Abstract
Introduction
Raising awareness of acute kidney injury (AKI) is an essential strategy for minimizing the burden of this lethal syndrome. The AKI Commission of the Latin American Society of Nephrology and Hypertension conducted an educational program based on networked learning.
Methods
Two online courses with similar methodologies were developed, 1 course for nephrologists and the other for primary care physicians (PCP). The courses were developed as a distance education, asynchronous online modality with multiple educational strategies: written lessons, videos, e-rounds, and clinical simulation. Knowledge gain was explored through a 10-question test before and after course completion.
Results
The course for nephrologists had 779 participants from 21 countries; 52% were male, and 46% were <35 years of age. Mean qualification increased from 5.87 to 8.01 (36% gain of knowledge). The course for PCPs had 2011 participants, 81% of whom were physicians. The time from graduation was <5 years in 52%. In both courses, clinical simulation was considered the best part and lack of time the main limitation for learning. Because 48% of the nephrologist course attendees were interested in AKI activities, a Latin American AKI Network site (RedIRA) composed of a brief review, a clinical forum, a self-assessment, and a bibliography on AKI was launched on a monthly basis in November 2016. To date there are 335 users from 18 countries.
Conclusions
Distance education techniques were effective for learning about AKI and are a potential tool for the development of a sustainable structure for communication, exchange, and integration of physicians involved in the care of patients with AKI.
Keywords: acute kidney injury, continuing medical education, networked learning
AKI is a devastating condition that affects more than 13 million persons per year at a global level, with the majority living in socioeconomically vulnerable regions,1 becoming an important public health issue, especially in the developing world.2 Continuing education targeting physicians and nonphysicians involved in the care of patients at risk or with established AKI is a key tool to raise awareness and to update knowledge, as proposed by the International Society of Nephrology (ISN) through the ISN 0by25 Initiative.2
The use of information and communication technologies (ICT) is constantly evolving. Innovations and more interactive and engaging strategies have been incorporated into educational programming,3, 4 enabling greater participation of physicians, including those from remote locations in developing countries.
In 2015, the Acute Kidney Injury Committee of the Latin American Society of Nephrology and Hypertension (AKI/SLANH) in partnership with EviMed Corporation implemented 2 different online courses targeting nephrologists and related specialists and primary care physicians.
Our aim is to describe the design, implementation, and results of these courses and to evaluate the impact that this educational tool has had on medical knowledge.
Methods
The course for nephrologists was taught over 7 weeks from 20 August to 7 October 2015. The target audience was Spanish- and Portuguese-speaking nephrologists and other related specialists, such as intensivists and internists, working across the Latin American region.
The objectives were that by the end of the course the participants would be able to do the following: (i) understand that AKI is a public health issue, (ii) recognize the importance of the identification and subsequent control of risk factors for AKI, (iii) realize the importance of an early diagnosis and timely response, (iv) know the different renal replacement therapies and appropriate criteria for their initiation and dose, and (v) recognize the potential adverse long-term outcomes associated with AKI and the relevance of a control strategy for prevention and rehabilitation.
The AKI/SLANH Committee designed the course curriculum and provided regional and international experts. EviMed Corporation provided a multidisciplinary team of communication and educational experts, system engineers, medical information specialists, and translators. The course was asynchronous, and a multifaceted educational approach was used to maximize opportunities for health care teams’ participation, comprising material evaluation, interaction and discussion, and contact among the participants.
To design the course program, a mixed-method approach for the assessment of the requirements was performed in March 2015. In the first component, qualitative data were obtained via semistructured telephone interviews with 12 experts from Argentina, Bolivia, Brazil, Chile, El Salvador, Mexico, Paraguay, Peru, the Dominican Republic, and Venezuela. The respondents provided their opinions about the organization and content of the courses. The second component was an electronic survey targeted to all members of SLANH and all participants from previous SLANH courses. A total of 355 participants were asked about topics to be included in the courses. Most of the experts and participants thought that in their country, many patients with AKI died without a diagnosis due to the lack of diagnostic tools or a paucity of knowledge of the importance of timely therapeutic management. In addition, the experts generally believed that patients needing renal replacement therapy (RRT) frequently did not receive it for a variety of reasons.
