ABSTRACT
This study examines the association between household air pollution from use of polluting cooking fuels and perinatal mortality in Bangladesh. We analysed the data from the Bangladesh Demographic and Health Surveys (BDHS) 2004, 2007, 2011, and 2014. The two outcome variables were stillbirth and early neonatal mortality. The exposure variable was type of primary cooking fuel used in the household (clean vs. polluting). Bivariate and multivariable analyses were conducted to obtain the crude and adjusted odds ratio (aOR), respectively. In the adjusted model, the exposure to polluting fuels was associated with early neonatal mortality (aOR: 1.46, 95% confidence interval [CI]: 1.01–2.10), but not with stillbirth (aOR: 1.25, 95% CI: 0.85–1.84). The effect of cooking with agricultural crop waste was greater for stillbirth (aOR: 1.76, 95% CI: 1.10–2.80) and for early neonatal mortality (aOR: 1.78, 95% CI: 1.13–2.80) which was also associated with wood as the main fuel (aOR: 1.52, 95% CI: 1.04–2.21). Using polluting fuels in an indoor kitchen was associated with an increased odds of stillbirth (aOR: 4.12, 95% CI: 1.49–11.41). Cooking with polluting fuels is associated with perinatal mortality. The combined association of polluting cooking fuels and indoor kitchen location was greater for stillbirth. This effect and the effect of different fuel types need further investigation. Although this is a large sample, there are some limitations with the BDHS data in both recording the exposure and the outcomes. A large prospective trial is needed to determine the precise effect size.
KEYWORDS: Perinatal mortality, Bangladesh, cooking fuel, household air pollution, stillbirth, early neonatal mortality
Background
Household air pollution is the third leading health risk for global mortality and the most important environmental health risk in the world, accounting for 4.3 million deaths every year [1–3]. Combustion from polluting fuels such as coal, charcoal, wood, and animal dung is the main contributor to household air pollution [4]. Globally, around 41% of households rely on polluting fuels as their primary cooking fuel [5]. The proportion is even higher in South Asia where ~61% of households depend on polluting fuels for cooking which ranked household air pollution as the number one health risk in South Asia [1]. In addition, these fuels are used indoors or in partly enclosed cooking areas which, along with inefficient stoves, result in a very high level of air pollution [6]. These emissions are known to include numerous noxious pollutants, including particulate matter, carbon monoxide, nitrogen dioxide, and carcinogenic organic air pollutants [6,7]. These are the same pollutants in ambient air and environmental tobacco smoke and are associated with several adverse pregnancy outcomes such as stillbirth, early neonatal mortality, and low birthweight [8]. Several studies have attributed maternal exposure to cooking fuel with adverse perinatal outcomes [8–16]. Most of these studies have focused on low birthweight and preterm birth with few assessing the impact on stillbirth [8–16]. One recent systematic review and meta-analysis conducted by Amegah et al. reported an increased risk of stillbirth with polluting fuels, and the summary effect estimate was 1.29 (95% CI: 1.18–1.41) [17], which is slightly lower than the previous estimates in Pope et al.’s systematic review (odds ratio [OR]: 1.51, 95% CI: 1.23–1.85) [12]. These systematic reviews consisted of the same four studies to assess the role of polluting fuels for stillbirth [8,9,16,18], with an additional study included in the Amegah et al.'s systematic review [10]; of the included studies, two used an unclear definition of stillbirth with a small sample size [16,18] and one did not adequately adjust for confounders [18]. Further, there was considerable variability in exposure assessment, which was noted as a major limitation of these studies [12,17]. The association for early neonatal mortality is also not clearly understood from these studies.
Every year, about 2.6 million babies are stillborn and 2.8 million die in the first week of life. More than 98% of these largely preventable deaths occur in low- and middle-income countries including Bangladesh, where most of these remain under-reported or underestimated due to a lack of proper registration systems [19,20]. The 2014 Bangladesh Demographic and Health Survey (BDHS) reports perinatal mortality to be 44 per 1000 pregnancies, where about 82% of households use polluting fuels for cooking [21]. Moreover, perinatal mortality is 34% higher in rural areas than in urban areas of Bangladesh (47 vs. 35 per 1000 pregnancies), where ~95% households rely on polluting fuels for cooking [21]. Like other developing countries, in Bangladesh, the magnitude of exposure is much higher among women and their young children, as women are predominantly responsible for cooking and children are often carried by their mother during the cooking [4]. A study from Bangladesh reported that women aged 20–60 years on average spend 3.8 h per day in the cooking area [22]. There is very limited evidence of the impact of polluting cooking fuels on perinatal mortality in Bangladesh. We therefore aimed to examine the association between polluting cooking fuels and perinatal mortality (stillbirth and early neonatal mortality) in Bangladesh.
