Abstract
Background
Pelvic fractures represent one of the most challenging clinical problems in which an urgent multidisciplinary approach is required. The early management in a suspected pelvic fracture starts with the good radiological evaluation. The standard radiographic view includes the anteroposterior, inlet and outlet views. The inlet and outlet views are taken with 45° tilt from anteroposterior plane. However, recent studies have shown that there is significant individual variation within the population and these values should be redefined.
Material and Methods
This is a retrospective study carried out in a tertiary care teaching institute. Total 110 patients (including 42 female and 68 male patients) of age older than 18 years, who had a routine pelvic Computed Tomography (CT) scan performed for any indications unrelated to pelvic pathologies were included.
Statistical analysis
Mean and standard deviation were calculated. For each angle measured, the effect of age was determined and a comparison was made between male and female patients, p value <0.05 is considered significant.
Results
The mean angle of caudal tilt for the ideal screening inlet view was 33° +/−8 (16.3–31.3) and the mean angle of cephalic tilt for the ideal screening outlet view was 56° +/−9 (51.6–81.8).
Conclusion
This study re-evaluated the optimal inlet and outlet angles in Indians and demonstrated that the mean angles needed to create an ideal pelvic inlet and outlet views are 33° and 56° respectively.
Keywords: Pelvic fracture, Inlet angle, Outlet angle, Non orthogonal
1. Introduction
Patients with pelvis fracture require anteroposterior, inlet and outlet radiographic views of the pelvis to classify the injury and to assess the stability.1,2 The pelvic inlet view demonstrates abduction/adduction and anterior/posterior displacement of the injured hemipelvis. This is obtained with the patient supine and the x-ray beam directed 45° caudal from the anteroposterior view.3,4,5 The pelvic outlet view demonstrates vertical displacement and flexion/extension deformity of the injured hemipelvis and is obtained by directing the x-ray beam 45° cranial.3,4,5 Despite wide use of computed tomography (CT) scans, inlet and outlet views are still an essential part of the initial evaluation of pelvic injuries. It also provide important information about planning the surgery.
Different angles were reported in the literature to obtain accurate pelvis inlet and outlet views.3,4 The classical teaching was 45° caudal and cranial tilt for inlet and outlet views respectively. However, recent studies have shown that there is significant individual variation within the population and these values should be redefined.6,7 These individual anatomical variations frequently result in inadequate x-rays.
In the present study, we hypothesize that inlet and outlet radiographic views is not 45° for Indians. The purpose of this study is to obtain accurate inlet and outlet views in Indian population.
2. Material and methods
This retrospective study was carried out in a tertiary care teaching institute where 110 consecutive patients (including 42 female patients and 68 male patients) of age older than 18 years, who had a routine pelvic CT performed for any indications unrelated to pelvic pathologies were included. The study was approved by Institutional ethics committee.
The optimal inlet and outlet angles required to profile the clinically relevant pelvic anatomy were quantified for each patient with use of CT reconstruction using the standard methods as described by Ricci et al.7 RadiAnt DICOM Viewer 4.0.3 version (64-bit) was used for determining inlet and outlet angles. The landmarks and calculation methodology is as follows:
The inlet angle (Method 1) is the angle formed between the line tangent to the anterior margin of body of first sacrum vertebra (S1) and a line in the anteroposterior plane (AP) (Fig. 1). Method 2 is the angle between the anterior margin of second sacrum vertebra (S2) and the AP line (Fig. 2). The inlet angle required to profile the pubic rami (Method 3) was the angle formed between the line bisecting the pubic ramus and AP line (Fig. 3). Because of the presence of the midline symphyseal cartilage, which is a soft tissue structure, sagittal CT reconstruction slices taken 1 cm lateral to the midline to define the pubic rami.
