Abstract
Purpose
To investigate the expression profile of the hypoxia-inducible transcription factor-1α (HIF-1α) and its downstream targets in malignancies of the ocular adnexa and to determine its relevance as a prognostic factor for clinical outcome.
Methods
We included 49 subjects with malignant tumours (25 squamous cell carcinomas (SCC), 15 non-Hodgkin lymphomas, 9 melanomas) and 30 patients with benign tumours of the ocular adnexa (13 papillomas, 7 reactive lymphoid hyperplasias (RLHs) and 10 nevi) as controls. We quantified HIF-1α protein expression by immunohistochemistry and assessed the association between HIF-1α and clinical outcome via Kaplan–Meier analysis. Furthermore, we assessed the expression of HIF-1α downstream factors by transcriptional sequencing using the MACE (massive analysis of cDNA ends) technology.
Results
SCCs revealed a strong HIF-1α expression in 61% of tumour cells in comparison with only 22% in papillomas (p < 0.0001). In contrast, malignant melanomas and lymphomas revealed a similar HIF-1α expression compared with nevi and RLHs. Transcriptional sequencing and Gene Ontology Cluster analysis demonstrated 37 hypoxia-associated factors, including HIF-1α, VEGF, SFRP1 and LOXL2 that are significantly increased in SCC and may contribute to tumour proliferation, angiogenesis, and metastasis. Association analysis between HIF-1α immunoreactivity and clinical outcome revealed a trend towards an unfavourable prognosis in malignant tumours with increased HIF-1α expression.
Conclusions
HIF-1α protein is increased in malignant tumours of the ocular adnexa, which is associated with an increase in multiple HIF-1α-downstream factors and a trend towards an unfavourable clinical outcome.
Subject terms: Eye cancer, Gene expression, Genomics
Introduction
Solid tumours experience mild to severe oxygen deprivation resulting from high tumour proliferation rates, dysfunctional vessels and/or reduced oxygen supply. Whereas normal oxygen concentrations reach a level of 2–9% (on average 40 mmHg) in most organs, this may drop to under 2% in malignancies, an event defined as hypoxia [1]. Local hypoxia has been postulated to play a major role in tumour metabolism, progression and its dissemination and hypoxic metabolites are currently investigated as potential prognostic markers and therapeutic targets [2].
Hypoxia-inducible transcription factors (HIFs) are activated in response to low oxygen concentrations and considered as master regulators of oxygen homoeostasis. HIFs are basic helix-loop-helix proteins that form heterodimers, composed of an oxygen-dependent α-subunit (HIF-α) and a constitutively expressed β-subunit (HIF-β). Humans have three distinct HIF-α isoforms (HIF-1α, HIF-2α (EPAS1, endothelial PAS domain-containing protein 1) and HIF-3α), of which HIF-1α and HIF-2α are the most studied ones. Under a normal oxygen concentration HIF-α is hydroxylated by prolyl-hydroxylases (PHD 1–3 = EGLN1–3), which require oxygen as a substrate, and consequently degraded by the 'von Hippel-Lindau' (VHL) factor in the proteasome. Under hypoxic conditions, however, HIF-α escapes PHD-mediated hydroxylation and translocates into the nucleus, where it binds to HIF-β and other co-factors leading to the expression of over 100 different hypoxia-associated genes. Together, these genes orchestrate adaptive tissue responses, such as angiogenesis, cell proliferation and improved glucose metabolism, with the shared aim of counteracting tissue hypoxia [3]. Next to its beneficial physiological role, HIF-α is also involved in tumour cell metabolism, vascularisation, growth and metastasis and has been associated with poor patient survival rates in a broad range of malignancies [4]. Increased HIF-1α expression was reported to occur in oesophageal, colorectal, hepatocellular, bladder and cutaneous cancer and to predict an unfavourable clinical outcome (topic extensively reviewed in ref. [4]). Whereas the relevance of HIF-1α in these malignancies is established, the expression of HIF-1α in tumours of the ocular adnexa and its potential relevance for clinical outcome is to date ill-defined. This is of particular interest as ocular tumours can significantly differ from other malignancies, as shown for ocular and cutaneous melanoma, which demonstrate different genetic and molecular alterations, metastatic potential and clinical response to treatment [5].
Furthermore, although most of the aforementioned studies focus on HIF-1α and selected HIF-1α downstream targets, a detailed overview of the hypoxia-related transcriptional changes in malignancies is lacking.
This study aimed to determine the expression pattern of HIF-1α protein in tumours of the ocular adnexa, to provide a comprehensive landscape of hypoxia-related transcriptional alterations in SCC and papilloma and to correlate HIF-1α levels with clinical outcome.
Methods
Patients
In this study a total of 79 subjects with tumours of the ocular adnexa who had been treated at the Eye Center of Freiburg University between 1995 and 2012 were included. Clinical data, such as histological diagnosis, age at diagnosis, gender, treatment modality, follow-up time, local recurrences, metastasis and/or death, were collected on each subject from patient charts, primary care physicians and the Clinical Tumour Registry of the Medical Center at the University of Freiburg [6]. As some of the patients had already died at the time of this retrospective analysis, we could not obtain informed consent from all patients. Therefore, a retrospective anonymous analysis was performed according to the local ethical standards. Institutional Review Board (IRB)/Ethics Committee approval was obtained for this study (approval number FR22/15).
Immunohistochemistry and scoring
Fixation, grossing and paraffin embedding were performed as previously described [7]. In brief, tumour specimens were fixed immediately after surgery in 4% formalin for 12 h, dehydrated in alcohol and finally processed for paraffin embedding. Sections (4 µm slices for solid tumours and 2 µm slices for lymphomas and reactive lymphoid hyperplasias (RLHs)) were cut, mounted on silanized slides and deparaffinized in xylol alcohol. Following routine histological staining, all specimens were classified by two independent pathologists. Tumour thickness was measured vertically from the surface to the deepest point of invasion in melanoma (n = 9) and squamous cell carcinoma (n = 22) but not in lymphoma because most of these specimens were incisional biopsies, which did not allow determination of the tumour margins with confidence.
