Abstract
Background
In this study, we examined the implementation and efficacy of Operation Change, a community-based, culturally sensitive program to stimulate behavioral changes in activity level and improve musculoskeletal health in African-American (AA) and Hispanic/Latina (H/L) women with obesity and early-stage osteoarthritis.
Methods
Sixty-two women (32 AA and 30 H/L), 40–75 years old, with nontraumatic knee pain and body mass index values > 30, participated in a 12-week program of presentations, motivational interviewing, goal setting, and physical activities. Assessments (at 0, 6, and 12 weeks) included a demographic questionnaire, physical assessment, timed 50-ft walking test, Western Ontario and McMaster Universities Arthritis Index (WOMAC), Short Form-36 Health Survey (SF-36), 8-Item Physical Health Questionnaire (PHQ-8), and motivational interview assessment.
Results
Walking time improved significantly for H/L women (P < 0.0001) but not AA women (P = 0.0759). Both groups had significant mean weight loss (P < 0.05) with high variability among individuals. WOMAC scores for both groups indicated decreased pain (P < 0.0001) and stiffness (P < 0.0001) and improved physical functioning (P < 0.0001) by 12 weeks. SF-36 results were comparable to those of the WOMAC. PHQ-8 results improved significantly for H/L women (P < 0.0001) but not AA women (P = 0.077). Participants scored the motivational interviewing component of the program favorably.
Conclusions
Participation in Operation Change increased physical activity, resulting in improvements in pain and function scores. This supports a new paradigm for behavioral modification that helps AA and H/L women take an active role in living with osteoarthritis.
Keywords: Behavioral change program, Early-stage osteoarthritis, Knee pain, Obesity, Outcomes, Physical activity level
Introduction
In the USA, approximately 23% of adults have self-reported, physician-diagnosed arthritis; this rate is 50% for those older than 65 years [1]. Radiographic osteoarthritis (OA) is more prevalent in non-Hispanic blacks and Mexican-Americans aged 60 years or older than in corresponding non-Hispanic whites [2]. According to the Centers for Disease Control and Prevention, a greater proportion of African-Americans (AAs) and Hispanics have activity limitations, work limitations, and severe joint pain compared with non-Hispanic whites [3]. Women make up 61% of OA patients [4], and AA and Hispanic women may have an even higher risk of developing OA [5].
The natural history of OA involves a vicious cycle of joint pain and limited mobility and is associated with comorbidities such as diabetes, fatigue, depression, and obesity. Many of these factors are interrelated, exacerbating the progression of OA. Pain may limit mobility and physical activity, leading to weight gain [6, 7]. Impaired mobility is associated with pain, instability, fear of physical activity or falling, and depression [2, 8, 9]. Obesity is associated with arthritis progression, joint pain, activity limitation, disability, reduced quality of life, need for total joint replacement, and poor clinical outcomes after total joint replacement [10, 11]. The risk of obesity is higher for women than for men [12, 13], and the association between higher BMI and depressive symptoms may be stronger for AAs than for whites [14].
Physical exercise programs for patients with early-stage OA [15] can increase strength and flexibility and reduce joint pain and chronic fatigue [16, 17]. Such several programs are available through community organizations, but few have been developed specifically for underserved minorities and/or obese women.
Operation Change is a community-based (i.e., implemented in the community using community resources), culturally sensitive (i.e., designed with knowledge of patients’ culture, acceptance of cultural differences, and adaptation of interpersonal skills to work with the community [18]) program that involves education, physical activity, group sessions, and motivational interviewing conducted by individuals of identical race or ethnicity. By incorporating these features, Operation Change is a paradigm shift from traditional exercise or weight loss programs. The goal of this exploratory study was to examine the implementation and efficacy of Operation Change to stimulate behavioral changes in activity level and improve musculoskeletal health in obese AA and Hispanic/Latina (H/L) women with early-stage osteoarthritis.
Patients and Methods
Study Population
Participants were recruited from the South Side of Chicago through flyers and word-of-mouth from local referral sources. The inclusion criteria were AA and H/L women, 40–75 years of age, self-reported knee pain and/or early-stage arthritis (self-reported physician diagnosis), and body mass index (BMI) of 30–45. Subjects were excluded if they reported uncontrolled medical conditions or stage-2 hypertension or were unable to stand unsupported for 10 min. Informed consent (institutional review board-approved) was obtained at the screening visit.
Program Design
The program, conducted in 2012, took place every Saturday for 3 h over 12 weeks. The AA women met in the local Young Men’s Christian Association, and the H/L women met in a local church. Each session included 1 h each of physical activity, health-education sessions, and motivational interviewing group sessions. Light breakfast and snacks were provided. Separate individualized visits were scheduled for assessments and goal setting at baseline, 6 weeks, and 12 weeks.
Physical Activity
Certified health trainers and community health workers led the physical activities, including walking, low-impact aerobics, stretching, dancing, meditation, and yoga. Optional activity classes were offered twice a week. Participants were encouraged to engage in exercise during the week.
