Abstract
A revisit to high riding jugular bulb with a newer classification. Observational study. Patients in the age group between 15 to 60 years, who underwent various Tympanomastoid and otosclerotic surgeries from April 2015 to 2018, have been included in the study. An analysis was made on high riding jugular bulb which encountered and different anatomical variations were noticed. A total of 531 patients underwent various tympanomastoid surgeries and 48 patients underwent otosclerotic surgeries. Out of which 8% of the cases (n = 49) were noticed to have high riding jugular bulb. In those 49 cases, 81% (n = 37) have Grade I, 11% (n = 5) have Grade II, 6% (n = 3) have grade III, 6% of the case (n = 3) have Grade IV and 2% (n = 1) has Grade V high riding Jugular bulb. Among these the prevalence of Grade I jugular bulb is high followed by Grade II. With the observation of our clinical study the authors have made a revisit to high riding jugular bulb and proposed a new clinical grading for high jugular bulb called BPH, that is Basava Prasad’s grading clinical on High jugular bulb (Channa Basava Hubli and K. C. Prasad) as: Grade I high riding jugular bulb up to the level of inferior tympanic annulus. Grade II extending from the level of tympanic annulus up to the inferior margin of the round window niche. Grade III Completely obliterating the round window niche. Grade IV Lies between superior margin of round window niche and stapes. Grade V Abuting the Stapes Arch.
Keywords: High riding jugular bulb, Tympanomastoid surgeries, Otosclerotic surgeries
Introduction
Jugular bulb is the expanded upper end of the jugular vein situated in the jugular fossa. Jugular bulb is a venous structure that can be located close to the inner ear. It’s not present at the time of birth. The size and location is dependent on the pneumatization of the mastoid bone. The size is not any criterion for any pathologies [1]. High riding jugular bulb is defined as an extension of the most cephalad portion of the Jugular bulb superior to the floor of the internal auditory canal or it can projects above the basal turn of the cochlea [2]. It could also be a diverticulum arising from the Jugular bulb. There may be a bony covering over the Jugular bulb or it may be lying in the middle ear mucosa next to the medial surface of the tympanic membrane. High riding jugular bulb has an intact sigmoid plate—a thin plate of bone separating the jugular bulb from the middle ear cavity. This can only be appreciated on thin slice bone algorithm CT, and is too thin to appreciate on MRI [3]. If the sigmoid plate is deficient, the bulb is free to protrude into the middle ear cavity, and is then known as a dehiscent jugular bulb and is a common cause of a retrotympanic vascular mass.
According to the literature, it’s a common venous anomaly with an incidence of 2.4–7% of temporal bones and fivefold higher prevalence of high jugular bulb in patients with ear related symptoms [4]. It can occur as a two different entity. Either there will be a dehiscence in the floor of the middle ear or it causes protrusion of the jugular bulb through this dehiscence or as a congenital variant associated with large jugular fossa and usually not associated with a dehiscent floor. Dehiscence of the floor can occur due to frequent infections, trauma, aneurysms or by tumour invasions [5].
Jugular bulb for its varying anatomical positions, it may extend laterally to the tympanic membrane or external auditory canal, medially to the petrous apex or inner ear. In rare cases the jugular bulb may extend upwards, elevating the floor of hypotympanum presenting in the middle ear space with a thinner or absent septum.
Most cases of high jugular bulb will be asymptomatic but symptoms have been reported. High-riding jugular bulb can cause pressure effects on the surrounding structures and include tinnitus and conductive hearing loss, which may be occurring due to turbulent blood flow through the aberrant anatomy resulting in unwanted sound transmission through the middle-ear apparatus. Symptoms may aggravated with conditions that increase the cardiac output. If it is medially located patient can present with vertigo, sensorineural hearing loss and tinnitus. High jugular bulb may also mimic Meniere’s disease showing severe acute vertiginous attacks, pulsatile tinnitus, and hearing loss [6].
If suspected preoperatively, investigation with CT angiography or venography may provide information regarding the anatomical location to aid surgical planning and to reduce complications.
In our clinical observational study these anatomical variations and analyzed and presenting a newer classification for a better perceptive of ear symptoms and signs for a clinician.
Materials and Methods
Patients in the age group between 15 to 60 years, who underwent various Tympanomastoid and otosclerotic surgeries from April 2015 to 2018 have been included in the study. An analysis were made on high riding jugular bulb which encountered and different anatomical variations were noticed.
All patients underwent otoscopic ear examinations, audiometry and impedance testing and other preoperative evaluations. All patients were noticed to have moderate hearing loss. They all were subjected for various tympanomastoid surgeries and otosclerotic surgeries.
Results
A total of 531 patients underwent various tympanomastoid surgeries and 48 patients underwent otosclerotic surgeries. Out of which 8% of the cases (n = 49) were noticed to have high riding jugular bulb. In those 49 cases, 81% (n = 37) have Grade I, 11% (n = 5) have Grade II, 6% (n = 3) have grade III, 6% of the case (n = 3) have Grade IV and 2% (n = 1) have Grade V high riding Jugular bulb. Among these the prevalence of Grade I jugular bulb is high followed by Grade II.
