Abstract
A medial open wedge high tibial osteotomy (MOWHTO) is an effective surgical procedure to correct varus deformity related to Knee Osteoarthritis. It consistently provides relief in knee pain and improves knee function. This technique is recommended for active, middle and old aged individuals with an isolated medial compartment knee OA. The MOWHTO scores several advantages over lateral closed wedge osteotomy and hence is now a preferred choice of HTO.
Keywords: Osteoarthritis, Knee joint, High tibial osteotomy, Genu varum, Deformity
1. Introduction
Osteoarthritis (OA) is one of the most common disorders of the knee joint in a human being and present a significant health problem that impairs quality of life in the middle or old age patient. The knee OA commonly leads to a genu varus deformity,1 which leads to medial compartment overload and progression of the disease in the knee. 2,3 A medial opening wedge high tibial osteotomy (MOWHTO) is a well-established surgical procedure for an isolated medial compartment OA, to realign the knee and to halt the progress of the disease process in younger patients. Medial open-wedge high tibial osteotomy (MOWHTO) is a well-established and a successful procedure to relieve pain and to improve knee function in medial compartment OA. The MOWHTO is expected to delay the need for possible future Total Knee Arthroplasty (TKA) and may be an optimal treatment approach for younger patients. Few alternative treatments for Knee OA include a lateral close wedge high tibial osteotomy (LCWHTO) and unicompartmental knee arthroplasty (UKA).4,5 In the critical appraisal of the current evidence available in the literature, we shall define the indications, contraindications, pros, and cons of MOWHTO and also compare this technique with the other contemporary procedures for Unicompartmental Knee OA.
2. Review
The optimal treatment of a symptomatic medial compartment knee OA in younger individuals is often debatable and challenging. There is a paradigm shift in favor of natural joint preservation in these cases and to postpone or alleviate the need for TKA, as much as possible. An angular deformity of the knee (like genu varum), in symptomatic and resistant cases, conservatively treated cases often requires surgical correction since HTO reduces pain and improves knee function with unicompartmental OA patients.6
The correction of varus knee deformity in OA patients is achievable with a HTO or a UKA. HTO and UKA share almost the same indications for medial unicompartmental knee arthritis but have several pros and cons (Table 1). The two most commonly done techniques of HTO include a medial open-wedge and a lateral closed-wedge HTO. (Fig. 1, Fig. 2) A MOWHTO offers several additional advantages over a lateral close-wedge HTO and UKA (Table 2). It is an easier surgical technique and carries much less risk of neurovascular injury.7,8 An additional advantage of MOWHTO is the possibility to perform biplanar corrections, which is vital to restoring knee stability. The MOWHTO has now become an established and popular operative procedure for the correction of varus deformity of the knee. The two types of the MOWHTO have been described, an ascending and a descending osteotomy. In ascending osteotomy, the tibial cut is the parallel upwardly pointing placement of two K-wires under fluoroscopic control of the tibial plateau,9 whereas, in descending osteotomy, the tibial cut slopes down. The aim of leg alignment correction is to put the mechanical axis at least through the lateral downslope of the tibial eminence or slightly more lateral, resulting in a minimal overcorrection.10,11 It can be done using a different types of implants. It has been reported in few studies that the patella height decreases significantly in ascending type of osteotomy compared to descending type. However, there was no significant difference in mechanical axis or posterior tibial slope between ascending and descending HTO groups.12 The authors, therefore, recommended bi-planar descending MOWHTO to avoid patellofemoral and slope-related knee kinematics problems. The indications of HTO are now slowly expanding from the medial compartment OA to chronic instabilities (such as PLC instability),13 ligament reconstruction failure due to malalignment, to protect a concurrent ligament reconstruction and malunited tibial condyle fracture.14 The factors influencing the outcomes of HTO are now better understood. The commonly identifiable factors include medial compartmental OA, restricted range of motion,15 ligamentous knee instability,16 patellofemoral arthrosis,17 obesity and improper or loss of correction of deformities after HTO.18 There are some pearls and pitfall of HTO which are tabulated in the table (Table 3).
Table 1.