Education
Lectures and question-and-answer sessions were provided by allied health professionals, nurses, a nutritionist, physical trainers, and physicians. Care was taken to be culturally sensitive during selection of topics and illustrative examples. Topic selection was based on participant input and consisted of movement as medicine, living with OA, healthy eating, depression, support networks, community resources, goals for lifestyle change, and chronic diseases associated with OA and obesity. For the H/L group, guest presenters were fluent in Spanish or teamed with a translator.
Motivational Interviewing
Motivational interviewing addresses ambivalence to change by supporting and encouraging individuals to set goals to create change. Although many publications have addressed diet and weight loss, our focus was on increasing mobility. To achieve this, Operation Change used motivational interviewing, which is based on the highly validated trans-theoretical model (TTM) of behavioral change [19]. Application of TTM in Operation Change involved using motivational interviewing to conceptualize where participants are along the stages of change continuum to determine readiness for change and which type of “change talk” is needed to help them make a behavior change. Research reveals that behavioral change is significantly more achievable when patients are granted autonomy in setting their personal goals. The Operation Change program was concerned foremost that (1) participants set their own goals and (2) they work to meet those goals, identifying any potential barriers. Our motivational interviews were therefore focused on empowering individuals to make healthier decisions for themselves and to become more active participants in their own health.
Each participant was assigned a community-based layperson (Champion) and encouraged to share thoughts and personal experiences related to barriers to making behavioral changes. Several resources (i.e., SMART goals [20], My Steps Toward Change [21], and The Fishbone Tool for Root Cause Analysis [22]) were used to help participants identify strategies for change.
Weekly facilitated discussions examined influences that motivate positive behavior changes, overcoming obstacles, action plan development, community resources, and the importance of defining goals that are specific, measurable, attainable, realistic, and timely. Individualized weekly goals were established by each participant. Participants received one additional hour of individualized motivational interviewing by the Champions at baseline, 6 weeks, and 12 weeks (not during the Saturday program). Champions made weekly follow-up telephone calls to participants to support their participation.
Baseline and Follow-up Assessments
Evaluations were obtained by the study coordinators at baseline, 6 weeks, and 12 weeks (Table 1). Physical assessments included measurement of weight, height, blood pressure, and resting heart rate. The Western Ontario and McMaster Universities Arthritis Index (WOMAC-LK3.0) and Short Form-36 Health Survey (SF-36 v2; OPTUM, Inc., Eden Prairie, MN) were licensed for this study. The 8-Item Patient Health Questionnaire Depression Scale (PHQ-8) was used to assess depression. Instructed to walk as quickly as possible, participants performed a timed 50-ft walking test. A motivational interviewing discussion guide evaluated participants’ perceptions of the importance of their goals, their readiness to achieve them, and their confidence in in their ability to achieve them [23, 24].
Table 1.
Schedule of assessments during the 12-week Operation Change program
| Assessment | Baseline | Program week | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | ||
| Demographic questionnaire | X | ||||||||||||
| 8-Item Patient Health Questionnaire Depression Scale | X | X | X | ||||||||||
| Exercise log | X | X | X | X | X | X | X | X | X | X | X | X | |
| Focus groups | X | X | X | ||||||||||
| Global Pain Scale | X | X | X | ||||||||||
| List of medications | X | ||||||||||||
| Motivational interviewing | X | X | X | ||||||||||
| Physical assessmenta | X | X | X | ||||||||||
| Short Form-36 Health Survey | X | X | X | ||||||||||
| Timed 50-ft walking test | X | X | X | ||||||||||
| Western Ontario and McMaster Universities Osteoarthritis Index | X | X | X | ||||||||||
aPhysical assessment measured weight, height, blood pressure, and resting heart rate
Incentives
Participants received an Operation Change T-shirt and a pedometer, bus passes as needed, and $25 gift cards for each motivational interviewing session and completed evaluation.
Program Team
The Operation Change program team included experienced study coordinators, program assistants (Champions), and activity facilitators. The AA study coordinator was recruited by the principal investigator, and the H/L coordinator was recruited through the board of a community health workers’ organization, both located in the South Side of Chicago. Champions and activity facilitators were recruited through connections within the community, the healthcare system, and churches. Champions had to be community members or of the same race/ethnicity as the participant group. Certified health trainers and community health workers led the physical activity. H/L team members were required to have previous experience working with the H/L community and to be bilingual (Spanish/English). A faculty member from a local university instructed the Champions in motivational interviewing techniques, including using change talk and OARS (open-ended questions, affirmation, reflection, and summary statements).
Statistical Analysis
Statistical analysis was performed using JMP, version 10, software (SAS, Cary, North Carolina) and VassarStats: Website for Statistical Computation (VassarStats.net; ©Richard Lowry, 1998–2015). Parametric data were analyzed using analysis of variance for repeated measures; the Tukey honest significant difference test was performed when the analysis of variance yielded a significant F-ratio. Pre-post testing was assessed using Student’s t tests for matched pairs. Frequencies were compared using likelihood-ratio chi-square tests. Significance was accepted when P < 0.05. In response to a request from Operation Change participants, no statistical comparisons were made between the AA and H/L groups.
