Abstract
The interest about upper airway evaluation has increased lately. Therefore, many softwares have been developed aiming to improve and facilitate the analysis of airway volume. The objective of this study was to compare two different softwares packages, Mimics and Dolphin, in their accuracy and precision in upper airway space measurements. Preoperative cone beam computed tomography scans of nine nonsyndromic patients submitted to surgically assisted rapid maxillary expansion were included in this study. The imaging exams were converted to DICOM (digital imaging and communications in medicine) files and imported to the softwares. The mean volume for the Dolphin group (G1) was 10.791 cm 3 (SD = 4.269 cm 3 ) and for the Mimics group (G2) was 10.553 cm 3 (SD = 4.564 cm 3 ). There was no statistically significant difference between the two groups ( p = 0.105).
Keywords: imaging software, CBCT, posterior airway
Upper airway (UA) evaluation can be performed through adequate imaging exams. Furthermore, those imaging exams may assist the diagnosis of respiratory problems associated with dentofacial deformities. 1 Traditionally, the UA space is evaluated by lateral cephalometric radiography. 2 However, nowadays cone beam computed tomography (CBCT) is widely used for UA evaluation due to the three-dimensional (3D) assessment of UA with high spatial resolution between the soft tissues and airway space. 3 4
As CBCT scan became fairly used in oral and maxillofacial surgery, many softwares were developed to evaluate anatomical structures in details. 5 Those software packages use digital imaging and communications in medicine (DICOM) files. 6 Moreover, many of those softwares have optional tools responsible to segment and measure the UA space. 3 Despite the evolution of the software packages in the assessment of the UA space, some aspects are very important to achieve trustworthy results, such as respiration and tongue position during the exam, mandible morphology, and definition of the anatomical limits. 7
Guijarro-Martínez and Swennen 3 performed a systematic review of UA evaluation and reported 18 softwares used for volumetric UA evaluation using CBCT scans. Among those softwares, Mimics (Materialise Interactive Medical Image Control System, Leuven, Belgium) and Dolphin (Dolphin Imaging and Management Solutions, Chatsworth, CA) were selected. Burkhard et al 8 compared Mimics software to other two softwares , OsiriX 64-bit (Bernex, Switzerland) and BrainLab (Munich, Germany), demonstrating similar UA measurements. Similarly, El and Palomo 9 presented that Dolphin and the other two different softwares had a high reliability in UA space measurements.
The aim of this study is to compare two different softwares packages, Mimics and Dolphin, in their accuracy and precision in posterior airway space measurements. According to the authors, there is no study that compares these two softwares.
Materials and Methods
This pilot study was submitted and approved by the Ethics Committee of the Dental School of Araraquara—São Paulo State University, UNESP (protocol number 0036/09). The preoperative CBCT scans of nine nonsyndromic patients submitted to surgically assisted rapid maxillary expansion were included. The imaging data were collected from records of the Diagnosis and Surgery Department, UNESP.
All patients underwent the CBCT scan in the same scanner (iCAT, Imaging Science International, Hatfield, PA). The following scanning protocol was used in obtaining all the images. The patients were placed in natural head position and instructed to make a deep inspiration and hold their breath. Also, patients were requested to maintain the tongue in the palate and to avoid swallowing during the scanning. After the exam, the DICOM files were imported into the Dolphin and Mimics softwares ( Figs. 1 and 2 ). Two groups were created according to the software used (G1: Dolphin; G2: Mimics).
Fig. 1.

3D reconstruction and demarcation of the space airway in Mimics software.
Fig. 2.

3D reconstruction and demarcation of the space airway in Dolphin software.
Each specific software tool was used to measure the UA volume. The volumetric region of interest was defined selecting a midsagittal image of the airway and determining the superior and inferior limits. Both limits were traced parallel to the Frankfurt plane. The superior limit was determined by the posterior nasal spine, and the inferior limit was determined by the most anteroinferior point of C2 ( Fig. 3 ). A single operator made all the measurements repeatedly in different moments presenting no significant differences between the periods. Statistical analysis was performed between the two groups. The data distribution was normal and paired t -test was performed considering a 95% confidence interval.
