Abstract
Background
High blood pressure (BP) and diabetes have been suggested to be non-communicable diseases (NCDs), and they are components in the definition of metabolic syndrome. Further, several studies have reported that the risk of developing NCDs can be reduced by increased physical activity. In addition, a daily target of 10,000 steps has been generally suggested to increase physical activity in sedentary lifestyles. Therefore, the purpose of this study was to determine the effect of an accumulation of 10,000 steps daily on BP and blood glucose in overweight participants.
Methods
Participants were recruited from males and females, aged 35–59 years, with sedentary lifestyles. A longitudinal quasi-experimental study was designed with 35 participants who had body mass indices ≥25 kg/m2. These volunteers were assigned to the 12-week pedometer-based walking program (an accumulation of at least 10,000 steps daily). Blood glucose and BP were measured before and after the intervention.
Results
Systolic blood pressure (SBP) was significantly lower in 30 individuals who accumulated 10,000 steps daily (−13.74 mmHg). In addition, the reduction of blood glucose levels (−14.89 mg/dl) in the intervention participants was statistically significant (p < 0.001).
Conclusion
The accumulation of at least 10,000 steps daily resulted in decreased SBP and blood glucose in overweight Thai subjects. It could also reduce the risk of cardiovascular disease (e.g., hypertension and diabetes).
Keywords: Blood pressure, Physical activity, Walking, Diabetes, Blood glucose
Overweight and obesity are modifiable risk factors for cardiovascular disease, and they lead to non-communicable diseases (NCDs) [1, 2]. Further, the clinical diagnosis criteria of metabolic syndrome have been defined as ≥3 of the following: central obesity, elevated blood pressure (BP), low high-density lipoprotein cholesterol or elevated triglyceride values, impaired fasting glucose and obesity [i.e., body mass index (BMI), waist circumference] [1]. In a survey in Thailand, the prevalence of being overweight and obese (BMI ≥25 kg m−2) among adults is up to 23.8% [3]. Moreover, lack of exercise or sedentary lifestyle is a modifiable behavior that leads to an increased risk of NCDs. It is well known that individual accumulation of 30 min of moderate-intensity physical activity at least 5 days per week or 150 min per week has been recommended in all population groups to increase physical activity [4].
An accumulation of at least 10,000 steps per day has been shown to meet the necessary minimum current physical activity level required [5–8]. In recent years, a pedometer or step-counting device has been commonly used to measure and promote physical activity. In addition, the benefits of pedometers are that they are easy to attach, are inexpensive, provide immediate feedback and are non-invasive [9]. Several studies have been conducted in Western countries and reported that walking can decreases BP and the risk of NCDs. However, in Thailand, no study has so far reported on the relationship between increasing physical activity by the accumulation of 10,000 steps per day and the risk of NCDs and also metabolic syndrome. Therefore, the aim of this study is to explore the effect of an accumulated 10,000 steps daily on the risk of NCDs in overweight participants.
Materials and methods
Participants and design
The quasi-experimental cohort study with 12 weeks of follow-up was designed to determine the effect of a pedometer on BP and blood glucose. Thirty-five overweight participants aged 35–59 years old were recruited from the community. The participants who had a known history of neurologic disorder (i.e., stroke) or cardiovascular disease (i.e., myocardial infraction, percutaneous coronary intervention or coronary artery bypass graft), chronic renal failure or disease, or history of psychiatric problems were excluded. The risks of NCDs in the study were defined as raised BP, overweight/obesity (i.e., increased waist circumference) and high blood glucose levels, which can lead to cardiovascular disease and an NCD. The ethics and protocol were approved by the Human Ethics Committee of Thammasat University 065/2555; the approval date was 2 November 2012.
Measures and apparatus
Prior to arrival, all participants were requested to abstain from consuming foods and beverages for 8–12 h prior to the assessment. Upon arrival on the initial study day, participants were given an information sheet. They then gave written informed consent to participate in the study. Blood samples were drawn by a registered nurse for analysis of glucose levels. Measurement of BP, weight and height were obtained. Participants were asked to sit quietly on a comfortable chair while resting BP and heart rate (HR) readings were obtained. BP was measured by an Omron® M6 Comfort BP monitor [HEM-7211 (HEM-7211; Omron Healthcare B.V., Kruisweg, Hoofddorp, The Netherlands], which is an automated, non-invasive, oscillometric BP device meeting the revised validation requirement of the 2010 European Society of Hypertension's international protocol [10]. The automated BP monitor was set to read and record BP and HR at 5 and 6 min, respectively, with a 1-min interval reading. An averaged BP was then calculated. The waist circumference was assessed at the level of the umbilicus while the participants were standing. Weight and height were measured for the calculation of BMI [body weight (kg)/height (cm)2]. The participants were required to wear the pedometer (Yamax Digi-Walker SW-200; Yamax Tokei Keiki Co., Ltd., Tokyo, Japan) while following their normal daily routine. After that, the researcher gave them a logbook and then asked the individuals to record their daily walking steps. Baseline daily walking steps were recorded for 5 working days.
