Abstract
Background/Objective: The heterogeneous clinical presentations of individuals with Autism Spectrum Disorders (ASD) pose a significant challenge for sample characterization. Therefore the main goal of DSM-5 must be to identify subgroups of ASD, including comorbidity disorders and severity. The main goal of this study is to explore the psychiatric comorbidities and the severity of symptoms that could be relevant for the phenotype characterization in ASD and also to compare these results according to the different classification criteria between the DSM-IV-TR and the DSM-5. Method: A comparative study of severity and psychiatric comorbidities was carried out between a sample of participants that only met criteria for Pervasive Developmental Disorder (PDD) according to the DSM-IV-TR and a sample of participants that also met ASD criteria according to DSM-5 classification. The recruitment of children was via educational (N = 123). The psychiatric symptoms, comorbid disorders and severity of symptoms were assessed through The Nisonger Child Behavior Rating Form, clinical interview and The Inventory of Autism Spectrum Disorder, respectively. The psychiatric comorbidities considered were: anxiety, eating behavioural problems, self-aggressiveness, hetero–aggressiveness, self-harm, obsessive compulsive disorder and attention deficit and hyperactivity disorder. Results: Statistically significant differences between both groups were found regarding obsessive compulsive disorder, eating behavioural problems and severity. Conclusions: The results support the hypothesis that patients who meet the DSM-5 criteria have more severe symptoms, not only regarding the core autistic symptoms but also in relation with psychiatric comorbidities.
Keywords: Autism spectrum disorder, DSM-IV-TR, DSM-5, Psychiatric-comorbidities, Descriptive study
Resumen
Antecedentes/Objetivo: Los Trastornos del Espectro Autista (TEA) incluyen un grupo heterogéneo en cuanto a su presentación clínica, que supone un desafío a nivel de caracterización diagnóstica. Por consiguiente, el objetivo principal de la clasificación DSM-5 debería de ser identificar subgrupos de TEA incluyendo severidad y comorbilidades psiquiátricas. El objetivo principal de este estudio es explorar las comorbilidades diagnósticas que pueden ser relevantes como descriptores de fenotipos autistas así como la severidad de los síntomas de autismo y comparar los resultados de las diferentes criterios de clasificación entre el DSM-IV-TR y el DSM-5. Método: Se realiza un estudio comparativo de severidad y comorbilidades psiquiátricas entre una muestra con diagnóstico de Trastorno Generalizado del Desarrollo, según criterios DSM-IV-TR, y una muestra que cumplía también criterios para TEA según la clasificación DSM-5. La muestra fue obtenida en centros educativos (N = 123). Las comorbilidades psiquiátricas y la severidad de los síntomas se evaluaron a través del The Nisonger Child Behavior Rating Form, entrevista clínica y el Inventario de Trastorno del Espectro Autista, respectivamente. Las comorbilidades estudiadas fueron ansiedad, alteraciones de la conducta alimentaria, auto-agresividad, hetero-agresividad, autolesiones, trastorno obsesivo-compulsivo y déficit de atención e hiperactividad. Resultados: Se encontraron diferencias estadísticamente significativas entre ambos grupos para trastorno obsesivo-compulsivo, alteraciones de la conducta alimentaria y severidad. Conclusiones: Se apoya la hipótesis de que los individuos que cumplen criterios diagnósticos según DSM-5 tienen mayor severidad sintomática, no sólo con respecto a los síntomas autistas centrales, sino también en relación con comorbilidades psiquiátricas.
Palabras clave: Trastorno del Espectro Autista, DSM-IV-TR, DSM-5, comorbilidades psiquiátricas, estudio descriptivo
Autism Spectrum Disorder (ASD) is characterized by deficits in social interaction and communication, as well as the presence as stereotyped behaviour and restrictive interests (American Psychiatric Association, APA, 2013). In the past, all psychiatric problems in children and adults with autism used to be attributed to autism itself. However, an increasing number of studies are arguing for accepting behaviours and symptoms that had been considered additional or associated features of ASD as potentially indicating the presence of comorbidities warranting additional diagnosis. Individuals diagnosed with ASD often present other psychiatric disorders, such as attention deficit and hyperactivity disorder (ADHD), anxiety disorders, mood alterations, etc. (Simonoff et al., 2008). It has been suggested that comorbidity will generally lead to more severe impairments as a result of the cumulative effects of having more than one disorder (Gadow, Guttmann-Steinmetz, Rieffe, & Devincent, 2012). Autism is generally a lifelong condition beginning in childhood and with pathological outcomes in adulthood. Outcomes are often described as difficulties or issues in finance, employment and socialization (Fountain, Winter, & Bearman, 2012). When other problematic symptoms are recognized as manifestation of comorbid psychiatric disorders, rather than just isolated symptoms, more specific treatment is possible. For this reason, comorbidity identification should include those symptoms which are sufficient for a comorbidity diagnosis and those isolated symptoms which can be relevant as descriptors of individual phenotypes such as eating behaviour problems, behaviour difficulties such as self-aggression or hetero-aggression.
One of the goals of the new classification (DSM-5) must be to identify subgroups of ASD, including comorbidity disorders, which may be important to understand the biological mechanisms, the clinical results and the reactions of the individuals with ASD to the treatment. It has been proposed a phenotypic characterization to improve the classification of ASD based not only on the specific items of ASD, but involving other specific characterizations such as cognitive and adaptive function, language skills, comorbidity, other medical conditions and other psychiatric features in order to standardize the clinical characteristics of individuals with ASD (Grzadzinski, Huerta, & Lord, 2013).
