the church community, the church leaders can also be changed.
(Eshe, Ethiopia, age 42; FG)
Education of religious leaders appeared to be critical for effective HIV prevention among AIW.
Some AIW (n = 5; FG and IDI) shared strategies for engaging African immigrant communities in HIV prevention interventions. These included promotion of available HIV services in the U.S. (e.g., free HIV testing), creating awareness through media and other sources and engaging the church leaders: “We have to promote what we have such as free testing, free services using brochure, flyer…” (Adera, Ethiopia, age 33; IDI). A suggested strategy was to implement HIV prevention programs in locations where immigrants are most likely to come in for services:
The first contact point for immigrants are the providers of the social security card, ID, DMV. … Maybe food stamp, maybe TANF, maybe WIC. Resettlement agencies… programs designed for cultural orientation. We have to mainstream HIV with other services.
(Eshe, Ethiopia, age 42; FG)
Nyala highlighted the need to target specific locations:
You need to start from where the risk behaviors are coming from. For example, the night clubs. … Ethiopian restaurants, where there are a lot of them who don’t have work permit to get hired by companies. A woman who is struggling to fulfill her livelihood can easily be a target by an HIV positive person. Start where they work. … go to school.
(Nyala, Ethiopia, age 38; IDI)
Other suggested strategies were to package the HIV program as a general health program and integrating HIV education with other services: “Don’t say upfront that it’s about HIV—call it community health fair … or health practice. Let there be some free food. For any conversations in the community, just call it health education.” (Morayo, Nigeria, age 32; FG). Anyalem provided suggestions for integrated HIV programs: “HIV should be integrated with other services. It cannot be a separate HIV service. If that office gives some service on immigration, for example, you can integrate those things with it.” (Aynalenm, Ethiopia, age 39; IDI). Network of AIW in the community could be used to promote HIV prevention programming. “African immigrant women help each other. If some woman from our community is uncomfortable, they can help her. They can come every day, visit her, and support her.” (Aarifa, Sudan, age 34; IDI).
RELATIONSHIP-LEVEL FACTORS AND NEEDS FOR INTERVENTIONS
RELATIONSHIP-LEVEL FACTORS RELATED TO RISK FOR HIV INFECTION
(a) Power Imbalance, Abuse, and Inability to Negotiate Condom Use With a Partner. Many AIW (n = 9; FG and IDI) discussed the role of power imbalance and abuse in heterosexual relationships which lead to inability to negotiate protective sex:
Everything puts women in abusive relationships at risk because they don’t have control. … Once they are in a relationship, they can’t do anything to prevent HIV. They only have two options, either challenging their partner or leaving the marriage.
(Nyala, Ethiopia, age 38; IDI)
Women in abusive relationships are at higher risk than women in non-abusive relationships:
If the person that has hit you on the head, has slapped you, you are not going to ask him to use condom. If somebody’s abusing you, they may be having other partners. They think they’re entitled to have concubines all over. You just have to have sex with them. They force the woman to do whatever.
(Ododo, Nigeria, age 36; FG)
Married women are unable to negotiate protective sex. Further, according to Nyala, families pressurize women to stay in abusive relationships, which place them at risk for HIV infection.
You would be expected to fight for your marriage. It doesn’t matter at what cost. By encouraging you to stay in the marriage, family is, at the same time, encouraging you to live that HIV risk life.
(Nyala, Ethiopia, age 38; IDI)
(b) High-Risk Sexual Partner. According to many AIW (n = 13, FG and IDI), having a high-risk sexual partner/husband (i.e., a partner who is HIV positive, has multiple sexual relationships, and refuses to use condoms) placed AIW at risk for HIV infection. Kayla mentioned that a man being HIV positive and hiding his status is a risk factor for HIV:
Most HIV-infected women got it from their husbands. The husband may have already found out that he is positive. He may not tell her. If there is violence, the sexual relationship is abusive, and she has no right to negotiate about using condom.
(Kayla, Ethiopia, age 37; FG).
