Abstract
Background
Low cardiorespiratory fitness is strongly associated with cardiovascular diseases and mortality. Although increased physical activity can improve cardiorespiratory fitness, this relationship has not been examined in a large bariatric population undergoing perioperative care focusing on long-term lifestyle change.
Objectives
To evaluate changes in physical activity, weight loss, and cardiorespiratory fitness up to 24 months after bariatric surgery, and to evaluate the relationships of change in physical activity with weight loss and change in cardiorespiratory fitness.
Materials and Methods
Four thousand seven hundred eighty-five patients who underwent primary Roux-en-Y gastric bypass or sleeve gastrectomy between January 2012 and December 2014 were included. Physical activity was assessed by the Baecke questionnaire (work, leisure, and sport activity) and cardiorespiratory fitness, defined as VO2max relative to fat-free mass (VO2max/FFM), was assessed by the Åstrand test.
Results
Twenty-four months postoperative, significant improvements were seen in sport and leisure activity assessments (n = 3548, P < 0.001), weight loss (n = 3695, P < 0.001), and VO2max/FFM (n = 1852, P < 0.001). Furthermore, regression analysis showed that change in leisure activity was positively associated with weight loss (n = 3535, ß = 1.352, P < 0.001) and change in sport activity was positively associated with change in VO2max/FFM (n = 1743, ß = 1.730, P < 0.001).
Conclusion
Bariatric surgery complemented by a comprehensive bariatric care program can lead to improvement in physical activity, as well as weight loss and improvement in cardiorespiratory fitness. The positive associations of change in leisure activity with weight loss and change in sport activity with cardiorespiratory fitness suggest that bariatric care programs can enhance postoperative outcomes by improving the patient’s physical activity.
Keywords: Bariatric care, Cardiorespiratory fitness, VO2max, Weight loss, Physical activity
Introduction
Bariatric surgery has emerged as the most effective treatment option for those suffering from morbid obesity [1, 2]. The American Society of Metabolic and Bariatric Surgery (ASMBS), the American Heart Association (AHA), the American Association of Clinical Endocrinologists (AACE), and the National Institute for Health and Care Excellence (NICE) have recommended multicomponent perioperative care that includes increased physical activity for patients undergoing bariatric procedures [3–6].
Research has shown that increased physical activity can improve cardiorespiratory fitness in non-bariatric patients [7]. Cardiorespiratory improvements could result in substantial health benefits since low cardiorespiratory fitness is associated with cardiovascular disease and mortality [8]. Although previous studies have demonstrated associations of increases in physical activity with weight loss and cardiorespiratory fitness after bariatric surgery, these studies only focused on exercise interventions and short-term outcomes [9, 10]. As a result, the relationship between physical activity and cardiorespiratory fitness remains unclear in a bariatric population undergoing perioperative care focusing on long-term lifestyle change.
The aim of this study was to assess changes in physical activity (work, leisure, and sport), weight loss and cardiorespiratory fitness up to 24 months postoperative and to analyze the relationships between change in physical activity and weight loss, and between change in physical activity and change in cardiorespiratory fitness in a large group of bariatric patients undergoing perioperative care focusing on long-term lifestyle change.
Methods
Study Population
Twenty-four-month follow-up data was collected retrospectively from patients who underwent primary Roux-en-Y gastric bypass (91%, n = 4359) or sleeve gastrectomy (9%, n = 426) surgery between January 2012 and December 2014 and combined their procedure with a structured group counseling bariatric care program. Those patients who were unable to integrate into group sessions (e.g., non-Dutch speakers) were offered an individual care program as an alternative and are not included in this study.
Pre- and Postoperative Care
Eight Dutch bariatric care centers involved in this study delivered identical pre- and postoperative care programs to patients undergoing surgery for morbid obesity. Treatment consisted primarily of a bariatric procedure integrated into an intensive lifestyle change program. The program focused on developing a new healthy lifestyle, of which physical activity is an essential element. Treatment was provided by a multidisciplinary team consisting of a bariatric physician, dietitian, psychologist, physiotherapist, internist, and surgeon. All measurements (e.g., weight, Baecke physical activity questionnaire, Åstrand bicycle tests, and other data) were assessed at the treatment centers.
After screening, patients were enrolled in treatment groups of eight individuals and began the preoperative care program where they participated in group visits on a weekly basis for 7 weeks. The goal of this stage was to educate patients about healthy eating habits, physically active behavior, and to encourage patients to become intrinsically motivated for lifestyle changes. After surgery, patients began the 15-month lifestyle change program, during which patients had group visits every 3 weeks. Group visits throughout both the preoperative and postoperative stage consisted of three consecutive 1-h sessions with a psychologist, dietician, and physiotherapist respectively. The goal of the 15-month lifestyle change program was for the patients to adopt a new independent healthy lifestyle, without the support of the bariatric care team. Additionally, patients had an individual medical check with the bariatric physician at 2 weeks and every 3 months postoperative, up to 15 months.