Table showing the comparison between Medial open wedge high tibial osteotomy (MOWHTO), Lateral close wedge high tibial osteotomy (LCWHTO), Unicondylar knee arthroplasty (UKA).
| MOWHTO | LCWHTO | UKA | |
|---|---|---|---|
| Age(in years) | <65 | <65 | >55 |
| Activity level | Active | Active | Low demand |
| Weight(BMI) | Any | Any | <30 |
| Alignment | 5–150 | 8-150 | 0–50 |
| AP Instability | Any | Any | N 0 to grade I |
| ML Instability | N 0 to grade II | N 0 to grade II | N 0 to grade I |
| ROM | Arc 120*and <5* flexion contracture | Arc 120*and <5* flexion contracture | Arc 90*and <5* flexion contracture |
| Grade of OA | Ahlback II–II | Ahlback II–III | Ahlback III–IV |
BMI = body mass index; AP Instability = antero-posterior instability; ML Instability = medio-lateral instability; instability grading according to the American Medical Association (grade I = 0–5 mm, grade II = 5–10 mm, grade III = > 10 mm, no hard stop); Arthrosis severity = medial compartment arthrosis according to Ahlback classification, assuming that lateral and patellofemoral compartments are intact.
Fig. 1.
X-Ray Anteroposterior (AP) view of left knee showing lateral closing wedge High tibial osteotomy (HTO) with Staples.
Fig. 2.
X-Ray AP view of left knee showing medial open wedge HTO with tricalcium phosphate wedge.
Table 2.
Table showing the Pros and Cons of MOWHTO, LCWHTO, UKA.
| Pros | Cons | |
|---|---|---|
| MOWHTO | *Restores the height of the medial column | *May require conversion to TKA after 10 years or so |
| *Does not significantly alter the tibial slope | *Immobilization for few weeks required post-operatively | |
| *Does not alter the height of patella | ||
| * Easy to convert to TKA | ||
| *No fibular osteotomy required | ||
| *No restriction of activities needed | ||
| LCWHTO | *A long track record of this procedure is known | *Reduces the height of lateral column |
| *Cheaper with minimal inexpensive implants required | *Can affect tibial slope | |
| *May cause patella baja | ||
| * Difficult to convert to TKA | ||
| *Fibular osteotomy is necessary | ||
| *Lateral popliteal nerve injury is possible | ||
| *May require conversion to TKA after 10 years or so | ||
| *Immobilization for few weeks required post-operatively | ||
| UKA | *Immediate weight bearing and knee mobilization is allowed | *Limited life span |
| *Conversion to TKA may be challenging | ||
| *More expensive |
Table 3.
Table showing the pearls and pitfalls of HTO.
| Pearls | Pitfalls |
|---|---|
| The use of a radiolucent retractor to protect the posterior neurovascular structures that allows the surgeon to fluoroscopically access the osteotomy without having to remove the retractor to verify pin or osteotome position. | Opening proximal tibial osteotomy has been reported to increase the posterior tibial slope. Measuring the sagittal slope preoperatively helps planning the best position for the plate |
| Slow progression in the opening of the osteotomy using a specific spreader device and leaving it in place for 5 min that allow for stress relaxation of the lateral cortex it minimize the risk of an undesired fracture | Intra-articular tibial fracture is a possible complication. Keeping at least 1.5 cm of bone between the osteotomy and the cartilage on the coronal view minimizes this risk |
| The fixation plate may need to be bent to better conform to the tibia surface | Extra-articular fracture extending to the lateral tibial cortex may happen. Leave 1 cm of bone bridge on the lateral side to avoid this complication. |
| Beware of the bowl shape of the medial tibial plateau when placing the proximal screws to avoid damage to the joint. | If the lateral tibial cortex is damaged, a staple can be placed to prevent further propagation and stabilize the cortex |
| Placing a large Richards staple anteriorly while hyperextending the knee prevents the sagittal plane correction from altering postoperatively | Consolidation problems may happen with opening wedge osteotomies. Preserving local biology and filling the gap with bone graft when it is greater than 10 mm minimizes the risk of this complication. |
| Place an immobilizer brace after surgery to prevent loss of correction but begin early assisted knee mobilization to prevent adhesions. | Advise your patient to avoid smoking and the use of nicotine products to prevent consolidation problems. |
Both open-wedge and closed-wedge HTO lead to good and comparable results. However, the technique of MOWHTO provides a better outcome regarding functional scores in early as well as late follow-up with decreased duration required for the full-weight bearing.19 In the recent years, the classic lateral closed wedge osteotomy (LCWHTO) has given way to the MOWHTO. The advantage and limitation of MOWHTO are given in the table below (Table 4). An MOWHTO which is said to be more accurate has the advantage (Table 5) of using a medial approach and eliminates the need for a fibular osteotomy with the risk of peroneal nerve damage and fibular pseudarthrosis in the case of LCWHTO.20 There are various ways to fix the HTO with or without implant. The bone staples are simple and inexpensive