Methods
Data source
We used the BDHS data from the years 2004, 2007, 2011, and 2014. BDHS is a nationally representative household survey carried out every three to four years under the authority of the National Institute of Population Research and Training of the Ministry of Health and Family Welfare. The survey employed a two-stage stratified cluster-sampling design with rural and urban samples to collect information from ever-married women aged 15–49 years and ever-married men aged 15–54 years about demographic and health status. Data were obtained from the website www.measuredhs.com. The BDHS consists of three types of questionnaires: household, women, and men. Our analysis was limited to the information obtained from the women’s and household questionnaires. A total of 58,141 ever-married women aged 15–49 years (11,440 women in 2004, 10,996 in 2007, 17,842 women in 2011, and 17,863 women in 2014) were interviewed in four BDHSs with an overall response of 98.2%. For the stillbirth analysis, our study included any singleton pregnancy and excluded twin pregnancies and the pregnancies which lasted less than 7 months (Figure 1). For the early neonatal mortality analysis, our study was based on the information of all live-born children within the last 5-year period preceding the survey years (BDHS 2004, 2007, 2011, and 2014). Women who were non-residents during the surveys and whose fuel type or important covariates were not known or missing were excluded from the analysis.
Figure 1.
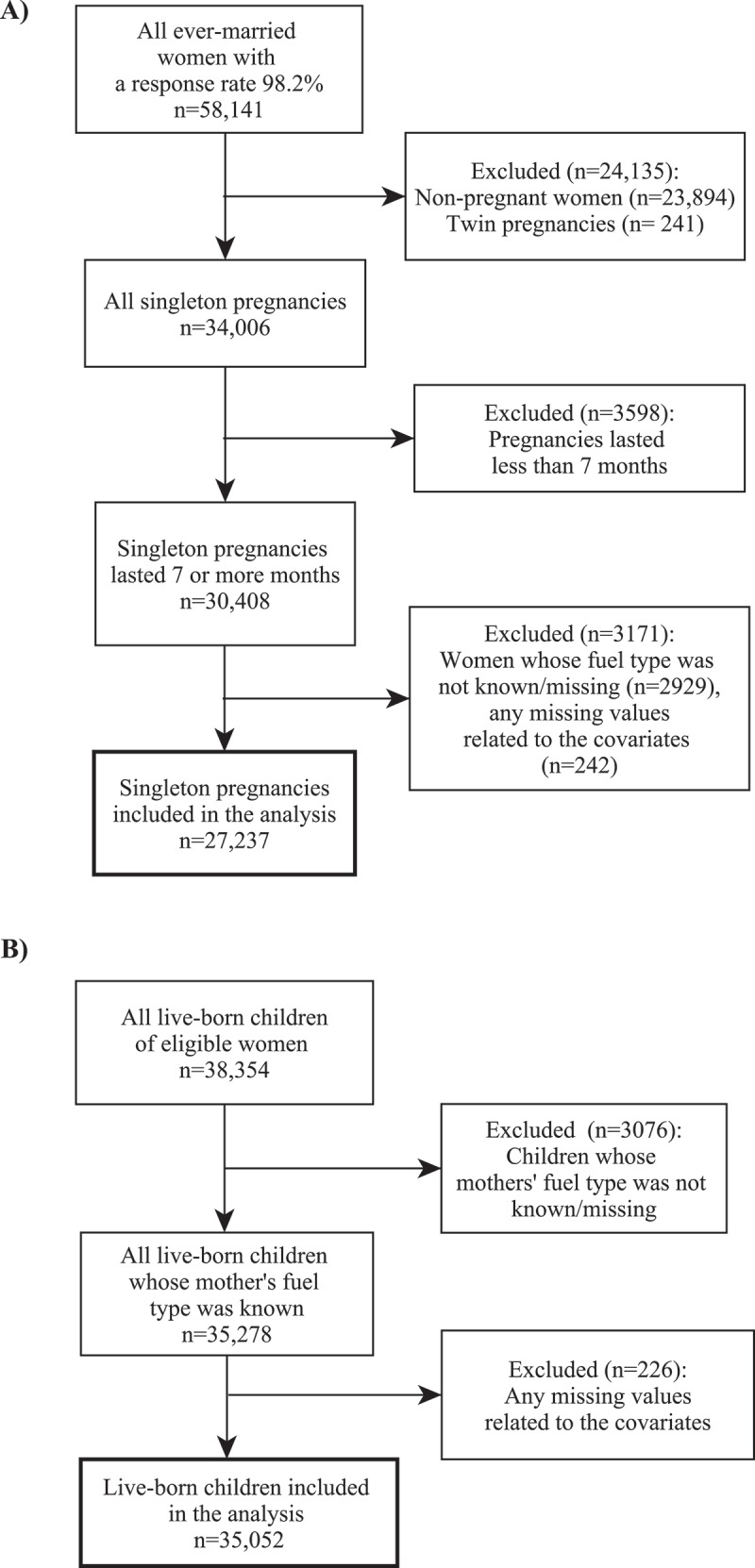
Flow diagram showing sample selection for stillbirth and early neonatal mortality analysis: (a) stillbirth and (b) early neonatal mortality.
Outcome variables
The outcome variables were stillbirth and early neonatal mortality. We used the international definition of stillbirth, a foetal death in pregnancy of at least seven or more months, and we defined early neonatal mortality as a death between the ages of 0 and 6 days among live-born children [23]. Both of the outcome variables were considered dichotomous for this analysis as yes (1) or no (0).
Exposure variable
The exposure variable was the type of primary cooking fuel used in the household. There were 12 types of cooking fuels in the BDHS data set. Based on previous studies, we classified cooking fuels into clean fuels (electricity, liquefied petroleum gas, natural gas, and biogas) and polluting fuels (kerosene, coal/lignite, charcoal, wood, straw/shrubs/grass, agricultural crop, and animal dung) [10,24–26].
