Abstract
Management of traumatic facial nerve injuries after temporal bone fractures is both challenging and controversial. The dilemma is whether to operate or not and if operating, when to operate and how much of the nerve to decompress. The aim of this study is to review our criteria for decision making in management of patients with temporal bone fracture induced facial nerve palsy, and analyze outcome of patients selected for surgical management. Review of 28 cases of temporal bone fracture between 2012 and 2016 was carried out. Patient assessment included clinical, audiological, computer tomography scans and electromyography (EMG) examinations. All 28 cases were initially started on conservative medical treatment. Based on criteria of complete clinical paralysis at onset, no improvement with conservative treatment and fibrillation potential in EMG, 10 cases underwent surgical decompression through the transmastoid approach. Among the 10 surgically-treated patients, lesions were predominantly found in geniculate ganglion area. Analysis of results after 12 months revealed 70% of cases who underwent surgery had House Brackmann (HB) Grade I–II recovery. Good recovery was achieved in all 18 medically treated patients (HB Grade I–II). Candidate selection based on accurate clinical judgment and judicious use of electrodiagnostic tests plays a vital role in outcomes in the treatment of post traumatic facial injury. Early surgical intervention gave better results in our study.
Keywords: Head injury, Post-traumatic facial palsy, Temporal bone fractures
Introduction
Facial nerve injuries result in devastating psychological and physical deformities which are difficult to hide. The facial nerve is affected in 7–10% of temporal bone fractures, commonest mode of injury being road traffic accidents [1, 2]. These injuries can have permanent disabling facial deformity as sequelae, if they are not treated promptly and effectively.
Traumatic facial palsy may be immediate when the onset begins within hours post injury or delayed due to secondary ischemia caused by edema in the fallopian canal. Onset of facial palsy can be unnoticed due to facial swelling caused by lacerations and abrasions [3].
High resolution computer tomography (HRCT) of the head remains the gold standard of investigation in cases of head trauma with facial nerve injuries. Temporal bone fractures have traditionally been divided into longitudinal, transverse or mixed fractures, based on the relation of the fracture line with the axis of the petrous bone as first described by Ulrich [4]. The Longitudinal fractures are most common (70–80%), followed by transverse (10–20%) and mixed (10%) fractures [5].
Electrophysiology diagnostic techniques for facial nerve functional analysis commonly used are nerve excitability test (NET), electroneuronography (ENoG), electromyography (EMG), and maximum stimulation test (MST). Ulug and Arif Ulubil advocate the early use of ENoG in the first 6 days after the onset of facial paralysis [6]. Electromyography (EMG) is useful when more than 2 weeks have passed after the onset of paralysis. It is generally believed that surgical exploration should be considered if ENOG shows a bilateral amplitude ratio of > 90% or NET shows a difference of > 3.5 mA or MST shows no reaction, especially when combined with EMG examination revealing fibrillation potentials indicating complete loss of nerve function with no recovery.
Controversies remain regarding correct management of facial nerve trauma. The dilemma includes which patients to operate, when to operate, and the preferred surgical approach to the injured segment. Treatment protocols are generally based on onset of facial weakness (immediate or delayed) and extent of facial weakness. Early onset and/or complete facial palsy indicate disruption of continuity of the nerve. A delayed onset and/or partial paresis of the nerve on the other hand, suggest secondary swelling or compression of the nerve which is more likely to recover spontaneously and hence surgery may be avoided [2].
In this study we present our experience of managing 28 patients of facial paralysis resulting from fracture of the temporal bone. The criteria for selection for surgery in these cases were immediate onset clinical HB grade V–VI palsy, no improvement in facial functions as determined by clinical examination and presence of fibrillation potential on EMG. Cases showing evidence of clinical recovery or presence of voluntary polyphasic reinnervation potentials on EMG, were managed by non surgical conservative measures only. Results were analyzed for efficacy of this strategy in management of facial nerve injury in temporal bone fractures.
Materials and Methods
A retrospective study was carried out on 28 cases of temporal bone fracture reporting between 2012 and 2016 to a multi specialty tertiary care center in Eastern India.
Inclusion Criteria
Patients with intratemporal facial nerve palsy who were managed with a minimum 12 months post-operative follow up after obtaining institutional ethical clearance and informed consent from the patients.
Exclusion Criteria
Patients with supranuclear facial nerve palsy and other intracranial complications post injury.
Injuries to the extra temporal part of the facial nerve.
Patients with less than 12 months follow up.