After bassline measurement (i.e., 1 week later), the participants who had high blood glucose and high BP levels were informed of their risks. The benefits of increasing their physical activity and walking 10,000 steps daily were explained. After being given the information, the participants were invited to participate in a research project being conducted by the researcher in which they would walk at least 10,000 steps per day, and they were asked to record their steps in a diary for 12 weeks.
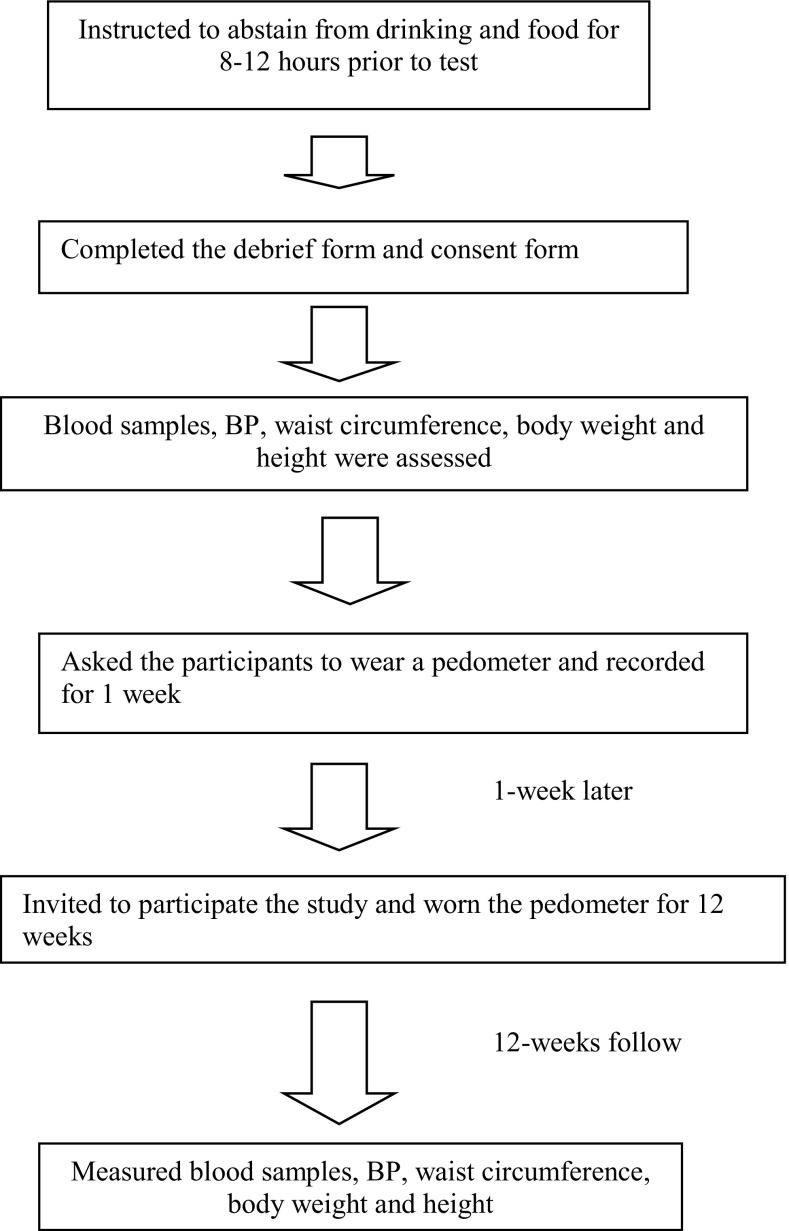
At the follow-up session, the participants who had completed the initial study were contacted by telephone and invited for a re-evaluation of the blood glucose and BP levels. Those who agreed to participate were also asked to refrain from drinking and eating at least 8–12 h before the follow-up session. Blood samples and BP were evaluated again. The pedometer and booklet were returned to the researcher. A summary of the experimental protocol is displayed below in Fig. 1.
