Abstract
Many surgical advancement paved to surgical success in endonasal endoscopic dacryocystorhinostomy. Mitomycin C is a systemic chemotherapeutic agent derived from Streptomyces caespitosus that inhibits the synthesis of DNA, cellular RNA, and protein by inhibiting the synthesis of collagen by fibroblasts. The objective of the study was to evaluate the advantage of mitomycin C in primary endoscopic endonasal dacryocystorhinostomy without stenting. Randomised case control design. Tertiary academic centre in central India. 112 patients who presented with epiphora and diagnosed as chronic dacryocystitis after syringing by ophthalmologist, were selected and randomised into two groups with or without mitomycin C intraoperative application. 112 eyes underwent endoscopic-dacryocystorhinostomy. Additional surgeries were done according to necessity. Mitomycin C was applied in concentration of 0.4 mg/dl for 5 min. Patients were followed up on OPD-basis at the end of 1st week, 1st month, 3rd month and over phone call at end of 1 year. Symptomatic improvement assessed by verbal enquiry and clinically by syringing by ophthalmologist. 8 patients underwent septal surgery in case group and 4 in control group along with 1 concha bullosa correction in the case group (p < 0.05). Nil intraoperative complications (p < 0.05) and nil postoperative complication noted (p < 0.05). Functional and anatomical patency found to be 100% at the end of 1st week in both groups, 96.5% at 3rd month in case group and 96.4% and 92.9% at 1 month and 3 month respectively in control group. Nasal endoscopy of all surgical failures showed restenosis in both case group and control group except 1 patient with granulation in control group. Eventhough intraoperative mitomycin C application is effective in increasing the success rate of endonasal DCR surgery in standard nasolacrimal duct obstruction, and with no significant complications from its use, the study did not show added benefit in the primary endoscopic endoscopic dacryocystorhinostomy without stenting.
Keywords: Chronic dacryocystitis, Dacryocystorhinostomy, Mitomycin C
Introduction
Chronic dacryocystitis is characterised predominantly by, epiphora which could pose minor inconvenience for some or may be a source of social embarrassment as it can alter refraction and patient has to wipe the tear of perpetually. It can also present with mucocoele, pyocoele, or recurrent acute dacryocystitis. In majority of cases, cause of obstruction is unknown. Such idiopathic obstruction is common with increasing age and has female preponderance. Other less common cases include surgical trauma, following middle meatal antrostomy, midface fractures, malignancy and granulomatous diseases.
The first report of dacryocystorhinostomy was by Caldwell in 1893, by removing a portion of inferior turbinate and following lacrimal duct to sac [1]. Later Toti in 1904, is credited with first description of an external approach. With the development of modern instruments, a century later resurgence of interest in endonasal approach had arisen. The early results being described by Steadman and McDonagh and Meiring [2]. The main indication of dacryocystorhinostomy is symptomatic distal obstruction of nasolacrimal duct, that is not relieved by simple probing and syringing.
Failure of surgery was due to closure of osteotomy stoma site by soft tissue and obstruction at common canaliculus. Antiproliferative agents like Mitomycin C are likely to reduce soft tissue proliferation and the fibrosis, which has been used in trabeulectomy in glaucoma. Thus may result in reduced closure of surgically created stoma in dacryocystorhinostomy. Only a few studies regarding the efficacy of this drug have been undertaken and further studies are needed to determine and confirm the efficacy of this drug in preventing post-operative closure of the stomal site. Therefore, the present study was done to determine, whether Mitomycin-C can influence the success rate of En DCR.
Materials and Methods
Source of Data
After approval by ethical committee, the prospective randomised case control study was conducted in the Department of Otorhinolaryngology and Head and Neck, Gandhi Medical College and Hamidia Hospital, Bhopal, India, (January 2016 to January 2018). 112 patient’s variables were analyzed including patient demographics, preoperative syringing, complete ophthalmologic, nasal cavity, paranasal sinus examination. Patients who presented with epiphora and chronic dacryocystitis confirmed by finding of postsaccal obstruction on syringing by expert ophthalmologist, were included in the study. Regurgitation was present from the opposite punctum on syringing, in which postsaccal obstruction was diagnosed.