All patients underwent a thorough clinical otoneurological evaluation by otoscopy and tuning fork tests. Audiological evaluation in form of Pure tone audiometry and tympanometry and stapedial reflex were done in all cases. The mean thresholds at 0.5, 1, 2 and 3 kHz, were used for audiometric evaluation of hearing loss.
Facial nerve analysis was done by the House–Brackmann (HB) grading system. All cases underwent a HRCT of the head. Serial EMG was done after 2 weeks of onset of facial palsy. EMG was followed up weekly. Presence of polyphasic reinnervation potential was criteria for conservative therapy while presence of fibrillation potential was criteria for surgical intervention.
Medical Treatment—medical treatment was instituted with tapering dose of Tab Prednisolone, starting with 1 mg/kg/day over 3 weeks in all cases. Physiotherapy and rehabilitation measures were exhibited in all cases.
Criteria for surgical intervention—Cases in which EMG displayed total denervation fibrillation potentials, when the facial palsy was of immediate onset and complete and when there was no improvement with medical and supportive therapy.
Surgical Procedure
All the patients underwent extended subtotal facial nerve decompression via the transmastoid approach. Following a standard postauricular incision, cortical mastoidectomy followed by extended posterior tympanotomy was performed. The facial nerve was exposed throughout its vertical segment to the stylomastoid foramen. Labrynthine segment, first genu and tympanic segment were decompressed after removal of the incus and malleus head where required. The final thin layer of bone overlying the nerve was removed with blunt elevators. The nerve sheath was slit and the facial nerve was decompressed. Bone spicules or hematoma around the facial nerve were removed when present. General surgical principles in the use of diamond-tipped burrs by copious irrigation to remove bone and prevent additional thermal trauma to the facial nerve were ensured. In patients with simultaneous ossicular chain fracture or dislocation and in cases where the incus was removed, suitable ossiculoplasty was carried out either with relevant prosthesis or by refashioning the incus.
Etiology of the traumatic facial paralysis, treatment modalities exhibited, intraoperative findings and the results of the treatment were noted. The patients were followed up and progress noted at 3, 6 and 12 months after surgery.
Observations and Results
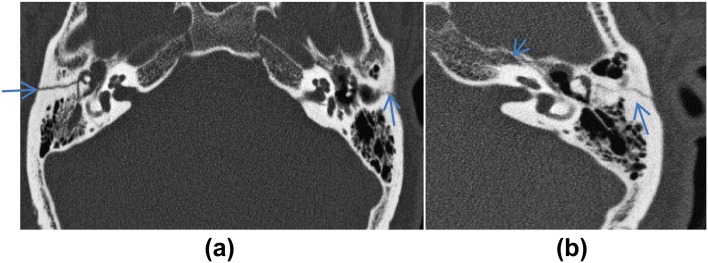
The age of the patients in our study varied from 12 to 48 years, with a mean age of 25. Of the 28 cases, 23 (82.14%) were male and 5(17.86%) were female. Road Traffic accident, 24 cases (85.7%), was the most common cause followed by fall in 3 cases (10.7%) and 1 case (3.6%) due to assault. Facial paralysis involved the right side in 17 patients, the left side in 10 cases and 1 patient had bilateral facial palsy due to bilateral temporal bone fractures (Fig. 1a). Longitudinal fractures were seen in 22 cases, transverse fractures in 4 cases, and mixed fracture in 2 cases in HRCT of the head (Fig. 1b). Facial paralysis was of immediate onset in 15 of the 28 cases whereas facial paralysis was delayed beyond 2 days in other 13 cases.
Fig. 1.
CT scans showing: a bilateral and b mixed temporal bone fractures
10 of the 28 cases of facial palsy underwent facial nerve exploration. All the cases taken up for surgical management were of immediate onset and had HB grade V–VI palsy and showed no improvement in facial functions as determined by clinical and electrodiagnostic tests. 8 of these cases underwent facial nerve exploration within 1 month of onset while 2 cases underwent surgery between 1 and 3 months after injury as they were recovering from other injuries. Remaining 18 patients were managed conservatively with oral steroids and physiotherapy. The cases were followed up clinically and by serial EMG. Details of findings and follow up of these cases are summarized in Table 1.
Table 1.