Covariates
Covariates were maternal age at birth (19 years or below, 20–29 years, and 30 years or above), maternal education (no education, primary and secondary, or higher), birth order (first, second, and third or above), maternal body mass index (BMI) (underweight, normal, overweight, and obese), place of residence (urban and rural), wealth index (poor, middle, and rich), maternal working status during survey (not working and working), kitchen location (indoor and outdoor), and year of survey (2004, 2007, 2011, and 2014). We constructed the wealth index variable using principal component analysis through ranking the available wealth variables in the pooled BDHS data set such as housing materials, type of toilet facility, source of drinking water, availability of electricity, ownership of assets (radio, television, fridge, etc.), and adjusted for urban–rural differences.
Data analysis
The “stillbirth” variable was calculated based on the reported duration of pregnancy from the reproductive calendar data in each survey year data set. The reproductive calendar collects a month‐by‐month retrospective history of women’s key reproductive events such as pregnancies, births, contraceptive use, and terminations (stillbirths, miscarriages, and abortions) in the five-year period prior to the interview. For each pregnancy that did not end in a live birth, the duration of the pregnancy was recorded. Pregnancy losses occurring after seven completed months of gestation were calculated as stillbirths [27]. In the BDHS data, information on stillbirth is not included in the birth history which only contains the information on the live births. The “early neonatal mortality” variable was calculated from the birth history data, where age at death was recorded in days if they were less than one month old. Frequencies with weighted percentage were calculated for the selected variables to describe the characteristics of the women who had a stillbirth or those who had an early neonatal death. We employed bivariate analysis to ascertain the association between each of the independent variables and the outcomes variables. Also, multivariable analysis was performed to obtain the adjusted odds ratio (aOR). Wald test was used to assess statistical significance with 95% CI. The association was adjusted for potential confounders including maternal age at birth, maternal education, birth order, maternal BMI, maternal wealth index, maternal working status, place of residence, location of kitchen, and year of survey. We considered the impact of cooking fuel independently, as well as clean vs. polluting. We also stratified our analysis by kitchen location (indoor/outdoor) to assess the effect of cooking fuel and kitchen location. All analyses were carried out using STATA version 14.2. The “svy” command was used to calculate the weighted values. We obtained permission from Monitoring and Evaluation to Assess and Use Results Demographic and Health Surveys (MEASURE DHS) to download the data from the DHS online archive. Ethics approval was not required for this study, as the data were anonymous and publicly available.
Results
In total, over the four surveys, there were 27,237 singleton pregnancies of at least 7 months gestation, of which 767 (2.8%) resulted in a stillbirth. There were 241 twin pregnancies which were excluded from the stillbirth analysis. There were 35,052 live-born children over the four surveys, of which 706 (2.0%) resulted in an early neonatal death.
Stillbirth
Of the pregnancies resulting in a stillbirth, approximately 93% (n = 703) were to the women using polluting fuels as the primary cooking fuel. Nearly half of the stillbirths occurred to the women aged 20–29 years (n = 352, 44.1%) and were classified as “poor” on the wealth index (n = 359, 45.3%). Approximately 34% of stillbirths occurred to women who did not have any formal education (n = 254). Women residing in rural areas were more likely to have stillbirth than in urban areas (82.4% vs. 17.6%). The proportion of stillbirth was approximately 14% for women who reported cooking in an indoor kitchen (n = 139). Of all the survey years, 2004 had the highest proportion of pregnancies resulting in a stillbirth (n = 243, 32.1%), whereas 2007 had the lowest proportion of pregnancies resulting in a stillbirth (n = 151, 20.0%) (Table 1).