Fig. 3.
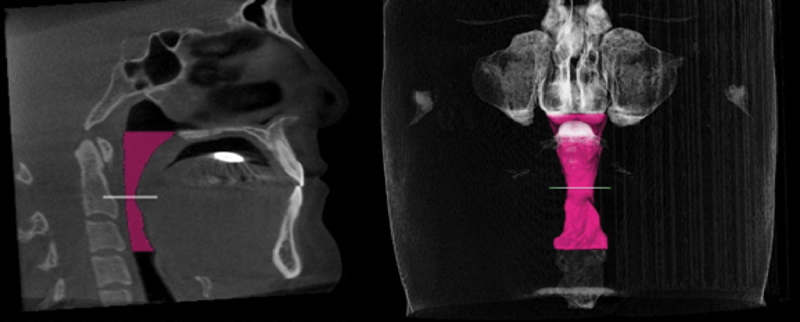
Delimitation of the area and evaluation of volume of the space airway in Dolphin software.
Results
Among the nine included patients, seven patients were female and two were male. The mean age was 32.77 years (SD = 7.31 years) ranging from 21 to 40 years. All patients had transversal deficiency of the maxilla as dentofacial deformity.
Table 1 and Fig. 4 show the measurements according to group and patient. All values were registered in cubic centimeters. The mean volume for the Dolphin group (G1) was 10.791 cm 3 (SD = 4.269 cm 3 ) and that for the Mimics group (G2) was 10.553 cm 3 (SD = 4.564 cm 3 ). There was no statistically significant difference between the two groups ( p = 0.105).
Table 1. Upper airway volume (cm 3 ) according to patient and software .
| Patient | Dolphin (G1) | Mimics (G2) |
|---|---|---|
| 1 | 16.424 | 16.332 |
| 2 | 4.788 | 4.477 |
| 3 | 6.897 | 6.317 |
| 4 | 10.631 | 10.154 |
| 5 | 17.881 | 18.554 |
| 6 | 7.388 | 6.942 |
| 7 | 10.330 | 9.881 |
| 8 | 11.597 | 11.141 |
| 9 | 11.181 | 11.180 |
| Mean | 10.791 | 10.553 |
| SD | 4.269 | 4.564 |
| Paired t -test | 0.1055 | |
Fig. 4.

Upper airway volume (cm 3 ) according to patient and software.
Discussion
Historically, UA space measurements started using lateral cephalometric radiographs; however, one of their major limitations was the restriction to two-dimensional (2D) analyses. Nowadays, CBCT is considered the gold standard exam because of its high accuracy and possibility to perform 3D measurements. 10 11 Also, this exam has become much more affordable in dentistry. 12
Although some authors have shown controversy regarding the measurements obtained from the CBCT, 13 this study corroborates to others 14 15 that already proved the accuracy of CBCT in UA space measurements. Furthermore, Cheng et al 16 presented that UA reconstruction and segmentation through CBCT's softwares is quite reliable. 14 15 16
The UA evaluation through CBCT requires some attention during image acquisition. There are some factors that may distort the results during or even before scanning, such as breathing, tongue position, and head movement. 17 Muto et al 18 stated that alterations of head and neck inclination produced by head extension were correlated with changes in the dimension of UA space. Therefore, any movement of the patient could affect the results of the imaging exam. To obtain uniform results, all scanning was performed by following a described protocol.
Another limitation about measurements of UA space is the comparison between them, regarding the calculated volumes and regions. This problem occurs due to the differences among all studies regarding the determination of UA limits. As a matter of fact, there are no standard UA limits, and even some studies do not clearly show how the UA area was determined. 3 7
Another important point for UA measurements is the way how the volume is segmented: automatic or manual. Manual segmentation may enable great control by the operator, resulting in optimal accuracy; however, it requires more operation time. 9 The sample evaluated in our study was analyzed manually. However, Ghoneima and Kula 19 measured the volume and area of an acrylic airway model using CBCT data by Dolphin software. They found no statistically significant differences between the manual and the digital measurements, thus proving the accuracy and reliability of the software for both 2D and 3D analysis.