to use and provide some stability to the osteotomy.21 (Fig. 3) However, the fixation given by the staples is not robust and sufficient enough to allow immediate movements of the knee and weight bearing on the operated leg. The OTIS-C plate help to stabilize HTO from the medial side (Fig. 4). Its specific locking system provides immediate compression of the graft as well as stable tibial fixation, thus allowing early weight bearing. The internal fixator TomoFix®, (Fig. 5) a long rigid plate was developed by the AO Knee Expert Group and Puddu plate (Fig. 6) (Arthrex, Naples, Florida). They can (Fig. 7) achieve optimal stability and hold the attained correction, without the need for additional bone substitutes to fill the gap produced by the osteotomy. The TomoFix plate is reported to provide superior stability in both compression and torsion compared to the Puddu Plate and is an effective option in elderly as well as in young patients. External fixators are also used by some surgeons to fix the osteotomy site. The advantage of using external fixators (Ilizarov technique, Taylor spatial frame or mono/Biplanar fixators) mainly include the modularity of the construct. The disadvantages include the local irritation because of cumbersome construct and pin tract infection. It is noted that age did not influence the clinical outcome and radiological outcomes after MOWHTO, using these plates. When treating in cases of persistent ligamentous instability, HTO can be performed in isolation, or with simultaneous ligament reconstruction or as a staged procedure with HTO first followed by ligament reconstruction. Studies with combined ACL reconstruction and HTO report higher postoperative activity levels when compared with HTO alone.22 Physically active elderly patients who are likely to show good compliance in a rehabilitation program can be recommended for MOWHTO. In active young patients with genu varus malalignment, MOWHTO is primarily indicated. These younger individuals may be considered for a staged procedure with the HTO before ligament reconstruction.
Table 4.
Table showing the advantages and limitations of HTO.
| Advantages | Limitations |
|---|---|
| It prevents stretching and failure of the grafts in cases of concomitant chronic PLC or ACL instabilities and varus malalignment | Chance of tibial fracture |
| Possibility to perform a biplanar correction, which can be adjusted according to the instability | Need for an 8-week period of non-weight bearing |
| In some patients, the correction of varus malalignment reduces the instability complaint | There is risk of consolidation problems is higher in opening osteotomies, when compared with lateral closing osteotomies. |
| Opening wedge osteotomies allow for better control of the correction | Big corrections may be better addressed with a distraction opening technique or double osteotomy |
| For treatment of early degenerative disease of the medial compartment, proximal tibial osteotomy can delay the need for a joint replacement procedure. | Significant changes in bony anatomy can challenge future conversion to a knee replacement |
Table 5.
Table showing the Pros and Cons of different method of fixation of MOWHTO.
| Methods of fixation for MOWHTO | Pros | Cons | |
|---|---|---|---|
| 1 | Iliac crest graft | Autologous graft | Two operative sites |
| Free of cost | Difficult to fashion the bone graft tofit the shape and size of the osteotomy | ||
| Fast bony union | Donor site associated morbidity (Infection, Persistent pain, paraesthesia, fracture) | ||
| No secondary surgery for removal | |||
| 2 | Synthetic bone graft alone | Easily available | Expensive |
| No surgery to other part of the body | Delayed incorporation in bone | ||
| Various size of grafts available to fit into the osteotomy site, as desired | Soft tissue irritation and infection possible | ||
| Small incision | Slippage of the graft is possible | ||
| Large deformity cannot be corrected | |||
| 3 | Synthetics bone graft with internal fixation | ||
| Staple | Easy availability | May loosen, postoperatively | |
| Less surgical time | Dislocation of staples | ||
| Economical | May cause transient palsy of the peroneal nerve | ||
| Puddu Plate | Better stability | Non union | |
| Can be used with or without bone/synthetic graft | Local irriatation | ||
| Hardware prominence causing anterior leg pain | |||
| May need another lateral fixation | |||
| Requires implant removal for future TKR | |||
| Tomofix plate | Adequate strength | Non-union of osteotomy is possible | |
| Good for obese pt | Local irritation | ||
| Large deformity correction can be achieved | Screw may penetrating into the knee joint | ||
| Unstable correction following lateral tibial cortex fracture | |||
| Long time form bone union | |||
| Larger incision | |||
| 4 | External Fixation | ||
| Ilizarov fixator | Modularity | Local irritation | |
| Pin tract infection | |||
| Taylor spatial frame | Modularity | Pin tract infection | |
| More accurate correction | Costly | ||
| Uniplanar/Biplanar External fixators | TKA if required doesn’t requires implant removal | Pin tract infection | |
Fig. 3.