With the observation of our clinical study the authors have made a revisit to high riding jugular bulb and proposed a new grading for high jugular bulb called BPH (Figs. 1 and 2), that is Basava Prasad’s grading on High jugular bulb (Channa Basava Hubli and K. C. Prasad) as:
Fig. 1.
Schematic representation of BPH I- Grade I, II- Grade II, III- Grade III, IV- Grade IV and V-Grade V
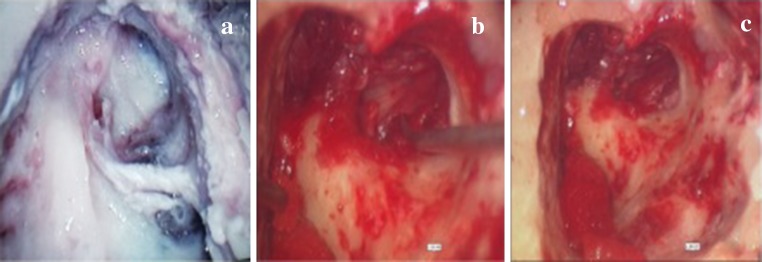
Fig. 2.
a Showing high jugular bulb covering the round window niche. b showing retracting the high jugular bulb with a pick c showing abutting the stapes arch
Grade I: High riding jugular bulb up to the level of tympanic annulus.
Grade II: Extending from the level of tympanic annulus up to the lower end of inferior margin of the round window niche.
Grade III: Completely obliterating the round window niche.
Grade IV: Lies between superior margin of round window niche and stapes.
Grade V: Abuting the Stapes Arch.
Discussion
High riding jugular bulb encountered during surgery was uncommon. It is the extension of the most cephalad portion of the jugular bulb superior to the floor of the internal auditory canal. Otoscopically it is seen as a blue mass behind an intact tympanic membrane, can be misdiagnosed as Glomus Tumor, which may become distended on Valsalva or ipsilateral jugular compression.
During the surgeries, if a mass have been encountered in the middle ear cavity never attempt for a biopsy. In various tympanomastoid surgeries and otosclerotic surgeries the tympanomeatal flap must be elevated with utmost care. In these conditions if CT scan is not done prior to these surgeries and if there is any suspicious mass in the floor of the middle ear cavity surgeons should think of high jugular bulb one should be careful while elevating the tympanomeatal flap. In such situations it should be done closely following the fibrous annulus in order to avoid noxious complications. During elicitation of round window reflex we should not push down the mass vigorously if there is any suspicious mass over the round window niche especially in Grade III to V.
Sometimes it can present as a sessile polypoidal lesion adherent to the middle ear cavity the surgeons should be suspicious and never attempt to take a biopsy. If in case there is presence of any squamous epithelium, like that of cholesteatoma, covering over the mass especially in case of Grade III and Grade IV high riding jugular bulb utmost care should be taken while removing the epithelium. Avoid usage of sharp instruments while working on the middle ear cavity near to the mass if there is any suspicion [7–9].
Encountering high riding jugular bulb abnormalities during ear surgery are a rare but recognized problem. It can complicate other surgeries like myringotomy and grommet insertion as if opened it can lead to problems like brisk venous haemorrhage.
A normal jugular bulb may produce only a slight indentation on the undersurface of the petrous bone and if its extending up to the superior petrous ridge posterior to the labrynth and internal auditory canal, it blocks access to the internal auditory canal. In such cases, we should not access to the internal auditory canal by translabrynthine approach especially in acoustic neuroma surgeries. It could also be a diverticulum arising from the jugular bulb. It can also mimic conditions like cholsteatoma or other neoplasms. High jugular bulb may also mimic Meniere’s disease showing severe acute vertiginous attacks, pulsatile tinnitus, and hearing loss [10, 11].
When discovered intraoperatively, care should be taken to avoid haemorrhage and in this event of this, prompt hemostastis is required. In case of massive bleeding a study showed the usage of transcatheter endovascular embolization using detachable coils have been used [12].
With our research we could not encounter any literature showing a Grade V high riding jugular bulb, we are reporting for the first time a case of high riding jugular bulb abuting the stapes arch.
Conclusion
High jugular bulb encountered during the surgery is uncommon and is often asymptomatic and silent. In view of its varied presentations we should be aware of and kept in mind different anatomical variations of jugular bulb, be clinically suspicious and introperatively vigilant to encounter the high jugular bulb and its complications during the surgery.
Acknowledgements
We are thankful to Dr S. M. Azeem Mohiyuddin Head of ENT and Head and Neck Surgery, Sri Devaraj Urs Medical College, Tamaka, Kolar for his helpful discussion and technical expertise. My sincere and great thanks for Jagan O. A., Lecturer, Clinical Virology Department, Amrita Institute of Medical Science and Research for supporting me and helping in editing the article.