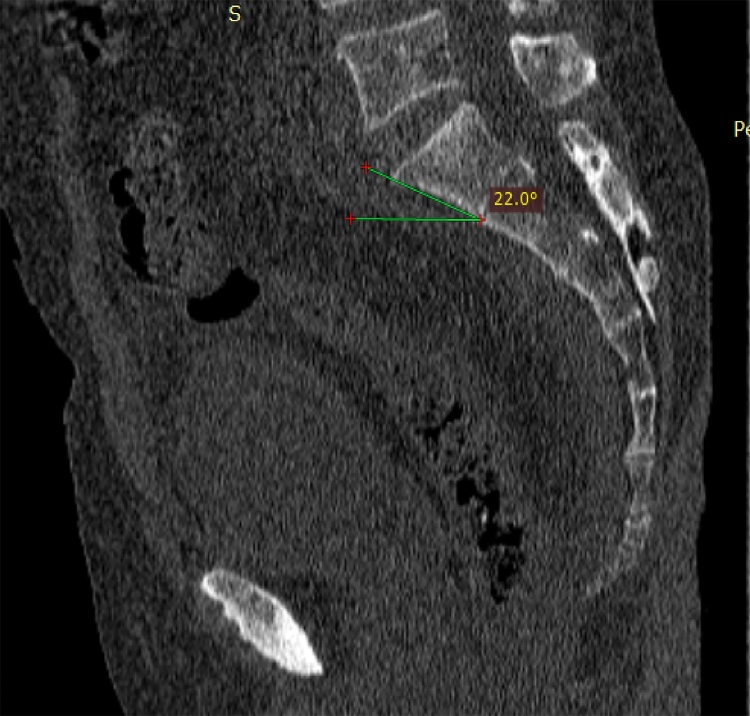
Fig. 1.
Sagittal CT scan of pelvis showing inlet angle calculated by method 1. One line drawn along anterior margin of S1 and another line drawn perpendicular to the table.
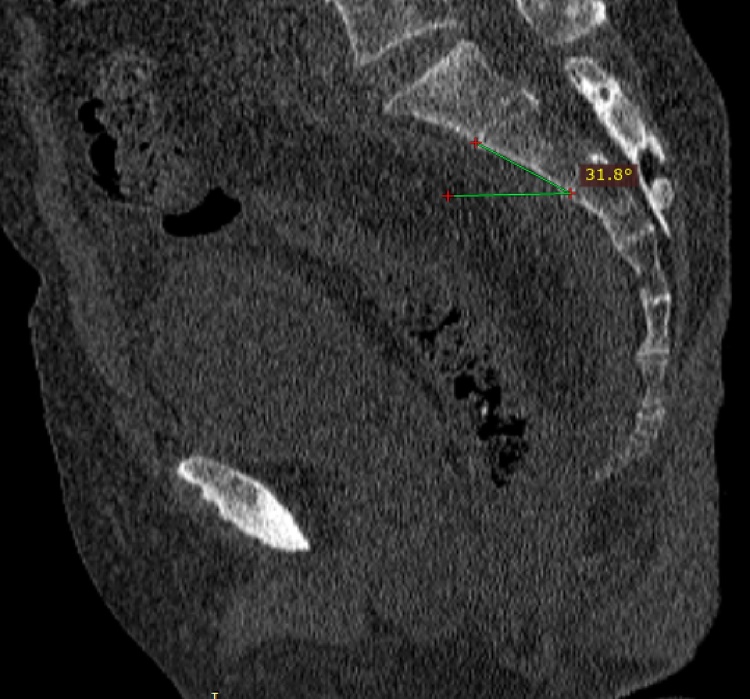
Fig. 2.
Sagittal CT scan of pelvis showing inlet angle calculated by method 2. One line drawn along anterior margin of S2 and another line perpendicular to the table.