With this information, the organizing committee designed the final program of courses that included 5 sections: (i) recognition of AKI, (ii) risk and response, (iii) AKI in particular settings, (iv) renal replacement therapies, and (v) results. The program details are provided in Supplementary Table S1.
The course had a registration fee of US $150. The activities began with an on-site and online synchronous launch event held in Montevideo, Uruguay, on August 20, 2015, which was broadcast in Spanish and Portuguese throughout Latin America.
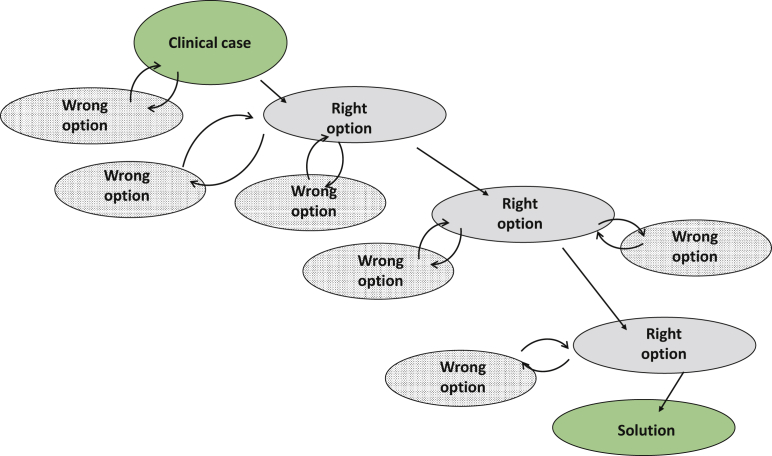
The course was developed as a distance education, asynchronous, online modality with multiple educational strategies. Reading resources, videos, and electronic rounds (e-rounds) on clinical cases were uploaded to the course’s Web-based platform. In addition, 2 clinical simulations using a custom tool developed with the School of Engineering, University of the Republic, Uruguay5 were used to provide applied learning through knowledge discovery and automatic feedback. This educational tool allows the definition of a workflow of possible decisions to be made by the student at each step of the process. Some are alternative paths (as there is not always just 1 right choice), allowing the participant to continue. Some are wrong, and after getting feedback the participant reconsidered the decision (Figure 1). The e-rounds were asynchronous discussion groups in both Spanish and Portuguese coordinated by tutors who were native speakers of both languages and who were specifically trained for the role. This modality allowed the course attendees to participate when it was convenient for them without a fixed schedule to access the e-round. The tutor interacted with participants during the forum and ended the e-round with a synthesis of the discussion and conclusions. The clinical case discussed in the e-round was related to the topic of the corresponding module. Before starting the course, the participants had to answer a 10-question test (pretest) that was repeated after the course (posttest). Questions were formulated to assess whether the participants had achieved the objectives of the course. The comparison of the main number of correct answers pre- and posttest is an approach to assess the gain of knowledge. The set of 10 questions is provided in Supplementary Table S2.
Figure 1.
Clinical simulation. Possible paths are shown.
The course workload totaled 30 hours over 7 weeks. Course evaluation, participation, and satisfaction were evaluated, and knowledge gains were quantified through the differences in the aforementioned pre- and posttests. Moreover, a commitment to change statements was requested from the participants at the end of the course to evaluate how the course affected their clinical practice. The requirements for a certificate of completion were accessing at least 70% of the study materials, passing at least 70% of the tests in each module, completing the clinical simulation, and participating in at least 50% of the discussion forums. The requirements for a certificate of participation were accessing the virtual campus, using at least 10 study materials, and/or actively participating in the clinical discussions. The Wilcoxon signed-rank test was used to compare pre- and posttest results.
Fifty experts from 11 countries, 2 from Europe (GR and FL), and 1 from the United States (RLM), were the faculty members as lecturers, authors of texts, and e-round tutors (Supplementary Table S3). Forty-seven Latin American experts were from 8 Latin American countries (Argentina, Bolivia, Brazil, Chile, Dominican Republic, Mexico, Peru, and Uruguay).