X-Ray AP and lateral view of left knee showing medial open wedge HTO with Staples and graft.
Fig. 4.
X-Ray AP and lateral view of right knee showing medial open wedge HTO with OTIS-C plate with bone graft.
Fig. 5.
X-Ray AP and lateral view of left knee showing medial open wedge HTO with Tomofix plate and bone graft.
Fig. 6.
X-Ray AP view of left knee showing medial open wedge HTO with bone graft and Pudu plate.
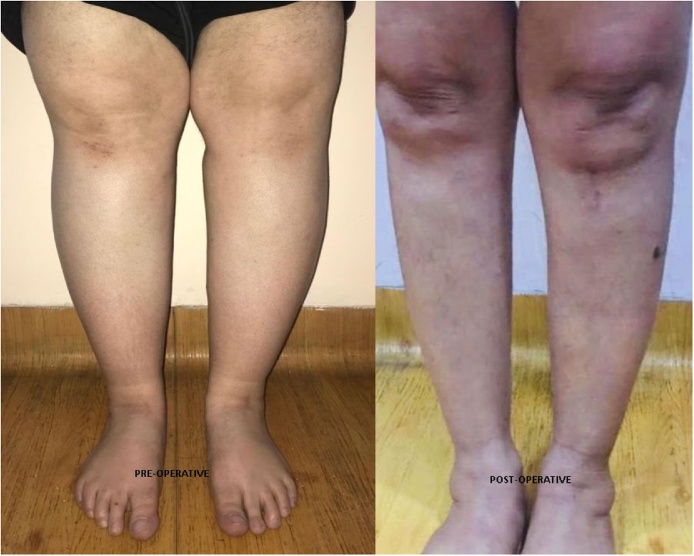
Fig. 7.
Clinical picture showing preop and postop after MOWHTO of a female patient with unicompartmental medial Knee OA.
2.1. Removal of the metal is optional
Several options are available to fill the gap created by the osteotomy, like an autograft, allograft or synthetic bone substitutes (hydroxyapatite, β-tricalcium phosphate, a combination of both and bone cement). These can be used with or without platelet-rich plasma (PRP), growth factors, and bone marrow aspirate concentrate (BMAC). Till date, autologous bone graft is considered as the gold standard for filling material because of its osteoconductive, osteoinductive, and osteogenic properties.23,24 Bone substitutes help to avoid donor site morbidity associated with bone autograft; however, bone substitute provides weaker resistance to compressive loading forces. It has been reported that smaller gaps (of less than 10 mm) can be left unfilled, with the concomitant use of a plate, because no pseudarthrosis or loss of correction was observed in these cases.25
Contraindications for MOWHTO include lateral compartment OA, severe limitation of range of knee motion (flexion less than 90° and a flexion contracture greater than 10°), severe patellofemoral symptoms, inflammatory arthritis, open growth plates or patients with patella Baja.26 Chronic smokers and chronic nicotine-derived product users should be discouraged from undergoing this procedure because of the high risk of nonunion.27 The coronal alignment of the proximal tibia will be corrected. However, this correction may also unintentionally alter the posterior tibial slope (PTS). Many studies report that the PTS increases after medial open-wedge HTO and others report that knee kinematics and stability in the sagittal plane may have influenced these unintended increases in PTS after medial open-wedge HTO.28, 29, 30
3. Conclusion
In conclusion, MOWHTO improves pain and knee function significantly in symptomatic medial compartment OA. Physically active middle-aged and elderly patients who are likely to show good compliance in a rehabilitation program can be recommended for MOWHTO. The MOWHTO using the long rigid plate is an effective procedure for all elderly patients and larger deformities but carries the drawback of the longer incision and heavy hardware. So there is no age barrier for doing MOWHTO. We can perform the MOWHTO using a different type of implants, and it will decrease the pain and improve the function of the affected knee. This method helps to postpone the early chance of TKA.
Contributor Information
Raju Vaishya, Email: raju_vaishya@apollohospitalsdelhi.com.
Anuj Raj Bijukchhe, Email: admin@phectnepal.org.
Amit Kumar Agarwal, Email: amitkumar_a@apollohospitalsdelhi.com.
Vipul Vijay, Email: drvipul_v@apollohospitalsdelhi.com.