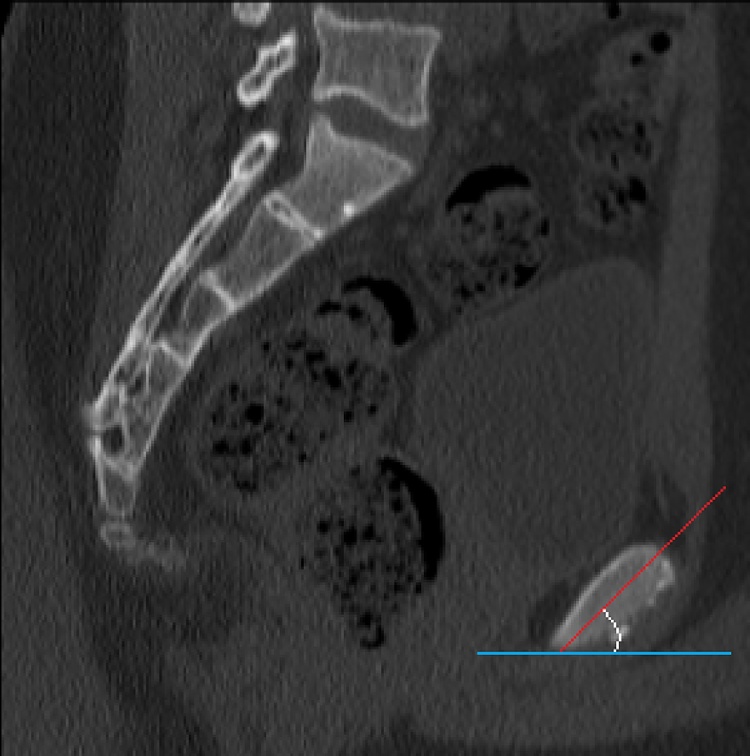
Fig. 3.
Sagittal CT scan of pelvis showing inlet angle calculated by method 3. One line bisecting the bone adjacent to symphysis pubis and another line perpendicular to the table.
Outlet angle - The ideal outlet view is defined as a view where the pubic symphysis is superimposed over the upper sacrum and the pubic tubercles are just inferior to the S1 foramina. Because of the trapezoidal shape of S1 and S2 bodies, perpendicular lines from both the anterior and posterior cortical surfaces were drawn and mean value is considered for calculation (Fig. 4, Fig. 5). The angle between each of these lines and AP line was measured and represents the outlet angle required to optimally examine these structures.
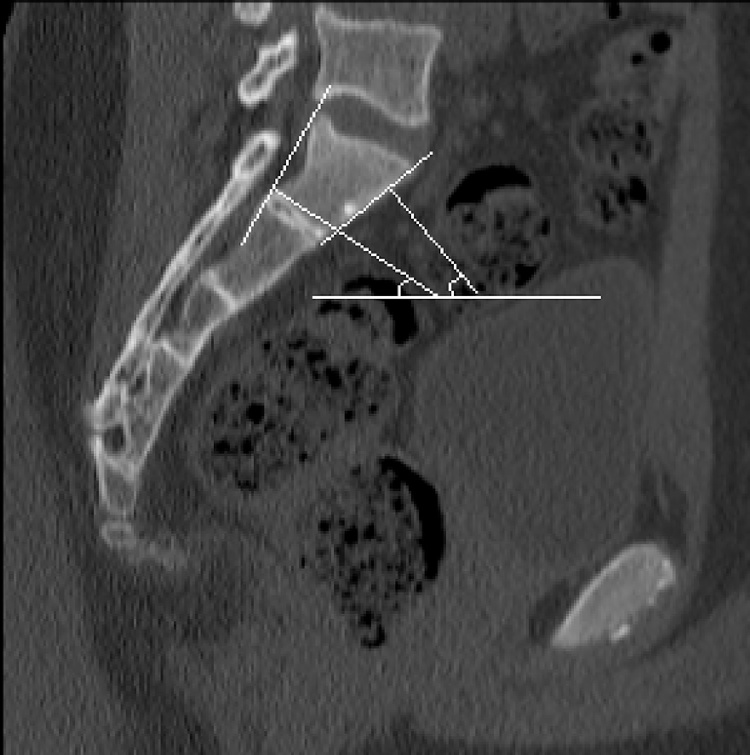
Fig. 4.
Sagittal CT scan of pelvis showing outlet angle (Method 1). One angle between a line perpendicular to anterior margin of S1 and AP line and another angle between a line perpendicular to posterior margin of S1 and AP line. The mean of both these angles is considered.
Fig. 5.
Sagittal CT scan of pelvis showing outlet angle (Method 2). One angle between a line perpendicular to anterior margin of S2 and AP line and another angle between a line perpendicular to posterior margin of S2 and AP line. The mean of both these angles is considered.
For each angle measured, the effect of age was determined and a comparison was made between male and female patients, p value <0.05 is considered significant.