HIF-1α immunohistochemistry was performed in a standardised matter, as previously described [8]. In brief, antigen retrieval was achieved by exposing slides in citrate buffer to 95 °C in a steamer for 1 h. Following incubation with a protein block and a blocking agent against endogenous peroxidase, the sections were incubated with primary monoclonal antibodies against HIF-1α (Novus Biologicals® NB 100-105 diluted in a 1:8000 proportion for SCC/papilloma, 1:4000 for melanoma/nevi and 1:2000 for lymphoma/RLH) for 24 h at 4 °C. After extensive washing, secondary polyclonal antibodies against rabbit (DAKO® CSA biotinylated Link) were applied for 60 min at room temperature. Finally, a catalysed signal amplification system (DAKO® CSA) was applied and streptavidin-horseradish peroidase added for 15 min. AEC (3-Amino-9-ethylcarbazole) was used as a chromogen and applied to the sections for 2 min. Nuclear counterstaining was performed using hematoxylin (GILL III LOT: 050113). Sections of human colon, mammary and ovarian carcinoma were employed as positive controls, based on findings demonstrating strong HIF-1α expression in these entities [9]. Tissue samples subjected to the same protocol, only omitting the primary antibody application, served as negative controls.
Following immunohistochemistry, the sections were immediately imaged using a microscope with a 40-fold magnification (Zeiss Axio Imager AX10). Four high magnification images (× 200) demonstrating a strong and representative HIF-1α immunoreactivity were randomly taken from different central and peripheral sites of the tumour in each case to avoid bias arising from intratumoural heterogeneity. HIF-1α expression was considered positive, if a specific nuclear staining was detected. In each image more than 100 tumour cells were counted and the percentage of HIF-1α-positive tumour cells was determined in a masked fashion by two independent examiners. The average value was used for further analysis.
RNA isolation
Total RNA was isolated from formalin-fixed and paraffin-embedded (FFPE) sections of five randomly chosen malignant SCCs and six benign tumours using the Quick-RNA FFPE Kit (Zymo Research). Following a DNAse I digestion using the Baseline-ZERO kit (Epicentre), the RNA concentration was measured with the Qubit RNA HS Assay Kit on a Qubit Fluorometer (Life Technologies). The RNA quality was determined with the RNA Pico Sensitivity Assay on a LabChip GXII Touch (PerkinElmer). The fragment size of all RNA samples ranged between 120 and 150 bp.
MACE libraries
The preparation of massive analysis of cDNA ends (MACE) libraries was carried out by GenXPro GmbH using 1 µg of total RNA, as previously described [10]. Eleven barcoded libraries (five SCCs and six papillomas) were sequenced simultaneously on the NextSeq 500 (Illumina) with 1 × 75 bp. Illumina sequence reads were processed with an in-house analysis pipeline (GenXPro), including TrueQuant PCR bias elimination and mapping against the human reference genome. Gene Ontology enrichment analysis was performed with the web-based Gene Ontology (GO)-enrichment toolkit from GenXPro.
Statistical analysis
To statistically analyse and compare all six tumour groups, we conducted the non-parametric Kruskal–Wallis test followed by a Dunn’ multiple comparison analysis method, which corrects for multiple testing and has no normality assumptions. Tumour thickness was compared using the unpaired two-sided t test. For MACE analysis, normalisation and test for differential gene expression were calculated using the DEGseq [11]. Differential gene expression was quantified as the log2 ratio of the normalised values between two libraries. Heat maps were generated using the freely available web server software Heatmapper (www.heatmapper.ca).
For the sake of clinical correlation, each subject’s charts were reviewed and clinical parameters including the patient’s gender, date of birth, age at diagnosis, histologic diagnosis, recurrences, metastasis and date and cause of death, as well as overall follow-up time, were recorded. The event-free survival was defined as the time from the date of histological diagnosis to the first date of either relapse, metastasis or death and estimated using Kaplan–Meier analysis. To examine association between HIF-1α immunoreactivity with clinical outcome, patients were dichotomised into a HIF-1α-high (defined as over the median value of HIF-1α-positive tumour cells, i.e., > 65% in SCCs, > 15% in lymphomas and >13% melanomas) and a HIF-1α-low group (< 65% in SCCs, < 15% in lymphomas and < 13% melanomas). Cox-regression analysis was applied including the age at inclusion and the binarized HIF-1α levels to compare the event-free survival time in both groups. All calculations were performed using GraphPad Prism® (GraphPad Version 5.04) and the R-System (available at: www.r-project.org). Unless otherwise stated, a significance level of 0.05 was adopted.
Results
Patient characteristics
Seventy-nine tumours of the ocular adnexa from 79 patients were included in this study. Histological analyses confirmed squamous cell carcinomas in 25 patients, non-Hodgkin B-cell lymphomas in 15 patients (eight MALT lymphoma, three mantle cell lymphoma, three follicular and one diffuse large cell lymphoma), malignant melanomas in 9 patients, benign papillomas in 13 patients, RLHs in 7 patients and nevi in 10 patients. Patient characteristics are summarised in Table 1. The mean follow-up time was 7.1 years in the SCC group (median 7.2 yrs, interquartile range (IQR) 6.5 yrs), 8.8 years in the lymphoma group (median 8.0 yrs, IQR 8.4 yrs) and 7.1 years in the melanoma group (median 7.1 yrs, IQR 7.4 yrs), respectively (see Table 1).
Table 1.
