Abstract
CONTEXT:
Health system reform plan refers to conducting some fundamental, systematic, and sustainable changes.
AIMS:
The aim of the present study was to evaluate different required inputs of Iran Health Transformation Plan from experts’ viewpoints.
SETTINGS AND DESIGN:
The data of this qualitative study were collected using semi-structured interviews.
SUBJECTS AND METHODS:
The purposive sampling method led to 18 participant selection and then they were interviewed. Interviewees were assured about confidentiality of information.
STATISTICAL ANALYSIS USED:
The thematic analysis method and MAXQDA software were employed for analyzing the data.
RESULTS:
There were 4 main themes and 35 subthemes extracted including management requirements for health development plan, human resources, information resources, and financial resources. Each theme had subthemes such as “resource allocation,” “development of required standards for human resources,” “human resources’ motivation,” “failures in IT infrastructures,” “hospital information management software,” “guidelines and instructions,” “costs controlling,” and “financing the plan”.
CONCLUSIONS:
Results of the present study put significant emphasis on the path of improving the effectiveness and efficacy of applying the discussed inputs, which can be a light for revising past policies and taking better future steps, it also can be a resource guide for policy-makers and managers of the health-care system.
Keywords: Health system reform plan, health-care system, inputs, inputs of Iran's health system reform plan, qualitative research
Introduction
Health system reforms (HSR) have been the central point of policy-makers’ discussions in developing and developed countries for many years[1] and now it changed to an international agenda in health-care policy-making statement.[2,3,4] HSR is defined as a positive change referring to a continuous and purposive evolution for improving efficacy, justice, and effectiveness of the health sector.[5] All available studies are in common in a fact that HSR has no single definition extendable to all conditions due to its political and heavy reliance on social and local conditions of a country. In Iran, the HSR refers to “measuring fundamental, purposive, and sustainable changes to increase efficacy and costs effectiveness of interventions, promote justice, improve services quality, and reform management practices in the health-care sector.”[6]
Factors such as system weaknesses, past failures, changing pattern of diseases (the epidemiological transition), demographic changes, new equipment and technologies, providers’ demands, raised health costs, and resource constraints (especially financial one); all can make the HSR unavoidable.[7,8,9] The HSR is an opportunity for identifying the needs and adding extra power to the health systems. For this reason, searching for a better health-care system can be considered as a permanent task. Even in those countries with 100-year-old health systems, an improved mechanism which can guarantees efficient financing, appropriate organization, and high-quality service delivery is an ongoing job.[6] Committing any changes in the term of HSR would be difficult and beneficiary institutions and groups will have enough resources and reasons for opposing these changes. As a consequence, the beginning of HSR will be along with different types of political and economic shocks such as budget crisis, changes in coalition of governments, strikes of service providers, or a combination of these problems. Therefore, reform designers should consider necessary capacities and take the opportunity of a big change in Iran's health system.[10,11]
Capacity building for policies, which covers all stages of the policy-making cycle from identifying problems to collecting data and developing options for basic actions in the early phase of developing policies, acceptance of policies, implementation, and even evaluation, is one of the most important factors of accepting a health-care reform.[12,13] Reform success and its survival will be at risk without the shareholders’ supports. Desirability of extracting stakeholders’ viewpoints including the staff in a lot of countries which their health systems faced reforms has been confirmed, particularly in the initial stages of reforms implementation in which changes and modification are still possible.[14]
What can be inferred from the review of studies related to the evaluation of the HSR both inside and outside each country is that designing and implementing any reform plan in the form of a policy requires providing necessary infrastructures. Clear policy statements, proper infrastructures to facilitate implementation, a developed road map, and approved processes selections are the vital elements for successful implementation of any reform. Without considering shareholders including individuals, groups, and organizations; which are at the center of policy-making triangle, all policies will definitely fail in the implementation phase and would not reach their goals. In developing countries health systems, the policies are seldom evaluated accurately. The main reason for this lack of assessment is the fact that reform concurrently carry out countrywide and generating a closed up picture would not be that easy.[15]
The spirit prevailing the higher orientation of system in the Iran's 20-year outlook program, the Article number 44 of the Fundamental Law, Iran's economic upheavals and its rely on developing sciences and technologies,[8,16] policies issued by the supreme leader, fourth and fifth development program legislation, etc., have been effective factors on the establishment of the HSR in this country. The Ministry of Health and Medical Education which is responsible for the health sector in Iran started the implementation of this change plan with the aim of increasing satisfaction, providing quality of appropriate services, and reducing patients’ costs since May 2014.[17,18]
This plan included seven executive packages including reducing the inpatients’ payment in hospitals affiliated to the Ministry of Medical Education, promoting natural delivery, increasing the quality of hospitals’ hoteling, the presence of specialists in hospitals, supporting physicians presence in remote areas, financial protecting of patients with incurable diseases and those in need, and finally improving the quality of outpatient services.[19] Therefore, the present study was conducted with the aim of investigating inputs of Iran HSR Plan based on viewpoints experts, managers, and authorities of Isfahan University of Medical Sciences.