The course for PCPs and allied health care workers took place over 4 weeks from November 16 to December 16, 2015. The target population was Spanish-speaking family and preventive medicine physicians, geriatrics, emergency medicine doctors, and nurses. For organizational and economic reasons, the course was offered only in Spanish.
The objectives were that at the end of the course the participants would be able to do the following: (i) understand that AKI is a public health issue, (ii) acquire tools for identifying risk factors for AKI and implementing a preventive strategy, (iii) gain skills to achieve an early and timely diagnosis and to provide adequate initial treatment, and (iv) be aware of the relevant role of the primary care team in the reference/counterreference system of patients with AKI.
The methodology was similar to that used in the course for nephrologists, and the course program was adapted to the target audience. The course was free of charge. The Pan American Health Organization (PAHO)/World Health Organization [WHO]) collaborated for the diffusion of the course among PCPs.
Finally, a satisfaction survey addressed to the nephrologists’ audience was conducted, including, among other questions, whether the registrants would be willing to participate in future educational and research activities organized by SLANH. Given that 48% of the participants expressed their agreement, a RedIRA site was developed and launched in November 2016. The RedIRA is composed of a review of a topic of interest, a clinical forum, a self-assessment test, and a bibliography. It is updated monthly.
Results
Course for Nephrologists
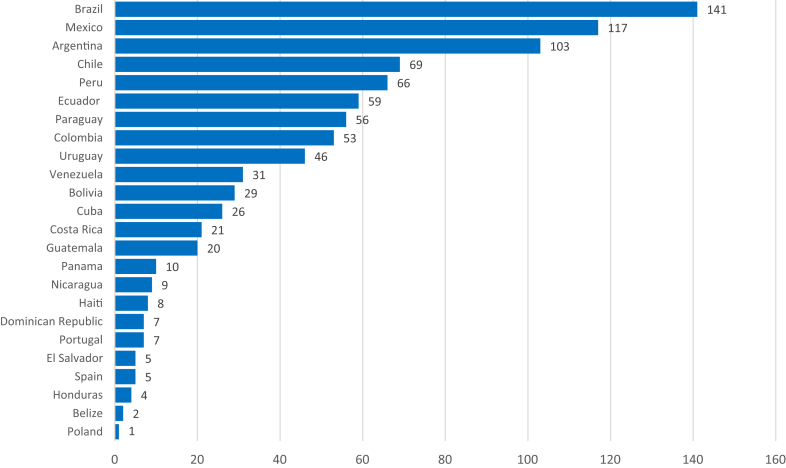
A total of 895 health care professionals from 21 Latin American countries registered for the course, of whom 779 (87%) actively participated (Figure 2). Among them, 405 (52%) were male, and the majority (56%) were less than 45 years old. Physicians prevailed (83%), and 74% of the participants were nephrologists. No intensivists registered for the course. The number of video and text entries by topic is shown in Supplementary Figure S1. A total of 453 participants completed the clinical simulation. Overall, 383 of the 779 participants approved the course according to the aforementioned approval criteria. Finally, the pretest and posttest were completed by 355 participants. The mean number of right answers was 5.87 and 8.01, respectively (P < 0.05), which can be considered as a gain knowledge equivalent to 36%. A survey revealed that the best-ranked educational tools were the clinical simulation (91%), videoconferences (88%), texts (85%), and e-rounds (78%). The platform was considered user-friendly by 80% of the participants. As limitations to learning, time constraints were indicated most frequently (48%), followed by Internet connection problems (16%), limited computer skills (5%), and the online modality (3%). Overall, 28% of the participants experienced no limitations. The best parts of the course were considered the clinical simulation (60%), the topic and the approach (56%), the educational tools (39%), and the methodology used (34%). Of the participants, 65% reported that the course had no negative aspects. A variety of issues, such as interactions with colleagues, clinical simulation, navigability of the website, educational tools and materials, subject and approach, educational methodology, and system support were considered negative by less than 8% of the participants. Only 1 of 394 participants considered the presence of commercial bias.
Figure 2.
Course for nephrologists. Number of participants per country.