Although patients were not subjected to a specific physical activity regimen during the program, they were educated about moderate-intensity daily physical activity, aerobic training, and muscle-strengthening according to the recommendations of the World Health Organization 2011 guidelines for physical activity [11]. In addition, patients were coached on SMART (Specific, Measurable, Assignable, Realistic, and Time-related) goal setting and were trained to recognize and cope with body signals like pain, exhaustion, and fatigue [12]. Furthermore, patients were encouraged to pursue individually preferred physical activities to enhance long-term intrinsic motivation.
After the 15-month lifestyle change program, patients visited the clinic annually up to 5 years postoperatively for follow-up measurements, medical health checks, and additional individual patient-specific support if needed. Data were directly uploaded into an electronic medical record using an automated error detection system to flag grossly incorrect data for review and to minimize human error.
Weight Loss and Other Anthropometric Parameters
Body weight was assessed preoperatively and 3, 6, 9, 12, 15, and 24 months postoperatively. Weight loss was reported as percent total weight loss (%TWL), percent excess weight loss (%EWL), and change in body mass index (Δ BMI, kg/m2) as stated in the guidelines developed by Brethauer et al. [13]. Fat mass and fat percentage were measured by a bioelectrical impedance analysis (TANITA®), a valid method to determine body composition in obese populations [14]. Sex, age, and height were registered at baseline.
Physical Activity
Physical activity was assessed preoperatively and 9, 15, and 24 months postoperatively with the Baecke questionnaire [15]. The Baecke questionnaire has been used frequently within studies of the bariatric population [16]. Designed as a 5-point Likert scale, the questionnaire consists of 18 inquiries regarding the amount of time subjects spent on several physical activities. Outcome is expressed in three main subscales: leisure, work, and sport activity. Each subscale reports an index score between 1 and 5, in which a higher score means a higher level of physical activity.
Cardiorespiratory Fitness
Cardiorespiratory fitness was assessed preoperatively and 9, 15, and 24 months postoperatively. VO2max is widely accepted as the best measure for cardiorespiratory fitness, representing the highest amount of oxygen an individual can take in and utilize to produce ATP aerobically while breathing air during heavy exercise [17, 18]. Although generally measured by a maximal exercise test, to avoid medical risks within the morbidly obese population the submaximal Åstrand test (considered a reliable and valid method) was performed to assess VO2max [19]. During the Åstrand test, participants cycled for 6 min on a cycle ergometer on submaximal level. After the test, VO2max was calculated by combining the patient’s characteristics (age, sex, weight, and fat-free mass) with outcomes of the Åstrand test (level of resistance and heart rate) [20]. Due to equipment limitations, the Åstrand test could not be performed if patients weighed more than 182 kg, or if patients consumed beta blockers or tricyclic antidepressants due to their influence on heart rate. Additionally, some patients were unable to test because of joint problems. Furthermore, the test was discontinued if participants were not able to keep a speed of 50 rpm, or when the patient’s heart rate was insufficient (< 120 or > 170 beats per minute).
Besides as an absolute measure, VO2max can also be expressed as VO2max relative to weight or relative to fat-free mass (FFM). Since FFM and not body weight is the preferred co-variate for comparing different body size and body composition, VO2max relative to fat-free mass (VO2max/FFM) was used in the analysis as a measure for cardiorespiratory fitness [21]. This measure best represents the patient’s cardiorespiratory fitness, especially in a bariatric population that changes in body composition, because oxygen is mainly absorbed by muscles and bones and less by fat mass. VO2max/FFM was calculated as milliliters oxygen, per kilogram fat-free mass, per minute (ml/kg FFM/min). Additionally VO2max/FFM data was separated by sex for comparison to Dutch population reference values [20].
Statistical Analysis
Statistical analyses were performed using SPSS 23. All continuous variables were visually inspected and tested for normality by the Shapiro-Wilk test. Patients’ characteristics that followed a normal distribution were defined by the mean and standard deviation. Qualitative variables were defined by the number and percentage of cases. Descriptive statistics summarized the patient’s characteristics. Each score per follow-up month was compared to baseline using a paired sample t test. In addition, new variables were created to express change between baseline and 24 months: 24 m Δ leisure activity, 24 m Δ work activity, 24 m Δ sport activity, 24 m Δ BMI, and 24 m Δ VO2max/FFM. Furthermore, 24 m %TWL and 24 m %EWL were calculated. Multiple regression analysis was performed with change in physical activity (Δ leisure activity, Δ work activity, and Δ sport activity) as independent variables and 24 m %TWL and 24 m Δ VO2max/FFM as dependent variables. %TWL was chosen as a representative measure of weight loss, since %TWL is not biased by baseline BMI in the way %EWL can be [22]. Multiple regression analysis adjusted for baseline BMI, age, and sex.