Results
Study Population
Ninety-two women (54 AA and 38 H/L) were screened. Twenty-two failed the screening (16 AA and 6 H/L), and 8 dropped out of the study (6 AA and 2 H/L), 1 of whom dropped out after completing 6 weeks of the program. Consequently, 62 participants (32 AA and 30 H/L) completed the 12-week program. As indicated in Table 2, mean ages were 61 years (range 41–75 years) for AA women and 52 years (range 45–66 years) for H/L women. Mean baseline BMI values were 36.6 ± 8.6 for AA women and 35.6 ± 5.6 for H/L women. Regarding weekly participation, 83% of AA and 87% of H/L women attended at least 70% of the sessions during the 12-week program (Fig. 1).
Table 2.
Demographic characteristics of 62 women participating in Operation Change
| Group | No. of participants | Mean (range) age, years | Mean ± SD BMI |
|---|---|---|---|
| African-American | 32 | 61 (41–75) | 36.6 ± 8.6 |
| Hispanic/Latina | 30 | 52 (45–66) | 35.6 ± 5.6 |
| Total | 62 | 57 (41–75) | 35.4 ± 5.0 |
| P value | NA | < 0.0001 | 0.6198 |
BMI body mass index, NA not applicable, SD standard deviation
Fig. 1.
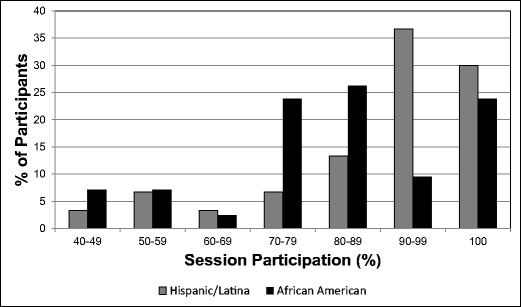
Rate of participation of African-American and Hispanic/Latina women in Operation Change. Session participation is the percentage of sessions that were attended by each participant
General Health
No significant differences were observed in blood pressure or resting heart rates during the 12-week period for the AA or H/L women. Timed 50-ft walking test results improved significantly for the H/L women (P < 0.0001) but not for the AA women (P = 0.0759). Mean weight decreased significantly at 12 weeks compared with baseline for AA (P = 0.04) and H/L (P = 0.03) women. However, considerable variability existed for both AA (range 5-kg gain to 11-kg loss) and H/L (range 3-kg gain to 7-kg loss) women (Fig. 2).
Fig. 2.
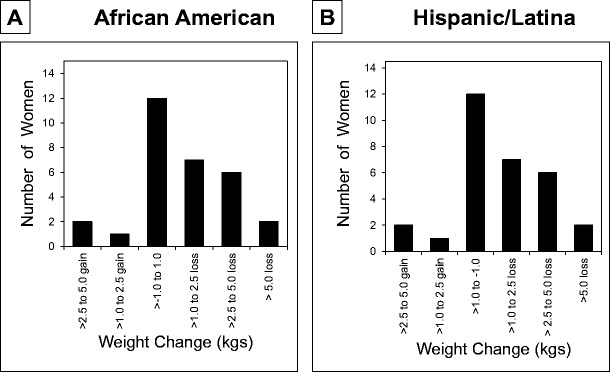
Frequency distribution of weight change in 32 African-American women and 30 Hispanic/Latina women who completed the 12-week community-based Operation Change program
Outcomes
Patient-reported outcomes were obtained at baseline, 6 weeks, and 12 weeks for all participants except 1 AA participant at 6 weeks. For the WOMAC, significant improvements in pain, stiffness, and physical functioning subscores (all P < 0.0001) were observed for both AA and H/L groups (Fig. 3) during the 12-week period. All differences in mean WOMAC scores were greater than the minimal clinically important differences for each subscore [25].
Fig. 3.