Course for Primary Care Physicians
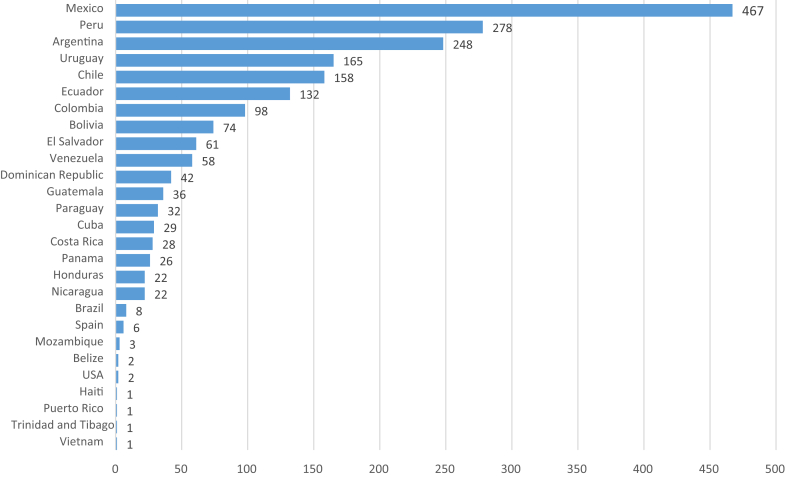
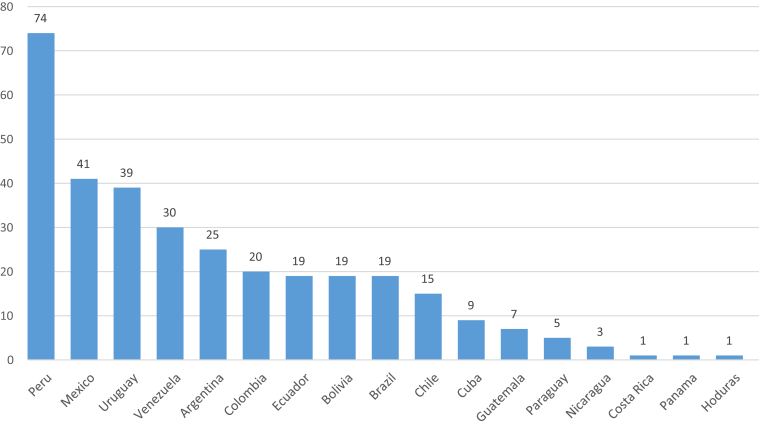
A total of 2011 persons participated in the course, of whom 1221 (61%) were female. Figure 3 shows the distribution of the participants by country. Overall, 79% were physicians, 14% were nurses, and 7% were other professionals. A total of 52% were 5 or fewer years from graduation, 11% were between 16 and 25 years, and 8% were more than 25 years from graduation. Overall, 28% of the participants did not provide this information. The majority (67%) worked at public health institutions. The topics that aroused the greatest interest according to the number of entries of videos and texts are depicted in Supplementary Figure S2. A total of 1036 participants completed the clinical simulation. Only 121 answered the satisfaction survey; of these, 118 were satisfied or very satisfied. Clinical simulation, videoconferences, and texts were ranked as the best components of the course. Navigability was considered user-friendly by 78% of the participants. The main limitations to learning were a lack of time (33%), poor Internet connection (18%), the interactive modality (14%), and discomfort in dealing with computer tools (9%). Similar to the nephrologists, a considerable number of participants (35%) reported no limitations to learning. The best-ranked aspects of the course were the subject and the approach for 76 participants (63%), the clinical simulation for 62 (51%), the methodology for 53 (44%), and the educational tool for 50 (41%). The course had no negative aspects for 77 participants (64%). Interaction with colleagues, support, the subject and approach, clinical simulation, educational tools, navigability, and the participation of many countries were reported as negative aspects by a small percentage of the respondents. The presence of commercial bias was related only by 2% of the participants. Comparative characteristics of both courses are summarized in Supplementary Table S4.
Figure 3.
Participants per country in the course for primary care physicians.