Results
Study Population
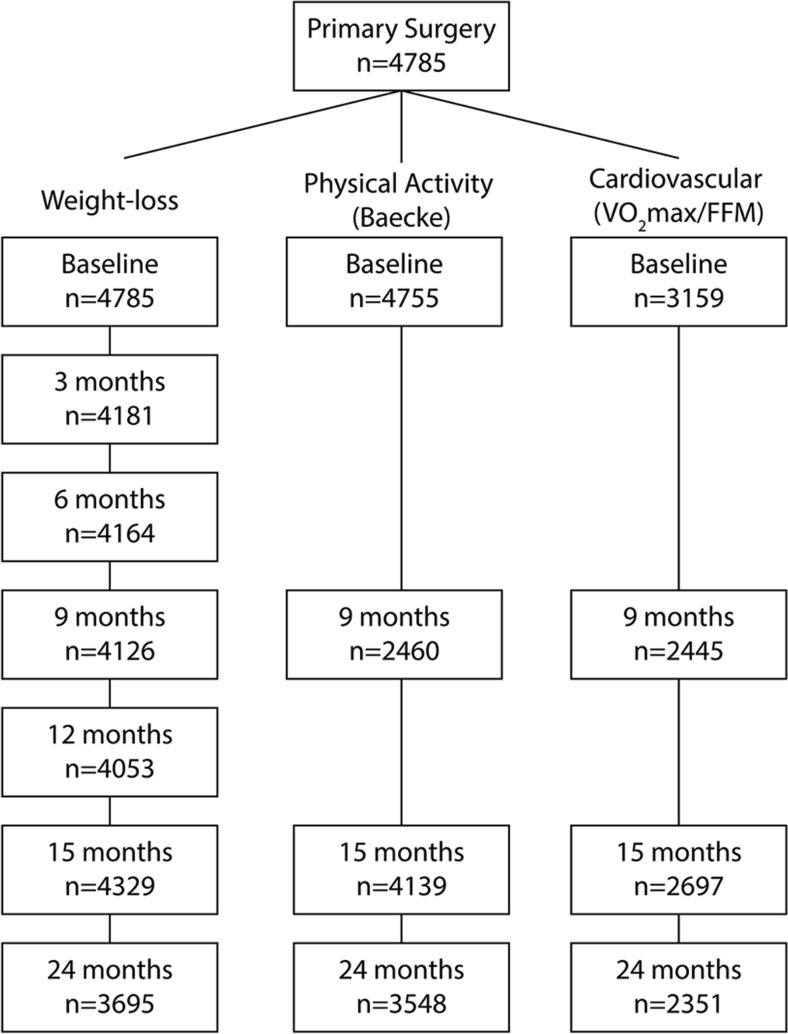
The study sample consisted of 4785 patients who underwent primary bariatric surgery with a mean age of 43.1 ± 10.7 years, a mean BMI of 44.9 ± 6.2 kg/m2 of which 81% were female (Table 1). In 3695 (77%) of the included patients, weight loss data was available at 24 months (Fig. 1). At 24 months, postoperative data was available for the Baecke questionnaire in 3548 (74%) of patients and for the VO2max/FFM scores in 2351 (49%) of patients (Fig. 1). The lower availability of VO2max/FFM data was due largely to the Åstrand test exclusion criteria (> 182 kg, beta blockers or tricyclic antidepressants, joint problems, and insufficient heartrate (< 120 or > 170)). The median overall compliance of the group sessions (pre- and postoperative) was 70%, with an interquartile range of 60 to 79%.
Table 1.
Baseline characteristics of the included study population
| Total (n = 4785) | Mean ± SD | Percentage (n) |
|---|---|---|
| Age (years) | 43.2 ± 10.7 | |
| Female | 81% (3867) | |
| BMI (kg/m2) | 44.9 ± 6.2 | |
| Height (cm) | 169.8 ± 8.9 | |
| Weight (kg) | 129.7 ± 22 |
BMI, body mass index
Fig. 1.
Flow chart of participant follow-up
Physical Activity
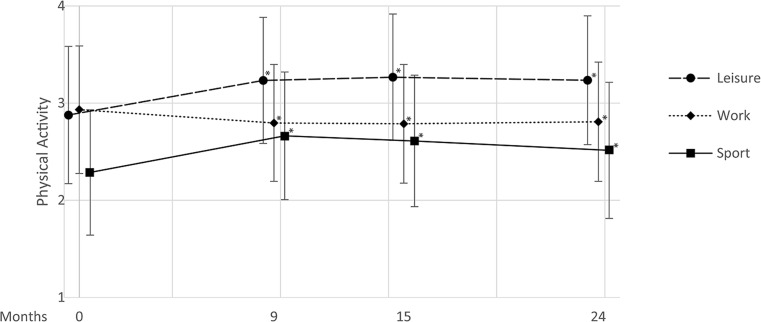
Baecke questionnaire outcomes showed significant increases in leisure and sport activity at 24 months postoperative compared to baseline (2.88 ± 0.71 vs. 3.23 ± 0.66, P < 0.001 and 2.29 ± 0.64 vs. 2.51 ± 0.70, P < 0.001, respectively). Furthermore, a small but significant decrease was seen in the work component at 24 months compared to baseline (2.93 ± 0.66 vs. 2.81 ± 0.61, P < 0.001). In all cases, significant changes were also seen at earlier 9 and 15 months points when compared to baseline (Fig. 2).