Table 1.
Stillbirth and early neonatal mortality by maternal characteristics in Bangladesh: BDHS 2004–2014.
| Stillbirth (N = 27,237) n (%) |
Early neonatal mortality (N = 35,052) n (%) |
||||
|---|---|---|---|---|---|
| Predictors | Yes (n = 767) | No (n = 26,470) | Yes (n = 706) | No (n = 34,346) | |
| Type of cooking fuels | Clean | 64 (7.1) | 3012 (11.1) | 58 (7.4) | 3554 (10.1) |
| Polluting | 703 (92.9) | 23,458 (88.9) | 648 (92.6) | 30,792 (89.9) | |
| Maternal age at birth | 19 years or below | 272 (36.5) | 8072 (31.1) | 290 (41.8) | 11,753 (34.8) |
| 20–29 years | 352 (44.1) | 14,154 (53.4) | 312 (43.9) | 17,710 (51.5) | |
| 30 years or above | 143 (19.4) | 4244 (15.5) | 104 (14.3) | 4883 (13.7) | |
| Maternal education | No education | 254 (34.1) | 6669 (26.2) | 187 (27.6) | 11,493 (34.8) |
| Primary | 236 (30.4) | 8076 (30.5) | 232 (32.4) | 10,427 (30.1) | |
| Secondary or higher | 277 (35.5) | 11,725 (43.3) | 287 (40.0) | 12,426 (35.2) | |
| Birth order | 1 | 253 (32.8) | 14,677 (55.6) | 313 (44.4) | 11,152 (32.3) |
| 2 | 344 (44.1) | 9497 (36.0) | 157 (22.3) | 9202 (26.9) | |
| 3 or above | 170 (23.1) | 2296 (8.4) | 236 (33.3) | 13,992 (40.8) | |
| Maternal BMI | Underweight | 226 (29.8) | 7731 (29.3) | 189 (26.5) | 10,330 (30.1) |
| Normal | 452 (60.1) | 15,353 (58.9) | 426 (61.7) | 19,605 (57.9) | |
| Overweight | 67 (7.2) | 2657 (9.3) | 66 (8.5) | 3438 (9.3) | |
| Obese | 22 (2.9) | 729 (2.5) | 25 (3.3) | 973 (2.7) | |
| Place of residence | Urban | 209 (17.6) | 8369 (22.5) | 224 (21.3) | 10,513 (21.6) |
| Rural | 558 (82.4) | 18,101 (77.5) | 482 (78.7) | 23,833 (78.4) | |
| Wealth index | Poor | 359 (45.3) | 11,269 (41.5) | 330 (44.9) | 15,959 (45.1) |
| Middle | 163 (21.0) | 5079 (19.4) | 160 (24.0) | 6335 (18.8) | |
| Rich | 245 (33.7) | 10,122 (39.1) | 216 (31.0) | 12,052 (36.1) | |
| Maternal working status | Not working | 610 (77.9) | 21,304 (79.4) | 553 (76.0) | 26,980 (77.8) |
| Working | 157 (22.1) | 5166 (20.6) | 153 (24.0) | 7366 (22.2) | |
| Kitchen location | Indoor | 139 (13.5) | 5316 (15.9) | 122 (12.8) | 6762 (15.5) |
| Outdoor | 628 (86.5) | 21,154 (84.1) | 584 (87.2) | 27,584 (84.5) | |
| Year of survey | 2004 | 243 (32.1) | 6137 (23.4) | 184 (27.6) | 8351 (24.5) |
| 2007 | 151 (20.0) | 5485 (20.2) | 162 (21.8) | 7297 (20.8) | |
| 2011 | 208 (26.9) | 7757 (29.2) | 193 (27.4) | 9933 (28.9) | |
| 2014 | 165 (21.0) | 7091 (27.2) | 167 (23.2) | 8765 (25.8) | |
Early neonatal mortality
For early neonatal mortality, approximately 93% (n = 648) of the infants were born to mothers who used polluting fuels as the primary cooking fuel. The highest proportion of the infants were born to the mothers aged 20–29 years (n = 312, 43.9%). Mother’s education level was inversely distributed within early neonatal mortality, with nearly 40% (n = 287) of early neonatal deaths occurring to mothers who completed secondary or higher education. Infants who died within the early neonatal period were more likely to be firstborn (n = 313, 44.4%). Similar to stillbirth, nearly half of the infants with early neonatal mortality were born to mothers classified as “poor” on the wealth index (n = 330). A major proportion of the infants with early neonatal mortality were born to mothers who lived in rural areas (n = 482, 78.7%) (Table 1).
Association of cooking fuel with stillbirth
In the unadjusted model, we found that exposure to polluting fuels compared to exposure to clean fuels was associated with the increased odds of stillbirth (aOR: 1.64, 95% CI: 1.20–2.25). After adjustment for potential confounders, the effect of cooking fuel remained positive although the effect was reduced and the CI included one (aOR: 1.25, 95% CI: 0.85–1.84). Also, maternal age at birth and birth order were associated with stillbirth in the adjusted model (Table 2). In a sensitivity analysis of types of cooking fuel used, we found that cooking with agricultural crops (as the main fuel type) was associated with an increased odds of stillbirth compared to clean cooking fuels even after adjustment (aOR: 1.76, 95% CI: 1.10–2.80) (Table 3).
Table 2.
Potential risk factors for stillbirth and early neonatal mortality in Bangladesh: BDHS 2004–2014.
| Stillbirth |
Early neonatal mortality |
||||||||
|---|---|---|---|---|---|---|---|---|---|