Latin American AKI Network
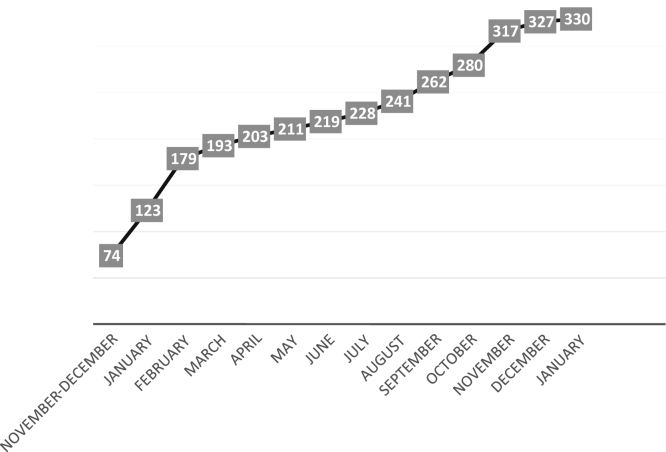
As a corollary to the interest in AKI shown by many nephrologists in Latin America, SLANH supported and increased the strategy of its AKI Committee to renew and refresh AKI knowledge and skills of Latin American nephrologists through the creation of a forum for exchange, communication, education, and epidemiological research. The Latin American AKI Network (RedIRA in Spanish; www.redira.slanh.net) was launched in November 2016 with 74 participants, and now has about 330 (Figure 4). The website is edited monthly and consists of the following 4 sections: (i) the Topic of the Month: this is a concise update of a topic of interest related to AKI. Priority is given to forms of AKI seen in the region (general epidemiology, AKI in infectious communicable diseases, poisonous animals, accidents, herbalism, etc.). The list of covered topics is provided in Table 1. (ii) Clinical Forums: in these forums, clinical cases and vignettes are offered to participants for analysis with 4 or 5 key questions for discussion. (iii) Self-Assessment Test: in this test, a clinical case or a controversial aspect of AKI is presented followed by single-best-answer questions. The correct answers are available separately so the participants can evaluate their knowledge. (iv) Bibliography of Interest: two or 3 free open-access references considered of relevance by the editorial team are uploaded each month. In addition, a section called “Did you know that?” consisting of 2 or 3 vignettes extracted from articles of interest with the respective references is published every other month. An e-mail is sent to the network subscribers every 15 days. At present, 330 persons participate in the RedIRA. Slightly more than half (52.3%) are male. The mean age is 42.2 ± 11.9 years. Figure 5 presents the distribution of users in 18 countries. Most users work in cities (93.1%), in the public health system (41.1%), or in both public and private systems (40.5%). A user survey found that the vast majority reported satisfaction with the site, which fulfilled their expectations (87% rated the network as good or very good). The main cause of dissatisfaction was limited student−teacher interaction. The most useful sections were the Clinical Forums (83%) and the Topic of the Month (73%). Approximately half of the respondents found the self-evaluation and the AKI bibliography interesting.
Figure 4.
Number of RedIRA (a Latin American AKI Network site) users.
Table 1.
List of topics of the month
| Topic | Speaker |
|---|---|
| AKI in malaria and dengue | Mauricio Younes-Ibrahim |
| Risk reduction of iatrogenic AKI | Raúl Lombardi |
| AKI in natural disasters | Abdías Hurtado, Sandra Rodríguez, Ronald Weinstein |
| Mesoamerican nephropathy and AKI | Alejandro Ferreiro |
| The ISN 0by25 initiative | Giuseppe Remuzzi |
| AKI after cardiac surgery | Alejandro Ferreiro |
| Acute-on-chronic kidney disease | Guillermo Rosa-Diez |
| Cardiorenal syndrome | Luis Yu |
| Rhabdomyolysis and AKI | Alejandro Ferreiro |
| AKI in hypothyroidism | Mauricio Younes-Ibrahim |
| Beginning and ending of RRT in AKI | Emanuel Burdmann |
| Drug-induced AKI | Antonio Seguro |
| Natural herbs and AKI | Rolando Claure-Del Granado |
| The new paradigm of AKI: from the hospital to community | Raúl Lombardi |
| End-of-life care in AKI | Raúl Lombardi |
Figure 5.
Distribution of users per country.