Subjects and Methods
In the present applied study conducted in 2015, the qualitative research approach was used. To collect the required data, in-depth interviewing technique was employed. The interview structure consisted of four main categories of questions: The first category was about implementations process, the second one ask about the plan weakness and problems, the third part ask about plan evaluation, and the final category of the questions work on the participant suggestions to improve the overall plan process. Participants included experienced experts who were aware in the field of study. Face-to-face interviews were carried out in Isfahan University of Medical Sciences subordinates including hospitals and treatment centers, Management and Development of Human Resources Deputy, Treatment Deputy, Food and Drugs Deputy, Health Deputy; and two main insurer organizations including Iranian Health Insurance and Social Security Insurance. In addition, those executive managers and policy-makers participating in reform plan implementation and its advancement were involved. Adding participants to the sample size continued for reaching data saturation. The duration of interviews ranged from 30 to 90 min.
To achieve validity and reliability of interviews, the triangulation technique including the use of interview guide and confirmation of frameworks of interviews using ideas of other researchers were used. Interviewees obey the neutralism while collecting the data. Some interviews were conducted as a trial before the official beginning of the study. Then, to obtain the validity, these interviews were investigated in terms of accuracy. After essential modifications, the main phase of research started. To enhance the trustworthiness of findings, researchers referred transcribed interviews to participants and their comments were considered. In addition, researchers tried to use high analytical subtlety for creating a theoretical framework. The use of coding existing categories in interviews contributed to enriching the research. Criteria such as “reliability of the data,” “trustworthiness,” and “confirmability” were considered. The data analysis is based on the thematic analysis method.
The stages of data analysis included extracting and transcribing data as well as saving them in the computer, being saturated in data, coding, recording reflective signs, abbreviating, and developing suggestions. To do these stages, MAXQDA version 10 software was employed. In the first step, after holding each interview, it was transcribed, typed, and then saved to the computer. In the next step, the texts were reviewed in a way that the researchers gained sufficient proficiency. In the third step, the data were divided into thematic units (codes) in the form of propositions and paragraphs related to the main theme. Those thematic units were reviewed several times and then appropriate codes of each thematic unit were transcribed. So that in each interview, subthemes were separated from each other and after that, those subthemes were mixed and reductionism was conducted; and finally, the main themes were determined. Recording reflective and peripheral signs is in fact recording notes of thoughts and ideas created in researchers’ minds and registered during interviews and data analysis. These signs connected notes to other parts of the data. Ethical considerations (code 78862) were taken into account; interviewees’ informed consent forms were prepared and they were informed that their interviews would be recorded for facilitation of transcription. Interviewees were assured that their statements and information were confidential.
Results
The input required for implementing Iran health system reform plan
In this study performed based on thematic analysis, four themes and four subthemes were found. The four main themes that participants considered as the inputs of Iran HSR Plan and the main factors in its implementation included “Management Requirements for the Health Reform Plan,” “Human Resources,” “Information Resources,” and “Financial Resources” [Table 1].