| Predictors | OR (95% CI) | P-value | aOR (95% CI) | P-value | OR (95% CI) | P-value | aOR (95% CI) | P-value | |
| Type of cooking fuels | Clean | Reference | Reference | Reference | Reference | ||||
| Polluting | 1.64 (1.20–2.25) | <0.01 | 1.25 (0.85–1.84) | 0.25 | 1.40 (1.01–1.95) | <0.05 | 1.46 (1.01–2.10) | <0.05 | |
| Maternal age at birth | 19 years or below | Reference | Reference | Reference | Reference | ||||
| 20–29 years | 0.70 (0.58–0.85) | <0.001 | 0.64 (0.53–0.78) | <0.001 | 0.71 (0.58–0.86) | <0.01 | 1.03 (0.80–1.33) | <0.05 | |
| 30 years or above | 1.07 (0.82–1.39) | 1.02 (0.78–1.34) | 0.87 (0.66–1.13) | 1.51 (1.03–2.20) | |||||
| Maternal education | No education | 1.58 (1.29–1.95) | <0.001 | 1.33 (1.01–1.74) | 0.10 | 0.70 (0.56–0.88) | <0.01 | 0.67 (0.52–0.87) | <0.01 |
| Primary | 1.22 (0.99–1.50) | 1.10 (0.88–1.39) | 0.95 (0.77–1.18) | 0.93 (0.73–1.18) | |||||
| Secondary or higher | Reference | Reference | Reference | Reference | |||||
| Birth order | 1 | Reference | Reference | Reference | Reference | ||||
| 2 | 2.07 (1.71–2.51) | <0.001 | 2.10 (1.73–2.54) | <0.001 | 0.60 (0.48–0.75) | <0.001 | 0.59 (0.45–0.76) | <0.001 | |
| 3 or above | 4.64 (3.61–5.96) | 4.57 (3.52–5.92) | 0.59 (0.48–0.73) | 0.53 (0.39–0.73) | |||||
| Maternal BMI | Underweight | 0.99 (0.82–1.21) | 0.30 | 0.89 (0.73–1.08) | 0.35 | 0.83 (0.67–1.02) | 0.25 | 0.80 (0.65–0.99) | 0.13 |
| Normal | Reference | Reference | Reference | Reference | |||||
| Overweight | 0.76 (0.57–1.02) | 1.03 (0.75–1.41) | 0.85 (0.61–1.18) | 0.96 (0.68–1.36) | |||||
| Obese | 1.14 (0.62–2.09) | 1.52 (0.82–2.82) | 1.16 (0.66–2.06) | 1.39 (0.77–2.49) | |||||
| Place of residence | Urban | Reference | Reference | Reference | Reference | ||||
| Rural | 1.36 (1.11–1.66) | <0.01 | 1.13 (0.90–1.40) | 0.29 | 1.02 (0.83–1.25) | 0.87 | 0.94 (0.75–1.19) | 0.62 | |
| Wealth index | Poor | 1.27 (1.05–1.53) | <0.05 | 0.86 (0.68–1.10) | 0.26 | 1.16 (0.94–1.43) | <0.01 | 1.29 (1.00–1.65) | <0.01 |
| Middle | 1.26 (1.01–1.57) | 1.02 (0.80–1.32) | 1.48 (1.16–1.90) | 1.51 (1.16–1.97) | |||||
| Rich | Reference | Reference | Reference | Reference | |||||
| Maternal working status | Not working | Reference | Reference | Reference | Reference | ||||
| Working | 1.09 (0.87–1.36) | 0.45 | 1.16 (0.92–1.46) | 0.20 | 1.10 (0.90–1.35) | 0.35 | 1.14 (0.92–1.42) | 0.22 | |
| Kitchen location | Indoor | Reference | Reference | Reference | Reference | ||||
| Outdoor | 1.21 (0.94–1.56) | 0.13 | 1.27 (0.98–1.65) | 0.07 | 1.25 (0.99–1.58) | 0.06 | 1.16 (0.90–1.48) | 0.25 | |
| Year of survey | 2004 | 1.79 (1.40–2.29) | <0.001 | 1.33 (1.03–1.73) | 0.17 | 1.25 (0.98–1.61) | 0.27 | 1.40 (1.07–1.83) | 0.08 |
| 2007 | 1.29 (0.98–1.70) | 1.11 (0.84–1.46) | 1.17 (0.89–1.54) | 1.22 (0.92–1.63) | |||||
| 2011 | 1.20 (0.93–1.54) | 1.11 (0.86–1.44) | 1.06 (0.82–1.36) | 1.12 (0.86–1.45) | |||||
| 2014 | Reference | Reference | Reference | Reference | |||||
Odds ratio was adjusted for maternal age at birth, maternal education, birth order, maternal BMI, place of residence, wealth index, maternal working status, location of kitchen, and year of survey.
Table 3.
Stillbirth and early neonatal mortality by different types of cooking fuel: BDHS 2004–2014.
| Stillbirth n (%) |
Early neonatal mortality n (%) |
|||||||
|---|---|---|---|---|---|---|---|---|
| Type of cooking fuels | Yes | No | aOR (95% CI) | P-value | Yes | No | aOR (95% CI) | P-value |
| Clean | 64 (7.1) | 3039 (11.2) | Reference | 58 (7.4) | 3584 (10.2) | Reference | ||
| Kerosene/coal/ lignite/charcoal |
86 (10.3) | 2510 (8.6) | 0.97 (0.56–1.68) | 0.92 | 76 (9.7) | 3319 (8.7) | 1.18 (0.71–1.98) | 0.53 |
| Wood | 287 (35.0) | 11,177 (39.3) | 1.34 (0.89–2.02) | 0.16 | 293 (37.2) | 14,172 (38.2) | 1.52 (1.04–2.21) | <0.05 |
| Straw/shrubs/grass | 124 (17.5) | 2945 (12.4) | 1.06 (0.63–1.78) | 0.82 | 85 (14.7) | 4161 (13.4) | 1.26 (0.75–2.14) | 0.39 |
| Agricultural crop | 170 (26.1) | 5138 (22.4) | 1.76 (1.10–2.80) | <0.05 | 152 (25.3) | 6992 (23.3) | 1.78 (1.13–2.80) | <0.05 |
| Animal dung | 36 (4.0) | 1661 (6.1) | 0.99 (0.55–1.75) | 0.96 | 42 (5.7) | 2118 (6.2) | 1.53 (0.88–2.67) | 0.13 |
Odds ratio was adjusted for maternal age at birth, maternal education, birth order, maternal BMI, place of residence, wealth index, maternal working status, location of kitchen, and year of survey.
