Abstract
Objective
Avascular necrosis (AVN) of the femoral head is a painful, progressive disease that can lead to limited mobility and early hip replacement. Autologous stem cell implantation into the necrotic lesion of the femoral head has been described, on the basis that patients with AVN have a reduced number of stem cells in the marrow. In this study, we aim to describe our technique for decompression of the hip with autologous implantation of stem cells for AVN of the femoral head, as well as retrospectively analyze our results.
Methods
The records and imaging of patients with avascular necrosis of the femoral head treated by a single surgeon were retrospectively reviewed. All patients were treated with the combination of core decompression with autologous stem cell implantation from the iliac crest. Preoperatively, demographic information, stage of AVN per Association Research Circulation Osseous (ARCO) classification on magnetic resonance imaging and radiograph, and visual analogue pain scores (VAS) of the hip were recorded. Postoperatively, VAS were recorded and imaging was reviewed for progression of AVN or evidence of femoral head collapse. Statistical analysis was conducted comparing pre and postoperative VAS scores.
Results
Overall, we treated 43 hips in 28 patients with autologous stem cell implantation, with an average follow up of 16 months. Patients ranged from ARCO Ia to ARCO IIc classification of AVN. The average pre-operative visual analogue scale (VAS) of pain was 7.8. Post operatively, the average VAS score decreased to 2.5 (p < 0.0001), with 78% of patients reporting at least a 50% decrease in pain. 40 of the 43 operatively treated hips showed no radiologic progression of the disease during the follow up period, while 3 of the 43 hips had evidence of femoral head collapse and needed subsequent total hip arthroplasty at an average of 17 months after the initial decompression.
Conclusion
Our findings indicate that hip compression with autologous stem cell implantation for AVN of the femoral head provides significant symptomatic relief and may be beneficial in arresting progression of disease.
Keywords: Avascular necrosis, Autologous bone marrow implantation, Stem cells, Femoral head
1. Introduction
Avascular necrosis (AVN; or osteonecrosis) of the femoral head is an unrelenting, progressive disease that may affect an estimated 10,000–20,000 individuals yearly in the United States.1 Resulting from a number of etiologies, including steroid use, alcohol abuse, sickle cell disease, and idiopathic, AVN can lead to a painful and early collapse of the femoral head if left untreated. The pathogenesis of this disease stems from diminished blood supply to the femoral head from the circumflex arteries, leading to necrosis of the bone. In fact, several studies have suggested that thrombosis and osteonecrosis may be related and share similarities in pathophysiology. Björkman et al found that thromboembolic events were more common in patients with idiopathic avascular necrosis of the femoral head versus those patients with alcohol or steroid induced AVN.2 Hypercoagulability has been suggested as a risk factor for idiopathic AVN of the femoral head,3 and Glueck et al found correlations between inherited thrombophilia and hypofibrinolysis and femoral head osteonecrosis.4 Similar avascular conditions exist in the knee5 and humeral head.6 After collapse of the femoral head, treatment is generally limited to total hip arthroplasty (THA); in fact, it is responsible for 5–12% of all THAs in the United States.7 However, because AVN typically presents in the late 30s-early 40 s of age,8,= THA is not an ideal option, as the implants will likely need revision over the patient’s life.9 Although THA after femoral head collapse has historically had poor outcomes,10 recent advancements in implant technology have made this a viable option for patients with collapse.11 Nevertheless, techniques to preserve the native hip and prevent femoral head collapse remain highly sought after.