Fig. 2.
Baseline and follow-up mean (± standard deviation) physical activity scores of Baecke leisure, work, and sport subscales for the entire study population. *P < 0.001 compared to respective baseline; n = 2452, 4118, and 3535 at 9, 15, and 24 months, respectively
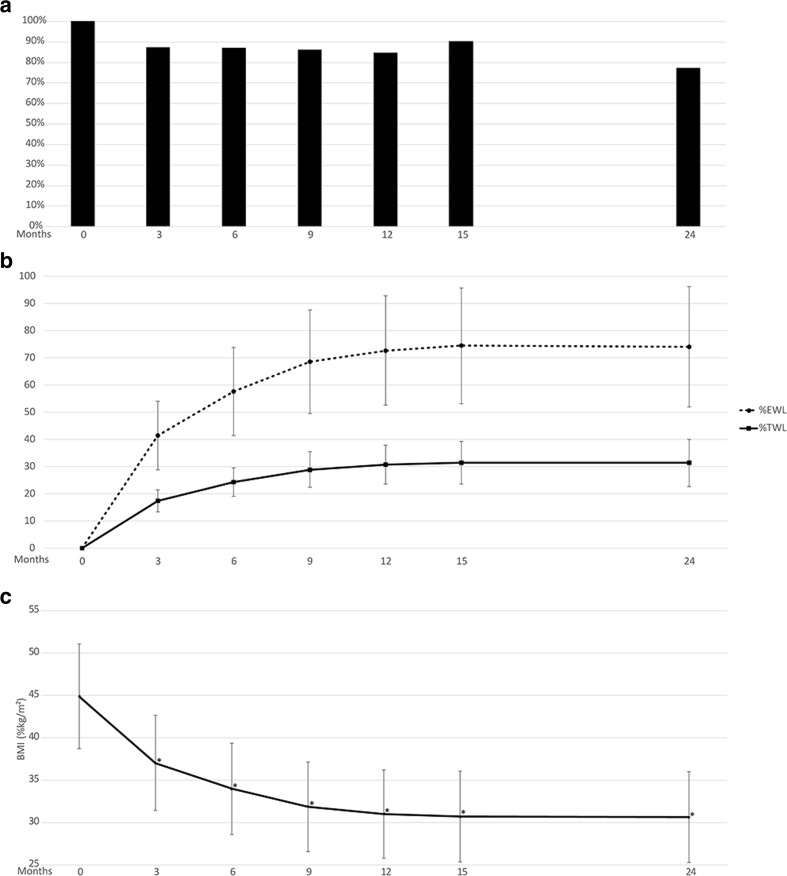
Weight Loss
At the completion of 22 session care program visits within the first 15 months, postoperative patient retention was 91% with a mean TWL of 31.5% (Fig. 3a, b). Follow-up rate at 24 months was 77% with a mean EWL of 74.0% and mean TWL of 31.3% (Fig. 3a, b). Significantly reduced BMI was also reported at each follow-up month throughout the 24 months when compared to baseline (Fig. 3c).
Fig. 3.