Patients’ characteristics
| Group | n | Sex (m:f) | Age in yrs, median (Q1, Q3) | Follow-up in yrs, median (Q1, Q3) | HIF-1α + cells in %, median (Q1, Q3) |
|---|---|---|---|---|---|
| Malignant tumours of the ocular adnexa | |||||
| SCC | 25 | 17/8 | 66 (53, 78) | 7.2 (3.1, 9.6) | 64 % (50.5, 71.5) |
| Lymphoma | 15 | 7/8 | 64 (57, 76) | 8.0 (4.1, 12.5) | 16 % (6.0, 22.0) |
| Melanoma | 9 | 7/2 | 62 (55, 70) | 5.6 (3.5, 10.9) | 13 % (4.0, 17.0) |
| Benign tumours of the ocular adnexa | |||||
| Papilloma | 13 | 7/6 | 56 (47, 66) | NA | 20 % (8.5, 33.5) |
| RLH | 7 | 2/5 | 61 (55, 69) | NA | 7 % (3.0, 13.0) |
| Naevus | 10 | 4/6 | 64 (58, 70) | NA | 12 % (0.0, 25.3) |
HIF-1α is increased in epithelial and lymphoid malignancies of the ocular adnexa
We successfully established an immunohistochemistry protocol for HIF-1α, which exhibited a robust nuclear staining pattern in the tumour sections of patients with colorectal, mammarian and ovarian carcinoma, as previously described (Suppl Fig. 1) [9]. SCCs revealed a strong nuclear expression pattern for HIF-1α in 61% (standard deviation (SD) 15%) of tumour cells, compared with only 22% (SD 15%) in benign papilloma (Fig. 1a, b). Malignant melanomas (13%, SD 11%) and lymphomas (15%, SD 9%), in contrast, revealed a similar percentage of tumour cells expressing HIF-1α compared with benign nevi (15%, SD 16%) and RLHs (8%, SD 6%, Fig. 1c–f). No significant difference in HIF-1α expression among the different lymphoma subtypes was detected (data not shown). Tumour thickness measurement revealed that SCC were in average significantly thicker than melanoma (mean 2.7 mm; SD 1.3 mm versus 0.8 mm, SD 0.5, p < 0.0001). Interestingly, a strong positive correlation was detected between tumour thickness and HIF-1α expression (Spearman r = 0.49, 95% CI 0.15–0.72, p = 0.006), which may be explained by increased hypoxia- or inflammation-driven HIF-1α expression in thicker tumours (Suppl Fig. 2). However, no specific staining pattern of HIF-1α-positive cells within a tumour in any entity was observed. In particular, no elevated HIF-1α expression in the avascular centre of the tumour, nor any obvious reduction in HIF-1α expression in the vicinity of vessels was noticed.
Fig. 1.
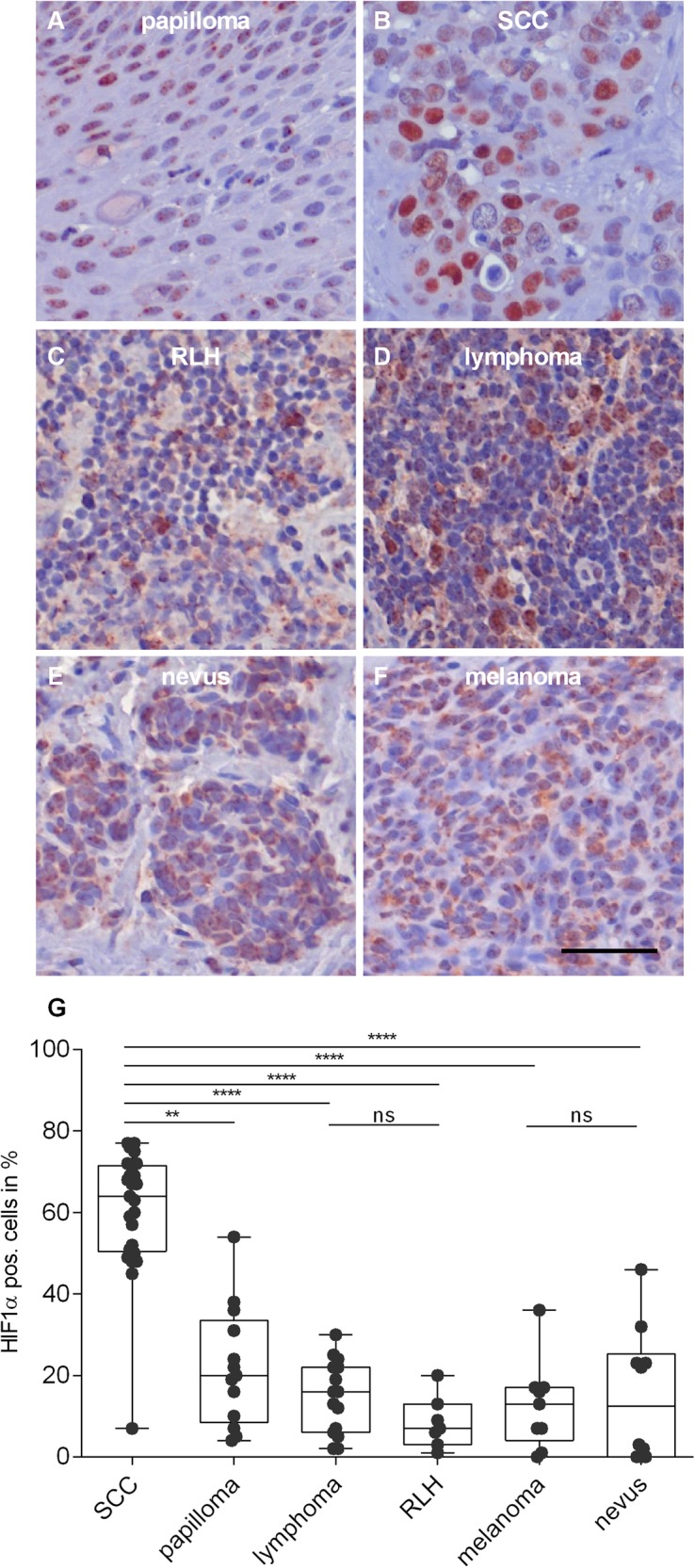
HIF-1α expression is increased in malignant tumours of the ocular adnexa. Representative HIF-1α immunostaining in papilloma a squamous cell carcinoma (SCC) b, reactive lymphoid hyperplasia (RLH) c, lymphoma d, naevus e and melanoma f of the ocular adnexa showing increased numbers of HIF-1-α positive tumour cells in SCC compared with papilloma and similar expression patterns in non-Hogkin lymphoma and melanoma compared with RLH and nevi. g Dot blot analysis of the percentage of HIF-1α-positive cells in tumours of the ocular adnexa. Each dot represents one subject. HIF-1α expression is significantly increased in SCC compared with other tumour entities (ANOVA P < 0.0001). Scale bar = 50 µm
To detect any differences in HIF-1α expression in distinct malignant entities of the ocular adnexa, we compared the percentage of HIF-1α-expressing tumour cells across all tumours. SCCs demonstrated a significant and about fourfold larger fraction of HIF-1α expressing cells compared with lymphoma and melanoma tumours (p < 0.0001), indicating a distinct expression pattern of HIF-1α in different ocular malignancies and a potential role on the part of HIF-1α in the pathogenesis of SCC (Fig. 1g).