In the precollapse stage of AVN, surgical options exist in order to salvage the femoral head and decrease the risk of hip replacement. Previously, this has been limited to simply core decompression of the femoral head, with some success.12 However, over the two decades, there have been a number of studies showing that core decompression augmented with autologous concentrated bone marrow from the iliac crest is successful in improving outcomes in early stage AVN.13, 14, 15, 16, 17 The largest study, from Hernigou et al in 2002, showed radiographic arrest of disease and prevented the need for THA in the vast majority of patients.12 More recent studies have shown similar results.14, 15, 16, 17 Patients with osteonecrosis of the femoral head typically have fatty infiltration of the bone marrow and a reduced number of stem cells.18 Therefore, it follows that autologous transfer of stem cells, typically from the iliac crest, combined with core decompression would promote regeneration of stem cells and improve vascularity in the femoral head. In this paper, we describe our technique for core decompression augmented with bone marrow aspirate for ARCO Stage I or II avascular necrosis of the femoral head, and review the outcomes of this procedure done on 43 hips at our institution.
2. Materials and methods
We retrospectively reviewed the electronic medical records and imaging of a consecutive series of patients who were treated by the senior author for AVN of the femoral head over a three-year period at our institution. Included patients had AVN of either a single or both hips and graded to be IA through IIC by the Association Research Circulation Osseous (ARCO) classification. All patients were treated with the combination of core decompression with autologous stem cell implantation from the iliac crest per the technique described by Hernigou et al.12 Overall, 43 hips in 28 patients were included in the study. Demographic information included age, gender, and Body Mass Index (BMI) (Table 1). The etiology of AVN was also noted (Table 2). Stage of AVN per the ARCO classification was determined by pre-operative radiographs and magnetic resonance imaging. Patient’s visual analog pain scores (VAS scale 0–10, with 10 being worst pain) were recorded pre- and post-operatively. From the operative record, any concurrent procedure, including contralateral THA, subchondroplasty procedure, and hip arthroscopy with labral repair, was noted. Statistical analysis included Student’s t-test run using Microsoft Excel (Microsoft Office 2013). The Institutional Review Board reviewed and approved this study prior to initiation.
Table 1.
Patient Demographics.
| N (%) | |
|---|---|
| Gender | |
| Male | 13 (46.4) |
| Female | 15 (53.6) |
| Age | |
| Range | 22-61 |
| Average | 40.5 |
| BMI | |
| Normal Weight | 8 (28.6) |
| Overweight | 16 (57.1) |
| Obese | 4 (14.3) |
| Average BMI | 29 |
Table 2.
Clinical Characteristics.
| N (%) | |
|---|---|
| Laterality | |
| Right | 6 |
| Left | 7 |
| Bilateral | 15 |
| AVN Etiology | |
| Steroid use | 15 (53.6) |
| Alcohol abuse | 5 (17.9) |
| Sickle cell disease | 3 (10.7) |
| Idiopathic | 2 (7.1) |
| Multiple causes | 3 (10.7) |
| ARCO Classification System Stage | |
| IA | 3 (10.7) |
| IB | 4 (14.3) |
| IC | 1 (3.6) |
| IIA | 8 (28.6) |
| IIB | 3 (10.7) |
| IIC | 9 (32.1) |
| Complications | |
| Femoral head collapse requiring THA | 3 (6%) |
| Post-operative deep venous thrombosis | 1 (3.6) |
2.1. Surgical technique
The patient is placed supine on a Jackson table under general anesthesia, and the patient is draped in such a manner that allows both anterior-posterior and frog-leg lateral views of the femoral head. A full surgical technique can be found online as described by the senior authorA. Fluoroscopy is used during the decompression of the hips. Both the iliac crests are included in the prep. A small, 2–3 mm incision is be made over one (or both) of the iliac crests. The incision runs proximal-lateral to the anterior-superior iliac spine (ASIS), and the trajectory of the aspiration will be aimed for the supra-acetabular area. Anticoagulant-coated trocars are malleted through the outer pelvis crest cortex and advanced between the two tables of the ilium. Bone marrow can then be aspirated into 10 ml aliquots to decreases chance of cell lysis with large volume aspiration under high negative pressure. 120 cc of bone marrow aspirate (BMA) was withdrawn for the unilateral hip, and 240cc withdrawn for bilateral hip cases (Fig. 1a). This yields 12 and 24 ccs of bone marrow concentrate, respectively, for unilateral and bilateral hip procedures. 60 ccs of whole blood is also aspirated from a peripheral vein prior to anesthesia for both unilateral and bilateral hips, yielding platelet rich plasma (PRP) in the amount of 12 ccs for a single hip or 6 ccs for each hip in a bilateral procedure. After collection, the BMA and whole blood are spun down for 15 min using a dedicated centrifuge system (Zimmer Biomet, Inc., Warsaw, IN).