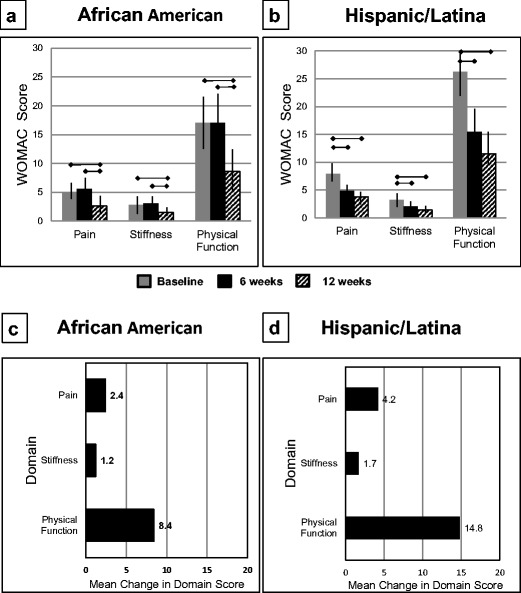
Western Ontario and McMaster Universities Arthritis Index (WOMAC) scores for the a 32 African-American women (scores unavailable at 6 weeks for one woman) and b 30 Hispanic/Latina women who participated in the Operation Change Program. The results are presented as means and 95% confidence intervals. Asterisk represents statistical significance at P < 0.05. The change in each WOMAC domain score is presented for the c African-American and d Hispanic/Latina women
At 12 weeks, AA women showed significant improvements in SF-36 subscores for physical functioning, bodily pain, and vitality (all P < 0.01). Improvements were also observed for role-physical, social functioning, and role-emotional, but these changes were not significant (Fig. 4a). There was no notable change in the general health subscore for the AA participants. H/L women showed significant improvement for all SF-36 subscores by 12 weeks (Fig. 4b), with the exception of general health (P = 0.298). All differences in mean SF-36 scores were greater than the minimal clinically important differences, except for social functioning [25, 26].
Fig. 4.
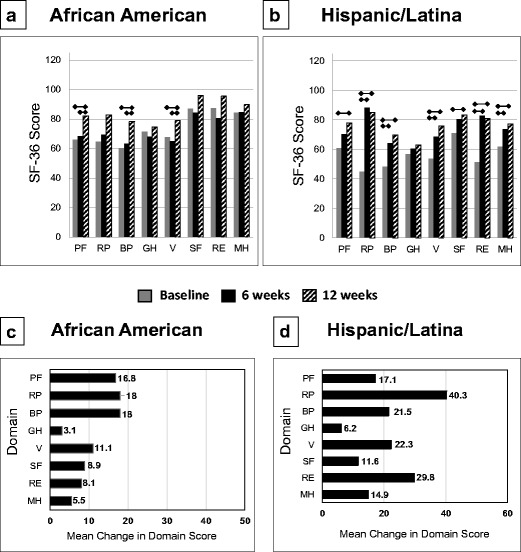
The mean Short Form-36 Health Survey scores for the a 32 African-American women (scores unavailable at 6 weeks for one woman) and b 30 Hispanic/Latina women who participated in the 12-week Operation Change program. The change in each SF-36 domain score is presented for the c African-American and d Hispanic/Latina women. The results are presented as means and 95% confidence intervals. Asterisk represents statistical significance at P < 0.05. BP bodily pain, GH general health, MH mental health, PF physical functioning, RE role emotional, RP role physical, SF social functioning, V vitality
For the AA women, there was an association between compliance (number of sessions attended) and the SF-36 BP subsection (r = 0.379, P < 0.05) and with the SF-36 Vitality subsection (r = 0.357, P < 0.05). Although there were no statistically significant associations for the H/L women, two subsections approached significance: WOMAC-stiffness (r = 0.334, P = 0.071) and SF-36 physical function (r = 0.355, P = 0.054).
AA women’s PHQ-8 scores were lower at 12 weeks than at baseline, although the difference was not significant (P = 0.077) (Fig. 5a). Many AA participants (53%) were in the range indicating no significant depression symptoms (score 0–4) for all three time periods. H/L women showed a significant decrease in PHQ-8 scores between baseline and 6 weeks and between baseline and 12 weeks (P < 0.0001) (Fig. 5b). Whereas only 27% of H/L women scored in the “no significant depressive symptoms” range at baseline, 57% scored at this level at 6 and 12 weeks.
Fig. 5.
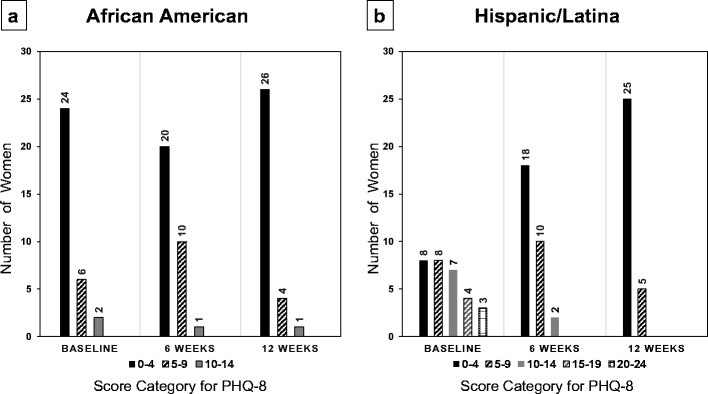
For the 8-Item Patient Health Questionnaire (PHQ-8), the frequency of each score category of a 32 African-American women (scores unavailable at 6 weeks for one woman) and b 30 Hispanic/Latina women who participated in the 12-week Operation Change program. The PHQ-8 uses the following score categories: 0–4 not significant, 5–9 mild, 10–14 moderate, 15–19 moderately severe, and 20–24 severe
Motivational Interviewing
All participants ranked as high the importance of goal setting, their readiness to set goals, and their confidence in their ability to do so. On a 10-point visual analog scale, the mean values of each component exceeded 9 points at 6 and 12 weeks.