In general, some studies use an acrylic model as a gold standard aiming to prove the reliability and accuracy of the measurements. An acrylic model consists of an air-filled plastic rectangular prism surrounded by water. This phantom has the possibility of the real measurements with a caliper and the measurements through the imaging obtained by its scan. For these reasons, this acrylic model is the perfect measurement and can be compared with the patients' exam.
With the range of softwares available in the market, they must be validated proving their accuracy and reliability between each other. Some authors 17 20 already provided reliable results using Dolphin, and others 21 using Mimics; however, the comparison between these two softwares was not done earlier. Some studies 8 9 22 compared different softwares and the results corroborate to the results of this pilot study showing no statistically significant differences between the softwares. However, further studies are required to confirm the results with a larger number of patients.
Acknowledgments
The authors thank funding agency FAPESP (Foundation for Research Support of Sao Paulo) and the Department of Diagnosis and Surgery, Dental School of Araraquara, UNESP.
Footnotes
Conflict of Interests The authors declare there was no conflict of interest.
References
- 1.Hatcher D C. Cone beam computed tomography: craniofacial and airway analysis. Dent Clin North Am. 2012;56(02):343–357. doi: 10.1016/j.cden.2012.02.002. [DOI] [PubMed] [Google Scholar]
- 2.Stratemann S, Huang J C, Maki K, Hatcher D, Miller A J. Three-dimensional analysis of the airway with cone-beam computed tomography. Am J Orthod Dentofacial Orthop. 2011;140(05):607–615. doi: 10.1016/j.ajodo.2010.12.019. [DOI] [PubMed] [Google Scholar]
- 3.Guijarro-Martínez R, Swennen G R. Cone-beam computerized tomography imaging and analysis of the upper airway: a systematic review of the literature. Int J Oral Maxillofac Surg. 2011;40(11):1227–1237. doi: 10.1016/j.ijom.2011.06.017. [DOI] [PubMed] [Google Scholar]
- 4.Lenza M G, Lenza M M, Dalstra M, Melsen B, Cattaneo P M. An analysis of different approaches to the assessment of upper airway morphology: a CBCT study. Orthod Craniofac Res. 2010;13(02):96–105. doi: 10.1111/j.1601-6343.2010.01482.x. [DOI] [PubMed] [Google Scholar]
- 5.Güldner C, Diogo I, Windfuhr J et al. Analysis of the fossa olfactoria using cone beam tomography (CBT) Acta Otolaryngol. 2011;131(01):72–78. doi: 10.3109/00016489.2010.506653. [DOI] [PubMed] [Google Scholar]
- 6.Sutthiprapaporn P, Tanimoto K, Ohtsuka M, Nagasaki T, Iida Y, Katsumata A. Positional changes of oropharyngeal structures due to gravity in the upright and supine positions. Dentomaxillofac Radiol. 2008;37(03):130–135. doi: 10.1259/dmfr/31005700. [DOI] [PubMed] [Google Scholar]
- 7.Guijarro-Martínez R, Swennen G R. Three-dimensional cone beam computed tomography definition of the anatomical subregions of the upper airway: a validation study. Int J Oral Maxillofac Surg. 2013;42(09):1140–1149. doi: 10.1016/j.ijom.2013.03.007. [DOI] [PubMed] [Google Scholar]
- 8.Burkhard J P, Dietrich A D, Jacobsen C, Roos M, Lübbers H T, Obwegeser J A. Cephalometric and three-dimensional assessment of the posterior airway space and imaging software reliability analysis before and after orthognathic surgery. J Craniomaxillofac Surg. 2014;42(07):1428–1436. doi: 10.1016/j.jcms.2014.04.005. [DOI] [PubMed] [Google Scholar]