Table 1.
Inputs of Iran health system reform plan
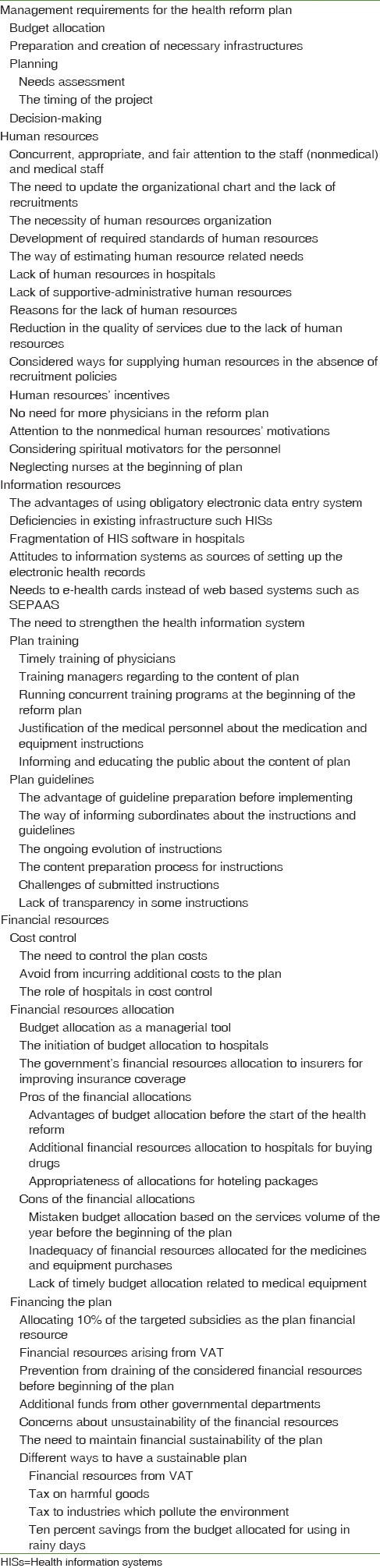
Management requirements for the health system reform plan
Statements made by participants showed that different administrative requirements were needed to initiate the Health Reform Plan: “resource allocation methods,” “preparation and developing infrastructures,” “planning,” and “decision-making.”
“There must be sort of interventions to people socioeconomically; and those with higher socioeconomical levels should be eliminated from the general subsidy and allocate the gained money to the Healthcare” (Interviewee number 13). “In hoteling, they thought about luxury; they didn’t think of infrastructures. At first, they said, “We should work on the wallpapers”, and we said “but the sewage system has many problems”; we need to install double glazed windows to decrease energy consumption; the first view was not firm.” (Interviewee number 1). “Some central studies had been done on this plan, but these prioritized preliminary studies had not been transferred to provinces and regional units.” (Interviewee number 5). “They said ‘bring your plan and get the money.’ Therefore, we had to quickly draft the initiative, which we had worked on before, and submit.” (Interviewee number 3). “Everything should be done in the form of a committee…from policy-making committee to committees of resources such as insurance committee, etc., A committee results in collective decisions rather than individuals’ opinions.” (Interviewee number 1).
Human resources
Participants discussed issues such as “concurrent, appropriate, and fair attention to the staff (nonmedical) and medical staff,” “the need to update the organizational chart and the lack of recruitments,” “the necessity of human resources organization,” “development of required standards of human resources,” “the way of estimating human resource-related needs,” “lack of human resources in hospitals,” “lack of supportive-administrative human resources,” “reasons for the lack of human resources,” “reduction in the quality of services due to the lack of human resources,” “considered ways for supplying human resources in the absence of recruitment policies,” and “human resources’ incentives.” Finally, two participants stated that “there is no need for more physicians in this reform plan.”
