Abstract
Twenty five patients of aural polyp who underwent canal wall down mastoidectomy were analysed retrospectively. Histopathological examination revealed cholesteatoma in 22 (88%) patients. However, histopathological diagnosis in 3 of these patients was unusual and rare benign tumors of the middle ear cleft-meningioma, neurilemmoma and capillary hemangioma. Review of the preoperative High Resolution Computed Tomography (HRCT) temporal bone revealed an unusual picture in all of the three cases. Features noted were: widening of the jugular foramen (meningioma), destruction of the anterior wall of mesotympanum (neurilemmoma), enhancing soft tissue density lesion (capillary hemangioma). Further, there was only partial loss of pneumatisation of the mastoid air cells in all of the 3 cases. It was observed that though HRCT temporal bone is a commonly advised investigation in patients of chronic otitis media (COM) with aural polyp, meticulous interpretation may reveal unusual features pointing towards sinister diagnosis. Conclusion: Aural polyp with preservation of pneumatisation of mastoid air cells points towards diagnosis other than COM.
Keywords: High-resolution computed tomography (HRCT), Aural polyp, Chronic otitis media (COM), Mastoid pneumatisation
Introduction
Chronic Otitis Media (COM) with or without cholesteatoma may be associated with the formation of an aural polyp which is usually confined to middle ear and external auditory canal (EAC) but may sometimes protrude outside the EAC. Owing to the high prevalence of COM and similar clinical features of ear discharge, hearing loss and an aural polyp, it is not surprising that recognition of other pathologies may be inadvertently missed/misinterpreted by ENT surgeons as well as radiologists. Further, preoperative biopsy of an aural polyp may not establish the correct diagnosis in these cases as it is from the most peripheral part of polyp. This may influence the management especially surgery. HRCT temporal bone is the imaging modality of choice for most of the pathological conditions of the temporal bone, which has a complex anatomy with multiple small structures. The present study was undertaken to evaluate the role of HRCT temporal bone in the diagnosis of patients initially diagnosed clinicoradiologically as squamosal COM with an aural polyp.
Materials and Methods
This was a retrospective study of 25 patients with the diagnosis of squamosal COM with an aural polyp who underwent canal wall down mastoidectomy. The cases which presented as polypoid mass, with suspicion of malignancy and preoperative biopsy reported as squamous cell carcinoma were excluded from the study. The available records of the patients were retrieved and analysed. The patients’ age, sex, detailed history with special emphasis on presenting symptoms and history of surgery was noted. Physical examination included the appearance, friability and site of origin of an aural polyp. HRCT temporal bone reports/films, surgical notes, and histopathological reports were reviewed. The protocol of the investigations and surgery was in accordance with the hospital norms. The patients were investigated and operated as a part of routine procedures after obtaining written informed consent from each participant or each participant’s guardian.
Observations and Results
There were 13 males and 12 females in our study. The mean age of patients was 26.88 years (range 7–53 years). The maximum number of patients (21) were between 10 to 40 years. The duration of ear symptoms ranged from 7 months to 12 years. Aural polyps were more on the right side in comparison to the left side (56 vs 44%). Table 1 shows findings on preoperative HRCT temporal bone. Histopathologically, majority of the cases (22) were of squamosal COM, however, there was one case each of meningioma, neurilemmoma and capillary hemangioma (Table 2).
Table 1.
Findings on preoperative HRCT temporal bone
| HRCT findings | Number of patients | Percentage |
|---|---|---|
| Non enhancing soft tissue density lesion in the tympanic cavity, aditus and antrum | 24 | 96 |
| Enhancing soft tissue density lesion in the tympanic cavity, aditus and antrum | 1 | 4 |
| Ossicular erosion | 24 | 96 |
| Lateral semicircular canal erosion with fistula | – | – |
| Tegmen tympani erosion | 2 | 8 |
| Sinus plate erosion | 1 | 4 |
| Facial canal erosion | 1 | 4 |
| Jugular foramen widening | 1 | 4 |
| Erosion of anterior wall of the middle ear | 1 | 4 |
Table 2.