Fig. 1.
(a) A demonstration of the aspiration technique of bone marrow aspirate (BMA) from the supra-acetabular area bilaterally. (b) Instrumentation of the trocar into the femoral head. The use of fluoroscopy during malleting will help ensure proper placement of the trocar. (c) Injection of the bone marrow aspirate into the femoral head.
While the concentrate is being prepared in the centrifuge, the core decompression of the hip is started. A 1 cm incision is made laterally over the femur, just below the vastus ridge. The entry point of the trochar is kept above the level of the lesser trochanter. The instrument is malleted at 90 degrees to the cortex in order to seat it. The trochar is then directed towards the AVN lesion in the femoral head. Upon entering the lesion, a change of pitch should be noted, and a tactile change is appreciated. Frequent use of fluoroscopy during the malleting will help guide the instrument into the necrotic lesion (Fig. 1b). After core decompression, the bone marrow concentrate is injected into the lesion (Fig. 1c). After injection, the trochar is withdrawn, and the cancellous tracks is closed off using bone graft. A subchondroplasty procedure was used for stage I B/C and II B/C lesions. Postoperatively, patients were allowed to bear weight as tolerated, with aspirin and a statin for anticoagulation. Follow up appointments were at 2 weeks, 6 weeks, 3 months, 6 months, 1 year, and 2 years. Radiographs were obtained at 6 weeks, 3 months, and 6 months, and 1 year post-operatively. MRIs were taken at 6 months and 1 year.
3. Results
Hip decompression with autologous concentrated bone marrow aspiration was performed on 28 patients with 43 affected hips. Our study included 13 males and 15 females, with an average age of 40.1 and an average BMI of 29 (Table 1). The most common etiology of AVN was corticosteroid use at 53.6 percent (n = 15), but there were a variety of causes (see Table 2). ARCO classifications ranged from stage IA to IIC (Table 2). Five patients also received subchondroplasty at the time of surgery, while two patients were treated with concomitant hip arthroscopy for femoroacetabular impingement/labral pathology. Eight patients (28.6%) had a THA performed under the same anesthetic for collapse of a contralateral femoral head.
Patients were followed for an average of 16 months. Postoperatively, three patients had collapse of the femoral head after the decompression procedure and were converted to THA (6%) at a mean time of 17.6 months after the decompression. The remainder of patients showed no overt progression of AVN in post-operative imaging (n = 25). One patient experienced a deep vein thrombosis. There were no post-operative infections or wound healing complications.
A comparison was made between pre-operative and post-operative VAS pain scores. The pre-operative average score was 7.8, and the post-operative average score was 2.5 (p < 0.0001; Table 3). 86% (n = 24) of patients reported at least a 2 point decrease in VAS pain scores after the operation, and 78% of patients (n = 22) reported a greater than 50% improvement in pain scores after the operation.
Table 3.
Pre and Post Operative Hip Pain Scores (0–10).