The publication of the fifth edition of the DSM has intensified a debate since the announcement of the changes in diagnostic criteria proposed by the APA. There is an increment of studies that open many questions about the diagnostic validity of the DSM-5 (Robles et al., 2014, Rodríguez-Testal et al., 2014, Timini, 2014). One of the important controversies is the diagnosis of ASD. The DSM-5 unifies the first and the second domain into a single category which include meeting all three distinctions of Social Communication and Interaction (SCI). The DSM-5 classification assembles the Pervasive Developmental Disorders (PDD) with different diagnostic subtypes into a single dimensional category of ASD, grouped by severity levels McPartland et al., 2012, Worley and Matson, 2012). There is an accord in different articles, stating that the new classification requires more severe symptomatology for the diagnosis (Gibbs et al., 2012, Matson et al., 2012b, Turygin et al., 2013).
The DSM-5, with difference to DSM-IV-TR, admits comorbidity with Attention Deficit and Hyperactivity Disorders (ADHD) in patients diagnosed with ASD. Many studies showed a high percentage of children diagnosed with ASD, who require health services, have ADHD comorbidity (Brereton et al., 2006, Holtmann et al., 2007, Sinzig et al., 2009, Yerys et al., 2011). Also, estimates of impairing anxiety range from 11–84% in school-aged children with ASD and as many as 40% meet criteria for an anxiety disorder (Kerns and Kendall, 2013, van Steensel et al., 2011, White et al., 2009). These reviews note a wide range of estimates attributable to differences in the sample source, sample size and assessment methods employed. These rates of anxiety disorders in youth with ASD are nearly two-fold higher than current estimates in typically developing children (Costello, 2005). Other reports indicate that Separation Anxiety and Generalized Anxiety (Gadow, DeVincent, Pomeroy, & Azizian, 2004) also occur at higher than expected rates in youth with ASD. Although the majority of previous studies involved clinic-based samples, community-based studies also indicate that children with ASD are at greater risk of anxiety (Simonoff et al., 2008).
Because of pure phenomenological reasons, the Obsessive Compulsive Disorders (OCD) and autism include the behavioural appearances (e.g., the compulsions in the OCD; rituals and routines in ASD) and cognitive appearances (the obsession in the OCD; equality insistence and worries in ASD). Although the form and content of these symptoms are different in both disorders (McDougle et al., 1995, Zandt et al., 2007; autism tends to involve less complex forms which are perhaps due to the existence of cognitive disorders and/or language. Despite of any overlap, the profile of repetitive behaviours in autism and OCD is also differentiable (Bejerot, 2007). For example, individuals with OCD usually do not have repetitive motor behaviours often associated with autism (e.g., hand flapping). In addition, individuals with OCD exhibit more cleaning, checking and counting behaviours, while individuals with autism engage in more hoarding, ordering, touching/tapping, and self-inflicted injuries (McDougle et al., 1995). The underlying causes of repetitive behaviour are unclear, although the modulation of arousal is usually suggested for ASD, and anxiety for OCD (Zandt et al., 2007).
In addition, children with early symptoms of neuropsychiatric disorders present a higher frequency of behavioural eating problems (Bandini et al., 2010) compared with children who do not have any disorders (Bryant-Waugh, Markham, Kreipe, & Walsh, 2010). Some published studies of children diagnosed with ASD, show an estimated 90% prevalence of eating problems (Kodak & Piazza, 2008). According to another study, the prevalence of eating problems was 0.6% in the control study population and, among children with eating problems, 40% were screened positive for ADHD and/or ASD (Rastam et al., 2013). Similarly, self-harm, self-injurious behaviours and hetero-aggression are very common in children diagnosed with Pervasive Developmental Disorder (PDD). In fact, the drugs used in ASD are aimed at treating behavioural and symptomatic problems, despite these symptoms are not part of the core symptoms of ASD (Soutollo, 2010). For this reason, the characterization of ASD should consider the assessment, not only of the comorbid disorders but also, the independent symptoms that might influence on the functionality or on the medical treatment of this population.
Therefore, the main goal of the present study was to analyse the clinical diagnostic comorbidities and the isolated psychiatric symptoms which can be relevant as descriptors of autistic's phenotype. A comparative study was carried out between a sample of patients with PDD diagnosis according to the DSM-IV-TR criteria and a sample of patients with clinical diagnosis of ASD according to DSM-5. It is hypothesized that the group of patients who met the DSM-5 criteria have more severe symptomatology, not only regarding the severity of core autistic symptoms but also in relation with different comorbid conditions.
Method
Participants
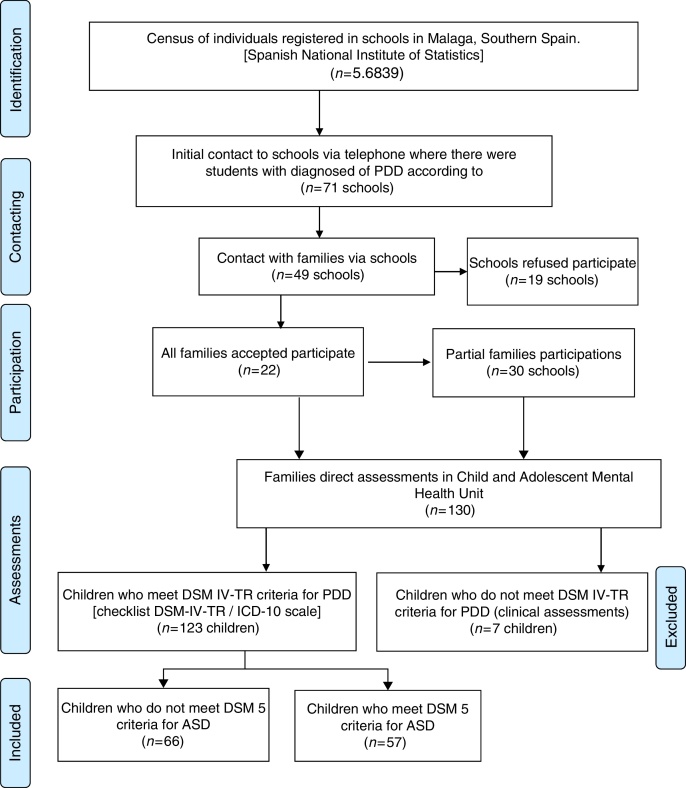
The recruitment of patients was via educational institutions in Málaga (Southern Spain). According to the census of individuals between 5 and 15 years registered in the province of Malaga and data from the Spanish National Institute of Statistics, the number of individuals enrolled in school was 56,839. The study was conducted accordingly with the Helsinski Declaration and was approved by the Local Community Ethics Committee. See flow diagram in Figure 2.