3. Results
The data was collected from the calculations done on the CT films of 110 patients included in the study. This included 42 females and 68 male patients with no significant pelvic deformity.
The results of the study are shown in Table 1.
Table 1.
Comparison of X-ray and CT as imaging modalities in emergency setup.
| Pelvic inlet and outlet X-rays | CT based evaluation |
|---|---|
| Easily available | Difficult to obtain in resource stricken setup |
| Faster procedure | Longer procedure |
| Can be conducted with limited expertise | Requires expertise |
| Minimal radiation | More radiation |
| Provides required information in emergency department | Detail information can be obtained |
Inlet angle: The Mean ± SD for inlet angle by Method 1 was 25.64 ± 10.9413, by Method 2 was 33.095 ± 6.7550 and by Method 3 was 40.983 ± 7.3405. The mean angle of caudal tilt for the ideal screening inlet view using CT reconstruction was 33° +/−8 (16.3–31.3).
Outlet angle: The mean angle of cephalic tilt for the ideal screening outlet view was 56° +/−9 (51.6–81.8)
Significant statistical difference was observed between inlet and outlet angles.
There was no significant difference observed between males and females with respect to inlet and outlet angles.
4. Discussion
The evaluation and management of pelvic fractures is based on anteroposterior, inlet, and outlet radiographic views. Different angles were reported in the literature for inlet and outlet views.3,4 However, the classical teaching was 45° for both the inlet and outlet views until recently, when Ricci et al.7 recommended using 25° for the inlet and 60° for the outlet on the basis of CT scan of normal subjects.
In emergency setup, especially in developing nations, the value of obtaining optimal pelvic inlet and outlet views becomes extremely important. The limited availability of CT scans in a resource constrained place makes the properly obtained inlet and outlet views of paramount importance (Table 1).
Pelvic tilt is defined as the angle between a line drawn from the centre of the S1 endplate to the centre of the femoral heads and a line perpendicular to the S1 endplate. Its value ranges from 30 to 80° and is related to lumbar lordosis that in turn affects sacral slope.8 Therefore, the pelvic tilt is specific to patient and inlet and outlet angle should be defined for each patient to get optimal views.
The orientation of the inlet view is perpendicular to the pelvic brim such that the sacral promontory overlaps the anterior cortical margin of S1.9 The angle to obtain such view ranges 40–60° and is most typically used as 45°.10 The orientation for an outlet radiograph is one when symphysis pubis overlaps the upper sacral body. The corresponding recommended angle has ranged between 30–45° and is also most commonly used as 45°, providing an orthogonal view to inlet view.10 These recommendations are empirical or based on Level-V evidence.11
The optimum angle calculated from the study is 33° for the inlet angle and 56° for the outlet angle, which proves that inlet and outlet views are non-orthogonal in Indians. This information is significant in iliosacral screw placement for sacroiliac joint fixation. If a screw appears inside the bone in two orthogonal views, it is safe. However, if the views are not orthogonal, there may be a large area, which is not visualized unless the image intensifier is further tilted until the second view is orthogonal to the first one.12
In a study done by Ricci et al.7 in 2010, the inlet angle was 25° and outlet angle was 60°, which suggests greater variation in the inlet angle whereas similar result for outlet view as compared to present study. Also, the data of Ricci et al was re-evaluated by Pekmezci et al.12 using 3D reconstruction suggesting the ideal inlet angle to be 25° and ideal outlet angle to be 45°. Though these data from the study may have variations from the current study but it does reinforce the fact that there is significant deviation of the inlet and outlet angle from the traditional practice. Gender has been described as another potential source of variability among individuals. Our data, however, revealed no difference between males and females for any of the measurements made. In fact, the average values for males and females were nearly identical.
In spite of all the relevant information generated from the study, there are few evident limitations associated with this study. Firstly, the limited sample size of the study to determine variability based on race. Secondly, since the study involves the calculations in non-injured pelvis films, the variations in the anatomy secondary to the fractures cannot be taken into account. However, our goal was to define the normal values in patients without pelvic ring injury. A follow-up study to test these values in a prospective series of trauma patients should be performed to verify these results.