Discussion
The Operation Change program was introduced to middle-aged and elderly AA or H/L women in two underserved communities in the South Side of Chicago and led to measurable improvements in outcomes. Using validated instruments, we observed decreases in pain and stiffness, improved physical functioning, and diminished depression in AA and H/L women with early-stage arthritis and obesity, as well as a corresponding significant but modest decrease in weight for some participants during the 12-week study period. A significant decrease in the frequency of depressive symptoms was observed, although this cannot be correlated independently with the physical activity component of the program.
Regular, moderate-intensity physical activity has been reported to decrease the severity of arthritis and its associated pain, fatigue, and stiffness [27]. Little information has been published concerning exercise among AA or H/L women with OA. Wyatt et al. [28] reported that 117 AA participants (93% women; 56% obese) who completed the Arthritis Foundation’s 6-week Walk with Ease program experienced significant decreases in pain, fatigue, and stiffness, which were maintained at 1-year follow-up. Parker et al. [29] found that pain intensity and mood scores improved significantly in AA, Hispanic, and non-Hispanic white participants with walking. The 112 participants were primarily women (83%), and although BMI and obesity status were not reported, 32% of participants were diabetic. The results of these studies agree with the experiences of the AA and H/L participants in Operation Change.
Physical activity trials indicate that 9 to 87% (mean 45%) of participants do not adhere to an intervention [30] and that high dropout rates impede maintenance of physical activity programs for populations similar to those in this study [31, 32]. Barriers include time limitations due to work-life obligations, physical and mental fatigue, depression, negative attitudes toward exercise, including fear of exercise (apprehension regarding pain or falling), and lack of role models [8, 31, 33–35]. The physical environment may present challenges because of poor safety (poor sidewalk or road conditions, inadequate or nonexistent street lights, lack of personal safety) and lack of access to healthy foods (i.e., food deserts) and the corresponding availability of unhealthy foods [12, 31, 36]. Some Operation Change participants described lack of support from spouses to lose weight, unwillingness to change eating habits, and unwillingness to exercise in a program with “thin” participants. The biggest challenge may be behavioral change itself (e.g., increasing activity level) [37]. Most adults, regardless of sex, race, or ethnicity, do not exercise, and exercise participation declines with increasing age [38].
Operation Change offers three critical elements: (1) A focus on increasing mobility rather than losing weight may make the goal appear more attainable to participants, (2) the network of support created by Operation Change can encourage success, and (3) motivational interviewing enhances behavior change. It has been used by large musculoskeletal programs [34, 39] and has been shown to help patients with fibromyalgia [27], diabetes [40], and chronic heart failure [41] to increase their physical activity by helping them overcome ambivalence about changing their behavior [27, 34, 39]. In group-based interventions, physical activity can be coupled with counseling, which includes discussion of self-regulatory skills to help establish behavioral change [42]. Operation Change is a paradigm shift from more traditional programs.
There is the possibility of the Hawthorne effect with any patient-reported outcomes assessment [43]. For example, some participants may report better results to keep the program going, whereas other participants may report worse results, at least initially, because they want to show that their situation is “worse” than that of other participants. Participants were referred to or signed up for the study on the basis of their health status or interest in improving. Although they knew they were being observed, they understood that this observation was being conducted to improve their health and that of others like them. This understanding showed in the results of the study. Participants were asked to complete evaluations of the study at three time points. There was consistency between the two measures of quality of life—the WOMAC and the SF-36. The program evaluation asked both quantitative and qualitative participant perceptions of the programs and ways to improve it. It was learned, by using these evaluations, that participants enjoyed the program tremendously and wanted it to continue.
Strengths of the program include that it was community-based (i.e., designed to be implemented and operationalized with community resources and by community members, who may or may not be associated with healthcare agencies) and that discussion topics reflected the interests of participants. The staff were of the same race or ethnicity as the participants; culturally or racially concordant care has been shown to be more satisfying and to result in positive patient outcomes [44]. A multi-strategy approach was used by Operation Change to encourage behavioral change: a variety of activities, education by physicians and trained healthcare providers, and motivational interviewing. The program overcame some of the obstacles of the built environment by providing a safe space for group physical activities.
A major challenge for the program was the shortage of highly educated professionals who work within the AA and H/L communities. In the H/L group, use of a translator was found to hinder participant engagement; we recommend having bilingual presenters. A limitation of this pilot study was that there were no control groups. This decision was made, after consultation with the community, to avoid possible treatment contamination after community participants raised concerns about the perception of unfairness (i.e., that the treatment group would be receiving “more” than the control group) and the likelihood of communication between treatment and control groups. The AA and HL groups were significantly different in age, although this occurred by chance within the established inclusion criteria. Another limitation is that there was no long-term evaluation of individual sustainability of increased activity level of this 12-week program. Other limitations are the relatively small sample size and the inclusion of some participants with knee pain but lack of physician-reported knee OA.