Figure 2.
Flow diagram.
Individual and parents’ interviews were made in the Unit of Child and Adolescents Mental Health in Carlos Haya Hospital in Malaga (Southern Spain), after signing the informed consent. Psychiatrists and psychologists with experience in children and adolescents carried out the assessments. Firstly, it was confirmed the community diagnosis for PDD by the clinical interview and according to the checklist DSM-IV-TR/ICD-10 scale. In term of demographic features; the mean age of participants was 10.62 and 82% of the sample were males.
Instruments and Procedure
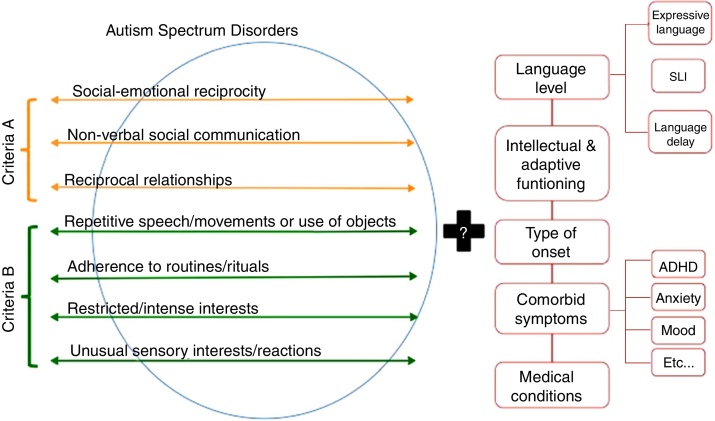
In order to confirm the clinical diagnosis of PDD, the DSM-IV-TR/ICD-10 Checklists were selected. Psychometric properties of the DSM-IV-TR/ICD-10 Checklist have been shown to be satisfactory as inter-rater reliability (r = .89), test-retest reliability (r = .97), and internal consistency (α = .95) were all robust (Gonzalez, 2008, Matson et al., 2008, Worley and Matson, 2012). The DSM-5 clinical diagnosis for ASD was assessed by child psychiatrists according to the DSM-5 manual, published in May, 2013. As we can see in the Figure 1, and consistently with the DSM-5, patients should have meet the three items of the criteria A, belonging to the domain of sociability and at least two items for the criteria B, restrictive interest and/or repetitive behaviour domain (RRB). The DSM-IV-TR/ICD-10 checklist scale was also used for this purpose. Finally, the total sample of patients diagnosed with PDD according to DSM-IV-TR was divided into two groups: (1) DSM-5 group; individuals who met also the DSM-5 criteria for ASD and (2) Non DSM-5 group; individuals who only met DSM-IV-TR criteria for PDD (not DSM-5 criteria).
Figure 1.
Proposed Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5) criteria and associated features to be considered when characterizing autism spectrum disorder (ASM) samples (Grzadzinski et al., 2013, with permission).
Variables of psychiatric comorbidities were obtained by the clinical assessment, and parents’ interviews, using the DSM-IV-TR criteria. The comorbid conditions studied were: (1) Attention Deficit and Hyperactivity Disorder and (2) Obsessive Compulsive Disorder. Moreover, the following independent psychiatric symptoms were assessed the same way: (1) Anxious or too fearful, (2) Physically harms or hurts self on purpose, (3) Physically attacks people, (4) Self-harm enough to leave tooth marks or break skin and (5) Eating behavioural problems.
The prevalence and frequency of some of these symptoms (1, 2, 3), were collected according to The Nisonger Child Behaviour Rating Form (NCBRF) (Problem behaviour subscale) (Aman, Burrow, & Wolford, 1995). The NCBRF (Norris & Lecavalier, 2011) is a factor-analytically derived scale with items rated from; did not occur or was no a problem (0) to behaviour occurred a lot or was a severe problem (3). There are two versions of the NCBRF: a parent and teacher version. The Conduct subscale of the NCBRF has been used as an outcome measure in placebo controlled trials of children with mild developmental disabilities (Brown et al., 2002, Snyder et al., 2002). It has also been used to characterize a large sample of children with ASD (Lecavalier, 2006). Concerning the item of (4) self-harm enough to leave tooth marks or break skin, the symptom was collected through the clinical history of the emergency visits or medical specialist consultation due to this cause (YES/NO).
Finally, the information about eating behaviour problems was collected during the clinical interview with the parents. It was codified according to the frequency of appearance, similar to the NCBRF scale; from did not occur or was no a problem (0) to behaviour occurred a lot or was a severe problem (3).
Severity of symptomatology was assessed by Autism Spectrum Disorder Inventory (IDEA) (Rivière, 2002). It is an inventory that includes 12 dimensions of development, divided into 4 areas (Social development, language and communication, anticipation and flexibility, symbolizing). Each dimension is scored from 0 (no qualitative disorder) to 8 (maximum involvement level) at intervals of 2 (0, 2, 4, 6, 8), being able to use odd scores when considering that the symptomatology is at an intermediate point between 2 consecutive items. The inventory was built with the aim of assess the severity of the core features of ASD.