According to Akifa, husband’s sexual behaviors (e.g., having multiple sexual partners) place women at risk for HIV infection: “You only get it from your husband because we don’t go outside. It’s the only source. They cannot get it from anybody” (Akifa, Sudan, age 35; FG).
(c) Level of Support From Extended Family Members. Five AIW (FG and IDI) highlighted the roles of extended family members in women’s risk for HIV infection in intimate partner relationships. For instance, family pressure to stay with an abusive or a high-risk sexual partner (e.g., a husband who engages in multiple sexual relationships and is HIV positive) can place women at risk for HIV infection. Mermba, however, discussed the protective role of family in addressing the risk associated with the partner: “If a wife knows he has some other women on the outside she has to tell the parents. Family of the girl can tell her to leave him. Families bring communities to settle that matter” (Miermba, Uganda, age 61; IDI). Abbo discussed how family protect women by asking them to abstain from sexual relationships outside marriage. “[Family members] decrease the risk of HIV by saying, ‘Don’t go with any other man’” (Abbo, Uganda, age 60; IDI). However, families may not always play a protective role. Zoya, for instance, explained: “If she’s married, people will not involve at all.... If she’s older in age, and if she’s by herself, nobody will comment on anything” (Zoya, Ethiopia, age 41; FG).
NEEDS FOR RELATIONSHIP-LEVEL HIV PREVENTION INTERVENTIONS
Promoting healthy relationships and addressing IPV and sexual risk behaviors (e.g., multiple partners) were highlighted as critical needs for prevention by five survivors (FG and IDI): “If we train both men and women not to mishandle their marriage then I think HIV will be eradicated. Graze in your field, in your area, in your territory. Husband and wife only” (Namazzi, Uganda, age 67; IDI). The importance of promoting condom usage in marriages was discussed: “Immigrant women have to take all precautions like using condoms. They have to know their husband risk for HIV” (Kamali, Ethiopia, age 40; IDI). Nyala believed a healthy relationship in itself is protective against HIV: “If it’s a really caring, loving, romantic relationship, HIV wouldn’t be a problem. If you marry a guy who really loves you for who you are. That person would care about you” (Nyala, Ethiopia, age 38; FG).
INDIVIDUAL-LEVEL FACTORS AND NEEDS FOR INTERVENTIONS
INDIVIDUAL-LEVEL FACTORS RELATED TO RISK FOR HIV INFECTION
(a) Poverty, Financial, and Other Needs. Some AIW (n = 5; FG and IDI) highlighted the roles of poverty, finances, and other needs (e.g., trading sex for help with immigration) in increasing women’s risk for HIV infection. Namazzi, for example, mentioned:
One of the things that place women at the risk for HIV infection is they are poor. You don’t have food at home, and somebody come and say I will give you money. … you are vulnerable to committing adultery.
(Namazzi, Uganda, age 67; IDI)
Nyala shared that needs besides finances can also increase HIV risk: “I hear stories that women engage in prostitution, for money, for green card, for so many things.” (Nyala, Ethiopia, age 38; IDI)
(b) Engagement in High-Risk Behaviors. According to some AIW (n = 5; FG and IDI), women’s own behaviors and choices (e.g., multiple partners, substance misuse) can also place them at risk for HIV infection. For some women, their high-risk behaviors and choices could be related to their traumatic life experiences. For instance, one of the consequences of trauma is giving up in life. Neela shared an experience of her friend who had to migrate to the U.S. because of circumstances back home:
She ended up being a server and one night was raped by multiple people. After that, she became mental because of the trauma. She became a prostitute. When people start to give up in life, they don’t care whether they caught HIV or not, so they start to become careless about everything.
(Neela, Ethiopia, age 36; IDI)
Use of alcohol or drugs was also identified as a risk factor, as stated by Abbo: “Involvement in alcohol, drugs, can lead many women to strangers” (Abbo, Uganda, age 60; IDI).