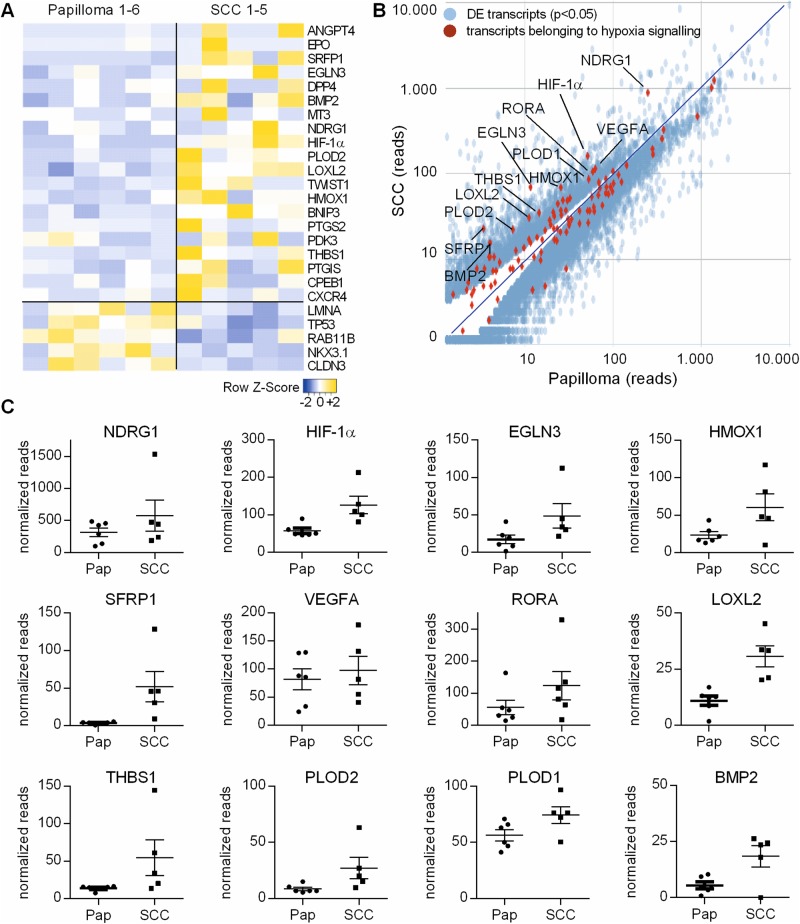
HIF-1α downstream factors are increased in SCC of the ocular adnexa
To validate our finding of increased HIF-1α activity in SCC, we performed MACE RNA sequencing analysis and determined the differential expression of hypoxia-regulated factors in SCC and papilloma.
Before TrueQuant elimination of PCR-induced replicates and artifacts, each MACE library included 1.7–19.2 million reads raw reads, after TrueQuant processing 0.48–5.38 million reads, which allowed an exact quantification and comparison of mRNA expression (sense and antisense transcripts) for all SCC and papilloma specimens.
GO Cluster analysis revealed significant enrichment of hypoxia-regulated factors in SCC compared with papilloma of the ocular adnexa (p = 0.004). Of a total of 113 annotated hypoxia-regulated genes, we identified 71 factors that yielded a significant differential expression in SCC when compared with papilloma. Of those, 37 mRNAs were significantly increased and 34 mRNAs significantly decreased in SCC, while 42 factors revealed no significant difference between papilloma and SCC (Fig. 2, Suppl Tables 1–3). HIF-1α and HIF-3α mRNA expression was significantly increased in SCC compared with papilloma (p < 0.0001 and p < 0.05, respectively), whereas HIF-2α and VHL mRNA levels were significantly downregulated in SCC (p < 0.0001) indicating a differential expression of HIF-α isoforms in SCC. Interestingly, EGLN1 and EGLN3 were significantly upregulated in SCC compared with papilloma (p < 0.0001 and 0.001, respectively) suggesting a direct negative regulatory mechanism of HIF-1α on its degradation in hypoxia. In addition, pro-angiogenic factors, such as secreted frizzled-related protein 1 (SFRP1, p < 0.0001), VEGF (p < 0.0001), angiopoietin 4 (ANGPT4, p < 0.0001) and erythropoietin (EPO, p < 0.05) were significantly increased in SCC, illustrating a pro-angiogenic environment in SCC. Furthermore, hypoxia-induced factors contributing to tumourigenesis and metastasis, such as lysyl oxidase homologue 2 (LOXL2), thrombospondin 1 (THBS1), angiopoietin-like 4 (ANGPTL4), dipeptidyl peptidase-4 (DPP4) and Twist-related protein 1 (TWIST1), as well as inflammatory factors, such as bone morphogenic protein 2 (BMP2) and prostaglandin synthases (PTGS2, PTGIS) were significantly increased in SCC in comparison with papilloma, indicating a more aggressive tumour fingerprint in SCC (Table S1).
Fig. 2.