Statistical analysis
Statistical analysis was performed using SPSS™ 21.0 with 1000 samples bootstrapping. After checking the linear model assumptions (Kolmogorov–Smirnov and Shapiro–Wilk tests) dimensional variables and frequencies were compared by parametric or non-parametric tests as appropriate (Chi Square Test and Student t-test). The bivariate association between the two groups (DSM-5 vs. Non DSM-5) and independent variables (comorbid disorders, other psychiatric symptoms and severity of symptoms) was initially explored using either two-way cross-tabulations or mean comparisons. We assumed a significance level of p ≤ .05.
Results
Clinical and sociodemographic distribution
The Table 1 shows the distribution of the number of patients who met DSM-5 criteria (DSM-5 group) and patients who did not (Non DSM-5) and the prevalence of the different Autism Spectrum Disorders (ASD) subgroups according to the DSM-IV TR [Autistic Disorder, Asperger's and pervasive developmental disorder-not otherwise specified (PDD-NOS)]. There were no significant differences between both groups in relation with the distribution of ASD subtypes (χ2 = 0.99; p = .61). Also, no significant differences in age was found between both groups (t-Student = -0.47; p = .64) (mean age: 10.62; SD: 2.99). The 82% of the sample were males and the ethnicity of the sample was 100% Caucasian.
Table 1.
Distribution of the number of patients who met DSM-5 criteria (DSM-5 group) and patients who did not (Non DSM-5) showing the prevalence of the different Autism Spectrum Disorders (ASD) subgroups and comorbidity with Attention Deficit Hyperactivity Disorder (ADHD), Obsessive Compulsive Disorder (OCD), Anxiety, Eating behavior problems, Auto-aggression, Hetero-aggression and Self-harm. Statistical differences between both groups are described.
| No DSM-5 Count (%) |
DSM-5 Count (%) |
Total Count (%) |
p | ||
|---|---|---|---|---|---|
| ASD subtypes | Autism | 17 (25.8%) | 17 (29.8%) | 34 (27.6%) | .61 |
| Asperger | 13 (19.7%) | 14 (24.6%) | 27 (22%) | ||
| PDD-NOS | 36 (54.5%) | 26 (45.6%) | 62 (50.4%) | ||
| Total | 66 (100%) | 57 (100%) | 123 (100%) | ||
| ADHD | No | 33 (50%) | 19 (33.3%) | 52 (42.3%) | .06 |
| Yes | 33 (50%) | 38 (66.7%) | 71 (57.7%) | ||
| Total | 66 (100%) | 57 (100%) | 123 (100%) | ||
| OCD | No | 51 (77.3%) | 22 (38.6%) | 73 (59.3%) | .0001 |
| Yes | 15 (22.7%) | 35 (61.4%) | 50 (40.7%) | ||
| Total | 66 (100%) | 57 (100%) | 123 (100%) | ||
| Anxiety | No occur | 6 (9.5%) | 4 (7%) | 10 (8.3%) | .09 |
| Occasional | 39 (61.9%) | 24 (42.1%) | 63 (52.5%) | ||
| Quite often | 4 (6.3%) | 5 (8.8%) | 9 (7.5%) | ||
| Severe problem | 14 (22.2%) | 24 (42.1%) | 38 (31.7%) | ||
| Eating behaviour problems | No occur | 33 (52.4%) | 16 (28.6%) | 49 (41.2%) | .05 |
| Occasional | 12 (19%) | 17 (30.4%) | 29 (24.4%) | ||
| Quite often | 4 (6.3%) | 3 (5.4%) | 7 (5.9%) | ||
| Severe problem | 14 (22.2%) | 20 (35.7%) | 34 (28.6%) | ||
| Auto-aggression | No occur | 42 (66.7%) | 31 (54.4%) | 73 (60.8%) | .57 |
| Occasional | 5 (7.9%) | 6 (10.5%) | 11 (9.2%) | ||
| Quite often | 4 (6.3%) | 6 (10.5%) | 10 (8.3%) | ||
| Severe problem | 12 (19%) | 14 (24.6%) | 26 (21.7%) | ||
| Hetero-aggression | No occur | 40 (64.5%) | 31 (56.4%) | 71 (60.7%) | .31 |
| Occasional | 12 (19.4%) | 12 (21.8%) | 24 (20.5%) | ||
| Quite often | 1 (1.6%) | 5 (9.1%) | 6 (5.1%) | ||
| Severe problem | 9 (14.5%) | 7 (12.7%) | 16 (13.7%) | ||
| Self-harm | No | 54 (81.8%) | 41 (71.9%) | 95 (77.2%) | .20 |
| Yes | 12 (18.2%) | 16 (28.1%) | 28 (22.8%) | ||
| Total | 66 (100%) | 57 (100%) | 123 (100%) |
Comorbidity with Attention Deficit Hyperactivity Disorder (ADHD)
The Table 1 illustrates the distribution of the number of participants who had clinical comorbidity with ADHD. Statistical analysis showed a non-significance value (χ2 = 3.48; p = .06), although it had a tendency toward the significance, as there was a higher percentage of participants with comorbidities in the DSM-5 group.
Comorbidity with Obsessive Compulsive Disorder (OCD)
As it can be seen in the Table 1, statistically significant differences between both groups were observed (χ2 = 18.96; p = .0001). In conclusion, patients fulfilling the DSM-5 criteria for ASD had higher prevalence of OCD diagnosis.
Anxiety or too fearful
Assessing the frequency of symptoms of anxiety or too fear between both groups, it was observed a tendency of having more severe problems in the group of participants who met DSM-5 criteria (63%), although there were no statistically significant differences between both groups (χ2 = 6.43; p = .09). See Table 1.
Eating behaviour problems
The Table 1 shows the distribution and the frequency of participants who presented eating behaviour problems. Statistically significant differences were found between both groups in relation with this symptom (χ2 = 7.57; p = .05). A higher prevalence of eating behaviour problems was observed in participants who met the criteria for ASD according to the DSM- 5.