Those were excluded from the study who had lid laxity, canalicular obstruction, malignancy, previous maxillary surgeries and those not giving consent for endonasal DCR. Paediatric age group was also excluded.
Patients were randomly divided into cases, in whom Mitomycin C was used and control in which the drug was not used.
A written consent from the patients was taken for endoscopic DCR.
Surgical Technique
Patients were hospitalized 1 day prior to surgery and antibiotic nonsteroidal eye drops and nasal decongestents (xylometazoline) were started. The nasal mucosa was decongested with cotton pledgets placed in nasal cavity soaked in xylocaine 4% with adrenaline (1:30,000) for 10 min in the preoperative preparation room. Surgery was done under general anaesthesia in a slightly reversed Trendelenburg position (30°). All patients underwent standardized procedure with an endonasal approach (using 0° endoscope of 4 mm diameter, 18 cm length) to lacrimal sac. Maxillary line was identified. The lateral nasal wall, just anterior to axilla of the middle turbinate was infiltrated with 2% Xylocaine with 1:100,000 adrenaline. After giving incision, C shaped mucosal flap was elevated gently using a suction elevator. Surgical removal of lacrimal bone and part of frontal process of maxilla, was carried out with straight and curved Smith- Kerrison’s punch forceps. The lacrimal bone removed until complete and adequate exposure of lacrimal sac. Posterior vertical incision of the medial sac wall was performed with keratome, thus creating an ample dacryo-cysto-rhino-stoma (Fig. 1). Patency was confirmed by free flow on syringing of both upper and lower punctum. In the study group (56 eyes), Mitomycin C (0.4 mg/ml) soaked gelfoam was kept in the stoma site for 5 min (Fig. 2) and was removed and no infiltration of the drug given in the peristomal region. In control group (56 eyes), standard endonasal dacryocystorhinostomy done without application of Mytomycin C. Additional surgeries like septal surgery, concha bullosa resection, removal of prominent aggernasi, if present was done to get good surgical operative field and vision. Uncinectomy was not carried out in any. Silicon intubation tubes were not used in the procedure. The mucosal flap was repositioned. Light nasal packing was done.
Fig. 1.
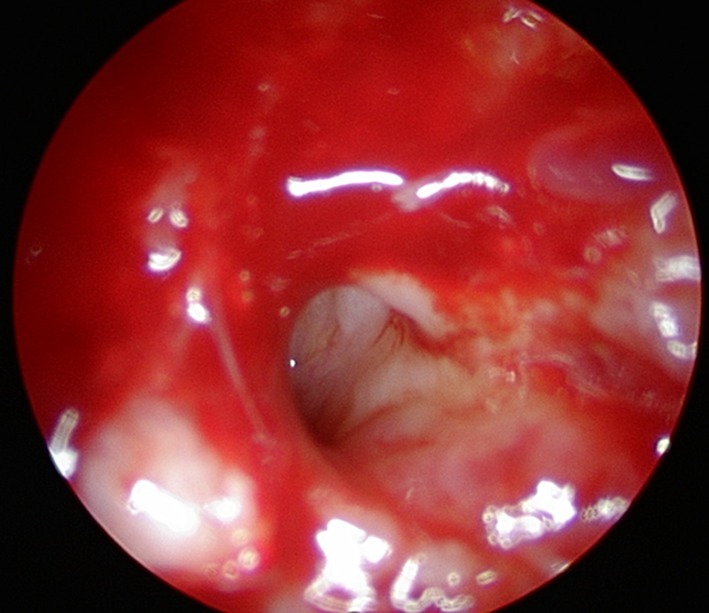
Common canaliculus
Fig. 2.