Association of cooking fuel with early neonatal mortality
Exposure to polluting fuels was associated with early neonatal mortality in both unadjusted and adjusted models. The unadjusted odds of early neonatal mortality were 1.40 times higher among the infants born to mothers using polluting fuels in comparison with mothers using clean fuels for cooking (95% CI: 1.01–1.95). After adjustment for all potential confounders, the result was similar (aOR: 1.46, 95% CI: 1.01–2.10) (Table 2). We further examined the effects of different fuel types on early neonatal mortality and found that the odds of early neonatal mortality were greater when exposure to agricultural crop waste (aOR: 1.78, 95% CI: 1.13–2.80) compared to mothers using clean fuels for cooking, and use of wood compared to clean cooking fuels also posed a greater odds (aOR: 1.52, 95% CI: 1.04–2.21) (Table 3).
Effect of polluting cooking fuel by kitchen location
Women using polluting fuels in an indoor kitchen were 4.12 times more likely to have stillbirth even after adjustment (95% CI: 1.49–11.41), while for early neonatal death, this combined effect was smaller (aOR: 1.19, 95% CI: 0.60–2.36) (Table 4).
Table 4.
Combined association of cooking fuel and kitchen location with stillbirth and early neonatal mortality in Bangladesh: BDHS 2004–2014.
| Stillbirth |
Early neonatal mortality |
||||
|---|---|---|---|---|---|
| Type of cooking fuels | aOR (95% CI) | P-value | aOR (95% CI) | P-value | |
| Type of cooking fuels*Indoor kitchen | Clean | Reference | Reference | ||
| Polluting | 4.12 (1.49–11.41) | <0.01 | 1.19 (0.60–2.36) | 0.61 | |
| Type of cooking fuels*Outdoor kitchen | Clean | Reference | Reference | ||
| Polluting | 0.93 (0.64–1.37) | 0.72 | 1.43 (0.93–2.20) | 0.10 | |
Odds ratio was adjusted for maternal age at birth, maternal education, birth order, maternal BMI, place of residence, wealth index, maternal working status, location of kitchen, and year of survey.
Discussion
This study examines the association between exposure to polluting cooking fuels and perinatal mortality in a nationally representative population in Bangladesh over a 10-year time period. Our findings suggest that women cooking with polluting fuels are at increased odds of having stillbirth and early neonatal death in Bangladesh. Over the four surveys, we found that most women with a stillbirth or an early neonatal death were exposed to polluting fuels for cooking in Bangladesh. Exposure to polluting cooking fuels was associated with greater odds of early neonatal mortality. We also examined different exposure combinations such as estimating the effect for each type of polluting fuels and combining the effect of fuel with kitchen location. We found that cooking with either wood or agricultural crops was associated with greater odds of an early neonatal death. We also found that cooking with agricultural crops was associated with greater odds of stillbirth. Using polluting cooking fuels in an indoor kitchen location was strongly associated with stillbirth, which to our knowledge has not been previously identified.
Women exposed to polluting fuels for cooking were more likely to have a stillbirth in Bangladesh. Our findings for stillbirth are consistent with the direction and size of the effect with recent studies conducted in India, Kenya, Pakistan, and Zambia and the two systematic reviews, which found ORs ranging from 1.29 to 2.06 [9–12,16,17,25]. The “stillbirth” variable was calculated from the calendar data of the women’s data set from the BDHS [27], which has several limitations [28]. It only records one reproductive event in each month of the calendar, in the context of twin pregnancies, where one is a stillbirth and one is a live birth, then only the live birth is captured in the calendar data or if both twins are stillbirths, only one stillbirth is captured in the calendar data, which results in an under-count of the overall numbers of stillbirth; hence, we excluded all twins. There may also have been misclassification of cooking fuel exposure at the point of data collection or dilution of the effect when we dichotomised fuel into clean vs. polluting.
Examining the six types of polluting fuel in Bangladesh individually, we found that cooking with agricultural crops compared to clean fuels was associated with increased odds of stillbirth. This is a new and notable finding of our study and has not been previously reported. A few studies have linked exposure to wood fuel with stillbirth [9,10,25]; however, we did not find a strong relationship between use of wood fuel and stillbirth, although the odds of stillbirth were greater among the women using wood for cooking compared to the women using clean fuels. Also, a limited number of studies suggest an association between cooking with kerosene and increased risk of perinatal outcomes [10,24]; we could not assess the impact for kerosene separately, as in our analysis less than 1% women were using kerosene as their primary fuel. Previous studies have reported the combined effect of indoor kitchen location and type of cooking fuel [29,30], and our results concur with these findings for stillbirth. This result also suggests that household air pollution is not driven by ambient air pollution in this setting, which is important for developing interventions to decrease exposure and suggests that converting into clean fuels in the home may reduce household air exposure. As an aside, addition to polluting cooking fuel, maternal age at birth and birth order were also associated with stillbirth, which is consistent with prior research [31–33].
Early neonatal mortality was 1.46 times higher among the infants born to the mothers using polluting fuels than the mothers using clean fuels for cooking. This finding is consistent with a cohort study of pregnant women and their babies from five countries though the neonatal period was different to ours and was only up to 2 days post-partum [11]. Various other studies have estimated the relationship between use of polluting cooking fuels and neonatal death [24,26], but the association in terms of early neonatal mortality is unknown, and to our knowledge, our study is the first to investigate this time period. When we examined each type of polluting fuel, we found that exposure to both wood and agricultural crop waste increased the odds of early neonatal mortality. This effect of wood is consistent with the previous literature which examined the association of cooking fuel for other perinatal outcomes such as low birthweight, preterm birth, and stillbirth [9,10,13,25]. In contrast to stillbirth, the combined odds of indoor kitchen location and exposure to polluting fuels were only 1.19 and did not show any association for early neonatal mortality, suggesting that other factors are more important contributors to early neonatal mortality.