Discussion
The paradigm of AKI is transitioning from the classic pattern of a life-threatening condition that affects patients frequently hospitalized in the intensive care unit to a public health issue, due to its rising frequency, the burden associated with early and late morbidity and mortality, and increasing costs.6 On the other hand, the fact that AKI is potentially avoidable poses a challenge to deploy a strategy to prevent its onset.
Caring for patients at risk for AKI is complex and involves a variety of physicians and other health care workers such as nurses, paramedical professionals, and social workers. The nephrologist is not often present to prevent AKI or to intervene as it develops. Therefore, the nephrologist’s main role is to educate caregivers who effectively face the variety of conditions that can lead to kidney injury and subsequent kidney failure. Primary care physicians, generalists, rescue teams, and paramedical workers among others are the targets of an educational strategy to recognize and to manage factors leading to kidney injury.
The continuous progress in the knowledge of AKI means that it is essential for nephrologists and other health care professionals who care for AKI patients to remain updated. Distance learning is an extraordinary tool for enhancing networked learning and the effectiveness of continuing medical education. Latin America is an extended and geographically heterogeneous region but has acceptable Internet connectivity and only 2 main languages (Spanish and Portuguese). Those factors make the development of online education activities possible, avoiding the cost of logistics, transportation, and hotel expenses necessary for face-to-face events, while engaging participants and experts in a more horizontal and prolonged exchange of knowledge and experiences.
In 2013, the Latin American Society of Nephrology and Hypertension launched a continuing medical education program in partnership with EviMed, a company specializing in networked learning. In 2015, the AKI Commission of SLANH implemented a course on AKI in accordance with the proposal of Raising Awareness on AKI of the 0by25 ISN Initiative.2
There is insufficient previous information to compare our results, but some data are consistent with the proposed objectives of the course. The number of participants can be considered acceptable, which represented approximately 12% of all nephrologists in Latin America, higher than in previous courses from SLANH-EviMed7 and about 30% of SLANH’s members, the organization that carried out the course. The participants’ profiles were as expected: young or middle-aged health care workers, often employed in the public health system. Considering the country distribution, the most populated countries such as Brazil, Mexico, and Argentina contributed higher numbers of participants. However, this profile changes when the number of participants is related to the number of nephrologists in each country. As an example, the number of participants from Central America represented 35% of the total number of nephrologists.
Evaluation of knowledge acquisition implies the design of a predefined and complex system to assess the process and results of learning. If we consider Moore’s framework for evaluating continuing medical education,8 we reach only level 3 of 7 (that is, learning), and only to a limited extent, as the 10-question test is not sufficient to test the gain of knowledge throughout the course. However, the use of the evaluation tool commitment to change intends to cover to a certain extent level 5 (that is, performance), because this tool correlates to changes in clinical performance.9 In the present course, the mean gain of knowledge was greater than observed in previous courses from EviMed and SLANH,4, 7, 10 which could be considered satisfactory. How new knowledge affects clinical practice, which is the final goal of education, is difficult to evaluate.
Three relevant achievements of this experience should be noted. First, to date, this is the first educational initiative on AKI with such characteristics in Latin America and possibly globally. The design of the course, the number and qualifications of the faculty, the multifaceted approach, the educational tools used, the scope, and the adherence and satisfaction of the participants should be highlighted as accomplishments that validated this educational strategy. Second, the number of participants in the PCP course, possibly due to the collaboration with the Pan American Health Organization for its distribution and the fact that it was cost free, reveal that AKI per se arouses the interest of primary care professionals. To the best of our knowledge, this is the first time that 2 medical disciplines such as nephrology and primary care medicine have shared an educational activity based on a strategy of complementation and interaction among professionals who treat AKI patients. Third, this course demonstrated the possibility of leveraging new and advanced levels of organization due to the motivation inspired by the educational intervention. RedIRA is an example of a program with a sustainable structure for communication, exchange, and integration of those who care for AKI patients.
Lack of time was pointed out as the main limitation. This is mainly due to the conditions of medical work in the region, where multiemployment with high demand of time is very frequent, particularly among young practitioners. Reduction of course time does not seem to be a solution because, in our experience, less than 4 weeks limits learning results. Finally, the evaluation of how these courses affect clinical practice is a challenge that remains to be resolved.