Results of cases managed non surgically
| Total cases | House Brackmann grade | House Brackmann grade—at onset | House Brackmann grade—after therapy (12 month) | |
|---|---|---|---|---|
| Non surgical cases | 18 | I–II | 7 | 14 |
| III–IV | 9 | 4 | ||
| V–VI | 2 | – |
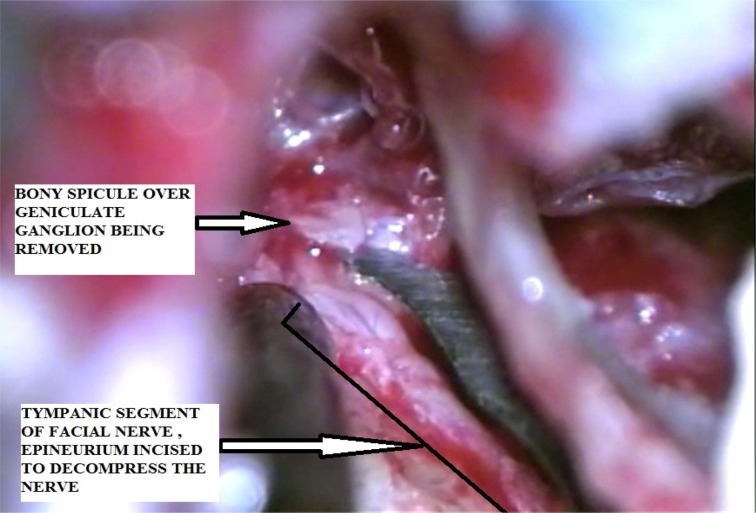
Operative Findings
Sites of injury, type of fracture and intraoperative facial nerve findings are summarized in Table 2. The most common affected area of the facial nerve by trauma was the geniculate ganglion (Fig. 2).
Table 2.
Preoperative and intraoperative findings of cases that underwent facial nerve decompression
| Sl no. | Age/sex | Cause | Site of paralysis | Type of fracture on HRCT | Intraoperative finding of facial nerve |
|---|---|---|---|---|---|
| 1 | 24/M | RTA | Left | Longitudinal | Edema of tympanic part of facial nerve |
| 2 | 29/M | RTA | Right | Longitudinal | Compression of geniculate ganglion with bony fragment, and edema |
| 3 | 21/M | RTA | Left | Longitudinal | Edema and granulation tissue in peri geniculate area |
| 4 | 24/M | Fall | Right | Transverse | Granulation tissue in the vertical segment of the nerve |
| 5 | 36/M | RTA | Left | Longitudinal | Granulation and compression with bony fragment at geniculate area |
| 6 | 32/M | RTA | Left | Longitudinal | Edema and hyperaemia in geniculate ganglion |
| 7 | 26/M | RTA | Right | Mixed | Haematoma and granulation on geniculate ganglion |
| 8 | 40/M | Fall | Left | Longitudinal | Granulation tissue and edema at tympanic segment of nerve |
| 9 | 28/M | Fall | Right | Transverse | Diffuse edema and fibrosis in vertical segment |
| 10 | 24/M | RTA | Bilateral | Longitudinal (left) and mixed (right) | Haematoma and compression with bone chips over geniculate ganglion (right) |
Fig. 2.
Intraoperative picture showing injury to facial nerve at geniculate ganglion area
Postoperative Results
The minimum follow-up period was 12 months and results evaluated accordingly. Clinical and Electrophysiological evaluation was performed every 3 months. Results analyzed after 1 year of follow up revealed a recovery to grade II HB in 7 cases and to grade III to IV in 3 other cases. In the 8 cases who underwent surgery within 1 month of onset, the results were HB Grade I–II in 7 cases and Grade III in 1 case. In the cases operated after 1 month of onset, HB Grade III was achieved in one case and Grade IV in one case (Table 3). 18 cases managed conservatively based on clinical improvement and presence of nerve conductivity on EMG, had recovery to HB grade I–II in 14 cases and III–IV in 4 cases (Table 1).
Table 3.
Time of surgery post trauma and outcome of surgical decompression of facial nerve
| Sl no. | Preop House Brackmann grade | Time of surgery (in weeks) | Post op House Brackmann grade (at 12 months) |
|---|---|---|---|
| 1 | VI | 3 | II |
| 2 | VI | 2 | II |
| 3 | V | 4 | II |
| 4 | VI | 3 | II |
| 5 | V | 4 | III |
| 6 | VI | 3 | I |
| 7 | V | 11 | III |
| 8 | VI | 3 | II |
| 9 | VI | 3 | II |
| 10 | V | 8 | IV |
Post Operative Complications
Mild conductive hearing loss was seen in 5 of the 7 cases who underwent ossicular reconstruction. Three months after surgery average conductive hearing loss was 18 dB. No serious complication, including sensorineural hearing loss and meningitis, was seen.