“One of the most important factors that could lead to the success or failure of this plan is human resources. The number of the personnel and their payments mechanism should be seen as a whole.” (Interviewee number 13). “Our organizational chart is not up-to-date, we’ve had a lot of personnel drain and the volume of operations and the types and varieties of operations which have become part of hospitals’ duties are more varied now and they are seen in the organizational charts.” (Interviewee number 2). “The challenge that this plan faces is human resources; we haven’t recruited in the last couple of years, especially in Nonmedical staffs. There are rapidly increased number of physicians’ visits and high levels of expectations” (Interviewee number 12). “Medical staff was included in this plan, nurses were gradually included, midwives were included, but administrative personnel such as IT and medical document staffs who have to be included and motivated are not seen in the initiative's packages.” (Interviewee number 5). “A nurse must have the time to take care of other patients; money doesn’t solve this. You should employ enough nurses to take care of your patients; this isn’t the way to do it” (Interviewee number 2). “Look, the ministry of health had some alternatives: Retirement will happen after thirty years of work experience, but the ministry abolished this limitation and allowed nurses to remain in their jobs. Our university also allowed employees to work more than 30 years. It allowed us to employ part-time personnel to replace with those who go on pregnancy or to work where there are staff shortages. Yes there will be different rules, but this has resolved the issue of human resources, especially in nursing staffs.” (Interviewee number 1). “Considering the budgeting and incentives for clinical staffs is really important” (Interviewee number 12). “Nurses were very dissatisfied at first, they were right somehow. Because the system worked based on doctors’ authority (Interviewee number 17).
Information resources
In the information resources section of the initiative, participants mentioned the following issues: “the advantages of using obligatory electronic data entry system,” “deficiencies in existing infrastructure such as health information systems (HISs),” “Fragmentation of HIS software in hospitals,” “Attitudes to information systems as sources of setting up the Electronic Health Records (EHRs),” “needs to e-health cards instead of web-based systems such as SEPAAS,” “the need to strengthen the health information system,” “plan training,” and “plan guidelines.”
“One of the advantages of this initiative was the obligation of hospitals to be connected to the HIS and SEPAAS programs. Also, all treatment centres discovered existing defects of their HIS” (Interviewee number 17). “We wanted to have deposits of information and their outputs should be integrated as well. Variety of IT companies have suggested designing integrated output reports of their different software and they can be linked nationwide” (Interviewee number 9). “This was a shock to different types of HIS software and considering SEPAAS web-based Software so that the patient's electronic records and the more efficient costs controls can be reached.” (Interviewee number 2). “These could lead to smart e-health cards feasibility study for Iranian people who their health information can be stored in it” (Interviewee number 2).
Regarding the necessary of trainings for best implementation of the initiative, participants mentioned the following: “Timely Education of Physicians,” “Training Managers Regarding to the Content of Plan,” “Running Concurrent Training Programs at the Beginning of the Reform Plan,” “Justification of the Medical Personnel about the Medication and Equipment Instructions,” and “Informing and Educating the Public About the Content of Plan.”
“First, they should have completely briefed the educational-medical society about this initiative. We implemented the plan and asked them to follow it, well this has consequences. Some accept and some try to change the paths.” (Interviewee number 10). “Two training courses were organized for Heads of hospitals till now; the University of Medical Sciences has organized several educational classes for hospital directors and head nurses.” (Interviewee number 12). “When the initiative was announced, we organized several meetings. We organized separate meetings for our physicians and staff in their respected fields (surgery, nursing, supervising, etc.) and everything was explained in detail” (Interviewee number 12). “It seems that mass Media like National TV and Radio, journals and hospitals themselves have promoted the plan in proper ways.” (Interviewee number 2).
Participants mentioned some subthemes in the broader category of “Plan Guidelines:” “The Advantage of Guideline Preparation before Implementing,” “The Way of Informing Subordinates about the instructions and Guidelines,” “The Ongoing Evolution of Instructions,” “The Content Preparation Process for Instructions,” “Challenges of Submitted Instructions,” and finally “Lack of Transparency in some Instructions.”