Distribution of diseases
| Diagnosis | Number of patients | Percentage |
|---|---|---|
| Squamosal COM | 22 | 88 |
| Meningioma | 1 | 4 |
| Neurilemmoma | 1 | 4 |
| Capillary hemangioma | 1 | 4 |
Discussion
An aural polyp in the external auditory canal (EAC) may arise from (a) the external auditory canal, (b) middle ear as various lesions of the middle ear can fungate through the tympanic membrane and cause appearance of a polypoid mass in the external auditory canal, (c) from the adjacent structures such as parotid gland and temporomandibular joint (due to secondary invasion by the disease from these sites) [1, 2]. These polypoid masses are commonly inflammatory in nature, however, this may also be manifestation of more severe disease. Gliklich et al. [2] reported that chronic otitis media (43%), cholesteatoma (29%), and retained tympanostomy tubes (23%) were the common causes of aural polyps, unusual causes included mycobacterial infection and Langerhans cell histiocytosis. The incidence of either granulomatous or neoplastic disease is estimated at up to 3% of surgical specimens in some studies [2, 3].
Aural polyps clinically manifest with common symptoms of decreased hearing, ear discharge or fullness in the ear. An aural polyp which is not attached with the walls of the EAC and is not resolved with topical antibiotics and corticosteroids is commonly diagnosed to be due to squamosal COM because of high incidence of association of these masses with squamosal COM. Further, preoperative biopsy of the aural polyps in these patients may delay the correct diagnosis if the sample is obtained from the most peripheral site of the lesion which is not the representative area. Xenellis et al. analysed 185 consecutive patients with chronic otitis media; 75 showed a polypoid mass in the EAC. In 65(86.7%) out of the 75 patients histological examination after mastoidectomy revealed cholesteatoma. In the remaining 10 (13.3%) cases, the histological diagnosis was: glomus tumor, melanoma, mucosal adenoma, fibrous dysplasia, squamous cell carcinoma, adenoma of the endolymphatic sac, encephalocoele and tuberculosis [4].
In the present study 22 out of the 25 (88%) cases showed evidence of cholesteatoma. In the remaining 3 (12%) cases, the histological diagnosis was: meningioma, neurilemmoma and capillary hemangioma involving the middle ear and mastoid. Wrong clinical diagnosis, as unsafe ear in 2 out of these 3 cases was reinforced by misreading HRCT temporal bone findings by the radiologist, who gave final impression as “radiological findings are suggestive of squamosal COM. Also, in one of our cases (neurilemmoma) preoperative biopsy of the polypoid mass was reported histologically as inflammatory polyp. This may be due to the secondary inflammatory response in the lesion.
In the present study we tried to evaluate whether HRCT temporal bone could help in the diagnosis of unusual lesions in patients initially diagnosed as squamosal COM with an aural polyp.
On CT examination, squamosal COM demonstrates a soft tissue opacification in the middle ear cavity with or without the involvement of the mastoid [5]. Since a soft tissue attenuation is a common finding in most of the middle ear pathologies, careful analysis of the soft tissue is crucial in order to facilitate differential diagnosis [6, 7]. Evaluation of middle ear soft tissue is most commonly done with HRCT using the “bone algorithm”. Unless a vascular abnormality or another enhancing lesion such as a tumor is suspected, studies are usually performed without intravenous contrast administration. While interpreting HRCT images attention should be paid to location and extent of the soft tissue, bone erosion, CT attenuation value and contrast enhancement (if any) [8]. On HRCT temporal bone, a cholesteatoma appears as a soft tissue mass within the tympano-mastoid cavity (non-dependant location), it is usually accompanied by bone erosion involving the wall of the epitympanum and ossicles (the erosion of the long process of incus is commonest) [9]. In tuberculosis of the middle ear, HRCT reveals a soft tissue occupying the middle ear-mastoid region, which may extend into the external auditory canal but without bony erosions. The mastoid air cells would be preserved with absence of sclerosis [10]. This was also observed in all the three unusual lesions e.g., meningioma, neurilemmoma, capillary hemangioma. In Langerhans cell histiocytosis (LCH) the mastoid is commonly involved, the typical finding being a lytic, “punched out” bone lesion. Erosion of the postero-superior bony canal wall is common though involvement of the middle ear and ossicles is rare [11]. Glomus tumor shows soft tissue on the cochlear promontory (Glomus tympanicum) or at jugular fossa extending to hypotympanum (Glomus jugulare). Glomus tumor shows prominent contrast enhancement and may show bony erosion [12]. Key HRCT finding in facial nerve schwannoma is smooth expansion of the facial nerve canal and it may show enhancement. Hemangioma of the middle ear shows soft tissue density with or without associated ossicular or bone erosion [8]. Malignant tumors involving the middle ear appear as enhancing soft tissue on HRCT, usually with evidence of bone destruction [12].