NEEDS FOR INDIVIDUAL-LEVEL HIV PREVENTION INTERVENTIONS
Many survivors (n = 14; FG and IDI) shared that AIW can be protected from risk for HIV infection through education, and empowerment. Two survivors expressed the need for promoting abstinence before marriage. Eshe, for instance, mentioned: “Abstinence is the best way. That’s what we are told and learnt through church and the culture itself” (Eshe, Ethiopia, age 42; FG). Women’s empowerment was considered an important component for HIV prevention: “Empowering women is really important. Even when you’re married, you can demand your husband to put it on, especially if you start to see something that’s not right.” (Adama, Sierra Leone, age 33; FG). This is especially important for women in abusive relationships: “If the husband abuses her, she has to be away from him because he’s going to give her the virus. You can help her find some place for her. You have to help her from A to Z because she needs a lot of help.” (Aarifa, Sudan, age 34; IDI). HIV prevention needs to incorporate other needs for women’s empowerment:
The first thing you should approach it from is from what is most important in their life. The HIV issue … abuse. … has always the second importance in life. The majority of women who you find in this situation are those who are still struggling in their lives.
(Nyala, Ethiopia, age 38; IDI)
Also highlighted was the need for women to educate themselves: “We have to educate ourselves … especially being a woman” (Awusi, Ghana, age 42; IDI). Some AIW (n = 5) discussed strategies women can use to keep themselves safe from HIV. For example, Kamali mentioned: “Maybe she needs to spy on her husband if he is involved with another person. It is always better to use condoms, especially if he drinks or socializes a lot.” (Kamali, Ethiopia, age 40; IDI). Dembe suggested: “Women should also be carrying their own condoms instead of relying on the male” (Dembe, Uganda, age 55; IDI).
DISCUSSION
This study identified risk and protective factors for HIV and needs for interventions at multiple levels from the perspectives of AIW survivors of cumulative trauma. For example, one community-level risk for HIV infection was lack of knowledge and awareness of HIV among AIs. Polygamy and stigma of HIV were culturally specific risks that served as barriers to disclosure and treatment. Lack of knowledge of the care system was also identified as a barrier to care among HIV positive AIs in a study in the Twin Cities (Othieno, 2007). Thus, community-level interventions for AIs must focus on building knowledge and awareness of HIV, providing free services such as condoms and addressing stigma of HIV. It is important to involve key stake-holders such as church leaders or community leaders in designing and implementing HIV prevention programs for AIs. At the relationship level, AIW identified IPV, and inability to negotiate condom use, as factors that placed women at risk for HIV infection. The relationship between IPV and HIV is supported by many studies (e.g., Li et al., 2014; Mitchell, Wight, Van Heerden, & Rochat, 2016). In a systematic review and meta-analysis of 28 studies (Li et al., 2014) involving 16 countries, physical IPV, and both physical and sexual IPV were significantly associated with HIV infection (Li et al., 2014). Specifically, sexual IPV can directly lead to HIV through forced unprotected sex or inability to negotiate condom use with an infected abusive partner. Physiologically, risk for HIV infection increases through trauma to the vaginal or rectal mucosa (Bergmann & Stockman, 2015; Mitchell et al., 2016). Further, chronic stress in IPV can increase susceptibility to HIV infection by compromising the immune system (Campbell et al., 2008). Additional evidence suggests that abusive partners are more likely than those who are non-abusive to engage in a range of HIV risk behaviors such as multiple partners (Mitchell et al., 2016).