Discussion
Facial nerve paralysis is the most noticeable cranial neuropathy having tremendous psychological, emotional and social impact. Patients often present late to the otologist as management of associated neurosurgical emergency precedes the management of facial nerve trauma. Indication and timing of the facial nerve decompression for facial paralysis and the anatomical extent of decompression has been a subject of controversy for years. In our study of 28 cases of facial nerve injury following temporal bone fracture, 10 patients underwent surgical decompression and 18 cases were managed conservatively.
Motor vehicle accident reportedly is the most common cause of facial nerve trauma following temporal fractures [3]. Commonest cause in our study was also road traffic accidents (85.7%).
Coker et al. [7] have reported that 14 of 18 patients with temporal bone fracture who needed to have facial nerve exploration had longitudinal fracture. Ulug and Ulubil reported 7 of 11 fractures to be of longitudinal type in their surgical treatment series. All the cases had pathology involving the geniculate ganglion or perigenicullate areas [6]. In our study also, longitudinal fractures were more common than transverse or mixed type and the commonest site of injury was found to be in region of geniculate ganglion (6 out of 10 cases). Granulation tissue, edema and compression by multiple bone chips were the main intraoperative findings in our patients as described in Table 2.
Electrodiagnostic tests play an important role in decision making for surgical management in cases of facial nerve injury. ENoG although at present is the most accurate test for guiding treatment, often is unfeasible to perform in a polytrauma case or is not readily available. Traditional electromyography (EMG) is most useful more than 2 weeks after the onset of paralysis. Needle EMG may be used intraoperatively early after an injury has occurred to test integrity of the facial nerve [8]. Electroneurography (ENoG) showing more than 90% of facial nerve degeneration and electromusculography (EMG) revealing no regeneration potentials are identified as surgical indications. In our centre due to nonavailablity of ENoG, our study was based on EMG findings. Presence of fibrillation potentials was a definite indication of surgical management. In cases with incomplete paralysis, the presence of voluntary polyphasic reinnervation potentials on EMG, were found to be a good prognostic factor and the best indicator that regeneration is taking place. Such cases were managed conservatively. Our results of recovery to HB Grade I and II in all such cases match a similar study by Dahiya et al. [9].
Recommendations for exploration of the traumatic facial nerve remain contentious and based on personal opinion and data. Many studies profess the utility of surgery as the outcome was found to be poor without surgical intervention [6]. However, certain studies prefer conservative management in such cases. Darrouzet [10] reported about 94% recovery in patients managed conservatively. They therefore question the benefit of surgical intervention in cases of post traumatic facial paralysis. In our series, 18 patients who underwent non surgical conservative management also had good recovery of facial nerve function (Table 1).
The surgical approach to the facial nerve is controversial in such cases. Basis of approach depends on site of injury, association with hearing loss and CSF leak. While some advocate limited exploration of the facial nerve based on clinical and radiographic information, Fisch advocates a total facial nerve exploration and decompression by a middle fossa and transmastoid approach and in patients with total hearing loss, a translabyrinthine approach [11]. In our study of 10 cases managed by the transmastoid approach, we could approach the perigeniculate area after dislocation of the incudo malleolar joint. We found this approach to be simple, safe and effective. A similar approach and results were achieved by Hai Jin et al. [12] in a series of 26 cases.
Timing of surgery is another controversial area in management of traumatic facial nerve palsy. Early exploration is advocated for immediate onset facial nerve injuries [13]. A systematic review of 6 studies showed early intervention (before 2 weeks) had better results than those undergoing surgery after 2 weeks [14]. Decompressive surgery is however frequently delayed in patients having polytrauma for reasons such as, treatment of life threatening injuries suffered in the original trauma, referral delay, or poor neurological status. Studies of delayed surgery are at variance in their opinion. Studies such as by Sanus et al. [15] and Quaranta et al. [16] advocate exploration even after late presentations post injury. However, Liu et al. [17], attained HB grade I/II in only 66.7% cases who underwent decompression between 9 and 14 weeks after injury. Though in our study there were only 2 patients operated after 1 month of onset of facial palsy but the results in these two patients were poorer than those who were operated earlier post onset of trauma.
The rate of recovery to HB Grade I–II after facial nerve exploration in our series is 70% and to grade III or IV in 30%. Stretch, compression injuries with disruption of the endoneurial tubules undetectable at the time of surgery may be associated with suboptimal results. The follow-up results of our study are comparable with those of other studies [2, 6].
Conclusion
Despite various studies, approach to the management of intratemporal facial paralysis following trauma remains controversial. Our criteria for surgical intervention based on the non-progression of clinical status and absence of regeneration potentials on EMG gave satisfactory results. Further larger studies, preferably multi-centric is the road ahead in removing the dust on such contentious issues.