a Patient retention for weight loss assessment through 24 months postoperative. b %EWL and %TWL through 24 months postoperative. c BMI (BMI, kg/m2) through 24 months postoperative. *P < 0.001 compared to respective baseline
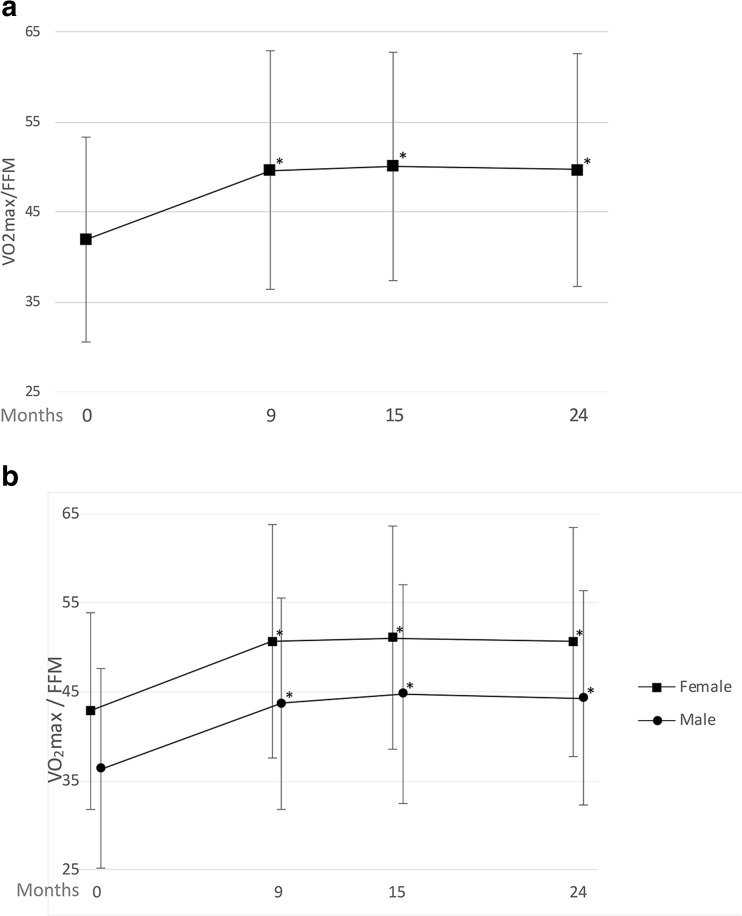
Cardiorespiratory Fitness
Åstrand bicycle test outcomes showed significant increase of mean absolute VO2max between baseline and 24 months follow-up (3.05 ± 0.79 vs. 3.25 ± 0.88, P < 0.001). Cardiorespiratory fitness, VO2max/FFM, also improved significantly throughout the study with an increase from 41.94 ± 11.32 at baseline to 49.67 ± 12.95 at 24-months (P < 0.001). Significant improvement in VO2max/FFM was also seen at each follow-up month throughout the 24 months when compared to baseline (Fig. 4a). When separated by sex, male patients showed a lower cardiorespiratory fitness through the 24-month period, although the overall change between baseline and 24 months was similar when comparing males and females in both groups (Fig. 4b). For both males and females, VO2max/FFM at 9, 15, and 24 months showed significant increases when compared to their respective baselines.
Fig. 4.
a Baseline and follow-up mean (± standard deviation) Åstrand bicycle test outcomes, showing VO2Max/FFM (ml/kg FFM/min). *P < 0.001 compared to baseline; n = 1900, 2072, and 1825 at 9, 15, and 24 months respectively. b VO2Max/FFM from females (81%) and males (19%). *P < 0.001 compared to respective baseline
Association of Physical Activity with Weight Loss and Cardiorespiratory Fitness
Change in leisure activity at 24 months was positively associated with %TWL at 24 months (P < 0.001, Table 2), thus patients who had higher improvements in leisure activity had better weight loss. No significant associations of change in sport and work activity were found with %TWL however.
Table 2.
Multiple regression analyses of change in physical activity relating to %TWL and change in VO2max/FFM
| Independent variable | Dependent variable | N | ß | 95% CI | p value | R 2 | |
|---|---|---|---|---|---|---|---|
| Lower | Upper | ||||||
| Δ sport Δ leisure Δ work |
24 m %TWL | 3484 | > .05 | ||||
| 24 m %TWL | 3484 | 1.352 | .912 | 1.792 | < .001 | .054 | |
| 24 m %TWL | 3484 | > .05 | |||||
| Δ sport Δ leisure Δ work |
24 m Δ VO2max/FFM | 1743 | 1.730 | 1.039 | 2.420 | < .001 | .070 |
| 24 m Δ VO2max/FFM | 1743 | > .05 | |||||
| 24 m Δ VO2max/FFM | 1743 | > .05 | |||||
24 m %TWL, percentage total weight loss at 24-month follow-up
24 m Δ VO2max/FFM, change in VO2max relative to fat-free mass (ml/kg FFM/min) at 24-month follow-up
Multiple regression analysis was adjusted for baseline BMI, age, and sex
Change in sport activity at 24 months was positively associated with change in VO2max/FFM at 24 months (P < 0.001, Table 2), thus patients who had higher improvements in sport activity had better cardiorespiratory fitness improvements. No significant associations of change in leisure and work activity with change in VO2max/FFM were identified.
Discussion
The aim of this study was to assess changes in physical activity, weight loss, and cardiorespiratory fitness after bariatric surgery complemented by a perioperative lifestyle change program and to evaluate the association of changes in physical activity with weight loss and change in cardiorespiratory fitness. Results showed significant postoperative improvement in physical activity, weight loss, and cardiorespiratory fitness. In addition, positive associations were found between change in sport activity and change in cardiorespiratory fitness, but not weight loss. While on the other hand, positive associations were found between change in leisure activity and weight loss, but not change in cardiorespiratory fitness.
A positive aspect of this study is the robustness of the sample, resulting in large statistical power. However, this also increases the chance on finding significant effects that may not be clinically relevant. Nevertheless, the observed improvements in health outcomes from preoperative to 2 years postoperative have a substantial impact on the patient’s life. For example, the EWL of 74% reported in this study is higher than the weight loss results seen in the systematic review of bariatric clinical studies by Puzziferri et al. in 2014 [23]. Furthermore, improvements in VO2max are associated with lower risks of all-cause and cardiovascular mortality [24]. In this study, cardiorespiratory fitness as measured by VO2max relative to fat-free mass improved by 18.4% compared to pre-surgery measures (41.94 to 49.67 respectively), reflecting a substantial improvement. In comparison, most training studies (3–12 months) in patients achieve improvements of less than 10–15% [25].