AIW perceived male partner not disclosing his HIV positive (+) status as a risk factor for HIV infection. Disclosure of HIV+ status to a sexual partner is critical for HIV prevention (Kalichman, Kalichman, Cherry, & Grebler, 2016). Kalichman et al. (2016), in their study, with 538 sexually active HIV+ men found that undisclosed HIV+ status was common and associated with unprotected sex with uninfected partners and less adherence to care. Thus, interventions are needed that enhance disclosure self-efficacy, and increase understanding of HIV infectiousness (Kalichman et al., 2016). The relationship-level interventions, therefore, must focus on promoting healthy relationships, addressing IPV, building healthy communication including condom negotiation skills and skills in identifying and addressing risks associated with a high-risk partner. Educating AI men about HIV care options for HIV+ individuals, and addressing fear and stigma related to disclosure may lead to more openness about the HIV+ status with a sexual partner. In this study, family support in addressing risk associated with a high-risk partner was identified as protective. Research shows that higher levels of social support, consistent with HIV prevention can lead to fewer HIV risk behaviors among adults (Qiao, Li, & Stanton, 2014).
As shown in prior research (Hallman, 2005), poverty and other needs were identified as individual-level risk factors for HIV. Poverty can lead to transactional sex for money or reduce access to information about safe sex practices (Hallman, 2005). The protective factors identified were AIW’s education and empowerment. Thus, HIV prevention for AIW must incorporate empowerment components such as connecting them with educational opportunities and other resources in the U.S. Consistent with prior research among non-immigrants (Fisher, Bang, & Kapinga, 2007; Pence et al., 2008), alcohol/drug abuse was perceived as a risk factor for HIV infection. Alcohol/drug use increases risk for HIV infection through sharing of injection drug use equipment, exchange of sex for drugs and sexual disinhibition resulting from drug/alcohol use (Pence et al., 2008). Abusive partner’s alcohol/drug problems can further place AIW at risk for HIV infection. Some AIW emphasized the importance of abstinence and use of self-protection strategies. It is, however, important to consider contextual factors affecting AIW’s ability to protect themselves from HIV and to move beyond the individual woman and her behaviors (Webber, 2007). For instance, traumatic experiences and unmet needs for mental health care can lead to high risk sexual behaviors. Thus, it is critical to screen AIW for their traumatic life experiences, impact on mental health and role of these experiences and mental health on risk for HIV infection.
CONCLUSION
For AIW survivors of cumulative trauma, there is need for multifaceted HIV prevention interventions that incorporate socio-cultural contexts and needs such as education, skills, and overall empowerment. Our study findings can be useful in developing HIV prevention programs for AIW in the U.S. This study was based on self-report and is therefore limited by retrospective bias and survivors’ willingness to share information. Nonetheless, this study provides an important contribution to the knowledge of HIV prevention needs of diverse groups of AIW survivors of cumulative in the U.S., which could be used in designing culturally tailored trauma informed multicomponent HIV prevention programs.
Acknowledgments
This research was supported by the Eunice Kennedy Shriver National Institute for Child Health & Human Development (K99HD082350 and R00HD082350).
REFERENCES
- Ahmed M (2013). Determinants of condom use and HIV prevention among East African immigrants in Minnesota (Doctoral dissertation). University of Texas; at El Paso. [Google Scholar]
- Akinsulure-Smith AM Chu T Keatley E, & Rasmussen A (2013). Intimate partner violence among West African immigrants. Journal of Aggression, Maltreatment & Trauma, 22, 109–129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anda RF Butchart A Felitti VJ, & Brown DW (2010). Building a framework for global surveillance of the public health implications of adverse childhood experiences. American Journal of Preventative Medicine, 39, 93–98. [DOI] [PubMed] [Google Scholar]