MACE mRNA sequencing of hypoxia-related factors in SCC and papilloma of the ocular adnexa. a Heatmap of differentially regulated hypoxia-dependent mRNAs in SCC (n = 5) and papilloma (n = 6) of the ocular adnexa focusing on factors with a False Discovery Rate (FDR) < 0.02 and a log2fold of > or < 1. The Z score represents the deviation from the mean by standard deviation units. Colours ranging from blue to yellow indicate low to high abundance levels. b scatter blot and c dot blot visualisation of the top 12 differentially regulated hypoxia-related factors that are increased in SCC compared with papilloma sorted according to the FDR. Each dot represents one tumour sample. DE = differentially expressed
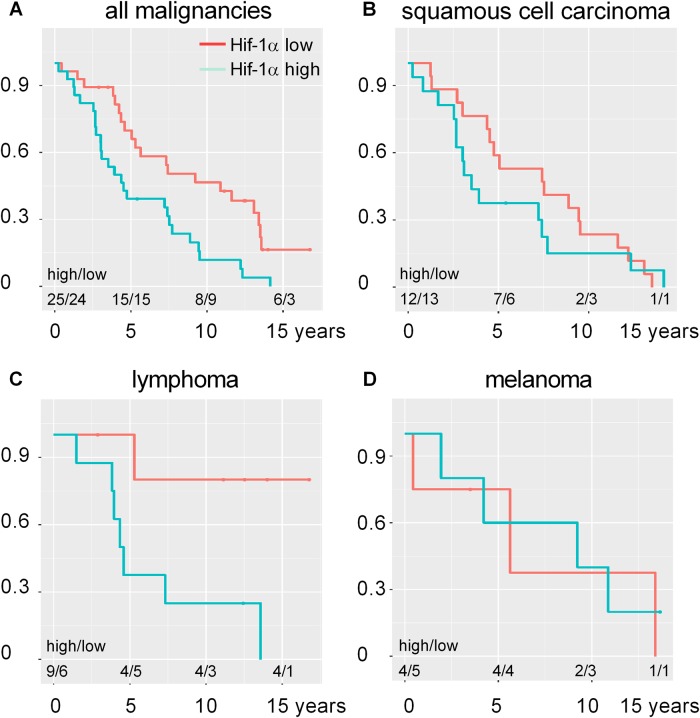
Enhanced HIF-1α activity is associated with poor clinical outcome
To determine whether HIF-1α expression in malignancies of the ocular adnexa has an impact on clinical outcome, we performed a Kaplan–Meier analysis. For this purpose, we divided subjects into a HIF-1α-high and HIF-1α-low group and determined the survival, recurrence rate and frequency of metastasis depending on the grade of HIF-1α expression (Fig. 3). We observed that malignant tumours characterised by strong HIF-1α activity were associated with a trend towards higher incidence of negative outcomes. The median time to reach an endpoint (i.e., death, metastasis or relapse) for all subjects with malignancies of the ocular adnexa with strong HIF-1α expression was 4.6 years compared with 7.4 years in subjects with low HIF-1α expression (hazard ratio (HR) age = 0.99 per year, 95% CI 0.96–1.01; HR HIF-1α 2.31, 95% CI 1.19–4.49). Subgroup analysis revealed a median event-free survival time of 4.5 years for HIF-1α-low SCC, 5.2 years for HIF-1α-high SCC, 9.2 years for HIF-1α-low melanoma, 5.6 years for HIF-1α-high melanoma as well as 4.5 years for HIF-1α-high lymphoma. The median event-free time for HIF-1α low lymphoma could not be determined owing to the sparsity of events. The insufficient number of observations in this study precluded any reasonable statistical modelling of the intercorrelated covariates HIF-1α and tumour thickness.
Fig. 3.
Kaplan–Meier curves for HIF-1α-high and HIF-1α-low malignancies. The median survival time from tumour resection (t0) to the first event (i.e., death, metastasis relapse) is depicted for a all malignant tumours (hazard ratio HIF-1α 2.31, 95% CI 1.19 −4.49), b squamous cell carcinoma, c lymphoma and d melanoma. Patients were dichotomised into a HIF-1α-high (defined as over the median value of HIF-1α-positive tumour cells, i.e., > 65% in SCCs, > 15% in lymphomas and > 13% melanomas) and a HIF-1α-low group ( < 65% in SCCs, < 15% in lymphomas and < 13% melanomas). Mean follow-up time was 7.2 years (SD 4.3) in the SCC, 8.8 years (SD 6.1) in the lymphoma and 7.1 years (SD 4.9) in the melanoma group. The number of patients at risk with HIF-1α-high and HIF-1α-low levels at 0, 5, 10 and 15 years following t0 are shown at the bottom of each plot
Discussion
Hypoxia is a cardinal feature in many types of solid tumours and the consequence of rapid tumour proliferation and high metabolic demand combined with structurally and functionally inadequate vessels. Hypoxia-inducible transcription factors represent central mediators for hypoxia-sensing in tumours and initiate adaptive tissue responses through the transcriptional activation of over 100 target genes [3].
This study demonstrates that HIF-1α expression is significantly increased in malignant SCC of the ocular adnexa, when compared with benign papilloma. Our results are in line with several immunohistochemical studies demonstrating enhanced HIF-1α protein expression in malignant tumours of the bladder, brain, breast, colon, ovaries, prostate, kidneys and skin compared with corresponding healthy tissues [12]. Among the ocular malignancies HIF-1α protein expression was most pronounced in SCC, which may be attributed to the rapid and voluminous tumour growth of SCCs in contrast to the rather thin and superficially growing lymphomas and melanomas. Our study reveals that most of the tumour cells in SCC of the ocular adnexa were HIF-1α positive (68%, SD 15%), which is in agreement with other SCC of the body [13, 14] indicating a putative role for HIF-1α in the pathogenesis of SCC. However, we did not detect enhanced HIF-1α expression in the centre of the tumour or any obvious reduction in HIF-1α expression in cells close to vessels. This observation is in accordance with studies demonstrating that hypoxic regions (determined either via histochemical markers or in vivo imaging) reveal a less-pronounced co-incidence with regions of HIF upregulation within malignant tumours than might be expected [15]. Taken together, these studies indicate that although micro-environmental hypoxia may contribute to the activation of HIF in ocular malignancies, other non-oxygen-dependent factors must also play a role in stabilising HIF-1α such as oncogene activation and/or tumour suppressor gene inactivation during SCC progression.
To validate our finding of increased HIF-1α activity in SCC, we analysed hypoxia-related transcriptional changes in SCC and noted a significant enrichment of hypoxia-regulated factors in SCC compared with papilloma. HIF-1α mRNA was significantly increased in SCC, indicating that HIF-1α is not only controlled through post-translational modifications and stabilisation but also on a transcriptional level in SCC. Next to HIF-1α, HIF-3α mRNA was increased, whereas HIF-2α was downregulated in SCC, suggesting a differential expression of HIF-α isoforms and their downstream targets in SCC. There is emerging evidence that different HIF-α isoforms can selectively induce the gene expression of different target genes and thereby initiate various cellular functions [3, 16]. For instance, in renal cell carcinoma HIF-1α targets the pro-apoptotic gene BNIP3, whereas HIF-2α drives the cell cycle regulator Cyclin D1 [17], a finding supported by our transcriptional analysis. It is tempting to speculate that this study’s transcriptional analysis might reflect the differential expression of HIF-1α and HIF-2α in SCC. However, given the enormous complexity of gene regulation, further research is warranted to define HIF-1α and HIF-2α targets and their respective cellular functions with confidence. Interestingly, we found a significant upregulation of EGLN1 and EGLN3 in SCC, which play an important role in degrading HIF-α. This finding is counterintuitive, but in line with previous studies demonstrating increased levels of EGLN1 and EGLN3 in hypoxic tissues and suggesting a direct, negative regulatory mechanism, which limits and counteracts the hypoxic HIF response [18]. This negative feedback loop was also found in human glioblastoma tissue and suggested to protect tumour cells against hypoxia-induced cell death [19], which may explain the paucity of hypoxia-induced pro-apoptotic factors found in SCC.