Auto-aggression, hetero-aggression, self-harm
Comorbidities with auto-aggression, hetero-aggression and self-harm, are shown in Table 1, respectively. When both groups were compared, not significant differences were found (χ2 = 2.01; p = .57), (χ2 = 3.65; p = .31) and (χ2 = 1.70; p = .20), respectively.
Severity of Autism Spectrum Disorder
In order to assess the severity of the core autistic symptoms, The Autism Spectrum Inventory (IDEA) was used (Table 2). The null hypothesis of equal variances (Levene's test), was rejected and it was concluded that there was a significant difference between the variances of these measures. Consequently, the statistical analysis Kolmogorov-Smirnov was used and it showed that the group of patients who met DSM-5 criteria had more severe symptoms than the Non DSM-5 group with statistical significant differences (p = .0001).
Table 2.
Comparative study between No Autism Spectrum Disorders (ASD) DSM-5 and ASD DSM 5 group for severity of autistic symptoms. Mean (SD) [CI 95].
| Total Sample (n = 120) |
No-ASD DSM-5 (n = 63) |
ASD DSM-5 (n = 57) |
p | |
|---|---|---|---|---|
| IDEA | 43(8.82) [41.41 to 44.59] |
38,86 (8.69) [36.67 to 41.04] |
47,58 (6.41) [45.88 to 49.28] |
.0001 |
Discussion
Based on the data presented in this study, there is no question that comorbid symptomatology are quite prevalent in children with ASD. Variables such as specific behavioural symptoms, ADHD, OCD and severity of symptoms, likely have an influence on the autism individual's experience. The present study shows that the new classification DSM-5 requires more severe symptomatology for the diagnosis of ASD and also, the group of patients who met the DSM-5 criteria for ASD, are more likely to develop psychiatric comorbidities, specifically OCD and eating problems. Previous studies have supported the hypothesis of the DSM-5 could significantly improve the specificity at the expense of loss sensitivity in ASD (APA, 2013, Frazier et al., 2012, Grzadzinski et al., 2013, Wing et al., 2011). However, to the best of our knowledge, no previous studies have compared both classifications in term of severity and comorbidities in this population. Therefore, this study suggests that DSM-5 classification has been able to identify children with the most severe symptomology; however, it might fail to identify those with high functioning autism or less severe symptomatology. Consequently, in term of clinical implication, the DSM-5 criteria could have a high impact in the diagnosis of ASD. Authors of the present study also support the proposal of a phenotypic characterization, to improve the DSM-5 classification for ASD.
Methodology issues and further research
By addressing methodological issues that limit the findings of this study, future studies can contribute noticeably to our better understanding about the impact of the new classification in this population and answer more pointed scientific questions in relation with the phenotypic characterization. The present study did not employ any independent ‘gold standard’ confirmation for the ASD diagnoses [i.e., Autism Diagnostic Interview-Revised (ADI-R); (Lord, Rutter, & Le Couteur, 1994) or Autism Diagnostic Observation Schedule (ADOS) Lord et al., 2000)]; instead, including children based on community and clinical diagnosis with the DSM-IV-TR/ICD-10 Checklists confirmation.
This study was also limited by the fact that the diagnosis of ASD according to DSM-5 was completed using the items of DSM-IV-TR/ICD-10 Checklists. Although this method has been also used previously in other studies (Beighley et al., 2013, Matson et al., 2012a), new objective measures will need to be developed in order to accurately capture the patients who meet ASD criteria according to DSM-5 classification if valid and reliable measures cannot be identified at the current time.
In relation with the assessment for comorbid psychiatric symptoms such as eating disorders, anxiety, auto-and hetero-aggressiveness and self-arm, research on the applicability of traditional measures of childhood psychiatric symptoms, is sorely needed. Until we have consensus on ‘best practice’ measures, a healthy skepticism is called for with respect to the precision of the tools we currently have for measuring symptoms of comorbid problems in children with ASD. Assessment of global severity is another important consideration in treatment outcome research; yet, there is little guidance on its evidence-based assessment for children with ASD (White, Smith, & Schry, 2014).
One of the main strength of the methodology in this study was in relation with the representativeness of the sample of participants. The present study drew their ASD sample from a large population-derived, non-clinical patients. Clinical samples are often needed to accrue an adequate number of participants and for ensuring statistical power, but such samples can make it difficult to generalize findings. Clinic-based samples are likely not representative of all children with ASD in many important respects, such as degree of parental investment, level of behaviour disturbance, etc.
Main results
The findings of the current study support the overall a priori hypothesis. It was found that participants who met DSM-5 criteria had higher prevalence of clinical comorbidities and severity. According to the analysis of comorbidity with attention deficit disorder and hyperactivity (ADHD), the results showed that there were no statistical significant differences between both groups. However, there is a tendency toward higher prevalence in the DSM-5 group. The absence of a statistical significance could be due the sample size of patients with comorbid ADHD (n = 71). According to the last review, the prevalence has been remarkably heterogeneous, ranging from 4% to 94% (weighted mean prevalence = 48%; Frias, Palma, & Farriols, 2015). For example, Rao and Landa (2014) obtained a lower percentage of 29% as it focused on a non-clinical recruitment to avoid over diagnosis. Congruently, the current study was focused on non-clinical participants and we found a prevalence of 57.7%. These findings support the hypothesis that the comorbidity with ADHD may constitute a distinctive phenotype of ASD, and these children may be at a greater risk of involvement and socially adaptive problems. Moreover, ADHD is a condition that produces high academic dysfunctionality and therefore, exacerbates the academic and social needs of children who present comorbidity with ASD. This is important because participants with both conditions are given various treatments or strength requirements than those which have only ASD. These results are congruent with a growing number of studies that have shown that both pathologies can co-exist (Rao & Landa, 2014).