Conflict of interest
All authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed were in accordance with the ethical standards of the institutional and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
References
- 1.Chang C, Case S. Management of facial nerve injury due to temporal bone trauma. Am J Otol. 1999;20:96–114. doi: 10.1016/S0196-0709(99)90018-2. [DOI] [PubMed] [Google Scholar]
- 2.Yetiser S. Total facial nerve decompression for severe traumatic facial nerve paralysis: a review of 10 cases. Int J Otolaryngol. 2012 doi: 10.1155/2012/607359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Patel A, Groppo E. Management of temporal bone trauma. Craniomaxillofac Trauma Reconstr. 2010;3(2):105–113. doi: 10.1055/s-0030-1254383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ulrich K. Verletzungen des Gehorlorgans bel Schadelbasisfrakturen (Ein Histologisch und Klinissche Studie) Acta Otolaryngol Suppl. 1926;6:1–150. [Google Scholar]
- 5.Gordon E, Thomas S, Ducic Y, Arnaoutakis D. Facial nerve trauma: evaluation and considerations in management. Craniomaxillofac Trauma Reconstr. 2015;8(1):1–13. doi: 10.1055/s-0034-1372522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ulug T, Ulubil SA. Management of facial paralysis in temporal bone fractures: a prospective study analyzing 11 operated fractures. Am J Otolaryngol. 2005;26(4):230–238. doi: 10.1016/j.amjoto.2005.01.004. [DOI] [PubMed] [Google Scholar]
- 7.Coker NJ, Kendall KA, Jenkins HA, et al. Traumatic intratemporal facial nerve injury: management rationale for preservation of function. Otolaryngol Head Neck Surg. 1987;97(3):262–269. doi: 10.1177/019459988709700303. [DOI] [PubMed] [Google Scholar]
- 8.Kim J, Moon IS, Shim DB, Lee WS. The effect of surgical timing on functional outcomes of traumatic facial nerve paralysis. J Trauma. 2010;68(4):924–929. doi: 10.1097/TA.0b013e3181a8b2d9. [DOI] [PubMed] [Google Scholar]
- 9.Dahiya R, Keller J, Litofsky N, et al. Temporal bone fractures: otic capsule sparing versus otic capsule violating clinical and radiographic considerations. J Trauma. 1999;47(6):1079–1083. doi: 10.1097/00005373-199912000-00014. [DOI] [PubMed] [Google Scholar]
- 10.Darrouzet V. Management of facial paralysis resulting from temporal bone fractures: our experience in 115 cases. Otolaryngol Head Neck Surg. 2001;125(1):77–84. doi: 10.1067/mhn.2001.116182. [DOI] [PubMed] [Google Scholar]
- 11.Fisch U. Facial paralysis in fractures of the petrous bone. Laryngoscope. 1974;84(12):2141–2154. doi: 10.1288/00005537-197412000-00005. [DOI] [PubMed] [Google Scholar]
- 12.Hai-jin Y, Pi-Nan L, Shi-ming Y. Surgical management of traumatic facial paralysis: a case review study. J Otol. 2001;6(2):38–42. doi: 10.1016/S1672-2930(11)50020-0. [DOI] [Google Scholar]
- 13.Singh H, Sharma JK, Pippal JK. Evaluation and treatment options of post traumatic facial nerve palsy. J Otol Rhinol. 2016;5:3. doi: 10.4172/2324-8785.1000279. [DOI] [Google Scholar]
- 14.Xie Shaobing, Xuewen Wu, Zhang Yanni, Zhenhang Xu, et al. The timing of surgical treatment of traumatic facial paralysis: a systematic review. J Acta Oto Laryngol. 2016;136(12):1197–1200. doi: 10.1080/00016489.2016.1201862. [DOI] [PubMed] [Google Scholar]
- 15.Sanuş GZ, Tanriöver N, Tanriverdi T, et al. Late decompression in patients with acute facial nerve paralysis after temporal bone fracture. Turk Neurosurg. 2007;17(1):7–12. [PubMed] [Google Scholar]
- 16.Quaranta A, Campobasso G, Piazza F, et al. Facial nerve paralysis in temporal bone fractures: outcomes after late decompression surgery. Acta Otolaryngol. 2001;121(5):652–655. doi: 10.1080/000164801316878999. [DOI] [PubMed] [Google Scholar]
- 17.Liu Y, Liu S, Li J, Chen X, Sun J, Li Y. Management of facial palsy after temporal bone fracture via the transmastoid approach. Acta Otolaryngol. 2015;135(3):307–311. doi: 10.3109/00016489.2014.981287. [DOI] [PubMed] [Google Scholar]