The regulation of angiogenesis by hypoxia and HIF is an important component of tumour development and progression, as tumour cell growth frequently outstrips the supply of oxygen and nutrients. In our study, numerous pro-angiogenic factors were significantly increased in SCC, including ANGPT4, EPO, SFRP1 and VEGF. Among these biomolecules, VEGF and EPO are well-established factors in tumour angiogenesis. Several studies demonstrate increased VEGF or EPO expression and respective positive correlations with HIF-1α in various SCC types, including oral SCC [20] and head and neck SCC [21]. ANGPT4 and SFRP1, in contrast, have so far received less attention in SCC-associated tumour angiogenesis, but they are additional potent angiogenic factors, contributing to tumour angiogenesis eg in oesophageal and oral SCC [22]. Together, these HIF-1α-induced factors create a pro-angiogenic microenvironment in SCC that may facilitate angiogenesis, tumour growth and possibly metastatic affinity.
Metastasis is a complex process, in which tumour cells must acquire an invasive phenotype, enter the blood and lymphatic circulation, survive the immune response and cell death and once localised to a distant site, proliferate and endure in a hostile environment. Tumour hypoxia and HIF-1α signalling are critical for these processes and HIF-1α confers a significant risk of metastasis [4]. Our study identifies several HIF-1α-dependent factors in SCC that are involved in tumour metastasis including LOXL2, THBS1, ANGPTL4, DPP4, TWIST1, TGFB2 and CXCR4. These factors play central roles in different stages of metastatic development. CXCR4, TGFB2 and TWIST1, for instance, contribute to epithelial-mesenchymal transition (EMT), a process, in which tumour cells change from an epithelial non-motile phenotype to a mesenchymal migratory phenotype and become able to invade other tissues [23, 24]. ANGPTL4, on the other hand, protects tumour cells from programmed cell death, which is induced when contact-dependent cells detach from the surrounding tissue matrix [25]. Furthermore, ANGPTL4 disrupts endothelial cell junctions by directly interacting with integrin, VE-cadherin and claudin-5, thereby facilitating metastasis [26]. Finally, HIF-1α-induced expression of LOXL2 contributes to EMT and cancer metastasis and initiates the recruitment of bone marrow-derived cells to the metastatic niche, thus creating a receptive environment for cancer cells [27]. Taken together, these observations strongly support a significant role for HIF-1α in promoting tumour growth and metastasis in SCC of the ocular adnexa. Although well addressed in other tumour types, the mechanistic aspects of HIF-1α-mediated metastasis in SCC still remain largely unexplored and need further investigation.
Our study suggests that increased HIF-1α expression in ocular malignancies is associated with a tendency towards an unfavourable patient outcome, defined as tumour recurrence, metastasis or death. This correlation is in line with other studies showing an unfavourable outcome for patients presenting increased HIF-1α expression in SCC of the oesophagus, colorectal cancer, hepatocellular carcinoma, bladder cancer and many others (topic extensively reviewed in ref. [4]). Although these correlation studies are potentially informative, we emphasise that they provide no evidence for causality. Although HIF-1α signalling might make malignancies more aggressive and result in a worse clinical outcome, it is also possible that intrinsically aggressive tumours lead to lower oxygen tensions and thereby to more pronounced HIF-1α activation. However, there are also reports describing that HIF-1α overexpression provides a better prognosis for patients with an early-stage SCC of the oral floor [28] or renal cell carcinoma [29]. Vleugel and colleagues investigated HIF-1α concentrations in invasive breast cancers and observed increased HIF-1α expression around necrotic tissue, a finding associated with a poor prognosis, whereas on the other hand, diffuse HIF-1α expression within the tumour correlated with a better prognosis [30]. These contradicting findings highlight the complexity of HIF’s involvement in cancer, and suggest that the effect of HIF-1α on prognosis may depend on the differential expression profile within the tumour, the tumour stage and the specific malignant phenotype itself.
Limitations of the current study include its retrospective character and the possibility of RNA degradation within FFPE samples over time. However, as malignancies of the ocular adnexa are very rare tumour entities with reported incidences of 0.02–3.5 per 100,000 for SCC [31], 0.2–0.8 per 1,000,000 for melanoma [32, 33] and 2–4 per 1,000,000 for lymphoma [34], a prospective collection of tumour samples would be challenging and require a multi-centre collaborative approach to include sufficient numbers of tumour patients. Even though some of the samples had been stored in paraffin for over 10 years, each MACE library included an adequate number of reads, thus allowing for exact quantification and comparison of mRNA profiles. Another limiting factor is the small number of study participants, which again is owing to the rare incidence of these tumours. Despite the limited number of study participants in the subgroup, we identified a clinical trend towards an unfavourable outcome in patients suffering from lymphoma of the ocular adnexa. However, the number of patients analysed in this study is too small to make conclusive statements. Further multi-centre collaborative approaches are warranted to define the role of HIF-1α as a prognostic factor for patient outcome with confidence. This is especially mandatory in light of the first clinical trials addressing the use of pharmaceuticals to selectively suppress the HIF-1α-subunit in solid malignancies [35].
In conclusion, the present study demonstrates significantly higher levels of HIF-1α in SCC compared with the corresponding benign papilloma. SCC exhibited significant alteration of 71 HIF-1α-regulated factors that may contribute to angiogenesis, tumour progression and metastasis in SCC. Moreover, increased HIF-1α levels were associated with a trend towards an unfavourable clinical outcome in SCC. Although our subgroup analysis of patients with SCC and lymphoma demonstrated a clinical trend for a negative outcome, it failed to attain significance, possibly owing to the rather low number of patients enroled in this study. Further investigations with increased statistical power are needed to determine with confidence the role of HIF-1α as a prognostic factor and a potential treatment target in patients with malignancies of the ocular adnexa.