Strengths and limitations
The main strength of our study was that the data were based on a large nationally representative sample from four surveys, between the years 2004 and 2014. Furthermore, we were able to control for several known confounding factors. We also tried to examine different exposure combinations such as estimating the effect for each type of polluting fuel and combining the effect of fuel with kitchen location, which is novel.
We acknowledge several limitations of our study which should be taken into account when interpreting the results. The observed OR for stillbirth was small and could easily be impacted by residual confounding. Other important factors that are unmeasured in this data are likely to be contributors to stillbirths. Also, there are several important potential confounders that we were unable to include, such as antenatal care, place of delivery, obstetric history, and health facility-related factors in our analysis, as BDHS only collects information regarding these variables for live births. There may also be a possibility of overlapping the count of stillbirth and early neonatal death across the survey years, as we pooled four BDHS data sets. Exposure to polluting fuels for cooking was ascertained indirectly from the main type of fuel used for cooking rather than by direct measurement of household air pollution. Also, we could not consider the frequency of cooking and total time spent for cooking per day which will contribute to the actual exposure level, as this information is not reported by the BDHS. We were only able to consider the primary cooking fuel, and a substantial proportion of women may use more than one cooking fuel resulting in misclassification, although this is unlikely to be differential among the women who had a stillbirth or early neonatal death, as women are not aware of the association of fuel and pregnancy outcomes.
Conclusions
We found an association between exposure to polluting cooking fuels and early neonatal mortality. Exposure to agricultural crops for cooking was associated with stillbirth, and the combined effect of indoor kitchen location and exposure to polluting fuels was also associated with stillbirth. There is an important need to conduct a prospective study to thoroughly investigate the association between household air pollution from polluting cooking fuels and adverse perinatal outcomes.
Acknowledgements
This paper is a part of MKN’s PhD thesis. We are grateful to Sydney Medical School, The University of Sydney, for funding MKN’s PhD (Early Career Researcher Postgraduate Scholarship). We would like to thank MEASURE DHS and NIPORT for permitting us to analyse the BDHS 2004–2014 data sets. CRG is funded by the National Health and Medical Research Council, Career Development Fellowship #1087062.
Authors’ contributions
MKN, CRG, and AA conceptualised and designed the study. MKN performed the literature review and statistical analysis and drafted the manuscript. MKN and CRG contributed to the interpretation of the data. CRG and AA contributed to the critical revision of the manuscript. All the authors read and approved the final manuscript.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- [1]. Lim SS, Vos T, Flaxman AD, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2224–2260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2]. Fullerton DG, Bruce N, Gordon SB.. Indoor air pollution from biomass fuel smoke is a major health concern in the developing world. Trans R Soc Trop Med Hyg. 2008;102(9):843–851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3]. Burden of disease from household air pollution for 2012 . 2015 May12; Available from: http://www.who.int/phe/health_topics/outdoorair/databases/HAP_BoD_results_March2014.pdf?ua=1.
- [4]. Bruce N, Perez-Padilla R, Albalak R. Indoor air pollution in developing countries: a major environmental and public health challenge. Bull World Health Organ. 2000;78(9):1078–1092. [PMC free article] [PubMed] [Google Scholar]
- [5]. Bonjour S, Adair-Rohani H, Wolf J, et al. Solid fuel use for household cooking: country and regional estimates for 1980–2010. Environ Health Perspect. 2013;121(7):784–790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].World Health Organization. Indoor air pollution from solid fuels and risk of low birth weight and stillbirth: report from a symposium held at the Annual Conference of the International Society for Environmental Epidemiology (ISEE), September 2005, Johannesburg. 2007. [Google Scholar]
- [7]. Ezzati M, Kammen MB. DM, Comparison of emissions and residential exposure from traditional and improved cookstoves in Kenya . Environ Sci Technol. 2000;34(4):578–583. [Google Scholar]
- [8]. Tielsch JM, Katz J, Thulasiraj RD, et al. Exposure to indoor biomass fuel and tobacco smoke and risk of adverse reproductive outcomes, mortality, respiratory morbidity and growth among newborn infants in south India. Int J Epidemiol. 2009;38(5):1351–1363. [DOI] [PubMed] [Google Scholar]
- [9]. Mishra V, Retherford RD, Smith KR. Cooking smoke and tobacco smoke as risk factors for stillbirth. Int J Environ Health Res. 2005;15(6):397–410. [DOI] [PubMed] [Google Scholar]
- [10]. Lakshmi PVM, Virdi NK, Sharma A, et al. Household air pollution and stillbirths in India: analysis of the DLHS-II National Survey. Environ Res. 2013;121:17–22. [DOI] [PubMed] [Google Scholar]