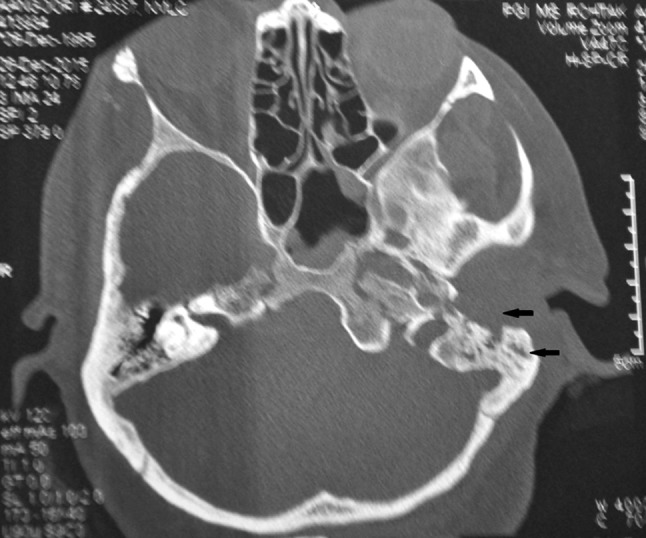
In our study HRCT films were reviewed and discussed with experienced radiologist. In the patient diagnosed histologically as meningioma, the preoperative CT showed soft tissue density lesion in the middle ear and mastoid with widening of the jugular foramen (Fig. 1). Table 3 enumerates the benign and malignant causes of soft tissue density lesions of the middle ear causing widening of the jugular foramen [12–14]. HRCT temporal bone in neurilemmoma patient showed soft tissue density lesion in the middle ear and mastoid with erosion of the anterior wall of middle ear and only partial loss of pneumatisation of the mastoid air cells (Fig. 2). This picture is unusual in squamosal COM and point towards an alternative diagnosis. In the patient diagnosed histologically as capillary hemangioma of the middle ear, the preoperative CT showed enhancing soft tissue density mass involving the middle ear without widening of the jugular foramen (Fig. 3). Table 4 enumerates the benign and malignant causes of enhancing soft tissue density lesions of the middle ear with and without widening of jugular foramen [12, 15]. In all of these cases the initial diagnosis was squamosal COM. Correct interpretation of the radiological images preoperatively in these cases along with sufficient clinical information would have narrowed the differential diagnosis.
Fig. 1.

HRCT Temporal bone (axial section), of the patient diagnosed histologically as meningioma, showing widening of the jugular foramen on the right side and presence of pneumatisation
Table 3.
| Benign | Malignant |
|---|---|
| Glomus jugulare | Metastasis |
| Schwannoma jugular foramen | Skull base chondrosarcoma |
| Meningioma jugular foramen | Skull base plasmacytoma |
| Pseudomasses |
Fig. 2.

HRCT temporal bone (axial section), of the patient diagnosed histologically as neurilemmoma, showing soft tissue density in the tympanic cavity, aditus and antrum with erosion of the anterior wall of the middle ear and only partial loss of pneumatisation of the mastoid air cells
Fig. 3.
HRCT temporal bone (axial section), of the patient diagnosed histologically as capillary hemangioma of the middle ear, showing enhancing soft tissue density mass in the middle ear without widening of the jugular foramen on the left side and partial loss of pneumatisation of mastoid air cells
Table 4.
| Benign | Malignant | Enhancing lesions with jugular foramen widening | Enhancing lesions without jugular foramen widening |
|---|---|---|---|
| Paraganglioma (glomus tympanicum) | Primary malignancy | Paraganglioma (glomus jugulare) | Paraganglioma (glomus tympanicum) |
| Paraganglioma (glomus jugulare) | Metastasis | Jugular bulb (dehiscent) | Hemangioma |
| Jugular bulb (dehiscent) | Rhabdomyosarcoma | Schwannoma (jugular foramen) | Adenoma |
| Hemangioma | Meningioma (jugular foramen) | ||
| Schwannoma | Metastasis | ||
| Meningioma | |||
| Adenoma | |||
| Langerhans cell histiocytosis |
In conclusion, this study highlights the importance of utilising HRCT temporal bone in patients presenting with aural polyps in the EAC. Correct preoperative interpretation will not only avoid unnecessary surgical interventions but also major complications e.g., cases have been reported in which aural polypectomy was done in patients with pseudoaneurysm of internal carotid artery (presenting as aural polyp) with resultant torrential bleeding [16]. Further, in the presence of pneumatisation in patients with an aural polyp, one must suspect diagnosis other than COM.