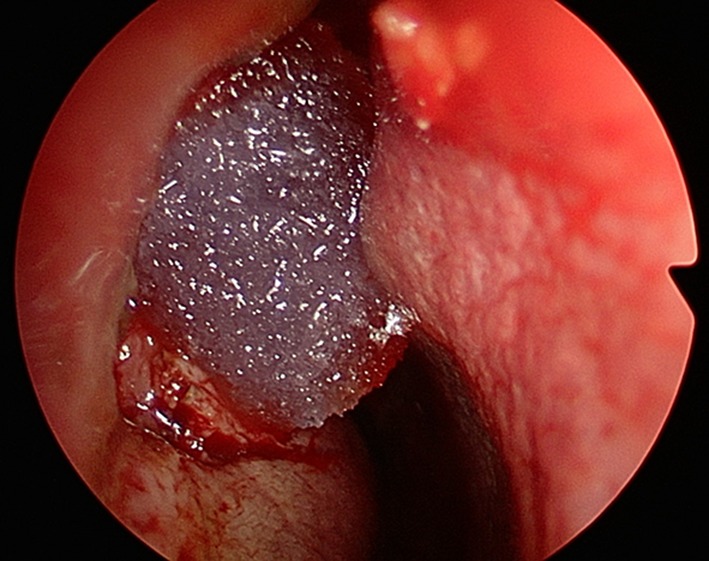
Application of mitomycin soaked gelfoam
Post Operative Care
Postoperatively, patients were stayed in hospital for 48 h, kept in semirecumbant position along with systemic decongestant, analgesics and intravenous antibiotic and topical steroidal antibiotic eye drops every 6 hourly. After 48 h, anterior nasal pack was taken and was discharged on oral antibiotic, and antibiotic eye drops. Alkaline nasal douching also adviced three to four times per day in the post operative week to remove the crust formation and debris and to fasten the healing. Periodic OPD based follow up was done at the end of 1st week, 1st month, 3st month and follow up over the phone at end of 1 year. Symptomatic improvement assessed with verbal enquiry and patency confirmed by nasolacrimal syringing by ophthalmologist. In postoperative visits, endoscopy was done in cases of persistence or recurrence of symptoms only. Weekly syringing by ophthalmolgists and nasal douching were adviced for initial 2 months of post operative period.
The main outcome measures were resolution of epiphora and patency of ostium confirmed by syringing.
The result were analysed statistically by entering the parameters in SPSS. Statistical heterogeneity was assessed using Chi square test, p value < 0.05 level was considered as statistically significant.
Results
Among the 112 patients, 56 patients each were in case and control group. Of these 70% were females and 30% were males. Mean age of presentation was 39 ± 15.27 years. The male–female ratio was 1:2.34.
58% of study subjects belonged to rural area and 70% were from lower middle class.
In this single blinded study, 100% patients had epiphora as major symptom. Mucocoele (20% patients) and pyocoele (10% patients) were also presented. No history of malignancy, epistaxis, features of chronic granulomatous disease was present. Only two patients had associated nasal obstruction. 46% patients had symptoms for ≤ 6 months duration, and symptomatic duration ranged from 3 months to 10 years. The mean duration of symptoms was 32 months. Both eyes were almost equally affected. Total 112 endonasal endoscopic dacryocystorhinostomy were done. 8 septoplasty, 4 submucosal resection and 1 concha bullectomy were done to access into the site. In the present study, no intraoperative complications (p ≤ 0.05) encountered and there was no immediate postoperative complication (p ≤ 0.05). No adverse event related to MMC was evident.
Outcome measured in terms of subjective (functional) and objective (anatomical) assessments for follow up duration of 1 year.
In the study group epiphora recurred in 2 patients at the end of 3rd month and in the control group, 2 patients at 1 month and 2 patients at 3 month. Functional patency (subsidence of epiphora) in the study group was 100% patients at the end of 1st week and 1st month but turned to 96.4% of patients at the end of 3rd month and that of control group was 100%, 96.4% and 92.9% at end of 1 week, 1 month and 3 month respectively. Patients were followed up over phone at 1 year and none of new symptomatic patients came through.
Anatomical patency was confirmed by syringing and recurrence confirmed as regurgitation seen from the opposite punctum in patients with symptoms. None of postoperative asymptomatic patients turned out to have blockade of stoma on syringing. Anatomical patency result was found to be same as functional patency.
Diagnostic nasal endoscopy showed restenosis in 2 patients of case group and 3 patients of control group along with granulation at stoma site in 1 patient in the control group. Revision surgery was done in 5 patients and was successful.