Summary
What was known before
Local hypoxia has been postulated to play a major role in tumour metabolism, progression and its dissemination.
Hypoxic metabolites are currently investigated as potential prognostic markers and therapeutic targets.
HIF-1-a is involved in tumour cell metabolism, vascularisation, growth and metastasis and has been associated with poor patient survival rates in a broad range of malignancies.
What this study adds
SCC of the ocular adnexa reveal a strong HIF-1α expression in 61% of tumour cells in comparison with only 22% in papillomas
Transcriptional sequencing and Gene Ontology Cluster analysis demonstrated 37 hypoxia-associated factors that are significantly increased in SCC and may contribute to tumour proliferation, angiogenesis and metastasis.
A correlation between HIF-1α immunoreactivity and clinical outcome revealed a trend towards an unfavourable prognosis in malignant tumours with increased HIF-1α expression.
Electronic supplementary material
Acknowledgements
We thank Sylvia Zeitler for the technical assistance.
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
The online version of this article (10.1038/s41433-018-0172-6) contains supplementary material, which is available to authorised users.
References
- 1.Bertout JA, Patel SA, Simon MC. The impact of O2 availability on human cancer. Nat Rev Cancer. 2008;8:967–75. doi: 10.1038/nrc2540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wilson WR, Hay MP. Targeting hypoxia in cancer therapy. Nat Rev Cancer. 2011;11:393–410. doi: 10.1038/nrc3064. [DOI] [PubMed] [Google Scholar]
- 3.Semenza GL. Hypoxia-inducible factors in physiology and medicine. Cell. 2012;148:399–408. doi: 10.1016/j.cell.2012.01.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brocato J, Chervona Y, Costa M. Molecular responses to hypoxia-inducible factor-1α and beyond. Mol Pharmacol. 2014;85:651–7. doi: 10.1124/mol.113.089623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Belmar-Lopez C, Mancheno-Corvo P, Saornil MA, Baril P, Vassaux G, Quintanilla M, et al. Uveal vs. cutaneous melanoma. Origins and causes of the differences. Clin Transl Oncol. 2008;10:137–42. doi: 10.1007/s12094-008-0170-4. [DOI] [PubMed] [Google Scholar]
- 6.Csanadi A, Kayser C, Donauer M, Gumpp V, Aumann K, Rawluk J, et al. Prognostic value of malic enzyme and ATP-citrate lyase in non-small cell lung cancer of the young and the elderly. PLoS ONE. 2015;10:e0126357. doi: 10.1371/journal.pone.0126357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lange CA, Tisch-Rottensteiner J, Böhringer D, Martin G, Schwartzkopff J, Auw-Haedrich C. Enhanced TKTL1 expression in malignant tumors of the ocular adnexa predicts clinical outcome. Ophthalmology. 2012;119:1924–9. doi: 10.1016/j.ophtha.2012.03.037. [DOI] [PubMed] [Google Scholar]
- 8.Lange C. A. K., Luhmann U. F. O., Mowat F. M., Georgiadis A., West E. L., Abrahams S., Sayed H., Powner M. B., Fruttiger M., Smith A. J., Sowden J. C., Maxwell P. H., Ali R. R., Bainbridge J. W. B. Von Hippel-Lindau protein in the RPE is essential for normal ocular growth and vascular development. Development. 2012;139(13):2340–2350. doi: 10.1242/dev.070813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yoshimura H, Dhar DK, Kohno H, Kubota H, Fujii T, Ueda S, et al. Prognostic impact of hypoxia-inducible factors 1α and 2α in colorectal cancer patients correlation with tumor angiogenesis and cyclooxygenase-2 expression. Clin Cancer Res. 2004;10:8554–60. doi: 10.1158/1078-0432.CCR-0946-03. [DOI] [PubMed] [Google Scholar]
- 10.Zajac BK, Amendt J, Horres R, Verhoff MA, Zehner R. De novo transcriptome analysis and highly sensitive digital gene expression profiling of Calliphora vicina (Diptera: Calliphoridae) pupae using MACE (Massive Analysis of cDNA Ends) Forensic Sci Int Genet. 2015;15:137–46. doi: 10.1016/j.fsigen.2014.11.013. [DOI] [PubMed] [Google Scholar]
- 11.Wang L, Feng Z, Wang X, Wang X, Zhang X. DEGseq: an R package for identifying differentially expressed genes from RNA-seq data. Bioinformatics. 2010;26:136–8. doi: 10.1093/bioinformatics/btp612. [DOI] [PubMed] [Google Scholar]
- 12.Talks KL, Turley H, Gatter KC, Maxwell PH, Pugh CW, Ratcliffe PJ, et al. The expression and distribution of the hypoxia-inducible factors HIF-1alpha and HIF-2alpha in normal human tissues, cancers, and tumor-associated macrophages. Am J Pathol. 2000;157:411–21. doi: 10.1016/S0002-9440(10)64554-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ribeiro M, Teixeira SR, Azevedo MN, Fraga AC, Jr, Gontijo AP, Vêncio EF. Expression of hypoxia-induced factor-1 alpha in early-stage and in metastatic oral squamous cell carcinoma. Tumor Biol. 2017;39:101042831769552. doi: 10.1177/1010428317695527. [DOI] [PubMed] [Google Scholar]
- 14.Swinson DEB, Jones JL, Cox G, Richardson D, Harris AL, O’Byrne KJ. Hypoxia-inducible factor-1? in non small cell lung cancer: Relation to growth factor, protease and apoptosis pathways. Int J Cancer. 2004;111:43–50. doi: 10.1002/ijc.20052. [DOI] [PubMed] [Google Scholar]