| Average | P value | |
|---|---|---|
| Pre Op | 7.8 | |
| Post Op | 2.5 | |
| Average Improvement | 5.11 | <0.0001 |
| Patients with Minimum 2 Point Improvement | 86% (n = 24) |
4. Discussion
We here present a consecutive series of patients with pre-collapse (ARCO Stage I and II) femoral head AVN lesions treated with core decompression and biologic augmentation. Our results treating pre-collapse AVN of the femoral head with decompression augmented by autologous concentrated bone marrow injection reflect the results of other case series and randomized control trials.13, 14, 15, 16, 17 Physiologically, the goal of this procedure is to stimulate new bone formation and replace the bone marrow of the femoral head with viable, new stem cells, as patients with AVN have been shown to have a decreased stem cell population in their area of necrosis.5,18 Compared to only hip decompression, the addition of concentrated bone marrow has been shown to improve clinical outcomes such as pain and function and may retard the radiographic progression of disease.14 This was reflected in our patients as well, as 86% (n = 24) of our patients experienced at least a 2-point decrease in pain VAS scores after the operation. A two point difference in pain on the visual analog scale has been established by Tubach et al19 as the minimal clinically important difference for hip osteoarthritis. 78% of our patients (n = 22) experienced a 50% improvement in postoperative pain, with the average pain score significantly dropping from 7.8 to 2.5 after the operation. Twenty-five patients had no evidence of progression of disease on imaging (Fig. 2, Fig. 3), while three patients did experience collapse of the femoral head and went on to require THA. Of note, all three patients who failed the core decompression treatment had a BMI of over 35 and an ARCO stage of IIa, IIa, and IIc, respectively. Body mass index has not been reported to affect outcomes for decompression augmented by autologous concentrated bone marrow injection previously, and while our sample size is too low to draw any statistical conclusions, this trend should be investigated in future studies.
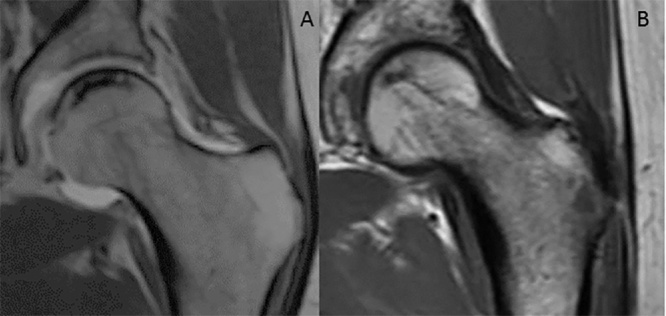
Fig. 2.
A magnetic resonance imaging slice of femoral head osteonecrosis preoperatively (A) and the partial regression of the same lesion two years postoperatively (B).
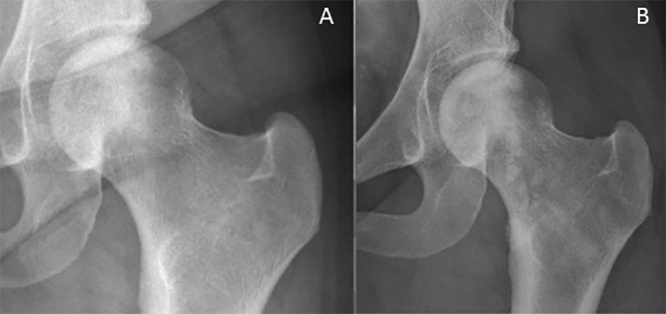
Fig. 3.
A plain radiograph of femoral head osteonecrosis preoperatively (A) and the arrest of the same lesion 14 months postoperatively (B).
As a retrospective review, our study carries the limitations that accompany such a study. Additionally, our patient population had varied causes of their AVN, including corticosteroid use (n = 15), alcohol (n = 5), sickle cell disease (n = 3), and multiple causes (n = 2). Demographically, our patients had a wide range of ages and BMIs, as well. Perhaps our greatest limitation is the lack of a control group, as we could not compare our procedure to either the natural history of AVN or to hip decompression only. Ongoing prospective studies will inform the utility of control populations in the management of AVN by core decompression. The sample size and period of follow up are other study limitations. Strengths of our study include all patients treated with a consistent operation by a single surgeon who has completed a significant number of these operations and is experienced in the technique and this philosophy of core decompression. Each operation was done at the same hospital, with the same preparation and draping, and all patients followed the same post operation protocol. There was a minimum of 12 ccs of concentrated bone marrow injected into the necrotic lesion in each femoral head, and all instruments used were from a single company (Zimmer Biomet).