To better understand the clinical relevance of the improvement in cardiorespiratory fitness, Dutch VO2max/FFM reference values of a healthy trained and a healthy untrained male and female population were evaluated [20]. When compared to these values, male patients showed a much lower VO2max/FFM at baseline as well as at 24 months (36.4 and 44.3, respectively) than the trained or untrained healthy male population (48.5 and 55.2, respectively). In contrast, female patients showed just a slightly lower VO2max/FFM at baseline than the untrained healthy female population and at 24 months their VO2max/FFM was almost as high as the trained healthy female population (female patients at baseline and 24 months, 42.9 and 50.7, respectively; healthy untrained and healthy trained female population, 44.0 and 52.7, respectively). Although VO2max/FFM between male and female patients was different, both showed similar improvements of 7.9 and 7.8 ml/kg FFM/min, respectively. These improvements between baseline and 24 months in VO2max/FFM are similar to the differences between the healthy untrained and healthy trained Dutch populations for both men and women (6.7 and 8.7 ml/kg FFM/min, respectively), indicating a clinically relevant level of cardiorespiratory fitness improvement.
It is not completely clear why the male patients have lower cardiorespiratory fitness than the female patients, both at baseline and postoperative. A higher BMI and more comorbidities in male patients pre- and postoperative may explain the lower cardiorespiratory fitness in men compared to women. The low preoperative VO2max in male patients indicates that male patients specifically may benefit from an improvement in VO2max, as low VO2max is associated with cardiovascular disease and strongly predicts one’s risk of dying from heart attack or stroke [26, 27].
The positive association of change in sport activity with change in cardiorespiratory fitness and not with weight loss, and change in leisure activity with weight loss and not with change in cardiorespiratory fitness, may be explained by the nature of the activities. Since sport requires a relatively high level of activity and leisure activity occurs relatively frequent, activity in sport might be more likely to increase cardiorespiratory fitness, while the more frequent leisure activity might help burn more calories over a long-time period, resulting in higher weight loss.
The results of this study demonstrate that bariatric surgery complemented by a comprehensive pre- and postoperative bariatric care program have the potential to increase physical activity, weight loss, and cardiorespiratory fitness. As previous studies have shown, this can reduce cardiovascular diseases and mortality as well as potentially decrease health care costs [8, 28]. Therefore, this treatment might have substantial beneficial consequences for the patients involved. Furthermore, the associations of physical activity with cardiorespiratory fitness and weight loss that were found suggest that practitioners could influence the patient’s outcome by stimulating sport and leisure activity. Recognition of these factors could aid in tailoring an intensive support program to improve clinical results.
Our analysis was limited by the availability of VO2max/FFM data, which was lower than that of Baecke and weight loss data. This was largely due to the exclusion criteria of the Åstrand test (> 182 kg, beta blockers or tricyclic antidepressants, joint or knee problems, insufficient heartrate during test). Since the absolute number of patients with available VO2max/FFM data was more than adequate, the association of change in physical activity with change in VO2max/FFM could still be demonstrated. For patients who are unable to complete an Åstrand test (e.g., not able to ride a stationary bicycle or weigh > 182 kg), we recommend considering the Bruce Protocol as an alternative instrument to measure VO2max [29, 30]. Additionally, although the Baecke is a self-reported questionnaire and may suffer from over- or underreporting, due to the retrospective design in this study, we think that these influences would minimally affect the overall scores. Moreover, if any bias occurred, we expect it to affect both preoperative and postoperative measures and therefore have minimal influence on Baecke change scores. However, future studies may wish to include quantifiable measures of physical activity to obtain more insight into physical activity patterns. Finally, there are differences in ability to improve VO2max/FFM between patients. For example, lower weight individuals may be able to improve less than overweight individuals, resulting in smaller but still substantial improvements. Additional research to assess these groups could provide insight into treatments based on the severity of individual weight.
Conclusion
In conclusion, this study demonstrated significant increase in physical activity, weight loss, and cardiorespiratory fitness after bariatric surgery complemented by a comprehensive pre- and postoperative lifestyle change program. Furthermore, improvement in sport activity was associated with improvement in cardiorespiratory fitness and improvement in leisure activity was associated with higher weight loss. By incorporating physical activity, bariatric programs could enhance weight loss and cardiorespiratory fitness to potentially reduce cardiovascular disease, mortality, and health care costs.
Acknowledgements
The authors would like to thank Nicholas Paquette (Medtronic) for the medical writing support, Lian Roovers for the assistance with data-analysis, and the multidisciplinary teams for providing the data.