- 15.Lehmann S, Stiehl DP, Honer M, Dominietto M, Keist R, Kotevic I, et al. Longitudinal and multimodal in vivo imaging of tumor hypoxia and its downstream molecular events. Proc Natl Acad Sci USA. 2009;106:14004–9. doi: 10.1073/pnas.0901194106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mowat FM, Luhmann UF, Smith AJ, Lange C, Duran Y, Harten S, et al. HIF-1alpha and HIF-2alpha are differentially activated in distinct cell populations in retinal ischaemia. PLoS ONE. 2010;5:e11103. doi: 10.1371/journal.pone.0011103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Maxwell PH. The HIF pathway in cancer. Semin Cell Dev Biol. 2005;16:523–30. doi: 10.1016/j.semcdb.2005.03.001. [DOI] [PubMed] [Google Scholar]
- 18.Marxsen JH, Stengel P, Doege K, Heikkinen P, Jokilehto T, Wagner T, et al. Hypoxia-inducible factor-1 (HIF-1) promotes its degradation by induction of HIF-α-prolyl-4-hydroxylases. Biochem J. 2004;381:761–7. doi: 10.1042/BJ20040620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Henze AT, Riedel J, Diem T, Wenner J, Flamme I, Pouyseggur J, et al. Prolyl hydroxylases 2 and 3 act in gliomas as protective negative feedback regulators of hypoxia-inducible factors. Cancer Res. 2010;70:357–66. doi: 10.1158/0008-5472.CAN-09-1876. [DOI] [PubMed] [Google Scholar]
- 20.El-Sayed Mohammed Youssef H, Eldeen Abo-Azma NE, Eldeen Megahed EM. Correlation of hypoxia-inducible factor-1 alpha (HIF-1α) and vascular endothelial growth factor (VEGF) expressions with clinico-pathological features of oral squamous cell carcinoma (OSCC) Tanta Dent J. 2015;12:S1–14. doi: 10.1016/j.tdj.2015.05.010. [DOI] [Google Scholar]
- 21.Mohyeldin A, Lu H, Dalgard C, Lai SY, Cohen N, Acs G, et al. Erythropoietin signaling promotes invasiveness of human head and neck squamous cell carcinoma. Neoplasia. 2005;7:537–43. doi: 10.1593/neo.04685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Yi J, Pan B, Xiong L, Song H. Clinical significance of angiopoietin-like protein 4 expression in tissue and serum of esophageal squamous cell carcinoma patients. Med Oncol. 2013;30:680. [DOI] [PMC free article] [PubMed]
- 23.Lv B, Yang X, Lv S, Wang L, Fan K, Shi R, et al. CXCR4 signaling induced epithelial-mesenchymal transition by PI3K/AKT and ERK pathways in glioblastoma. Mol Neurobiol. 2015;52:1263–8. doi: 10.1007/s12035-014-8935-y. [DOI] [PubMed] [Google Scholar]
- 24.Xu J, Lamouille S, Derynck R. TGF-beta-induced epithelial to mesenchymal transition. Cell Res. 2009;19:156–72. doi: 10.1038/cr.2009.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zhu P, Tan MJ, Huang RL, Tan CK, Chong HC, Pal M, et al. Angiopoietin-like 4 protein elevates the prosurvival intracellular O2−:H2O2 ratio and confers anoikis resistance to tumors. Cancer Cell. 2011;19:401–15. doi: 10.1016/j.ccr.2011.01.018. [DOI] [PubMed] [Google Scholar]
- 26.Huang RL, Teo Z, Chong HC, Zhu P, Tan MJ, Tan CK, et al. ANGPTL4 modulates vascular junction integrity by integrin signaling and disruption of intercellular VE-cadherin and claudin-5 clusters. Blood. 2011;118:3990–4002. doi: 10.1182/blood-2011-01-328716. [DOI] [PubMed] [Google Scholar]
- 27.Erler JT, Bennewith KL, Cox TR, Lang G, Bird D, Koong A, et al. Hypoxia-induced lysyl oxidase is a critical mediator of bone marrow cell recruitment to form the premetastatic niche. Cancer Cell. 2009;15:35–44. doi: 10.1016/j.ccr.2008.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fillies T, Werkmeister R, van Diest PJ, Brandt B, Joos U, Buerger H. HIF-1-alpha overexpression indicates a good prognosis in early stage squamous cell carcinomas of the oral floor. BMC Cancer. 2005;5:84. [DOI] [PMC free article] [PubMed]
- 29.Lidgren A, Hedberg Y, Grankvist K, Rasmuson T, Bergh A, Ljungberg B. Hypoxia-inducible factor 1alpha expression in renal cell carcinoma analyzed by tissue microarray. Eur Urol. 2006;50:1272–7. doi: 10.1016/j.eururo.2006.05.043. [DOI] [PubMed] [Google Scholar]
- 30.Vleugel MM, Greijer AE, Shvarts A, van der Groep P, van Berkel M, Aarbodem Y, et al. Differential prognostic impact of hypoxia induced and diffuse HIF-1alpha expression in invasive breast cancer. J Clin Pathol. 2005;58:172–7. doi: 10.1136/jcp.2004.019885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sun EC, Fears TR, Goedert JJ. Epidemiology of squamous cell conjunctival cancer. Cancer Epidemiol Biomark Prev. 1997;6:73–7. [PubMed] [Google Scholar]
- 32.Tuomaala S, Eskelin S, Tarkkanen A, Kivelä T. Population-based assessment of clinical characteristics predicting outcome of conjunctival melanoma in whites. Invest Ophthalmol Vis Sci. 2002;43:3399–408. [PubMed] [Google Scholar]
- 33.Yu GP, Hu DN, McCormick S, Finger PT. Conjunctival melanoma: is it increasing in the United States? Am J Ophthalmol. 2003;135:800–6. doi: 10.1016/S0002-9394(02)02288-2. [DOI] [PubMed] [Google Scholar]
- 34.Kirkegaard MM, Rasmussen PK, Coupland SE, Esmaeli B, Finger PT, Graue GF, et al. Conjunctival lymphoma--an international multicenter retrospective Study. JAMA Ophthalmol. 2016;134:406–14. doi: 10.1001/jamaophthalmol.2015.6122. [DOI] [PubMed] [Google Scholar]
- 35.Jeong W, Rapisarda A, Park SR, Kinders RJ, Chen A, Melillo G, et al. Pilot trial of EZN-2968, an antisense oligonucleotide inhibitor of hypoxia-inducible factor-1 alpha (HIF-1α), in patients with refractory solid tumors. Cancer Chemother Pharmacol. 2014;73:343–8. doi: 10.1007/s00280-013-2362-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.