Fig. 1.
Diagram showing the stages of the experimental protocol
Statistical analysis
Steps per day were averaged weekly. The change in the average number of steps per day over the 12-week intervention program was modeled for each participant. Data were presented as a percentage (%), mean and standard deviation (SD). Kolmogorov-Smirnov goodness of fit was tested to verify the normality of distribution. Paired t-test was used to determine whether the pedometer brought about significant changes in BP and blood glucose levels before and after walking intervention programs. Independent sample t-test was performed to indicate whether participants in the follow-up differed from those who did not complete the study after 12 weeks.
Results
The characteristics of the study participants are presented in Table 1. The mean age was 49.4 ± 6.9 years. The average BP was 129.6/84.4 mmHg, which is pre-hypertension [11]. Further, the average blood glucose level was 127.4 ± 23.1 mg/dl, which is a high fasting glucose level. The accumulated walking steps at the initial study were 4082.9 ± 2148.2 steps per day, which is defined as an inactive or sedentary lifestyle [7].
Table 1.
Demographic data of overweight participants (n = 35)
| Number (%) | Mean | SD | |
|---|---|---|---|
| Gender | |||
| Female | 22 (62.9) | ||
| Male | 13 (37.1) | ||
| History of taking hypertensive medicine | 8 (22.9) | ||
| Age (years) | 49.4 | 6. 9 | |
| BMI (kg*m−2) | 26.9 | 4.7 | |
| Waist circumference (cm) | 90.8 | 10.2 | |
| SBP (mmHg) | 129.6 | 12.5 | |
| DBP (mmHg) | 84.4 | 10.3 | |
| HR (bpm) | 79.9 | 8.9 | |
| Blood glucose (mg/dl) | 127.4 | 23.1 | |
| Steps walked per day | 4082.9 | 2148.2 | |
BMI body mass index, SBP systolic blood pressure, DBP diastolic blood pressure, HR heart rate
A total of 35 overweight participants (22 females and 13 males) participated in the initial study. However, only 30 participants (85.7%) completed the intervention program including 21 females and 9 males. A total of five (14.3%) participants did not follow the study; one was currently pregnant, one suffered from a herniated disc that led to difficulty walking, and three did not want to participate. Therefore, the results were based on 35 participants at entry and 30 participants at the 12-week intervention. However, there were no significant differences in age, BMI, waist circumference, BP and blood glucose level between those who completed the study and those who did not.
As shown in Table 2, systolic blood pressure (SBP), HR, waist circumference and BMI were significantly decreased after the pedometer-based intervention program. In addition, increasing physical activity by using a pedometer resulted in a decline in blood glucose levels after the 12-week intervention.
Table 2.
Comparisons between pre and post risk of metabolic syndrome after participating in the pedometer intervention program in overweight participants
| N | Pre | Post 12 weeks | Mean difference | 95% CI of the difference | P value | |
|---|---|---|---|---|---|---|
| Walking (steps/day) | 30 | 4540.5 ± 1959.0 | 10,500.2 ± 2070.5 | −5960.7 | −6774.9 to −5146.5 | <0.001 |
| Waist circumference (cm) | 30 | 92.6 ± 9.3 | 90.3 ± 8.2 | 2.3 | 0.8 to 3.8 | 0.004 |
| BMI (kg/m2)7 | 30 | 27.7 ± 4.3 | 27.3 ± 3.9 | 0.6 | 0.2 to 1.1 | 0.007 |
| SBP (mmHg) | 30 | 129.5 ± 7.8 | 115.8 ± 8.6 | 13.7 | 10.4 to 17.1 | <0.001 |
| DBP (mmHg) | 30 | 84.5 ± 10.0 | 81.7 ± 9.1 | 2.7 | −1.3 to 6.7 | 0.178 |
| HR (bpm) | 30 | 79.9 ± 8.9 | 74.5 ± 7.5 | 4.1 | 2.7 to 8.1 | <0.001 |
| Blood glucose (mg/dl) | 27 | 126.9 ± 20.3 | 112.0 ± 20.0 | 14.9 | 6.3 to 23.5 | 0.001 |
BMI body mass index, SBP systolic blood pressure, DBP diastolic blood pressure, HR heart rate, CI confidence interval
Discussion
The present study evaluated the effect of at least 10,000 accumulated steps daily measured by a pedometer on BP and blood glucose levels in overweight participants. Walking, one alternative for moderate physical activity, is the most common type of activity, and the American Heart Association (AHA) has recommended increasing physical activity. The benefits of walking, in particular for lowering BP, are well documented [12–14].