“We believe this was the first time an initiative was introduced with all the considerations taken into account before implementation; its infrastructures and rules were already there which means, there were plans. This didn’t exist before. It had a really good start too. Then they provided some tools, their answers were up to date, they had launched a website. Even the minister himself and his subordinates all were responsive to upcoming questions. In addition, policy-making committees were put in place which reduced much duplication.” (Interviewee number 1). “At first, there were many ambiguities, but later announcements they were clarified. Questions were asked and answered, but the instructions still need to be developed.” (Interviewee number 13). “For example, in one of its instructions… we have the rule. The fourth and fifth development law is that people should pay less than 10% of their healthcare costs. Many people, based on available information, face catastrophic payments due to their need to healthcare services”. (Interviewee number 14).
Financial resources
Participants mentioned the following regarding the “Financial Resources”: “Costs Control,” “Financial Resources Allocation,” and “Financing the Plan.”
Participants believed that issues such as “The Need to Control the Plan Costs,” Avoid from Incurring Additional Costs to the Plan,” and “The Role of Hospitals in Cost Control” are important in controlling the costs of the plan:
“When the government cuts its expenses so that it can pay for healthcare, it is normal that the head of our Hospitals or their financial supervisors be very meticulous in expending the funds.” (Interviewee number 4). “Patients have paid to commercial insurance companies, which are competing with each other in a free market. Now that the reform has happened, they should not evade their obligations and try to impose their expenses on hospitals.” (Interviewee number 4).
In the case of “Financial Resources Allocation,” participants pointed out issues such as “Budget Allocation as a Management Tool,” “The Initiation of Budget Allocation to Hospitals,” “The Government's Financial Resources Allocation to Insurers for Improving Insurance Coverage,” “Pros of the Financial Allocations,” and finally “Cons of the Financial Allocations.”
“It was a good idea that Medical Universities control and allocate the funds; it's a management tool which makes the reform goals more reachable.” (Interviewee number 13). “They said the information was obtained from nationwide hospitals in the last fiscal year; then a mean estimation was done and based on this estimation the reform funds were allocated to all Medical Universities.” (Interviewee number 3). “We conclude, then, that this numbers are only estimations and there is no clear data in this field. After one year of reform implementation, there might be more valid evidence for better resources allocation.” (Interviewee number 2). “Well, the insurances didn’t have enough money to pay for the unmet costs. The government said “we’ll provide you some funding to cover those services that are not in your schemes. Let the patient pay only the 10%.” (Interviewee number 8).
Participants pointed “Advantages of Budget Allocation before the Start of the Health Reform”, “Additional Financial Resources Allocation to Hospitals for Buying Drugs”, and “Appropriateness of Allocations for Hoteling Packages” as the strong points of the allocations done in this reform plan:
“This was the first time that funds were allocated first and then a plan was started. So since the government was really determined to address this, funds were allocated beforehand.” (Interviewee number 4). “The plan provided hospitals with money, money in addition to their revenues so that they could fill up the gaps using that money.” (Interviewee number 8). “Regarding to hoteling services, good funds were allocated in my opinion. It really gave hospitals a push.” (Interviewee number 17).
Participants mentioned the followings as shortages of resource allocation in this reform plan: “Mistaken Budget Allocation Based on the Services Volume of the Year before the Beginning of the Plan,” “Inadequacy of Financial Resources Allocated for the Medicines and Equipment Purchases,” and “Lack of Timely Budget Allocation Related to Medical Equipment.”
“They said that spending in the reform implementation year must be the same as previous fiscal year which means the overall volume of the provided services should have almost the fashion of that year. This means we are dictating to the great people of Iran not to get sick more than last year. This isn’t based on management principles.” (Interviewee number 9). “They forced us to buy our needed medicines and equipment in cash. Each year our hospital needs about 15 billion Rials for medicine and equipment; while they are paying just 5-6 billion Rials. How can we buy them in cash?” (Interviewee number 6).