In the present study the results have showed that participants meeting DSM-5 criteria for ASD have more OCD comorbidity. The ASD diagnosis according to DSM-5 requires greater rigidity in the behavioural domain, unlike in the DSM-IV-TR. One of the most significant changes in the DSM-5 classification is the higher requirement in the area of repetitive and restrictive behaviour, requiring two of the four items compared to the DSM-IV-TR criteria where only one item was required for the diagnosis of PDD (Howlin et al., 2004, Mattila et al., 2011). For that reason, the similarities that exist between routines and rituals behaviour in ASD and compulsions in OCD; obsession in the OCD and equality insistence and worries in ASD, indicate that clinicians should make the assessment very carefully in order to make a correct differential diagnosis. If the assessment is only focused on the DSM-5 criteria, the comorbid diagnosis of OCD might be imprecise in individuals with ASD. Therefore, exploration into the overlapping and distinct phenotypic presentations of individuals with comorbid presentations (e.g., ASD with OCD) versus presentations of OCD or ASD singly may be of potential importance for understanding the biological markers of these disorders. Further genetic and neuro-imaging studies are needed in order to better understand this approach.
In addition, the present study found significant differences with eating behaviour problems between both groups, supporting the hypothesis of having more comorbidity in the DSM-5 group. Previous published studies of children diagnosed with ASD showed an estimated eating problem which reaches 90% of prevalence (Kodak & Piazza, 2008). However, in this study we obtained a lower percentage between 28.6% and 51% because we focused on a non-clinical recruitment to avoid over diagnosis.
Even without a clinical diagnosis, the results found that 31.7% of patients had severe problems with anxiety, congruent with the review of van Steensel, Bogels, and Perrin (2011), in which a percentage of 40% was found. Anxiety is an important factor in the daily lives of many children and adolescents with ASD diagnosis. Children and adolescents with ASD generally take longer to communicate their symptoms of anxiety due to their communication problems, many of which only manifest themselves internally (i.e., constant worry). These limitations make it difficult for people with ASD to be diagnosed because of the difficulties to express their own feelings or problems. Unfortunately, there is little clarity on how best to assess other psychiatric comorbid symptoms in this population and the direct impact on the ASD severity.
Finally, these findings do support the proposal of Grzadzinski et al. (2013), in order to highlight the importance of carrying out a phenotypic characterization to improve the DSM-5 classification, based not only on the specific core symptoms of ASD but also in their comorbidities and other factors that may influence on the functionality of this complex spectrum of autism (Fig. 1).
Conclusions
This study supports the hypothesis that the DSM-5 classification includes patients who are more prone to clinical severity not only in relation to the core items of ASD, but also at the level of psychiatric comorbidities. Patients who met DSM-5 criteria had more comorbidity with OCD, eating behaviour problems and severity than patients who only met the DSM-IV-TR criteria. Future studies can contribute markedly to our better understanding the effect of the new classification in this population and answer more pointed scientific questions in relation with the phenotypic categorization of children with autism spectrum disorder.
References
- Aman M.G., Burrow W.H., Wolford P.L. The Aberrant Behavior Checklist-Community: Factor validity and effect of subject variables for adults in group homes. American Journal of Mental Retardation. 1995;100:283–292. [PubMed] [Google Scholar]
- American Psychiatric Association, APA . American Psychiatric Association; Washington. DC: 2013. Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5) [Google Scholar]
- Bandini L.G., Anderson S.E., Curtin C., Cermak S., Evans E.W., Scampini R., Maslin M., Must A. Food selectivity in children with autism spectrum disorders and typically developing children. Journal of Pediatrics. 2010;157:259–264. doi: 10.1016/j.jpeds.2010.02.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beighley J.S., Matson J.L., Rieske R.D., Jang J., Cervantes P.E., Goldin R.L. Comparing challenging behavior in children diagnosed with autism spectrum disorders according to the DSM-IV-TR and the proposed DSM-5. Developmental Neurorehabilitation. 2013;16:375–381. doi: 10.3109/17518423.2012.760119. [DOI] [PubMed] [Google Scholar]
- Bejerot S. An autistic dimension: a proposed subtype of obsessive-compulsive disorder. Autism. 2007;11:101–110. doi: 10.1177/1362361307075699. [DOI] [PubMed] [Google Scholar]
- Brereton A.V., Tonge B.J., Einfeld S.L. Psychopathology in children and adolescents with autism compared to young people with intellectual disability. Journal of Autism and Developmental Disorders. 2006;36:863–870. doi: 10.1007/s10803-006-0125-y. [DOI] [PubMed] [Google Scholar]
- Brown E.C., Aman M.G., Havercamp S.M. Factor analysis and norms for parent ratings on the Aberrant Behavior Checklist-Community for young people in special education. Research in Developmental Disabilities. 2002;23:45–60. doi: 10.1016/s0891-4222(01)00091-9. [DOI] [PubMed] [Google Scholar]