- Anderson M (2017). African immigrant population in US steadily climbs. Pew Research Center. Retrieved from http://www.pewre-search.org/fact-tank/2017/02/14/african-immigrant-population-in-u-s-steadily-climbs/
- Andersson N Cockcroft A, & Shea B (2008). Gender-based violence and HIV: Relevance for HIV prevention in hyperendemic countries of Southern Africa. AIDS, 22, S73–S86. [DOI] [PubMed] [Google Scholar]
- Beckwith CG DeLong AK Desjardins SF Gillani F Bazerman L Mitty JA, … Cu-Uvin S (2009). HIV infection in refugees: A case-control analysis of refugees in Rhode Island. International Journal of Infectious Diseases, 13, 186–192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bergmann JN, & Stockman JK (2015). How does intimate partner violence affect condom and oral contraceptive use in the United States: A systematic review of the literature. Contraception, 91, 438–455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blanas DA Nichols K Bekele M Lugg A Kerani RP, & Horowitz CR (2013). HIV/AIDS among African-born residents in the United States. Journal of Immigrant and Minority Health, 15, 718–724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bloor M Frankland J Thomas M, & Robson K (2001). Focus groups in social research. London, UK: Sage. [Google Scholar]
- Braun V, & Clarke V (2006). Using thematic analysis in psychology. Qualitative Research in Psychology, 3, 77–101. [Google Scholar]
- Campbell JC Baty ML Ghandour RM Stockman JK Francisco L, & Wagman J (2008). The intersection of intimate partner violence against women and HIV/AIDS: A review. International Journal of Injury Control and Safety Promotion, 15, 221–231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- M. De Jesus Carrete C Maine C, & Nalls P (2015) Attitudes, perceptions and behaviors towards HIV testing among African-American and East African immigrant women in Washington DC: Implications for targeted HIV testing promotion and communication strategies. Sexually Transmitted Infections, 91, 569–575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher JC Bang H, & Kapiga SH (2007). The association between HIV infection and alcohol use: A systematic review and meta-analysis of African studies. Sexually Transmitted Infections, 34, 856–863. [DOI] [PubMed] [Google Scholar]
- Foley EE (2005). HIV/AIDS and African immigrant women in Philadelphia: Structural and cultural barriers to care. AIDS Care, 17, 1030–1043. [DOI] [PubMed] [Google Scholar]
- Frechtling J, & Sharp L (1997). User-friendly handbook for mixed method evaluations. Division of Research, Evaluation and Communication, National Science Foundation; Retrieved from https://www.nsf.gov/pubs/1997/nsf97153/start.htm [Google Scholar]
- Golden SD, & Earp JAL (2012). Social ecological approaches to individuals and their contexts: Twenty years of health education & behavior health promotion interventions. Heath Education & Behavior, 39, 364–372. [DOI] [PubMed] [Google Scholar]
- Hallman K (2005). Gendered socioeconomic conditions and HIV risk behaviours among young people in South Africa. African Journal of AIDS Research, 4, 37–50. [DOI] [PubMed] [Google Scholar]
- Hillis SD Anda RF Felitti VJ, & March-banks PA (2001). Adverse childhood experiences and sexual risk behaviors in women: A retrospective cohort study. Family Planning Perspectives, 33, 206–211. [PubMed] [Google Scholar]
- Johnson AS Hu X, & Dean HD (2010). Epidemiologic differences between native-born and foreign-born black people diagnosed with HIV infection in 33 US states, 2001–2007. Public Health Reports, 125, 61–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalichman SC Kalichman MO Cherry C, & Grebler T (2016). HIV disclosure and transmission risks to sex partners among HIV-positive men. AIDS Patient Care and STDs, 30, 221–258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kerani RP Kent JB Sides T Dennis G Ibrahim AR Cross H, … Golden MR (2008). HIV among African-born persons in the United States: A hidden epidemic? Journal of Acquired Immune Deficiency Syndromes, 49, 102–106. [DOI] [PubMed] [Google Scholar]
- Koku EF Rajab-Gyagenda WM Korto MD Morrison SD Beyene Mbajah J, & Ashton C (2016). HIV/AIDS among African immigrants in the US: The need for disaggregating HIV surveillance data by country of birth. Journal of Health Care for the Poor and Underserved, 27, 1316–1329. [DOI] [PubMed] [Google Scholar]