Chi square test was used to compare the follow up results for stomal patency. p value was greater than 0.05 (p > 0.05), which is statistically insignificant, suggesting that there was no difference observed in various complications at the follow up’s between the two groups, as shown in Table 1. The result is suggesting that the difference in the results of case and control was not statistically significant. Hence these results indicate that there is no significant benefit in using Mitomycin-C as an adjunct to prevent stomal closure in primary En DCR.
Table 1.
Analysis of success rate of dacryocystorhinostomy with and without Mitomycin C
| Findings | Group A (Case) | Group B (control) | X2 | p value |
|---|---|---|---|---|
| Patent | 54 (96.4%) | 52 (92.9%) | 0.704 | 0.401 |
| Blockade | ||||
| Restenosis | 02 (03.6%) | 03 (05.3%) | ||
| Granulation | 0 | 01 (01.8%) |
As in Table 1 values, the result after applying Chi square test showed X2 = 0.704, p value of 0.401 which is greater than 0.05 (p > 0.05) was obtained. Therefore, the difference in the results of Group A (case) and Group B (control) was not statistically significant. Hence these results indicate that there is no significant benefit in using Mitomycin-C as an adjunct to prevent stomal closure in primary En-DCR.
Discussion
Endoscopic endonasal dacryocystorhinostomy is considered as a highly successful procedure for chronic dacryocystitis due to nasolacrimal duct obstruction, with the advent of telescopes and newer instruments for functional endoscopic sinus surgery, from early 1990s [3].
It also reduced blood loss, surgical trauma, operative and hospitalisation time, post operative discomfort and preserved medial canthal anatomy along with greater visualisation through straight and angled scopes. It gave greater cosmetic accessibility [4] and the access to correct the associated intranasal pathology and also made it possible to do bilateral DCR in single setting.
Appropriate selection of patients is a key point in determining good outcome after evaluating the saccal, presaccal and post saccal stenosis of lacrimal pathway. In recent systemic review of outcomes after DCR in adults success rate of EN-DCR was found to range from 84 to 94% [5].
Mitomycin C is an antineoplastic agent that inhibits the synthesis of DNA, cellular RNA, and protein by inhibiting the synthesis of collagen by fibroblasts [6]. It has been widely used in ophthalmic practice both intraoperatively and postoperatively for the prevention of pterygium recurrence, enhancing success rate of glaucoma filtration surgery. A meta-analysis found that MMC is safe adjuvant which could reduce closure rate of osteotomy site after primary external dacryocystorhinostomy. Recently, controlled trials have investigated adjunctive MMC for primary EN-DCR to augment surgical success rate, but the results are not completely consistent.
The present study conducted in tertiary care centre among 112 patients (112 eyes) presenting with symptoms and signs suggestive of nasolacrimal duct obstruction. They were assigned randomly into two groups Group A (case) patients with endonasal DCR with Mitomycin C application and Group B (control) with conventional endonasal DCR. As by Apuhan Mitomycin C, in appropriate doses is considered to increase the success rate of EN-DCR [7]. According to Zilelioğlu G also, adjunctive use (0.5 mg/ml for 2.5 min) of a wound healing inhibitor does not show much difference between two groups (77.8% in case/77.3% in control) in the success rate of endoscopic endonasal DCR [8]. Yildirim et al. [9] in a prospective randomized controlled study to study the adjunctive use of MMC in external DCRs noted that while the success rates of the MMC group were higher than those of the control group, the differences did not reach statistical significance. Prasannaraj et al. [10] in their results of endoscopic DCR, where 38 patients were randomized into either an MMC group (0.2 mg/dL) or a control group, reported a success rate of 82.3% with MMC 85.7% without MMC. In our study, the success rate at 12 months postoperatively was 96.5%. As in the literature the present study also showed increase in success rate, but was not statistically significant enough to declare the beneficiality of adjuvant use of MMC in primary EN-DCR. All failures were due to cicatricial closure of the ostium. Success rate of control group was 90%, which was in the range of other studies, reported by, Cokkeser et al. [11], McMaster’s et al. [12], Pittore et al. [13] as shown in Table 2.
Table 2.