In conclusion, these interactive, asynchronous, online courses are a valuable and successful tool for continuing medical education in Latin America, reducing heterogeneity in access to training across countries. However, reliable information is lacking regarding the impact of these courses on long-term knowledge retention and the ultimate benefit on quality of health. The application of distance education techniques has proved to be effective, not only in terms of primary learning objectives but also as a potential tool for the development of a sustainable structure for communication, exchange, and integration of physicians and allied professionals involved in the care of patients with AKI. This educational program demonstrated the feasibility of an international and interprofessional course on AKI providing quality education to health care providers.
Disclosure
AM is CEO of EviMed; FO is a consultant of EviMed. All the other authors declared no competing interests.
Acknowledgments
The authors thank the Pan American Health Organization and Dr. Pedro Ordúñez for the dissemination of the course.
Footnotes
Figure S1. Entries by topic (nephrologist course).
Figure S2. Entries by topic (primary care physician course).
Table S1. Program of the course.
Table S2. Questions of pre- and posttest.
Table S3. Faculty.
Table S4. Comparative table of the course’s features.
Supplementary material is linked to the online version of the paper at www.kireports.org.
Supplementary Material
Entries by topic (nephrologist course).
Entries by topic (primary care physician course).
Program of the course.
Questions of pre- and posttest.
Faculty.
Comparative table of the course’s features.
References
- 1.Lewington A.J., Cerdá J., Mehta R.L. Raising awareness of acute kidney injury: a global perspective of a silent killer. Kidney Int. 2013;84:457–467. doi: 10.1038/ki.2013.153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mehta R.L., Cerdá J., Burdmann E.A. International Society of Nephrology’s 0by25 initiative for acute kidney injury (zero preventable deaths by 2025): a human rights case for nephrology. Lancet. 2015;385:2616–2643. doi: 10.1016/S0140-6736(15)60126-X. [DOI] [PubMed] [Google Scholar]
- 3.Margolis A., Parboosingh J. Networked learning and network science: potential applications to health professionals' continuing education and development. J Contin Educ Health Prof. 2015;35:211–219. doi: 10.1002/chp.21295. [DOI] [PubMed] [Google Scholar]
- 4.Cohen H., Margolis A., González N. Implementation and evaluation of a blended learning course on gastroesophageal reflux disease for physicians in Latin America. Gastroenterol Hepatol. 2014;37:402–407. doi: 10.1016/j.gastrohep.2014.01.004. [in Spanish] [DOI] [PubMed] [Google Scholar]
- 5.Medeiros N, Pérez G, Sniadover N, et al. Generador de casos interactivos. Presented at MoodleMoot Uruguay 2011. Available at: http://www.moodlemoot.org.uy/moodlemoot_2011/moodlemoot/moodlemootuy2011_submission_26.pdf. Accessed April 23, 2018.
- 6.Lameire N.H., Bagga A., Cruz D. Acute kidney injury: an increasing global concern. Lancet. 2013;382:170–179. doi: 10.1016/S0140-6736(13)60647-9. [DOI] [PubMed] [Google Scholar]
- 7.Margolis A., Gonzalez-Martinez F., Noboa O. Online continuing medical education for the Latin American nephrology community. Stud Health Technol Inform. 2015;216:372–375. [PubMed] [Google Scholar]
- 8.Moore D.E., Jr., Green J.S., Gallis H.A. Achieving desired results and improved outcomes: integrating planning and assessment throughout learning activities. Contin Educ Health Prof. 2009;29:1–15. doi: 10.1002/chp.20001. [DOI] [PubMed] [Google Scholar]
- 9.Wakefield J., Herbert C.P., Maclure M. Commitment to change statements can predict actual change in practice. J Contin Educ Health Prof. 2003;23:81–93. doi: 10.1002/chp.1340230205. [DOI] [PubMed] [Google Scholar]
- 10.Medina-Presentado J.C., Margolis A., Teixeira L. Online continuing interprofessional education on hospital-acquired infections for Latin America. Braz J Infect Dis. 2017;21:140–147. doi: 10.1016/j.bjid.2016.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Entries by topic (nephrologist course).
Entries by topic (primary care physician course).
Program of the course.
Questions of pre- and posttest.
Faculty.
Comparative table of the course’s features.