5. Conclusion
Our study adds to the growing body of literature that femoral head core decompression combined with autologous bone marrow transplantation is a safe and effective way to treat early-stage AVN of the hip. Our patients experienced no serious complications, and 78% had significant pain relief. Of note, the 6% (n = 3) of patients who did fail this treatment did have a BMI over 35, something that should be investigated in future studies. Our institution is currently enrolling in a randomized clinical trial to further analyze the efficacy of this operation. For patients with ARCO stage I or II of the femoral head, hip core decompression combined with autologous bone marrow transplant appears to be a viable treatment option to provide symptomatic relief and perhaps arrest progression of this disease.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interest
The authors have no competing interests to declare.
Contributor Information
Nakul S. Talathi, Email: nakul.talathi@uphs.upenn.edu.
Atul F. Kamath, Email: atul.kamath@uphs.upenn.edu.
References
- 1.Lau R.L., Perruccio A.V., Evans H.M., Mahomed S.R., Mahomed N.N., Gandhi R. Stem cell therapy for the treatment of early stage avascular necrosis of the femoral head: a systematic review. BMC Musculoskelet Disord. 2014;15:156. doi: 10.1186/1471-2474-15-156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Björkman A., Svensson P.J., Hillarp A., Burtscher I.M., Rünow A., Benoni G. Factor V leiden and prothrombin gene mutation: risk factors for osteonecrosis of the femoral head in adults. Clin Orthop Relat Res. 2004;(August(425)):168–172. PubMed PMID: 15292803. [PubMed] [Google Scholar]
- 3.Jones J.P., Jr Intravascular coagulation and osteonecrosis. Clin Orthop. 1992;277:41–53. [PubMed] [Google Scholar]
- 4.Glueck C.J., Freiberg R.A., Wang P. Heritable thrombophilia-hypofibrinolysis and osteonecrosis of the femoral head. Clin Orthop Relat Res. 2008;466(May(5)):1034–1040. doi: 10.1007/s11999-008-0148-0. Epub 2008 Mar 19. PubMed PMID: 18350351; PubMed Central PMCID: PMC2311469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Marcacci M., Andriolo L., Kon E., Shabshin N., Filardo G. Aetiology and pathogenesis of bone marrow lesions and osteonecrosis of the knee. EFORT Open Rev. 2017;1(March,13 (5)):219–224. doi: 10.1302/2058-5241.1.000044. eCollection 2016 May. PubMed PMID: 28461951; PubMed Central PMCID: PMC5367544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Makihara Takeshi, Yoshioka Tomokazu, Sugaya Hisashi, Yamazaki Masashi, Mishima Hajime. Autologous concentrated bone marrow grafting for the treatment of osteonecrosis of the humeral head: a report of five shoulders in four cases. Case Rep Orthop. 2017;2017 doi: 10.1155/2017/4898057. Article ID 4898057, 8 pages. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mont M.A., Jones L.C., Hungerford D.S. Nontraumatic osteonecrosis of the femoral head: ten years later. J Bone Jt Surg Am. 2006;88(May(5)):1117–1132. doi: 10.2106/JBJS.E.01041. Review. Erratum in: J Bone Joint Surg Am. 2006 Jul;88(7):1602. Dosage error in article text. PubMed PMID: 16651589. [DOI] [PubMed] [Google Scholar]
- 8.Lavernia C.J., Sierra R.J., Grieco F.R. Osteonecrosis of the femoral head. J Am Acad Orthop Surg. 1999;7(July-August(4)):250–261. doi: 10.5435/00124635-199907000-00005. Review. PubMed PMID: 10434079. [DOI] [PubMed] [Google Scholar]