5. Conclusion
This study re-evaluated the optimal inlet and outlet angles in Indians and demonstrated that the average angles needed to create an ideal pelvic inlet and outlet views are 33° caudal tilt and 56° cephalad tilt respectively.
Conflict of interest
There is no conflict of interest in the submitted research work.
Contributor Information
Yugal Karkhur, Email: dryugal9890@gmail.com.
Anurag Tiwari, Email: dranurag.tiwari@gmail.com.
Lalit Maini, Email: lalit_maini@rediffmail.com.
Vivek Bansal, Email: bansalvivek1985@gmail.com.
Abhimanyu Kakralia, Email: kakralia86@gmail.com.
References
- 1.Chapman M.W., editor. Chapman’s orthopaedic surgery. 3rd ed. Lippincott Williams and Wilkins; Philadelphia: 2001. [Google Scholar]
- 2.Bucholz R.W., Heckman J.D., Court-Brown C.M., editors. Rockwood and Green’s fractures in adults. 6th ed. Lippincott Williams and Wilkins; Philadelphia: 2006. [Google Scholar]
- 3.Browner B.D., Jupiter J.B., Levine A.M. Skeletal trauma: fractures, dislocations, ligamentous injuries. In: Stover M.D., Mayo K.A., Kellam J.F., editors. Pelvic ring disruptions. 4th ed. WB Saunders; Philadelphia, PA: 2009. pp. 1007–1070. [Google Scholar]
- 4.Bucholz R.W., Heckman J.D., Court-Brown C.M. Rockwood and Green’s fractures in adults. In: Sagi H.C., editor. Pelvic ring fractures. 7th ed. Lippincott Williams & Wilkins; Philadelphia, PA: 2010. pp. 1415–1462. [Google Scholar]
- 5.Mears D.C., Durbhakula S.M. Fractures and dislocations of the pelvic ring. In: Chapman M.W., editor. Chapman’s orthopaedic surgery. 3rd ed. Lippincott Williams and Wilkins; Philadelphia: 2001. pp. 531–585. [Google Scholar]
- 6.Ziran B.H., Wasan A.D., Marks D.M., Olson S.A., Chapman M.W. Fluoroscopic imaging guides of the posterior pelvis pertaining to iliosacral screw placement. J Trauma. 2007;62:347–356. doi: 10.1097/01.ta.0000229789.18211.85. [DOI] [PubMed] [Google Scholar]
- 7.Ricci W.M., Mamczak C., Tynan M., Streubel P., Gardner M. Pelvic inlet and outlet radiographs redefined. J Bone Jt Surg Am. 2010;92:1947–1953. doi: 10.2106/JBJS.I.01580. [DOI] [PubMed] [Google Scholar]
- 8.Boulay C., Tardieu C., Hecquet J. Sagittal alignment of spine and pelvis regulated by pelvic incidence: standard values and prediction of lordosis. Eur Spine J. 2006;15:415–422. doi: 10.1007/s00586-005-0984-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Browner B.D., Jupiter J.B., Levine A.M., Trafton P.G., editors. Skeletal trauma: fractures, dislocations, ligamentous injuries. 2nd ed. WB Saunders; Philadelphia: 1998. [Google Scholar]
- 10.Mostafavi H.R., Tornetta P., III Radiologic evaluation of the pelvis. Clin Orthop Relat Res. 1996;329:6–14. doi: 10.1097/00003086-199608000-00003. [DOI] [PubMed] [Google Scholar]
- 11.Tile M., Rubenstein J. Defining the injury: assessment of pelvic fractures. In: Tile M., Helfet D.L., Kellem J.F., editors. Fractures of the pelvis and acetabulum. 3rd ed. Lippincott Williams and Wilkins; Philadelphia: 2003. pp. 101–115. [Google Scholar]
- 12.Pekmezci M., Rotter P., Toogood P., Morshed S., Kandemir U. Reexamination of pelvic inlet and outlet images using 3-dimensional computed tomography reconstructions. J Orthop Trauma. 2014;28:324–329. doi: 10.1097/BOT.0000000000000018. [DOI] [PubMed] [Google Scholar]