Analysis of results of studies without use of Mitomycin C
| Authors | Success without stent (%) |
|---|---|
| Cokkeser et al. | 88.2 |
| McMaster’s et al. | 89 |
| Pittore et al. | 89 |
Failures in En DCR are due to re-closure of the stoma. There is natural tendency to contract stoma during healing process. Mudhol shown that there is small reduction in size of lacrimal ostium in the first 4 weeks, corresponding to initial stages of healing [14]. The same finding correlated with that of Mann [15]. Furthermore, Boush and associates showed that most surgical failures occurred within the first 4 months after surgery [16] and Kong reported average onset of closure after primary DCR of 12.7 weeks [17] and Woog reported in the study as 7.5 weeks [18]. From this it is well sure that duration for recurrence ranges from 4 weeks 4 months. Hence duration of follow up period in our study was 1 year, which was considerably enough than minimum period of 6 months. In the present study also there was no reporting of recurrence after period of 3 months.
There was no MMC related adverse events noted in the study, as are the abnormal nasal bleeding, mucosal necrosis, infection, corneal ulcer, corneal perforation, sclera calcification, secondary cataract, endophthalmitis, hyptony and maculopathy [19, 20]. But, on the otherhand, though the complication of surgery like granulation was less, the result was not statistically significant.
The variation in the technique of drug delivery and the concentration of drug along with duration of its application was not assessed in the study, as drug was used for 5 min with concentration of 0.4 mg/ml applied in the gelfoam. Postoperative analysis of endoscopic stomal size for the successful case and control groups in the follow up period, was also not assessed in the study.
Outcome mainly depends on the quality of surgical technique with sharp punch removal of bone with minimal laceration of mucosal flap resulting large stoma with adequate fistulous communication along with the fine tuned use of instruments. Postoperative follow up is also essential part of adequate wound healing with saline nasal douching and repeated syringing.
Conclusion
Endonasal endoscopic dacryocystorhinostomy is safe, and highly successful procedure for chronic dacryocystitis due to nasolacrimal duct obstruction. The success rate of present study was 96.5%, showing higher success rate in MMC group, but no benefit is attributed in primary endonasal dacryocysorhinostomy as the comparative result with non-MMC group was not statistically significant. No mitomycin C related complication also reported in the study. The complication is less with mitomycin C, as no granulation or synechiae reported. The recurrence of symptom noted at 3 months postoperatvely. Appropriate patient selection, meticulous study of sinonasal anatomy and good experience in endoscopic sinus surgery is necessary.
Conflict of interest
The authors declare that they have no competing interests
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Contributor Information
Yashveer Jayantha Kedilaya, Email: yash045@yahoo.com.
Aneena Chacko, Email: aneenachacko@ymail.com.
V. K. Poorey, Email: drvkpoorey@gmail.com
References
- 1.Caldwell GW. Two new operations for obstruction of the nasal duct with preservation of the canaliculi. Am J Ophthalmol. 1893;10:189–191. [Google Scholar]
- 2.McDonogh M, Meiring JH. Endoscopic transnasal dacryocystorhinostomy. J Laryngol Otol. 1989;103:585–587. doi: 10.1017/S0022215100109405. [DOI] [PubMed] [Google Scholar]
- 3.Kennedy DW. Functional endoscopic sinus surgery technique. Arch Otolaryngol Head Neck Surg. 1985;111(10):643–649. doi: 10.1001/archotol.1985.00800120037003. [DOI] [PubMed] [Google Scholar]