References
- 1.Wolfe S.A., Brueckmann F.R. Conservative treatment of genu valgus and varum with medial/lateral heel wedges. Indiana Med. 1991;84:614–615. [PubMed] [Google Scholar]
- 2.Brouwer R.W., Huizinga M.R., Duivenvoorden T. Osteotomy for treating knee osteoarthritis. Cochrane Database Syst Rev. 2014;12 doi: 10.1002/14651858.CD004019.pub4. [CD004019] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Asik M., Sen C., Kilic B. High tibial osteotomy with Puddu plate for the treatment of varus gonarthrosis. Knee Surg Sports Traumatol Arthrosc. 2006;14:948–954. doi: 10.1007/s00167-006-0074-1. [DOI] [PubMed] [Google Scholar]
- 4.Bode G., von Heyden J., Pestka J. Prospective 5-year survival rate data following open-wedge valgus high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc. 2015;23:1949–1955. doi: 10.1007/s00167-013-2762-y. [DOI] [PubMed] [Google Scholar]
- 5.Arthur A., LaPrade R.F., Agel J. Proximal tibial opening wedge osteotomy as the initial treatment for chronic posterolateral corner deficiency in the varus knee: a prospective clinical study. Am J Sports Med. 2007;35:1844–1850. doi: 10.1177/0363546507304717. [DOI] [PubMed] [Google Scholar]
- 6.Brouwer R.W., Bierma-Zeinstra S.M.A., van Koeveringe A.J. Patellar height and the inclination of the tibial plateau after high tibial osteotomy. The open versus the closed-wedge technique. J Bone Joint Surg Br. 2005;87:1227–1232. doi: 10.1302/0301-620X.87B9.15972. [DOI] [PubMed] [Google Scholar]
- 7.McNamara I., Birmingham T.B., Fowler P.J. High tibial osteotomy: evolution of research and clinical applications—a Canadian experience. Knee Surg Sports Traumatol Arthrosc. 2013;21 doi: 10.1007/s00167-012-2218-9. [23–23. [DOI] [PubMed] [Google Scholar]
- 8.Bonin N., Ait Si Selmi T. Anterior cruciate reconstruction combined with valgus upper tibial osteotomy: 12 years follow-up. Knee. 2004;11:431–437. doi: 10.1016/j.knee.2004.02.001. [DOI] [PubMed] [Google Scholar]
- 9.Lobenhoffer P., Agneskirchner J.D. Improvements in surgical technique of valgus high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc. 2003;11:132–138. doi: 10.1007/s00167-002-0334-7. [DOI] [PubMed] [Google Scholar]
- 10.Cantin O., Magnussen R.A., Corbi F. The role of high tibial osteotomy in the treatment of knee laxity: a comprehensive review. Knee Surg Sports Traumatol Arthrosc. 2015;23:3026–3037. doi: 10.1007/s00167-015-3752-z. [DOI] [PubMed] [Google Scholar]
- 11.LaPrade R.F., Oro F.B., Ziegler C.G. Patellar height and tibial slope after opening-wedge proximal tibial osteotomy: a prospective study. Am J Sports Med. 2010;38:160–170. doi: 10.1177/0363546509342701. [DOI] [PubMed] [Google Scholar]
- 12.Krause M., Drenck T.C.L., Korthaus A. Patella height is not altered by descending medial open wedge high tibial osteotomy (HTO) compared to ascending HTO. Knee Surg Sports Traumatol Arthrosc. 2017 doi: 10.1007/s00167-017-4548-0. [DOI] [PubMed] [Google Scholar]
- 13.Gaasbeek R.D., Sonneveld H., van Heerwaarden R.J. Distal tuberosity osteotomy in open wedge high tibial osteotomy can prevent patella infera: a new technique. Knee. 2004;11 doi: 10.1016/j.knee.2004.02.002. [457–46. [DOI] [PubMed] [Google Scholar]
- 14.Sundararajan H.S., Nagaraja M.S., Rajasekaran S. Medial open wedge high tibial osteotomy for varus malunited tibial plateau fractures. Arthros. J. Arthrosc. Relat. Surg. 2017;33(3):586–594. doi: 10.1016/j.arthro.2016.08.027. [DOI] [PubMed] [Google Scholar]
- 15.Murray D.W., Fitzpatrick R., Rogers K. The use of the Oxford hip and knee scores. J Bone Joint Surg Br. 2007;89:1010–1014. doi: 10.1302/0301-620X.89B8.19424. [DOI] [PubMed] [Google Scholar]