This study supports the feasibility and efficacy of a community-based program for AA and H/L women that encourages them to take an active role in living with arthritis and incorporates shared decision-making, cultural sensitivity, and a focus on movement and activity. Future studies should address the long-term sustainability of behavioral change regarding physical activity levels.
Acknowledgments
We thank Thomas Mason, MD, for his many contributions to the success of the Operation Change Program in Chicago, including his help with the launch of the program and the editing of the manuscript. We appreciate the efforts of the following referral sources: Laura Bahena, Estela Hernandez, MD, Arnold Johnson, Susan Laws, Christina Martinez, Kelli Medious, Rosalva Nava, Surrenthia Parker, MD, Gerrie Pate, RN, Craig Peller, MSW, Concepcion Saldivar, James Watson, MD, and Carlton West, MD. We also thank the facilitators, Laura Bahena, Erin Pearson, Concepcion Saldivar, and Genice Wedgeworth; the Champions, Angela Hall, Carmen Lewis, Christina Martinez, Rosalva Nava, Tiffany Vann, and Jocelyn Wilder; and the study coordinators, Francisco Baiocchi, Kelli Medious, Delmar Wright, Yashika Watkins, and Duanny Alva. We thank Amy Jones and Kelsey Branch for data input; Michelle Tucci for assistance in the preparation of the figures; and Rachel Box, Eileen Martin, Jenni Weems, and Zan Naseer for editorial assistance. We especially want to thank Verona Brewton for her guidance and leadership of the Operation Change Program.
Compliance with Ethical Standards
Conflict of Interest
The Operation Change Program was underwritten by a grant from Zimmer, Inc., Warsaw, IN. Dr. Watkins reports personal fees received from Zimmer Biomet. Dr. Alva and Dr. Jones report consulting fees from Zimmer Biomet.
References
- 1.Centers for Disease Control and Prevention, Prevalence of doctor-diagnosed arthritis and arthritis-attributable activity limitation—United States, 2003–2005. MMWR Morb Mortal Wkly Rep. 2006;55(40):1089–92. [PubMed]
- 2.Dillon CF, Rasch EK, Gu Q, Hirsch R. Prevalence of knee osteoarthritis in the United States: arthritis data from the Third National Health and Nutrition Examination Survey 1991-94. J Rheumatol. 2006;33(11):2271–2279. [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention Racial/ethnic differences in the prevalence and impact of doctor-diagnosed arthritis—United States, 2002. MMWR Morb Mortal Wkly Rep. 2005;54(5):119–123. [PubMed] [Google Scholar]
- 4.Theis KA, Helmick CG, Hootman JM. Arthritis burden and impact are greater among U.S. women than men: intervention opportunities. J Women's Health (2002). 2007;16(4):441–53. doi:10.1089/jwh.2007.371. [DOI] [PubMed]
- 5.Losina E, Walensky RP, Reichmann WM, Holt HL, Gerlovin H, Solomon DH, Jordan JM, Hunter DJ, Suter LG, Weinstein AM, Paltiel AD, Katz JN. Impact of obesity and knee osteoarthritis on morbidity and mortality in older Americans. Ann Intern Med. 2011;154(4):217–226. doi: 10.7326/0003-4819-154-4-201102150-00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.MacKay C, Jaglal SB, Sale J, Badley EM, Davis AM. A qualitative study of the consequences of knee symptoms: ‘It’s like you’re an athlete and you go to a couch potato’. BMJ Open. 2014;4(10):e006006. doi: 10.1136/bmjopen-2014-006006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Neogi T. The epidemiology and impact of pain in osteoarthritis. Osteoarthritis Cartil OARS Osteoarthritis Res Soc. 2013;21(9):1145–1153. doi: 10.1016/j.joca.2013.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fitzgerald GK, White DK, Piva SR. Associations for change in physical and psychological factors and treatment response following exercise in knee osteoarthritis: an exploratory study. Arthritis Care Res. 2012;64(11):1673–1680. doi: 10.1002/acr.21751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Johnson VL, Hunter DJ. The epidemiology of osteoarthritis. Best Pract Res Clin Rheumatol. 2014;28(1):5–15. doi: 10.1016/j.berh.2014.01.004. [DOI] [PubMed] [Google Scholar]
- 10.Batsis JA, Zbehlik AJ, Barre LK, Bynum J, Pidgeon D, Bartels SJ. Impact of obesity on disability, function, and physical activity: data from the osteoarthritis initiative. Scand J Rheumatol 2015:1–8. doi:10.3109/03009742.2015.1021376, 44. [DOI] [PMC free article] [PubMed]
- 11.Centers for Disease Control and Prevention. Obesity trends in adults with arthritis. Available at http://www.cdc.gov/arthritis/resources/spotlights/obesity-trends.htm. Accessed on August 13. 2015.
- 12.American College of Obstetricians and Gynecologists Committee on Health Care for Underserved Women. Committee opinion no. 591: challenges for overweight and obese women. Obstetrics and Gynecology2014.