In relation to the “Financing the Reform Plan,” participants raised issues such as “Allocating 10 percent of the Targeted Subsidies as the Plan Financial Resource,” “Financial Resources Arising from VAT,” “Prevention from Draining of the Considered Financial Resources before Beginning of the Plan,” “Additional Funds from other Governmental Departments,” “Concerns about Unsustainability of the Financial Resources,” “The Need to Maintain Financial Sustainability of the Plan,” and “Different Ways to have a Sustainable Plan.”
“They passed a law in congress to spend 10% of the subsidies to support the health program.” (Interviewee number 10). “They said that 100% of the required financial resources will be procured.” (Interviewee number 12). “What happened here was the beginning of the Iranian Subsidy Reform plan. The government encourage people to voluntary relinquish their subsidies. Then the government tried to show that if people relinquish their subsidies, the gathered money will be spend to benefit the country and healthcare was a nice choice.” (Interviewee number 15). “Financial resources had already been specified even before the reform implementation, money it was in Universities’ bank accounts, but they were not allowed to withdraw sooner than they were allowed.” (Interviewee number 5). “Anyhow, this plan is funded by the government; the government is cutting down the expenses of other sectors to be able to cover the expenses of this plan.” (Interviewee number 4). “One concern that we all have is about the resources sustainability. According to physicians and other hospital staffs’ experiences, that been repeated in previous years. They say that there have been many such plans but they weren’t permanent. I heard someone say: “one of my friends said there is no need to try so hard! Like other plans this one would be cancelled after a while.” (Interviewee number 3).
In addition, participants indicated that “Financial Resources from VAT,” “Tax on Harmful Goods,” “Tax to Industries which Pollute the Environment,” and “Ten Percent Savings from the Budget Allocated for Using in Rainy Days” are some of the suitable strategies that can be considered for maintaining the financial resources of the reform plan:
“Generally, one of the financial resources predicted for the plan is this 1% value added tax which is a really sustainable resource.” (Interviewee number 1). “If they can levy permanent taxes on harmful goods…well, this requires enthusiasm in concurrent and next Congresses. This congress mans has supported the reform plan so far, since this is a right of all Iranian to have access to high quality and low cost services” (Interviewee number 1).
Discussion
Explaining experiences of policy-makers and managers in terms of Iranian HSR Plan in Isfahan University of Medical Sciences has been the main aim of the present study. Consequently, we tried to identify and present the recent reform's inputs.
Findings of the present study introduced management and executive requirements of the plan, financial resources, human resources, and information resources as the most important inputs required for implementing the HSR. Each of these items covered many details but only the most important ones are discussed here.
The resource allocation as one of the main topics sustainable financing was considered as an important issue in the matter of financial resources of the recent reform plan. Participants emphasized on Iranian recent subsidization change plan and utilizing the gained cash resources from higher socioeconomically level families to fill the health-related gape among poorer families of the society. Since the conflict of unlimited human needs and limited resources have always been the main problem in all economies; therefore, optimal resource allocation for priorities seems to be an unavoidable issue. Especially in our country's new economic condition – a rapid reduction in oil incomes – the necessity of paying attention to resistant economy policies as a solution for Iran's sustainable development; is really important. Macrolevel rules and plans in Iran support this resistant economy approach too. In addition, system financing through VAT tax as well as participation of private sector and insurance organizations which are applied as sustainable financing methods in developed countries health care. Hence, planning and targeting these in our macroeconomic plans and health care seem necessary.