- 16.Brinkman J.M., Lobenhoffer P., Agneskirchner J.D. Osteotomies around the knee: patient selection, the stability of fixation and bone healing in high tibial osteotomies. J Bone Joint Surg Br. 2008;90:1548–1557. doi: 10.1302/0301-620X.90B12.21198. [DOI] [PubMed] [Google Scholar]
- 17.Naudie D., Bourne R.B., Rorabeck C.H. The Install Award. Survivorship of the high tibial valgus osteotomy. A 10-to −22-year follow-up study. Clin Orthop Relat Res. 1999;367:18–27. [PubMed] [Google Scholar]
- 18.Odenbring S., Tjornstrand B., Egund N. Function after tibial osteotomy for medial gonarthrosis below aged 50 years. Acta Orthop Scand. 1989;60:527–531. doi: 10.3109/17453678909150116. [DOI] [PubMed] [Google Scholar]
- 19.Comparison of closing-wedge and opening-wedge high tibial osteotomies for medial compartment osteoarthritis of the knee in the Asian populationn. J Clin Orthop Trauma. 2016;7(4):272–275. doi: 10.1016/j.jcot.2016.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Stoffel K., Stachowiak G. Kuster Open wedge high tibial osteotomy: biomechanical investigation of the modified Arthrex Osteotomy Plate (Puddu Plate) and the TomoFix Plate. Clin Biomech. 2004;19(9):944–950. doi: 10.1016/j.clinbiomech.2004.06.007. [DOI] [PubMed] [Google Scholar]
- 21.Vaishya R., Vijay V., Kumar J.G., Agarwal A.K. A prospective study of the anterior cruciate ligament reconstruction associated with high tibial opening wedge osteotomy in knee arthritis associated with instability. J Clinic Orth Trauma. 2016;7(4):265–271. doi: 10.1016/j.jcot.2016.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kenichi G., Takeshi S., Daigo S. Age does not affect the clinical and radiological outcomes after open-wedge high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc. 2017;25:918–923. doi: 10.1007/s00167-015-3847-6. [DOI] [PubMed] [Google Scholar]
- 23.Amendola A., Fowler P.J., Litchfield R. Opening wedge high tibial osteotomy using a novel technique: early results and complications. J Knee Surg. 2004;17(3):164–169. doi: 10.1055/s-0030-1248216. [DOI] [PubMed] [Google Scholar]
- 24.Staubli A.E., De S.C., Babst R. TomoFix: a new LCP-concept for open wedge osteotomy of the medial proximal tibia—early results in 92 cases. Injury. 2003;34:B55–B62. doi: 10.1016/j.injury.2003.09.025. [DOI] [PubMed] [Google Scholar]
- 25.Kesmezacar H., Erginer R., Ogut T. Evaluation of patellar height and measurement methods after valgus high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc. 2005;13(7):539–544. doi: 10.1007/s00167-004-0572-y. [DOI] [PubMed] [Google Scholar]
- 26.Marriott K., Birmingham T.B., Kean C.O. Five-year changes in gait biomechanics after concomitant high tibial osteotomy and ACL reconstruction in patients with medial knee osteoarthritis. Am J Sports Med. 2015;43:2277–2285. doi: 10.1177/0363546515591995. [DOI] [PubMed] [Google Scholar]
- 27.Bonnin M.P., Laurent J.R., Zadegan F. Can patients really participate in sport after high tibial osteotomy? Knee Surg Sports Traumatol Arthrosc. 2013;21:64–73. doi: 10.1007/s00167-011-1461-9. [DOI] [PubMed] [Google Scholar]
- 28.Zuegel N.P., Braun W.G., Kundel K.P. Stabilization of high tibial osteotomy with staples. Arch Orthop Trauma Surg. 1996;115(5):290–294. doi: 10.1007/BF00439056. [DOI] [PubMed] [Google Scholar]
- 29.Spahn G., Wittig R. Primary stability of various implants in tibial opening wedge osteotomy: a biomechanical study. J Orthop Sci. 2002;7(6):683–687. doi: 10.1007/s007760200121. [DOI] [PubMed] [Google Scholar]
- 30.Lee Y.S., Kang J.Y., Lee M.C. Osteotomy configuration of the proximal wedge and analysis of the affecting factors in the medial open-wedge high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc. 2017;25:793–799. doi: 10.1007/s00167-015-3819-x. [DOI] [PubMed] [Google Scholar]