- 13.Raghuwanshi M, Kirschner M, Xenachis C, Ediale K, Amir J. Treatment of morbid obesity in inner-city women. Obes Res. 2001;9(6):342–347. doi: 10.1038/oby.2001.44. [DOI] [PubMed] [Google Scholar]
- 14.Sachs-Ericsson N, Burns AB, Gordon KH, Eckel LA, Wonderlich SA, Crosby RD, Blazer DG. Body mass index and depressive symptoms in older adults: the moderating roles of race, sex, and socioeconomic status. Am J Geriatr Psychiatry: Off J Am Assoc Geriatr Psychiatry. 2007;15(9):815–825. doi: 10.1097/JGP.0b013e3180a725d6. [DOI] [PubMed] [Google Scholar]
- 15.Nyrop KA, Charnock BL, Martin KR, Lias J, Altpeter M, Callahan LF. Effect of a six-week walking program on work place activity limitations among adults with arthritis. Arthritis Care Res. 2011;63(12):1773–1776. doi: 10.1002/acr.20604. [DOI] [PubMed] [Google Scholar]
- 16.Uthman OA, van der Windt DA, Jordan JL, Dziedzic KS, Healey EL, Peat GM, Foster NE. Exercise for lower limb osteoarthritis: systematic review incorporating trial sequential analysis and network meta-analysis. Br J Sports Med. 2014;48(21):1579. doi: 10.1136/bjsports-2014-5555rep. [DOI] [PubMed] [Google Scholar]
- 17.Weinstein AA, Chin LM, Keyser RE, Kennedy M, Nathan SD, Woolstenhulme JG, et al. Effect of aerobic exercise training on fatigue and physical activity in patients with pulmonary arterial hypertension. Respir Med. 2013;107(5):778–784. doi: 10.1016/j.rmed.2013.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fleming M, Towey K. Delivering culturally effective health care to adolescents. Available at https://depts.washington.edu/uwleah/sites/default/files/seminarFiles/culturallyeffectivecare%20AMA%20(3).pdf. Accessed on September 28. 2017.
- 19.Konkle-Parker DJ. A motivational intervention to improve adherence to treatment of chronic disease. J Am Acad Nurse Pract. 2001;13(2):61–68. doi: 10.1111/j.1745-7599.2001.tb00219.x. [DOI] [PubMed] [Google Scholar]
- 20.O'Sullivan GA, Yonkler JA, Morgan W, Merritt AP. A field guide to designing a health communication strategy. Baltimore, MD: Johns Hopkins Bloomberg School of Public Health/Center for Communication Programs, March; 2003. [Google Scholar]
- 21.University of North Carolina School of Medicine. Living with diabetes. Making lifestyle changes to last a lifetime. Available at https://www.med.unc.edu/im/patients/files/da-summaries/diabetes-da-summary. Accessed on March 22. 2016.
- 22.Virtual Healthcare Quality Service. Fishbone diagram. Available at http://www.improhealth.org/index.php?id=83. Accessed on March 18. 2016.
- 23.Moyers TB, Martin T, Houck JM, Christopher PJ, Tonigan JS. From in-session behaviors to drinking outcomes: a causal chain for motivational interviewing. J Consult Clin Psychol. 2009;77(6):1113–1124. doi: 10.1037/a0017189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Welch G, Rose G, Ernst D. Motivational interviewing and diabetes: what is it, how is it used, and does it work? Diabetes Spectrum. 2006;19(1):5–11. doi: 10.2337/diaspect.19.1.5. [DOI] [Google Scholar]
- 25.Angst F, Aeschlimann A, Stucki G. Smallest detectable and minimal clinically important differences of rehabilitation intervention with their implications for required sample sizes using WOMAC and SF-36 quality of life measurement instruments in patients with osteoarthritis of the lower extremities. Arthritis Rheum. 2001;45(4):384–391. doi: 10.1002/1529-0131(200108)45:4<384::AID-ART352>3.0.CO;2-0. [DOI] [PubMed] [Google Scholar]
- 26.Keurentjes JC, Van Tol FR, Fiocco M, Schoones JW, Nelissen RG. Minimal clinically important differences in health-related quality of life after total hip or knee replacement: a systematic review. Bone & Joint Res. 2012;1(5):71–77. doi: 10.1302/2046-3758.15.2000065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ang D, Kesavalu R, Lydon JR, Lane KA, Bigatti S. Exercise-based motivational interviewing for female patients with fibromyalgia: a case series. Clin Rheumatol. 2007;26(11):1843–1849. doi: 10.1007/s10067-007-0587-0. [DOI] [PubMed] [Google Scholar]