- Bryant-Waugh R., Markham L., Kreipe R.E., Walsh B.T. Feeding and eating disorders in childhood. International Journal of Eating Disorders. 2010;43:98–111. doi: 10.1002/eat.20795. [DOI] [PubMed] [Google Scholar]
- Costello E. Complementary and alternative therapies: Considerations for families after international adoption. Pediatric Clinic of North America. 2005;52:1463–1478. doi: 10.1016/j.pcl.2005.06.006. [DOI] [PubMed] [Google Scholar]
- Fountain C., Winter A.S., Bearman P.S. Six developmental trajectories characterize children with autism. Pediatrics. 2012;129:1112–1120. doi: 10.1542/peds.2011-1601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frazier T.W., Youngstrom E.A., Speer L., Embacher R., Law P., Constantino J., Eng C. Validation of proposed DSM-5 criteria for autism spectrum disorder. Journal of the American Academy of Child & Adolescent Psychiatry. 2012;51:28–40. doi: 10.1016/j.jaac.2011.09.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frias A., Palma C., Farriols N. Comorbidity in pediatric bipolar disorder: Prevalence, clinical impact, etiology and treatment. Journal of Affective Disorders. 2015;174:378–389. doi: 10.1016/j.jad.2014.12.008. [DOI] [PubMed] [Google Scholar]
- Gadow K.D., DeVincent C.J., Pomeroy J., Azizian A. Psychiatric symptoms in preschool children with PDD and clinic and comparison samples. Journal of Autism and Developmental Disorders. 2004;34:379–393. doi: 10.1023/b:jadd.0000037415.21458.93. [DOI] [PubMed] [Google Scholar]
- Gadow K.D., Guttmann-Steinmetz S., Rieffe C., Devincent C.J. Depression symptoms in boys with autism spectrum disorder and comparison samples. Journal of Autism and Developmental Disorders. 2012;42:1353–1363. doi: 10.1007/s10803-011-1367-x. [DOI] [PubMed] [Google Scholar]
- Gibbs V., Aldridge F., Chandler F., Witzlsperger E., Smith K. Brief report: An exploratory study comparing diagnostic outcomes for autism spectrum disorders under DSM-IV-TR with the proposed DSM-5 revision. Journal of Autism and Developmental Disorders. 2012;42:1750–1756. doi: 10.1007/s10803-012-1560-6. [DOI] [PubMed] [Google Scholar]
- Gonzalez M.L. Baton Rouge; Louisiana State University: 2008. The initial reliability and construct validity of the Autism Spectrum Disorders—Diagnostic in Children (ASD-DC). Unpublished doctoral dissertation. [Google Scholar]
- Grzadzinski R., Huerta M., Lord C. DSM-5 and autism spectrum disorders (ASDs): An opportunity for identifying ASD subtypes. Molecular Autism. 2013;4:12. doi: 10.1186/2040-2392-4-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holtmann M., Bolte S., Poustka F. Attention deficit hyperactivity disorder symptoms in pervasive developmental disorders: association with autistic behavior domains and coexisting psychopathology. Psychopathology. 2007;40:172–177. doi: 10.1159/000100007. [DOI] [PubMed] [Google Scholar]
- Howlin P., Goode S., Hutton J., Rutter M. Adult outcome for children with autism. Journal of Child Psychology and Psychiatry. 2004;45:212–229. doi: 10.1111/j.1469-7610.2004.00215.x. [DOI] [PubMed] [Google Scholar]
- Kerns C.M., Kendall P.C. The Presentation and Classification of Anxiety in Autism Spectrum Disorder. Clinical Psychology. Science and Practice. 2013;19:323–347. [Google Scholar]
- Kodak T., Piazza C.C. Assessment and behavioural treatment of feeding and sleeping disorders in children with autism spectrum disorders. Child and Adolescent Psychiatric Clinics of North America. 2008;17:887–905. doi: 10.1016/j.chc.2008.06.005. [DOI] [PubMed] [Google Scholar]
- Lecavalier L. Behavioral and emotional problems in young people with pervasive developmental disorders: Relative prevalence, effects of subject characteristics, and empirical classification. Journal of Autism and Developmental Disorders. 2006;36:1101–1114. doi: 10.1007/s10803-006-0147-5. [DOI] [PubMed] [Google Scholar]
- Lord C., Risi S., Lambrecht L., Cook E.H., Jr., Leventhal B.L., DiLavore P.C., Pickles A., Rutter M. The autism diagnostic observation schedule-generic: A standard measure of social and communication deficits associated with the spectrum of autism. Journal of Autism and Developmental Disorders. 2000;30:205–223. [PubMed] [Google Scholar]
- Lord C., Rutter M., Le Couteur A. Autism Diagnostic Interview-Revised: A revised version of a diagnostic interview for caregivers of individuals with possible pervasive developmental disorders. Journal of Autism and Developmental Disorders. 1994;24:659–685. doi: 10.1007/BF02172145. [DOI] [PubMed] [Google Scholar]
- Matson J.L., Dempsey T., Lovullo S.V., Wilkins J. The effects of intellectual functioning on the range of core symptoms of autism spectrum disorders. Research in Developmental Disabilities. 2008;29:341–350. doi: 10.1016/j.ridd.2007.06.006. [DOI] [PubMed] [Google Scholar]
- Matson J.L., Hattier M.A., Williams L.W. How does relaxing the algorithm for autism affect DSM-V prevalence rates? Journal of Autism and Developmental Disorders. 2012;42:1549–1556. doi: 10.1007/s10803-012-1582-0. [DOI] [PubMed] [Google Scholar]
- Matson J.L., Kozlowski A.M., Hattier M.A., Horovitz M., Sipes M. DSM-IV vs DSM-5 diagnostic criteria for toddlers with autism. Developmental Neurorehabilitation. 2012;15:185–190. doi: 10.3109/17518423.2012.672341. [DOI] [PubMed] [Google Scholar]
- Mattila M.L., Kielinen M., Linna S.L., Jussila K., Ebeling H., Bloigu R., Joseph R.M., Moilanen I. Autism spectrum disorders according to DSM-IV-TR and comparison with DSM-5 draft criteria: an epidemiological study. Journal of the American Academy of Child & Adolescent Psychiatry. 2011;50 doi: 10.1016/j.jaac.2011.04.001. 583-592.e511. [DOI] [PubMed] [Google Scholar]