- 9.Hernigou P., Trousselier M., Roubineau F. Stem cell therapy for the treatment of hip osteonecrosis: a 30-year review of progress. Clin Orthop Surg. 2016;8(March (1)):1–8. doi: 10.4055/cios.2016.8.1.1. Epub 2016 Feb 13. Review. PubMed PMID: 26929793; PubMed Central PMCID: PMC4761591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cornell C.N., Salvati E.A., Pellicci P.M. Long-term follow-up of total hip replacement in patients with osteonecrosis. Orthop Clin North Am. 1985;16(October(4)):757–769. PubMed PMID: 4058901. [PubMed] [Google Scholar]
- 11.Issa K., Pivec R., Kapadia B.H., Banerjee S., Mont M.A. Osteonecrosis of the femoral head: the total hip replacement solution. Bone Jt J. 2013;95-B(November (11 Suppl A)):46–50. doi: 10.1302/0301-620X.95B11.32644. Review. PubMed PMID: 24187351. [DOI] [PubMed] [Google Scholar]
- 12.Wang G.J., Dughman S.S., Reger S.I., Stamp W.G. The effect of core decompression on femoral head blood flow in steroid-induced avascular necrosis of the femoral head. J Bone Jt Surg Ser A. 1985;67(no. 1):121–124. [PubMed] [Google Scholar]
- 13.Hernigou P., Beaujean F. Treatment of osteonecrosis with autologous bone marrow grafting. Clin Orthop Relat Res. 2002;(December;(405)):14–23. doi: 10.1097/00003086-200212000-00003. PubMed PMID: 12461352. [DOI] [PubMed] [Google Scholar]
- 14.Tabatabaee R.M., Saberi S., Parvizi J., Mortazavi S.M., Farzan M. Combining concentrated autologous bone marrow stem cells injection with core decompression improves outcome for patients with early-stage osteonecrosis of the femoral head: a comparative study. J Arthroplasty. 2015;30(September (9 Suppl)):11–15. doi: 10.1016/j.arth.2015.06.022. [DOI] [PubMed] [Google Scholar]
- 15.Daltro G.C., Fortuna V., de Souza E.S. Efficacy of autologous stem cell-based therapy for osteonecrosis of the femoral head in sickle cell disease: a five-year follow-up study. Stem Cell Res Ther. 2015;29(May(6)):110. doi: 10.1186/s13287-015-0105-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sen R.K., Tripathy S.K., Aggarwal S., Marwaha N., Sharma R.R., Khandelwal N. Early results of core decompression and autologous bone marrow mononuclear cells instillation in femoral head osteonecrosis: a randomized control study. J Arthroplasty. 2012;27(May(5)):679–686. doi: 10.1016/j.arth.2011.08.008. [DOI] [PubMed] [Google Scholar]
- 17.Zhao D., Cui D., Wang B. Treatment of early stage osteonecrosis of the femoral head with autologous implantation of bone marrow-derived and cultured mesenchymal stem cells. Bone. 2012;50(January(1)):325–330. doi: 10.1016/j.bone.2011.11.002. [DOI] [PubMed] [Google Scholar]
- 18.Gangji V., Hauzeur J.P., Schoutens A., Hinsenkamp M., Appelboom T., Egrise D. Abnormalities in the replicative capacity of osteoblastic cells in the proximal femur of patients with osteonecrosis of the femoral head. J Rheumatol. 2003;30(2):348–351. [PubMed] [Google Scholar]
- 19.Tubach F., Ravaud P., Martin-Mola E. Minimum clinically important improvement and patient acceptable symptom state in pain and function in rheumatoid arthritis, ankylosing spondylitis, chronic back pain, hand osteoarthritis, and hip and knee osteoarthritis: results from a prospective multinational study. Arthritis Care Res (Hoboken) 2012;64(November(11)):1699–1707. doi: 10.1002/acr.21747. PubMed PMID: 22674853. [DOI] [PubMed] [Google Scholar]
Further Reading
A) https://zimmerbiomet.tv/videos/1257. Kamath AF. A video of the PerFuse Percutaneous Decompression System. Last Accessed 4/21/2018.