Regarding human resources, the present study indicated that most participants believed to the lack of human resources in different medical, clinical, and administrative sections and mentioned problems such as necessity of updating organizational charts and arrangement. In addition, in relation to financial motivators for the human resource, and also its acceptable standards, some weaknesses were cited. The main challenge caused by inadequate human resource is the reduction in services quality inferred from the comments of participants. They believed that by creating more financial motivators for current human forces not only solve the problem but also damages the services quality. Related literature also emphasizes on importance of quantity and quality of human forces in health systems. The World Health Organization 2006 report focused on the upcoming importance of health-care human resources (years 2006–2015). Moreover, studies conducted in most Eastern Mediterranean countries which the global bank have put them in the group of countries with low and middle income, indicate limited knowledge and awareness about the nature, variety, and combination, of health-related human resources needs. The insufficient health staff, other than adverse economic and social consequences, also will influences quality of health-care services with direct effects on the accessibility of those services.[20] In the 20-year outlook of the Human Resources Management Office, achieving a situation asks for real justice by creating fair job opportunities, decentralization, and elimination of deficiencies in human forces of the health sector are three main aims of the Health and Medical Education Ministry. Designing an efficient model fit in with for the health-related human resources expectations, requires detailed investigations on all the six stages of policy-making include identification, evaluation, development, implementation, assessment, and revision.[21] Therefore, revising the health human resources based on previous studies and complementary investigations seem necessary in such a way that by drawing the distance between the status quo and determining timetabled aims in the form of an operational plan, the desired aims can be achieved and the problem of lack of human resources as well as their arraignment and distribution can be solved.
Participants evaluated using integrated HIS programs nationwide as one of the advantages of this plan; however, some others declared some deficiencies. Participating managers’ opinion, like a lot of studies conducted in Iran and at the international level, and also health authorities’ ideas of during recent years emphasize on the necessity of EHRs. No connection among the existing EHRs systems was considered as one of the problems of the plan. According to participants, implementing the EHRs regarding to similar experiences in Iran is an achievable aim which has been neglected. Research evidence indicates that using the Computer Physician Order Entry (CPOE) has reduced the number of medication errors up to >80%, costs up to 13.1%, and duties up to 12.7%. Moreover, sing these technologies in outpatient care wards has resulted in 44 billion dollars of annual savings in costs and improving the quality of healthcare. The value of efficiency of using Information and Communications Technology (ICT) in the health industry has been estimated at least as 87 billion dollars per year. Therefore, realizing National Health Information Infrastructure (NHII) is considered as one of the applied achievements of ICT in the health sector.[21] What really affect our research process were the time limitations of the target population and rapid appointment cancellations because of heavy workload on them.
Conclusions
Conducted investigations in the present study indicated that Iran HSR Plan which is considered as the most comprehensive and serious plan in recent 10 years in the Iranian health system history, in addition to achieving significant successes, particularly in reducing individuals’ health costs in the society, requires some revisions. The results obtained from the present study regarding inputs of this plan were investigated in previous sections, but in conclusion, more considerable results can be presented here are not paying enough attention to the operational plans, weaknesses in plan designing, and generally the failure of transforming major policies into executive plans. Sometimes lack of down to earth policies, failure in understanding barriers, and lack of providing relevant feedbacks for the policy-makers can be seen. Each of these problems can cause the occurrence of the other. It seems that the lack of necessary motivation for making mutual relations, failure in benefit appropriate mechanism for presenting feedbacks, and deficiencies in understanding and regulating operational plans are issues which can be more investigated and studied.
Financial support and sponsorship
This study was financially supported by Isfahan University of Medical Sciences.
Conflicts of interest
There are no conflicts of interest
Acknowledgment
This paper is the result of a research project titled “decision makers and managers’ experiences from Healthcare Reform plan implementation in Isfahan University of Medical Sciences”. We thank all who guide and encouragement us in all research phases.