- McDougle C.J., Kresch L.E., Goodman W.K., Naylor S.T., Volkmar F.R., Cohen D.J., Price L.H. A case-controlled study of repetitive thoughts and behavior in adults with autistic disorder and obsessive-compulsive disorder. American Journal of Psychiatry. 1995;152:772–777. doi: 10.1176/ajp.152.5.772. [DOI] [PubMed] [Google Scholar]
- McPartland J.C., Reichow B., Volkmar F.R. Sensitivity and specificity of proposed DSM-5 diagnostic criteria for autism spectrum disorder. Journal of de American Academy of Child and Adolescent Psychiatry. 2012;51:368–383. doi: 10.1016/j.jaac.2012.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norris M., Lecavalier L. Evaluating the validity of the Nisonger Child Behavior Rating Form--parent version. Research in Developmental Disabilities. 2011;32:2894–2900. doi: 10.1016/j.ridd.2011.05.015. [DOI] [PubMed] [Google Scholar]
- Rao P.A., Landa R.J. Association between severity of behavioral phenotype and comorbid attention deficit hyperactivity disorder symptoms in children with autism spectrum disorders. Autism. 2014;18:272–280. doi: 10.1177/1362361312470494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rastam M., Taljemark J., Tajnia A., Lundström S., Gustafsson P., Lichtenstein P., Gillberg C., Anckarsäter H., Kerekes N. Eating Problems and Overlap with ADHD and Autism Spectrum Disorders in a Nationwide Twin Study of 9- and 12-year-old children. Scientific World Journal. 2013;2013:315429. doi: 10.1155/2013/315429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rivière A. Fundec; Buenos Aires: 2002. IDEA: Inventario de Espectro Autista. [Google Scholar]
- Robles R., Fresán A., Evans S.C., Lovell A.M., Medina-Mora M.E., Maj M., Reed G.M. Problematic, absent and stigmatizing diagnoses in current mental disorders classifications: Results from the WHO-WPA and WHOIUPsyS Global Surveys. International Journal of Clinical and Health Psychology. 2014;14:165–177. [Google Scholar]
- Rodríguez-Testal J.F., Senín-Calderón C., Perona-Garcelán S. From DSM-IV-TR to DSM-5: Analysis of some changes. International Journal of Clinical and Health Psychology. 2014;14:221–231. [Google Scholar]
- Simonoff E., Pickles A., Charman T., Chandler S., Loucas T., Baird G. Psychiatric disorders in children with autism spectrum disorders: Prevalence, comorbidity, and associated factors in a population-derived sample. Journal of the American Academy of Child and Adolescent Psychiatry. 2008;47:921–929. doi: 10.1097/CHI.0b013e318179964f. [DOI] [PubMed] [Google Scholar]
- Sinzig J., Walter D., Doepfner M. Attention deficit/hyperactivity disorder in children and adolescents with autism spectrum disorder: Symptom or syndrome? Journal of Attention Disorders. 2009;13:117–126. doi: 10.1177/1087054708326261. [DOI] [PubMed] [Google Scholar]
- Snyder R., Turgay A., Aman M., Binder C., Fisman S., Carroll A. Effects of risperidone on conduct and disruptive behavior disorders in children with subaverage IQs. Journal of the American Academy of Child and Adolescent Psychiatry. 2002;41:1026–1036. doi: 10.1097/00004583-200209000-00002. [DOI] [PubMed] [Google Scholar]
- Soutollo C.M. Editorial Médica Panamericana; Buenos Aires.: 2010. Manual de Psiquiatría del Niño y del Adolescente. [Google Scholar]
- Timini S. No more psychiatric labels: Why formal psychiatric diagnostic systems should be abolished. International Journal of Clinical and Health Psychology. 2014;14:208–215. [Google Scholar]
- Turygin N., Matson J.L., Beighley J., Adams H. The effect of DSM-5 criteria on the developmental quotient in toddlers diagnosed with autism spectrum disorder. Developmental Neurorehabilitation. 2013;16:38–43. doi: 10.3109/17518423.2012.712065. [DOI] [PubMed] [Google Scholar]
- van Steensel F.J., Bogels S.M., Perrin S. Anxiety disorders in children and adolescents with autistic spectrum disorders: a meta-analysis. Clinical Child and Family Psychology Review. 2011;14:302–317. doi: 10.1007/s10567-011-0097-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White S.W., Oswald D., Ollendick T., Scahill L. Anxiety in children and adolescents with autism spectrum disorders. Clinical Psychology Review. 2009;29:216–229. doi: 10.1016/j.cpr.2009.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White S.W., Smith L.A., Schry A.R. Assessment of global functioning in adolescents with autism spectrum disorders: utility of the Developmental Disability-Child Global Assessment Scale. Autism. 2014;18:362–369. doi: 10.1177/1362361313481287. [DOI] [PubMed] [Google Scholar]
- Wing L., Gould J., Gillberg C. Autism spectrum disorders in the DSM-V: Better or worse than the DSM-IV? Research in Developmental Disabilities. 2011;32:768–773. doi: 10.1016/j.ridd.2010.11.003. [DOI] [PubMed] [Google Scholar]
- Worley, J. A., & Matson, J. L. (2012). Comparing symptoms of autism spectrum disorders using the current DSM-IV-TR diagnostic criteria and the proposed DSM-V diagnostic criteria. Research in Autism Spectrum Disorders, 6, 965-970. http://dx.doi.org/10.1016/j.rasd.2011.12.012
- Yerys B.E., Wallace G.L., Jankowski K.F., Bollich A., Kenworthy L. Impaired Consonant Trigrams Test (CTT) performance relates to everyday working memory difficulties in children with autism spectrum disorders. Child Neuropsychology. 2011;17:391–399. doi: 10.1080/09297049.2010.547462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zandt F., Prior M., Kyrios M. Repetitive behaviour in children with high functioning autism and obsessive compulsive disorder. Journal of Autism and Developmental Disorders. 2007;37:251–259. doi: 10.1007/s10803-006-0158-2. [DOI] [PubMed] [Google Scholar]