High BP has been suggested to be a non-communicable disease and is one of the components in the definition of metabolic syndrome [1, 2]. The beneficial decrease of BP was demonstrated in the current study, which concurred with other studies. The results confirm recent findings indicating that walking 10,000 steps per day is effective in increasing physical activity. In addition, Freak-Poli et al. [13] evaluated the effect of pedometer-based walking on the risks of diabetes and cardiovascular disease. They reported that decreased systolic and diastolic BP was observed after a 4-month intervention. The results of the present study showed that increasing physical activity by increasing daily steps can reduce blood glucose levels and the mortality linked to diabetes in accordance with previous studies [15, 16]. In addition, a prospective cohort study indicated that walking, which is a moderate-intensity exercise, significantly decreased the risk for incident hypertension and diabetes mellitus [17]. Of note, waist circumference is relatively associated with the visceral adipose tissue compartment and is also proposed as one of the clinical diagnosis criteria for metabolic syndrome [1, 2]. Kim et al. reported that walking is advantageous for improving metabolic syndrome as well as SBP, fasting plasma glucose, waist circumference and HDL-C. Further, the prevalence of metabolic syndrome was reduced from 39.9 to 20.9% over a 1-year intervention [18].
Hence, the results of the study are consistent with the other evidence that increasing the number of walking steps daily (an accumulated 10,000 steps daily) could reduce the risks of cardiovascular disease including metabolic syndrome (i.e., reduced waist circumference, BP and blood glucose).
Limitations of the study
A few limitations of this study can be noted, which might have affected the results. A quasi-experimental study was designed. Therefore, the control group was not examined. The sample size was relatively small, and most participants recruited were female (70%). Therefore, results cannot be used to draw conclusions for the whole population. HbA1c is recommended as an accurate method for blood glucose analysis, although the measurement of this parameter is not common in Thailand. Results for other health risk factors for metabolic syndrome (e.g., high-density lipoprotein cholesterol or triglycerides) were not reported in the study. A larger sample size with random control trials should be considered.
Conclusion
At least 10,000 accumulated steps per day resulted in a reduction of SBP and blood glucose levels in overweight participants. These results suggest that an increase in physical activity by accumulating at least 10,000 steps per day could possibly reduce the risk of cardiovascular disease and hypertension in overweight adults.
Acknowledgements
The authors acknowledge the help of Mr. Paitoon Dhari, the head of the community health service, and Mrs. Somsong Duren, a registered nurse, in organizing and overseeing participant recruitment in the community. The authors would also like to thank the participants in the community for their participation. This study was fully supported by Thammasat University.
Conflict of interest
There is no conflict of interest in the present study.
Human rights statement and informed consent
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (Thammasat University, Thailand) and with the Helsinki Declaration of 1964 and later versions. Informed consent or a substitute for it was obtained from all patients for being included in the study.
Contributor Information
Kornanong Yuenyongchaiwat, Phone: +66 (0)29869213, Email: ykornano@tu.ac.th, Email: plekornanong@gmail.com.
Duangnate Pipatsitipong, Phone: +66 (0)29869213.
Panthip Sangprasert, Phone: +66 (0)29869213.