- [11]. Patel AB, Meleth S, Pasha O, et al. Impact of exposure to cooking fuels on stillbirths, perinatal, very early and late neonatal mortality – a multicenter prospective cohort study in rural communities in India, Pakistan, Kenya, Zambia and Guatemala. Matern Health, Neonatal Perinatology. 2015;1(1):18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12]. Pope DP, Mishra V, Thompson L, et al. Risk of low birth weight and stillbirth associated with indoor air pollution from solid fuel use in developing countries. Epidemiol Rev. 2010;32(1):70–81. [DOI] [PubMed] [Google Scholar]
- [13]. Boy E, Bruce N, Delgado H. Birth weight and exposure to kitchen wood smoke during pregnancy in rural Guatemala. Environ Health Perspect. 2002;110(1):109–114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14]. Mishra V, Dai X, Smith KR, et al. Maternal exposure to biomass smoke and reduced birth weight in Zimbabwe. Ann Epidemiol. 2004;14(10):740–747. [DOI] [PubMed] [Google Scholar]
- [15]. Kadam Y, Mimansa A, Chavan P, et al. Effect of prenatal exposure to kitchen fuel on birth weight. Indian J Community Med. 2013;38(4):212–216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16]. Mavalankar DV, Trivedi CR, Gray RH. Levels and risk factors for perinatal mortality in Ahmedabad, India. Bull World Health Organ. 1991;69(4):435–442. [PMC free article] [PubMed] [Google Scholar]
- [17]. Amegah AK, Quansah R, Jaakkola JJK. Household air pollution from solid fuel use and risk of adverse pregnancy outcomes: a systematic review and meta-analysis of the empirical evidence. PLoS One. 2014;9(12):e113920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18]. Siddiqui A, Gold E, Brown K, et al. Preliminary analyses of indoor air pollution and low birth weight (LBW) in Southern Pakistan . in Indoor air pollution from solid fuels and risk of low birth weight and stillbirth Report from a symposium held at the Annual Conference of the International Society for Environmental Epidemiology (ISEE): 2005 ; Johannesburg, South Africa 2005. [Google Scholar]
- [19]. Lawn JE, Blencowe H, Pattinson R, et al. Stillbirths: where? when? why? how to make the data count? The Lancet. 2011; 377(9775):1448–1463. [DOI] [PubMed] [Google Scholar]
- [20]. Blencowe H, Cousens S, Jassir FB, et al. National, regional, and worldwide estimates of stillbirth rates in 2015, with trends from 2000: a systematic analysis. The Lancet Global Health. 2016; 4(2):e98–e108. [DOI] [PubMed] [Google Scholar]
- [21]. National Institute of Population Research and Training (NIPORT), M.a.A., and ICF international, Bangladesh Demographic and Health Survey 2014. 2016, NIPORT, Mitra and Associates, and ICF International: Dhaka, Bangladesh, and Rockville, Maryland, USA. [Google Scholar]
- [22]. Dasgupta S, Huq M, Khaliquzzaman M, et al. Who suffers from indoor air pollution? Evidence from Bangladesh. Health Policy Plan. 2006;21(6):444–458. [DOI] [PubMed] [Google Scholar]
- [23]. World Health Organization Maternal and perinatal health. Maternal, newborn, child and adolescent health; [Cited 2017 Mar 03] Available from: http://www.who.int/maternal_child_adolescent/topics/maternal/maternal_perinatal/en/.
- [24]. Epstein MB, Bates MN, Arora NK, et al. Household fuels, low birth weight, and neonatal death in India: the separate impacts of biomass, kerosene, and coal. Int J Hyg Environ Health. 2013;216(5):523–532. [DOI] [PubMed] [Google Scholar]
- [25]. Wylie BJ, Coull BA, Hamer DH, et al. Impact of biomass fuels on pregnancy outcomes in central East India. Environ Health. 2014;13(1):1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26]. Naz S, Page A, Agho KE. Household air pollution and under-five mortality in Bangladesh (2004–2011). Int J Environ Res Public Health. 2015;12(10):12847–12862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27]. Rutstein SO, Rojas G. Guide to DHS statistics. Calverton, MD: ORC Macro; 2006. [Google Scholar]
- [28]. Christou A, Dibley MJ, Raynes-Greenow C. Beyond counting stillbirths to understanding their determinants in low- and middle-income countries: a systematic assessment of stillbirth data availability in household surveys. Trop Med Int Health. 2017;22(3):294–311. [DOI] [PubMed] [Google Scholar]
- [29]. Dasgupta S, Huq M, Khaliquzzaman M, et al. Indoor air quality for poor families: new evidence from Bangladesh. Indoor Air. 2006;16(6):426–444. [DOI] [PubMed] [Google Scholar]
- [30]. Rehfuess E.A., et al. Solid fuel use and cooking practices as a major risk factor for ALRI mortality among African children. J Epidemiol Community Health. 2009;63(11):887. [DOI] [PubMed] [Google Scholar]
- [31]. Gardosi J, Madurasinghe V, Williams M, et al. Maternal and fetal risk factors for stillbirth: population based study. BMJ: Br Med J. 2013;346: [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32]. Nahar S, Rahman A, Nasreen HE. Factors influencing stillbirth in Bangladesh: a case-control study. Paediatr Perinat Epidemiol. 2013;27(2):158–164. [DOI] [PubMed] [Google Scholar]
- [33]. KC A, Wrammert J, Ewald U, et al. Incidence of intrapartum stillbirth and associated risk factors in tertiary care setting of Nepal: a case-control study. Reprod Health. 2016;13(1):103. [DOI] [PMC free article] [PubMed] [Google Scholar]