Conflict of Interest
The authors report non-financial support from Medtronic during the conduct of the study; and Medtronic currently owns a 51% share in the Nederlandse Obesitas Kliniek (Dutch Obesity Clinic).
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Contributor Information
Onno M. Tettero, Email: otettero@obesitaskliniek.nl
Tianna Aronson, Email: tianna.d.aronson@medtronic.com.
Rens J. Wolf, Email: rwolf@obesitaskliniek.nl
Malou A. H. Nuijten, Email: malou.nuijten@radboudumc.nl
Maria T. E. Hopman, Email: maria.hopman@radboudumc.nl
Ignace M. C. Janssen, Email: ijanssen@obesitaskliniek.nl
References
- 1.Van Gaal LF, Mertens IL, De Block CE. Mechanisms linking obesity with cardiovascular disease. Nature. 2006;444(7121):875–880. doi: 10.1038/nature05487. [DOI] [PubMed] [Google Scholar]
- 2.Sjostrom L. Review of the key results from the Swedish Obese Subjects (SOS) trial - a prospective controlled intervention study of bariatric surgery. J Intern Med. 2013;273(3):219–234. doi: 10.1111/joim.12012. [DOI] [PubMed] [Google Scholar]
- 3.Mechanick JI, et al. Clinical practice guidelines for the perioperative nutritional, metabolic, and nonsurgical support of the bariatric surgery patient--2013 update: cosponsored by American Association of Clinical Endocrinologists, the Obesity Society, and American Society for Metabolic & Bariatric Surgery. Surg Obes Relat Dis. 2013;9(2):159–191. doi: 10.1016/j.soard.2012.12.010. [DOI] [PubMed] [Google Scholar]
- 4.Jensen MD, et al. 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. J Am Coll Cardiol. 2014;63(25 Pt B):2985–3023. doi: 10.1016/j.jacc.2013.11.004. [DOI] [PubMed] [Google Scholar]
- 5.Garvey WT, Mechanick JI, Brett EM, Garber AJ, Hurley DL, Jastreboff AM, Nadolsky K, Pessah-Pollack R, Plodkowski R, Reviewers of the AACE/ACE Obesity Clinical Practice Guidelines American Association of Clinical Endocrinologists and American College of Endocrinology comprehensive clinical practice guidelines for medical care of patients with obesity. Endocr Pract. 2016;22(Suppl 3):1–203. doi: 10.4158/EP161365.GL. [DOI] [PubMed] [Google Scholar]
- 6.National Institute for Health and Clinical Excellence (NICE), Obesity prevention (Clinical guideline CG43). 2006. Available from: https://www.nice.org.uk/guidance/cg43. [PubMed]
- 7.Lin X, et al. Effects of exercise training on cardiorespiratory fitness and biomarkers of cardiometabolic health: a systematic review and meta-analysis of randomized controlled trials. J Am Heart Assoc. 2015. 4(7). [DOI] [PMC free article] [PubMed]
- 8.Blair SN, Morris JN. Healthy hearts--and the universal benefits of being physically active: physical activity and health. Ann Epidemiol. 2009;19(4):253–256. doi: 10.1016/j.annepidem.2009.01.019. [DOI] [PubMed] [Google Scholar]
- 9.Woodlief TL, Carnero EA, Standley RA, Distefano G, Anthony SJ, Dubis GS, Jakicic JM, Houmard JA, Coen PM, Goodpaster BH. Dose response of exercise training following Roux-en-Y gastric bypass surgery: a randomized trial. Obesity (Silver Spring) 2015;23(12):2454–2461. doi: 10.1002/oby.21332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Herring LY, Stevinson C, Carter P, Biddle SJH, Bowrey D, Sutton C, Davies MJ. The effects of supervised exercise training 12-24 months after bariatric surgery on physical function and body composition: a randomised controlled trial. Int J Obes. 2017;41(6):909–916. doi: 10.1038/ijo.2017.60. [DOI] [PubMed] [Google Scholar]
- 11.In global recommendations on physical activity for health. 2010: Geneva. [PubMed]
- 12.Frey BS, Osterloh M. Successful management by motivation: balancing intrinsic and extrinsic incentives. Berlin: Springer; 2001. [Google Scholar]
- 13.Brethauer SA, et al. Standardized outcomes reporting in metabolic and bariatric surgery. Obes Surg. 2015;25(4):587–606. doi: 10.1007/s11695-015-1645-3. [DOI] [PubMed] [Google Scholar]
- 14.Lloret Linares C, Ciangura C, Bouillot JL, Coupaye M, Declèves X, Poitou C, Basdevant A, Oppert JM. Validity of leg-to-leg bioelectrical impedance analysis to estimate body fat in obesity. Obes Surg. 2011;21(7):917–923. doi: 10.1007/s11695-010-0296-7. [DOI] [PubMed] [Google Scholar]
- 15.Baecke JA, Burema J, Frijters JE. A short questionnaire for the measurement of habitual physical activity in epidemiological studies. Am J Clin Nutr. 1982;36(5):936–942. doi: 10.1093/ajcn/36.5.936. [DOI] [PubMed] [Google Scholar]
- 16.Livhits M, Mercado C, Yermilov I, Parikh JA, Dutson E, Mehran A, Ko CY, Gibbons MM. Exercise following bariatric surgery: systematic review. Obes Surg. 2010;20(5):657–665. doi: 10.1007/s11695-010-0096-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Montes J, Wulf G, Navalta JW. Maximal aerobic capacity can be increased by enhancing performers’ expectancies. J Sports Med Phys Fitness. 2018;58(5):744–9 [DOI] [PubMed]
- 18.Plowman S, Smith D. Exercise physiology for health, fitness, and performance. Philadelphia: Lippincott Williams & Wilkins; 2007. [Google Scholar]
- 19.Macsween A. The reliability and validity of the Astrand nomogram and linear extrapolation for deriving VO2max from submaximal exercise data. J Sports Med Phys Fitness. 2001;41(3):312–317. [PubMed] [Google Scholar]
- 20.Vos JA, Ergometrie en trainingsbegeleiding. Stichting Wetenschap en Scholing Fysiotherapie (S.W.S.F.). 1994.