References
- 1.Huang PL. A comprehensive definition for metabolic syndrome. Dis Model Mech. 2009;2:231–237. doi: 10.1242/dmm.001180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Park YW, Zhu S, Palaniappan L, Heshka S, Carnethon MR, Heymsfield SB. The metabolic syndrome: prevalence and associated risk factor findings in the US population from the Third National Health and Nutrition Examination Survey. Arch Intern Med. 2003;163:427–436. doi: 10.1001/archinte.163.4.427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jitnarin N, Kosulwat V, Rojroongwasinkul N, Boonpraderm A, Haddock C, Poston W. Prevalence of overweight and obesity in Thai population: results of the National Thai Food Consumption Survey. Eat Weight Disord. 2001;201(16):e242–e249. doi: 10.1007/BF03327467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Haskell WL, Lee IM, Pate RR, Powell KE, Blair SN, Franklin BA, Macera CA, Health GW, Thompson PD, Bauman A. Physical activity and public health: updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Med Sci Sports Exerc. 2007;39:1423–1434. doi: 10.1249/mss.0b013e3180616b27. [DOI] [PubMed] [Google Scholar]
- 5.Le Masurier GC, Sidman CL, Corbin CB. Accumulating 10,000 steps: does this meet current physical activity guidelines? Res Q Exerc Sport. 2003;74:389–394. doi: 10.1080/02701367.2003.10609109. [DOI] [PubMed] [Google Scholar]
- 6.Tudor-Locke C, Hatano Y, Pangraz RP, Kang M. Revisiting “How many steps are enough?”. Med Sci Sports Exerc. 2008;40:S537–S543. doi: 10.1249/MSS.0b013e31817c7133. [DOI] [PubMed] [Google Scholar]
- 7.Schneider PL, Bassett DR, Jr, Thompson DL, Pronk NP, Bielak KM. Effects of a 10,000 steps per day goal in overweight adults. Am J Health Promot. 2006;21:85–89. doi: 10.4278/0890-1171-21.2.85. [DOI] [PubMed] [Google Scholar]
- 8.Wilde BE, Sidman CL, Corbin CB. A 10,000 steps count as a physical activity target for sedentary women. Res Q Exerc Sport. 2001;72:411–414. doi: 10.1080/02701367.2001.10608977. [DOI] [PubMed] [Google Scholar]
- 9.Morgan CF, Jr, Pangrazi RP, Beighle A. Using pedometers to promote physical activity in physical education. JOPERD. 2003;74(7):33–38. [Google Scholar]
- 10.Topouchian J, Agnoletti D, Blacher J, Youssef A, Ibanez I, Khabouth J, Khawaja S, Beaino L, Asmar R. Validation of four automatic devices for self-measurement of blood pressure according to the international protocol of the European Society of Hypertension. Vasc Health Risk Manag. 2011;7:709–717. doi: 10.2147/VHRM.S27193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, et al. The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: the JNC 7 report. JAMA. 2003;289:2560–2572. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 12.Bravata DM, Smith-Spangler C, Sundaram V, Gienger AL, Lin N, et al. Using pedometers to increase physical activity and improve health: a systematic review. JAMA. 2007;298:2296–2304. doi: 10.1001/jama.298.19.2296. [DOI] [PubMed] [Google Scholar]
- 13.Freak-Poli R, Wolfe R, Backholer K, de Courten M, Peeters A. Impact of a pedometer-based workplace health program on cardiovascular and diabetes risk profile. Prev Med. 2011;53(3):162–171. doi: 10.1016/j.ypmed.2011.06.005. [DOI] [PubMed] [Google Scholar]
- 14.Semlitsch T, Jeitler K, Hemkens LG, Horvath K, Nagele E, Schuermann C, Pignitter N, Herrmann KH, Waffenschmidt S, Siebenhofer A. Increasing physical activity for the treatment of hypertension: a systematic review and meta-analysis. Sports Med. 2013;43:1009–1023. doi: 10.1007/s40279-013-0065-6. [DOI] [PubMed] [Google Scholar]
- 15.Araiza P, Hewes H, Gashetewa C, Vella CA, Burge MR. Efficacy of a pedometer-based physical activity program on parameters of diabetes control in type 2 diabetes mellitus. Metabolism. 2006;55:1382–1387. doi: 10.1016/j.metabol.2006.06.009. [DOI] [PubMed] [Google Scholar]
- 16.Smith TC, Wingard DL, Smith B, Kritz-Silverstein K, Barrett-Connor E. Walking decreased risk of cardiovascular disease mortality in older adults with diabetes. J Clin Epidemiol. 2007;60:309–317. doi: 10.1016/j.jclinepi.2006.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Williams PT, Thompson PD. Walking versus running for hypertension, cholesterol, and diabetes mellitus risk reduction. Arterioscler Thromb Vasc Biol. 2013;33:1085–1091. doi: 10.1161/ATVBAHA.112.300878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kim J, Tanabe K, Yoshizawa Y, Yokoyama N, Kuna S. Lifestyle-based physical activity intervention for one year improves metabolic syndrome in overweight male employees. Tohoku J Exp Med. 2013;229(1):11–17. doi: 10.1620/tjem.229.11. [DOI] [PubMed] [Google Scholar]