Author Contributions
Indu Varsha Gopi: Contributed to the design of study, collected samples, did data analysis and drafted the manuscript. Corresponding author for the manuscript.; K. C. Prasad: Contributed to the design of study, data analysis, helped frame and edited the manuscript; Channa Basava Hubli: Contributed to the design of study, data analysis, helped frame and edited the manuscript; Gopinathan Pillai: Contributed to the design of study, data analysis, helped frame and edited the manuscript; Harshitha T. R.: Contributed to the design of study, data analysis, helped frame and edited the manuscript; Balan Ashok Kumar: Contributed to the design of study, data analysis, helped frame and edited the manuscript.
Compliance with Ethical Standards
Conflict of interest
The authors declare no conflict of interest or commercial affiliation related to this study.
Contributor Information
Kothegala Chandrashekariah Prasad, Email: drkcprasad@yahoo.co.in.
Channa Hubli Basava, Email: cvhubli5@yahoo.com.
Pillai N. Gopinathan, Email: gopidrent@gmail.com
Gopi Induvarsha, Email: indugopinath1826@gmail.com.
R. T. Harshita, Email: harshiblissful@gmail.com
Balan Kumar Ashok, Email: drbalanashok84@gmail.com.
References
- 1.Sismanis A. Tympanoplasty glasscock-shambaugh surgery of the ear. 5. New York: Elsevier; 2002. pp. 463–485. [Google Scholar]
- 2.Sashidharan V, Joseph A, Abhraham SS, Hiremath SB. Case report on high riding jugular bulb: a rare entity. Indian J Otol. 2014;20(3):129. doi: 10.4103/0971-7749.136863. [DOI] [Google Scholar]
- 3.Sterkers O, Bozorg AG, Julien N, Bouccara D, Rihane S, Chaigne P (1993) Jugular bulb diverticulum mimicking Menière’s disease. Surgical treatment. In: Annales d’oto-laryngologie et de chirurgie cervico faciale: bulletin de la Societe d’oto-laryngologie des hopitaux de Paris, vol 110, No. 7, pp 363–371 [PubMed]
- 4.Kim MJ, Kwack BG, Cha HE, Han GC. Jugular bulb diverticulum mimicking Meniere’s disease: case report. Int Adv Otol. 2013;9(1):135–139. [Google Scholar]
- 5.Friedmann DR, Eubig J, Winata LS, Pramanik BK, Merchant SN, Lalwani AK. Prevalence of jugular bulb abnormalities and resultant inner ear dehiscence: a histopathologic and radiologic study. Otolaryngol Head Neck Surg. 2012;147(4):750–756. doi: 10.1177/0194599812448615. [DOI] [PubMed] [Google Scholar]
- 6.Couloigner V, Grayeli AB, Bouccara D, Julien N, Sterkers O. Surgical treatment of the high jugular bulb in patients with Meniere’s disease and pulsatile tinnitus. Eur Arch Otorhinolaryngol. 1999;256(5):224–229. doi: 10.1007/s004050050146. [DOI] [PubMed] [Google Scholar]
- 7.Atmaca S, Elmali M, Kucuk H. High and dehiscent jugular bulb: clear and present danger during middle ear surgery. Surg Radiol Anat. 2014;36(4):369–374. doi: 10.1007/s00276-013-1196-z. [DOI] [PubMed] [Google Scholar]
- 8.Weiss RL, Zahtz G, Goldofsky E, Parnes H, Shikowitz MJ. High jugular bulb and conductive hearing loss. The Laryngoscope. 1997;107(3):321–327. doi: 10.1097/00005537-199703000-00008. [DOI] [PubMed] [Google Scholar]
- 9.Sayit AT, Gunbey HP, Fethallah B, Gunbey E, Karabulut E. Radiological and audiometric evaluation of high jugular bulb and dehiscent high jugular bulb. J Laryngol Otol. 2016;130(11):1059–1063. doi: 10.1017/S0022215116009166. [DOI] [PubMed] [Google Scholar]
- 10.Friedmann DR, Le BT, Pramanik BK, Lalwani AK. Clinical spectrum of patients with erosion of the inner ear by jugular bulb abnormalities. The Laryngoscope. 2010;120(2):365–372. doi: 10.1002/lary.20699. [DOI] [PubMed] [Google Scholar]
- 11.Friedmann DR, Eubig J, Winata LS, Pramanik BK, Merchant SN, Lalwani AK. A clinical and histopathologic study of jugular bulb abnormalities. Arch Otolaryngol Head Neck Surg. 2012;138(1):66–71. doi: 10.1001/archoto.2011.231. [DOI] [PubMed] [Google Scholar]
- 12.Vachata P, Petrovicky P, Sames M. An anatomical and radiological study of the high jugular bulb on high-resolution CT scans and alcohol-fixed skulls of adults. J Clin Neurosci. 2010;17(4):473–478. doi: 10.1016/j.jocn.2009.07.121. [DOI] [PubMed] [Google Scholar]