- Li Y Marshall CM Rees HC Nunez A Ezeanolue EE, & Ehiri JE (2014). Intimate partner violence and HIV infection among women: A systematic review and meta-analysis. Journal of the International AIDS Society, 17, 18845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLeroy KR Bibeau D Steckler A, & Glanz K (1988). An ecological perspective on health promotion programs. Health Education Quarterly, 15, 351–377. [DOI] [PubMed] [Google Scholar]
- McLeroy KR Norton BL Kegler MC Burdine JN, & Sumaya CV (2003). Community-based interventions. American Journal of Public Health, 93, 529–533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell J Wight M Van Heerden A, & Ro-chat TJ (2016). Intimate partner violence, HIV and mental health: A triple epidemic of global proportions. International Review of Psychiatry, 28, 452–463. [DOI] [PubMed] [Google Scholar]
- Mose GB, & Gillum TL (2016). Intimate partner violence in African immigrant communities in the United States: Reflections from the IDVAAC African women’s round table on domestic violence. Journal of Aggression, Maltreatment & Trauma, 25, 50–62. [Google Scholar]
- Okoro ON, & Whitson SO (2017). HIV risk and barriers to care for African-born immigrant women: A socio-cultural outlook. International Journal of Women’s Health, 9, 421–429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Othieno J (2007). Understanding how contextual realities affect African born immigrants and refugees living with HIV in accessing care in the Twin Cities. Journal of Healthcare for Poor and Underserved, 18, 170–188. [DOI] [PubMed] [Google Scholar]
- Page LC Goldbaum G Kent JB, & Buskin SE (2009). Access to regular HIV care and disease progression among Black African immigrants. Journal of the National Medical Association, 101, 1230–1236. [DOI] [PubMed] [Google Scholar]
- Pence BW Thielman NM Whetten K Ostermann J Kumar V, & Mugavero MJ (2008). Coping strategies and patterns of alcohol and drug use among HIV-infected patients in the United States Southeast. AIDS Patient Care and STDs, 22, 869–877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ports KA Lee RD Raiford J Spikes P Manago C, & Wheeler DP (2017). Adverse childhood experiences and health and wellness outcomes among Black men who have sex with men. Journal of Urban Health, 94, 375–383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prosser AT Tang T, & Hall HI (2012). HIV in persons born outside the United States, 2007–2010. JAMA, 308, 601–607. [DOI] [PubMed] [Google Scholar]
- Qiao S Li X, & Stanton B (2014). Social support and HIV-related risk behaviors: A systematic review of the global literature. AIDS and Behavior, 18, 419–441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenthal L Scott DP Kelleta Z Zikarge A Momoh M Lahai-Momoh J, … Baker A (2003). Assessing the HIV/AIDS health services needs of African immigrants to Houston. AIDS Education and Prevention, 15, 570–580. [DOI] [PubMed] [Google Scholar]
- Sabri B Holliday C Alexander KA Huerta J Cimino A Callwood G, & Campbell JC (2016). Cumulative violence exposures: Black women’s responses and sources of strength. Social Work in Public Health, 31, 127–139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Small E Nikolova SP, & Narendorf SC (2013). Synthesizing gender-based HIV interventions in Sub-Sahara Africa: A systematic review of the evidence. AIDS and Behavior, 17, 2831–2844. [DOI] [PubMed] [Google Scholar]
- Wafula EG, & Snipes SA (2014). Barriers to healthcare access faced by Black immigrants in the US: Theoretical considerations and recommendations. Journal of Immigrant and Minority Health, 16, 689–698. [DOI] [PubMed] [Google Scholar]
- Webber G (2007). The impact of migration on HIV prevention for women: Constructing a conceptual framework. Health Care for Women International, 28, 712–730. [DOI] [PubMed] [Google Scholar]
- West CM (2016). African immigrant women and intimate partner violence: A systematic review. Journal of Aggression, Maltreatment & Trauma, 25, 4–17. [Google Scholar]
- Wyatt GE Myers HF Williams JK Kitchen CR Loeb T Carmona JV, … Presley N (2002). Does a history of trauma contribute to HIV risk for women of color? Implications for prevention and policy. American Journal of Public Health, 92, 660–665. [DOI] [PMC free article] [PubMed] [Google Scholar]