- 9.El H, Palomo J M.Measuring the airway in 3 dimensions: a reliability and accuracy study Am J Orthod Dentofacial Orthop 2010137(4, Suppl):500–50..e9, discussion S50–S52 [DOI] [PubMed] [Google Scholar]
- 10.Barkdull G C, Kohl C A, Patel M, Davidson T M. Computed tomography imaging of patients with obstructive sleep apnea. Laryngoscope. 2008;118(08):1486–1492. doi: 10.1097/MLG.0b013e3181782706. [DOI] [PubMed] [Google Scholar]
- 11.Chen N H, Li K K, Li S Y et al. Airway assessment by volumetric computed tomography in snorers and subjects with obstructive sleep apnea in a Far-East Asian population (Chinese) Laryngoscope. 2002;112(04):721–726. doi: 10.1097/00005537-200204000-00023. [DOI] [PubMed] [Google Scholar]
- 12.Schendel S A, Hatcher D. Automated 3-dimensional airway analysis from cone-beam computed tomography data. J Oral Maxillofac Surg. 2010;68(03):696–701. doi: 10.1016/j.joms.2009.07.040. [DOI] [PubMed] [Google Scholar]
- 13.Lascala C A, Panella J, Marques M M. Analysis of the accuracy of linear measurements obtained by cone beam computed tomography (CBCT-NewTom) Dentomaxillofac Radiol. 2004;33(05):291–294. doi: 10.1259/dmfr/25500850. [DOI] [PubMed] [Google Scholar]
- 14.Yamashina A, Tanimoto K, Sutthiprapaporn P, Hayakawa Y. The reliability of computed tomography (CT) values and dimensional measurements of the oropharyngeal region using cone beam CT: comparison with multidetector CT. Dentomaxillofac Radiol. 2008;37(05):245–251. doi: 10.1259/dmfr/45926904. [DOI] [PubMed] [Google Scholar]
- 15.Olszewska E, Sieskiewicz A, Rozycki J et al. A comparison of cephalometric analysis using radiographs and craniofacial computed tomography in patients with obstructive sleep apnea syndrome: preliminary report. Eur Arch Otorhinolaryngol. 2009;266(04):535–542. doi: 10.1007/s00405-008-0826-2. [DOI] [PubMed] [Google Scholar]
- 16.Cheng I, Nilufar S, Flores-Mir C, Basu A. Airway segmentation and measurement in CT images. Conf Proc IEEE Eng Med Biol Soc. 2007;2007:795–799. doi: 10.1109/IEMBS.2007.4352410. [DOI] [PubMed] [Google Scholar]
- 17.Alves M, Jr, Franzotti E S, Baratieri C, Nunes L K, Nojima L I, Ruellas A C. Evaluation of pharyngeal airway space amongst different skeletal patterns. Int J Oral Maxillofac Surg. 2012;41(07):814–819. doi: 10.1016/j.ijom.2012.01.015. [DOI] [PubMed] [Google Scholar]
- 18.Muto T, Takeda S, Kanazawa M, Yamazaki A, Fujiwara Y, Mizoguchi I. The effect of head posture on the pharyngeal airway space (PAS) Int J Oral Maxillofac Surg. 2002;31(06):579–583. doi: 10.1054/ijom.2002.0279. [DOI] [PubMed] [Google Scholar]
- 19.Ghoneima A, Kula K. Accuracy and reliability of cone-beam computed tomography for airway volume analysis. Eur J Orthod. 2013;35(02):256–261. doi: 10.1093/ejo/cjr099. [DOI] [PubMed] [Google Scholar]
- 20.Castro-Silva L, Monnazzi M S, Spin-Neto R et al. Cone-beam evaluation of pharyngeal airway space in class I, II, and III patients. Oral Surg Oral Med Oral Pathol Oral Radiol. 2015;120(06):679–683. doi: 10.1016/j.oooo.2015.07.006. [DOI] [PubMed] [Google Scholar]
- 21.El-Beialy A R, Fayed M S, El-Bialy A M, Mostafa Y A. Accuracy and reliability of cone-beam computed tomography measurements: influence of head orientation. Am J Orthod Dentofacial Orthop. 2011;140(02):157–165. doi: 10.1016/j.ajodo.2010.03.030. [DOI] [PubMed] [Google Scholar]
- 22.Smith J D, Thomas P M, Proffit W R. A comparison of current prediction imaging programs. Am J Orthod Dentofacial Orthop. 2004;125(05):527–536. doi: 10.1016/S0889540604001210. [DOI] [PMC free article] [PubMed] [Google Scholar]