- 28.Wyatt B, Mingo CA, Waterman MB, White P, Cleveland RJ, Callahan LF. Impact of the Arthritis Foundation’s walk with ease program on arthritis symptoms in African Americans. Prev Chronic Dis. 2014;11:E199. doi: 10.5888/pcd11.140147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Parker SJ, Vasquez R, Chen EK, Henderson CR, Jr, Pillemer K, Robbins L, et al. A comparison of the arthritis foundation self-help program across three race/ethnicity groups. Ethn Dis. 2011;21(4):444–450. [PMC free article] [PubMed] [Google Scholar]
- 30.Franklin BA. Program factors that influence exercise adherence: practical adherence skills for the clinical staff. In: Dishman RK, editor. Exercise adherence: its impact on public health. Champaign, IL: Human Kinetics Books; 1988. pp. 237–258. [Google Scholar]
- 31.Ingram D, Wilbur J, McDevitt J, Buchholz S. Women’s walking program for African American women: expectations and recommendations from participants as experts. Women Health. 2011;51(6):566–582. doi: 10.1080/03630242.2011.606357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Marcus BH, Williams DM, Dubbert PM, Sallis JF, King AC, Yancey AK, et al. Physical activity intervention studies: what we know and what we need to know: a scientific statement from the American Heart Association Council on Nutrition, Physical Activity, and Metabolism (Subcommittee on Physical Activity); Council on Cardiovascular Disease in the Young; and the Interdisciplinary Working Group on Quality of Care and Outcomes Research. Circulation. 2006;114(24):2739–2752. doi: 10.1161/CIRCULATIONAHA.106.179683. [DOI] [PubMed] [Google Scholar]
- 33.Callahan LF, Shreffler JH, Altpeter M, Schoster B, Hootman J, Houenou LO, Martin KR, Schwartz TA. Evaluation of group and self-directed formats of the Arthritis Foundation’s Walk With Ease Program. Arthritis Care Res. 2011;63(8):1098–1107. doi: 10.1002/acr.20490. [DOI] [PubMed] [Google Scholar]
- 34.Ehrlich-Jones L, Mallinson T, Fischer H, Bateman J, Semanik PA, Spring B, Ruderman E, Chang RW. Increasing physical activity in patients with arthritis: a tailored health promotion program. Chronic Illness. 2010;6(4):272–281. doi: 10.1177/1742395309351243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Messier SP, Loeser RF, Miller GD, Morgan TM, Rejeski WJ, Sevick MA, Ettinger WH, Pahor M, Williamson JD. Exercise and dietary weight loss in overweight and obese older adults with knee osteoarthritis: the arthritis, diet, and activity promotion trial. Arthritis Rheum. 2004;50(5):1501–1510. doi: 10.1002/art.20256. [DOI] [PubMed] [Google Scholar]
- 36.Booth KM, Pinkston MM, Poston WS. Obesity and the built environment. J Am Diet Assoc. 2005;105(5 Suppl 1):S110–S117. doi: 10.1016/j.jada.2005.02.045. [DOI] [PubMed] [Google Scholar]
- 37.Belza B, Warms C. Physical activity and exercise in women’s health. Nursing Clin North Am. 2004;39(1):181–193. doi: 10.1016/j.cnur.2003.11.011. [DOI] [PubMed] [Google Scholar]
- 38.Lee C. Factors related to the adoption of exercise among older women. J Behav Med. 1993;16(3):323–334. doi: 10.1007/BF00844763. [DOI] [PubMed] [Google Scholar]
- 39.Rosengren DB. Building motivational interviewing skills: a practitioner workbook. New York, New York: The Guilford Press; 2009. [Google Scholar]
- 40.Smith DE, Heckemeyer CM, Kratt PP, Mason DA. Motivational interviewing to improve adherence to a behavioral weight-control program for older obese women with NIDDM. A pilot study. Diabetes Care. 1997;20(1):52–54. doi: 10.2337/diacare.20.1.52. [DOI] [PubMed] [Google Scholar]
- 41.Brodie DA, Inoue A. Motivational interviewing to promote physical activity for people with chronic heart failure. J Adv Nurs. 2005;50(5):518–527. doi: 10.1111/j.1365-2648.2005.03422.x. [DOI] [PubMed] [Google Scholar]
- 42.Focht BC, Garver MJ, Devor ST, Dials J, Lucas AR, Emery CF, Hackshaw KV, Rejeski WJ. Group-mediated physical activity promotion and mobility in sedentary patients with knee osteoarthritis: results from the IMPACT-pilot trial. J Rheumatol. 2014;41(10):2068–2077. doi: 10.3899/jrheum.140054. [DOI] [PubMed] [Google Scholar]
- 43.Wolfe F, Michaud K. The Hawthorne effect, sponsored trials, and the overestimation of treatment effectiveness. J Rheumatol. 2010;37(11):2216–2220. doi: 10.3899/jrheum.100497. [DOI] [PubMed] [Google Scholar]
- 44.Cooper LA, Roter DL, Johnson RL, Ford DE, Steinwachs DM, Powe NR. Patient-centered communication, ratings of care, and concordance of patient and physician race. Ann Intern Med. 2003;139(11):907–15, E-16. [DOI] [PubMed]