References
- 1.Lundberg M, Wang L, Coudouel A, Paternostro S. Worldbank publication; 2006. Health sector reforms. Analyzing the Distributional Impact of Reforms; pp. 43–110. [Google Scholar]
- 2.Lloyd-Sherlock P. Health sector reform in argentina: A cautionary tale. Soc Sci Med. 2005;60:1893–903. doi: 10.1016/j.socscimed.2004.08.032. [DOI] [PubMed] [Google Scholar]
- 3.Naylor MD, Aiken LH, Kurtzman ET, Olds DM, Hirschman KB. The care span: The importance of transitional care in achieving health reform. Health Aff (Millwood) 2011;30:746–54. doi: 10.1377/hlthaff.2011.0041. [DOI] [PubMed] [Google Scholar]
- 4.Whitehead D. Workplace health promotion: The role and responsibility of health care managers. J Nurs Manag. 2006;14:59–68. doi: 10.1111/j.1365-2934.2005.00599.x. [DOI] [PubMed] [Google Scholar]
- 5.Tarin EK. PhD thesis. University of Leeds; 2003. Health Sector Reforms: Factors Influencing the Policy Process for Government Initiatives in the Punjab (Pakistan) Health Sector 1993-2000; pp. 24–43. [Google Scholar]
- 6.Shadpour K. Health sector reform in Islamic republic of Iran. J Qazvin Univ Med Sci. 2006;10:45–63. [Google Scholar]
- 7.Davooudi S. Generalities about health systems-third book. Health Syst Reform. 2006:78–81. [Google Scholar]
- 8.Bashshur RL, Shannon GW, Krupinski EA, Grigsby J, Kvedar JC, Weinstein RS, et al. National telemedicine initiatives: Essential to healthcare reform. Telemed J E Health. 2009;15:600–10. doi: 10.1089/tmj.2009.9960. [DOI] [PubMed] [Google Scholar]
- 9.Hickie I, Groom G. Primary care-led mental health service reform: An outline of the better outcomes in mental health care initiative. Australas Psychiatry. 2002;10:376–82. [Google Scholar]
- 10.Fattahzadeh A, Ahmadvand A, Akbari M, Basamanji K, Poor Asghari H, Jamshidi H. Tehran: Ebne Sina's Cultural Institution; 2005. Getting Health Reform Right: A Guide to Improving Performance and Equity. [Google Scholar]
- 11.Asadi-Lari M, Sayyari AA, Akbari ME, Gray D. Public health improvement in Iran – Lessons from the last 20 years. Public Health. 2004;118:395–402. doi: 10.1016/j.puhe.2004.05.011. [DOI] [PubMed] [Google Scholar]
- 12.Forest PG, Denis JL, Brown LD, Helms WD. Health reform requires policy capacity. Int J Health Policy Manag. 2015;4:265–6. doi: 10.15171/ijhpm.2015.85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Davari M, Khorasani E, Bakhshizade Z, Jafarian Jazi M, Ghaffari Darab M, Maracy MR. Measuring equity in access to pharmaceutical services using concentration curve; model development. Iran J Pharm Res. 2015;14:1317–26. [PMC free article] [PubMed] [Google Scholar]
- 14.Zhou XD, Li L, Hesketh T. Health system reform in rural China: Voices of health workers and service-users. Soc Sci Med. 2014;117:134–41. doi: 10.1016/j.socscimed.2014.07.040. [DOI] [PubMed] [Google Scholar]
- 15.Wagstaff A, Yu S. Do health sector reforms have their intended impacts? The World Bank's Health VIII project in Gansu province, China. J Health Econ. 2007;26:505–35. doi: 10.1016/j.jhealeco.2006.10.006. [DOI] [PubMed] [Google Scholar]
- 16.Policy-Making-Council. Development of Health System Map: The Experiences of Countries in Planning for Healthcare Reform. Ministry of Health and Medical Education. 2010:121–31. [Google Scholar]
- 17.Health-and-Medical-Education. Evaluation of Health System Reform Plan in the Treatment Area. National Institute of Health Research. 2013;11:87102. [Google Scholar]
- 18.Zaez-Mahdavi M, Vaez-Mahdavi Z. Planning for justice: Justice challenges in the health system. Q Sci J Soc Econ. 2010;7:191–210. [Google Scholar]
- 19.Treatment-Deputy. Guidelines for Health System Reform Plan. Ministry of Health and Medical Education. 2014:13–18. [Google Scholar]
- 20.Imani R, Asefzadeh S, Mamikhani J. Comparative study on health human resources composition in the Eastern. J Qazvin Univ Med Sci. 2012;15:5–12. [Google Scholar]
- 21.Asadi F, Moghaddasi H, Hosseini A, Azizi-Gondozlu S. Feasibility of implementing national health information infrastructure in Iran, 2009. Health Inf Manage. 2012;9:631. [Google Scholar]