- 21.Goran M, Fields DA, Hunter GR, Herd SL, Weinsier RL. Total body fat does not influence maximal aerobic capacity. Int J Obes Relat Metab Disord. 2000;24(7):841–848. doi: 10.1038/sj.ijo.0801241. [DOI] [PubMed] [Google Scholar]
- 22.van de Laar A, de Caluwe L, Dillemans B. Relative outcome measures for bariatric surgery. Evidence against excess weight loss and excess body mass index loss from a series of laparoscopic Roux-en-Y gastric bypass patients. Obes Surg. 2011;21(6):763–767. doi: 10.1007/s11695-010-0347-0. [DOI] [PubMed] [Google Scholar]
- 23.Puzziferri N, Roshek TB, III, Mayo HG, Gallagher R, Belle SH, Livingston EH. Long-term follow-up after bariatric surgery: a systematic review. JAMA. 2014;312(9):934–942. doi: 10.1001/jama.2014.10706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Swank AM, Horton J, Fleg JL, Fonarow GC, Keteyian S, Goldberg L, Wolfel G, Handberg EM, Bensimhon D, Illiou MC, Vest M, Ewald G, Blackburn G, Leifer E, Cooper L, Kraus WE, and for the HF-ACTION Investigators Modest increase in peak VO2 is related to better clinical outcomes in chronic heart failure patients: results from heart failure and a controlled trial to investigate outcomes of exercise training. Circ Heart Fail. 2012;5(5):579–585. doi: 10.1161/CIRCHEARTFAILURE.111.965186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hartman Yvonne A. W., Hopman Maria T. E., Schreuder Tim H., Verheggen Rebecca J. H. M., Scholten Ralph R., Oudegeest-Sander Madelijn H., Poelkens Fleur, Maiorana Andrew J., Naylor Louise H., Willems Peter H., Tack Cees J., Thijssen Dick H. J., Green Daniel J. Improvements in fitness are not obligatory for exercise training-induced improvements in CV risk factors. Physiological Reports. 2018;6(4):e13595. doi: 10.14814/phy2.13595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Harber MP, Kaminsky LA, Arena R, Blair SN, Franklin BA, Myers J, Ross R. Impact of cardiorespiratory fitness on all-cause and disease-specific mortality: advances since 2009. Prog Cardiovasc Dis. 2017;60(1):11–20. doi: 10.1016/j.pcad.2017.03.001. [DOI] [PubMed] [Google Scholar]
- 27.Ramos PS, Araujo CG. Cardiorespiratory optimal point during exercise testing as a predictor of all-cause mortality. Rev Port Cardiol. 2017;36(4):261–269. doi: 10.1016/j.repc.2016.09.017. [DOI] [PubMed] [Google Scholar]
- 28.Andreyeva T, Sturm R, Ringel JS. Moderate and severe obesity have large differences in health care costs. Obes Res. 2004;12(12):1936–1943. doi: 10.1038/oby.2004.243. [DOI] [PubMed] [Google Scholar]
- 29.Bruce RA, Lovejoy FW, Jr, Pearson R, Yu PNG, Brothers GB, Velasquez T. Normal respiratory and circulatory pathways of adaptation in exercise. J Clin Invest. 1949;28(6 Pt 2):1423–1430. doi: 10.1172/JCI102207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bruce RA, Pearson R, Lovejoy FW, Jr, Yu PNG, Brothers GB. Variability of respiratory and circulatory performance during standardized exercise. J Clin Invest. 1949;28(6 Pt 2):1431–1438. doi: 10.1172/JCI102208. [DOI] [PMC free article] [PubMed] [Google Scholar]