- 4.Korkut AY, Teker AM, Yazici MZ, Kahya V, Gedikli O, et al. Surgical outcomes of primary and revision endoscopic dacryocystorhinostomy. J Craniofac Surg. 2010;21:1706–1708. doi: 10.1097/SCS.0b013e3181f3c6c1. [DOI] [PubMed] [Google Scholar]
- 5.Leong SC, MacEwen CJ, White PS. A systematic review of outcomes after dacryocystorhinostomy in adults. Am J Rhinol Allergy. 2010;24:81–90. doi: 10.2500/ajra.2010.24.3393. [DOI] [PubMed] [Google Scholar]
- 6.Cheng S, Feng Y, Xu L, Li Y, Huang J. Efficacy of mitomycin C in endoscopic dacryocystorhinostomy: a systematic review and meta-analysis. PLoS One. 2013;8(5):e62737. doi: 10.1371/journal.pone.0062737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Apuhan T, Yıldırım YS, Eroglu F, Sipahier A. Effect of mitomycin C on endoscopic dacryocystorhinostomy. J Craniofac Surg. 2011;22:2057–2059. doi: 10.1097/SCS.0b013e3182319863. [DOI] [PubMed] [Google Scholar]
- 8.Zílelíoğlu G, Tekeli O, Uğurba SH, Akiner M, Aktürk T, et al. Results of endoscopic endonasal non-laser dacryocystorhinostomy. Doc Ophthalmol. 2002;105:57–62. doi: 10.1023/A:1015702902769. [DOI] [PubMed] [Google Scholar]
- 9.Yildirim C, Yaylali V, Esme A, Ozden S. Long-term results of adjunctive use of mitomycin C in external dacryocystorhinostomy. Int Ophthalmol. 2007;27:31–35. doi: 10.1007/s10792-007-9057-6. [DOI] [PubMed] [Google Scholar]
- 10.Prasannaraj T, Kumar BY, Narasimhan I, Shivaprakash KV. Significance of adjunctive mitomycin C in endoscopic dacryocystorhinostomy. Am J Otolaryngol. 2012;33(47–50):18. doi: 10.1016/j.amjoto.2011.01.001. [DOI] [PubMed] [Google Scholar]
- 11.Cokkeser Y, Evereklioglu C, Er H. Comparative external versus endoscopic dacryocystorhinostomy: results in 115 patients (130 eyes) Otolaryngol Head Neck Surg. 2000;123:488–491. doi: 10.1067/mhn.2000.105470. [DOI] [PubMed] [Google Scholar]
- 12.McMasters M, Messerli J, Wolfensberger M. Endonasal dacryocystorhinostomy: technique and results. Schweiz Med Wochenschr Suppl. 2000;116:74S–76S. [PubMed] [Google Scholar]
- 13.Pittore B, Tan N, et al. Endoscopic transnasal dacryocystorhinostomy without stenting: results in 64 consecutive procedures. Acta Otorhinolaryngol Ital. 2010;30:294–298. [PMC free article] [PubMed] [Google Scholar]
- 14.Mudhol RR, Zingade ND, Mudhol RS, Das A. Endoscopic ostium assessment following endonasal dacryocystorhinostomy with mitomycin C application. Al Ameen J Med Sci. 2012;5:320–324. [Google Scholar]
- 15.Mann BS, Wormald PJ. Endoscopic assessment of the dacryocystorhinostomy ostium after endoscopic surgery. Laryngoscope. 2006;116:1172–117440. doi: 10.1097/01.mlg.0000218099.33523.19. [DOI] [PubMed] [Google Scholar]
- 16.Boush GA, Lemke BN, Dortzbach RK. Results of endonasal laser-assisted dacryocystorhinostomy. Ophthalmology. 1994;101:955–959. doi: 10.1016/S0161-6420(94)31231-0. [DOI] [PubMed] [Google Scholar]
- 17.Kong YT, Kim TI, Kong BW. A report of 131 cases of endoscopic laser lacrimal surgery. Ophthalmology. 1994;101:1793–1800. doi: 10.1016/S0161-6420(94)31100-6. [DOI] [PubMed] [Google Scholar]
- 18.Woog JJ, Metson R, Puliafito CA. Holmium: YAG endonasal laser dacryocystorhinostomy. Am J Ophthalmol. 1993;116:1–10. doi: 10.1016/S0002-9394(14)71736-2. [DOI] [PubMed] [Google Scholar]
- 19.Rubinfield RS, Pfister RR, Stein RM, Foster CS, Martin NF, et al. Serious complications of topical mitomycin C after pterygium surgery. Ophthalmology. 1992;99:1647–1654. doi: 10.1016/S0161-6420(92)31749-X. [DOI] [PubMed] [Google Scholar]
- 20.Zacharria PT, Depperrman SR, Schuman JS. Ocular hypotony after trabeculectomy with mitomycin C. Am J Ophthalmol. 1993;116:314–336. doi: 10.1016/S0002-9394(14)71349-2. [DOI] [PubMed] [Google Scholar]