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Statement
Informed consent was taken at the time of surgery. This study is a retrospective analysis of operated patients. The investigations (CT scan) and surgery is routinely done worldwide and in our hospital, so no ethical aspect is involved in this study.
References
- 1.Friedmann I. Pathological lesions of the external auditory meatus: a review. J R Soc Med. 1991;83:34–37. doi: 10.1177/014107689008300115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gliklich RE, Cunningham MJ, Eavy RD. The cause of aural polyps in children. Arch Otolaryngol Head Neck Surg. 1993;119:669–671. doi: 10.1001/archotol.1993.01880180089016. [DOI] [PubMed] [Google Scholar]
- 3.Williams SR, Robinson PJ, Brightwell AP. Management of the inflammatory aural polyp. J Laryngol Otol. 1989;103:1040–1042. doi: 10.1017/S0022215100110916. [DOI] [PubMed] [Google Scholar]
- 4.Xenellis J, Mountriha K, Maragoudakis P. A histological examination in the cases of initial diagnosis as chronic otitis media with a polypoid mass in the external ear canal. Auris Nasus Larynx. 2011;38:325–328. doi: 10.1016/j.anl.2010.10.002. [DOI] [PubMed] [Google Scholar]
- 5.Anbarasu A, Chandrasekaran K, Balakrishnan S. Soft tissue attenuation in middle ear on HRCT: pictorial review. Indian J Radiol Imaging. 2012;22:289–304. doi: 10.4103/0971-3026.111483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Trojanowska A, Drop A, Trojanowski P, Rosinska-Bogusiewicz K, Janusz K, BobekBillewicz B. External and middle ear diseases: radiological diagnosis based on clinical signs and symptoms. Insights Imaging. 2012;3:33–48. doi: 10.1007/s13244-011-0126-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lemmerling MM, De Foer B, VandeVyer V, Vercruysse JP, Verstraete KL. Imaging of the opacified middle ear. Eur J Radiol. 2008;66:363–371. doi: 10.1016/j.ejrad.2008.01.020. [DOI] [PubMed] [Google Scholar]
- 8.Swartz JD. The middle ear and mastoid. In: Swartz JD, Loevner LA, editors. Imaging of the temporal bone. 4. NewYork: Thieme; 2009. pp. 58–246. [Google Scholar]
- 9.Nevoux J, Lenoir M, Roger G, et al. Childhood cholesteatoma. Eur Ann Otorhinolaryngol Head Neck Dis. 2010;127:143–150. doi: 10.1016/j.anorl.2010.07.001. [DOI] [PubMed] [Google Scholar]
- 10.Vaid S, Lee YYP, Rawat S. Tuberculosis in the head and neck: a forgotten differential diagnosis. Clin Radiol. 2010;65:73–81. doi: 10.1016/j.crad.2009.09.004. [DOI] [PubMed] [Google Scholar]
- 11.Irving RM, Broadbent V, Jones NS. Langerhans cell histiocytosis in childhood: management of head and neck manifestations. Laryngoscope. 1994;104:64–70. doi: 10.1288/00005537-199401000-00011. [DOI] [PubMed] [Google Scholar]
- 12.Juliano AF, Maya MM, Lo WW, Kovanolikaya I. Temporal bone tumors and cerebellopontine angle lesions. In: Som PM, Curtin HD, editors. Head and neck imaging. 5. St Louis: Elsevier Mosby; 2011. pp. 1263–1408. [Google Scholar]
- 13.Vogl TJ, Bisdas S. Differential diagnosis of jugular foramen lesions. Skull Base. 2009;19:3–16. doi: 10.1055/s-0028-1103121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Molony TB, Brackmann DE, Lo WW. Meningiomas of the jugular foramen. Otolaryngol Head Neck Surg. 1992;106:128–136. doi: 10.1177/019459989210600202. [DOI] [PubMed] [Google Scholar]
- 15.Harnsberger HR, et al. Enhancing middle ear lesions. In: Harnsberger HR, Glastonbury CM, Michael MA, Koch BL, Philips CG, Mosiel KM, et al., editors. Expert DD head and neck. Utah: Lippincott Williams and Wilkins; 2009. pp. 30–33. [Google Scholar]
- 16.Johnson M, Madhavakurup V, Sandeep AV. Pseudo aneurysm of petrous internal carotid artery presenting as aural polyp. Indian J Otol. 2013;19:27–29. doi: 10.4103/0971-7749.108163. [DOI] [Google Scholar]


