Abstract
OBJECTIVES
To explore the extent to which patients identify community pharmacists as healthcare providers and the relationship of this perception to a willingness to engage in pharmacist-provided services.
METHODS
A cross-sectional survey was conducted at a retail pharmacy and a patient centered medical home (PCMH) in the New Orleans, Louisiana metropolitan area. The survey assessed patients’ perception of community pharmacists and their roles in the provision of healthcare, as well as willingness to participate in commonly offered pharmacist-provided services.
RESULTS
This study included 49 participants who interacted with pharmacy personnel to receive prescriptions regularly. Of the 49 patients surveyed, 91.8% perceived community pharmacists to be healthcare providers and this perception significantly impacted patient willingness to participate in medication therapy management, medication optimization, and travel vaccination services. Other services were not significantly impacted by perception.
CONCLUSION
A greater percentage of patients perceived community pharmacists as healthcare providers. This affirmative perception positively impacted patient willingness to participate in several pharmacist-provided services. Since no comparative studies are available, further study is needed to assess consistency of observations and assess innovative ways to highlight pharmacists’ cognitive attributes and increase participation in pharmacist-provided services.
Keywords: Pharmacist, Provider status, healthcare provider, community pharmacy, pharmacy services
Background
There is no universally accepted definition as to what constitutes a healthcare provider. Although the United States Bureau of Labor and Statistics lists pharmacists under the same category as many other healthcare professionals including physicians and chiropractors,1, federal regulations do not name pharmacists as providers within Medicare. Pharmacists are currently seeking to be recognized as healthcare providers via the proposed Pharmacy and Medically Underserved Enhancement Act (H.R. 592/S. 109). This bill would amend title XVIII of the Social Security Act, to provide coverage under the Medicare program for pharmacist services within medically underserved areas2. Several states, including California, Washington, and Oregon have recently passed pharmacist provider status legislation. This pilot study explored patients’ perception of community pharmacists as healthcare providers and how this perception impacted their willingness to participate in pharmacist-provided services.
Methods
A dual-center, cross-sectional study was conducted between January 12, 2016 and February 10, 2016. After approval by the Institutional Review Board of Xavier University of Louisiana, participants were encountered at a community/retail pharmacy or a patient-centered medical home (PCMH) located in the greater New Orleans area. Patients were recruited via convenience sampling at the two practice sites of the researchers. At the sites, patients were randomly approached by two trained pharmacists and were screened to determine and eligibility. Eligible and consented patients were enrolled in the study and were administered a 36-item survey. Eligible participants were aged 18 years or older, filled at least one prescription every 90 days, and personally picked up their prescriptions from community pharmacies.
The survey instrument was developed based on an adaptation of a survey instrument3, then tested for clarity on a sample of 15 members of the general public. Multiple choice and two open-ended questions captured demographic information, medical information, perception of community pharmacists and willingness to participate in pharmacist-provided services. The primary outcome measure was willingness of patients to participate in pharmacist-provided services. The willingness measure (index) was derived by summing the 10 willingness items. For each item a response of “willing” was assigned a value of 1, “somewhat willing” was assigned a value of 2 and “unwilling” was assigned a value of 3. Hence, a total willingness score was derived from the 10 willingness items. This approach to deriving a total willingness score is not unique to this study4. A lower total score of the willingness measure implied willingness of study participants to participate in pharmacist-provided services. The primary exposure (independent) variable was perception of participants as to whether or not pharmacists are healthcare providers (responses of “Yes” coded 1 and “No” coded 0).
Two-Sample T-Tests were used to test difference in the individual and collective measures of patients’ and willingness to participate in various pharmacist-provided services based on the perception of whether or not pharmacists are healthcare providers. The derivation of the total willingness score and the use of T-test as opposed to the non-parametric are supported by the paper by Sullivan and Artino4. SAS (v9.4) was used to perform all statistical analyses and all inferential statistics were performed at a significance level of 5% (p < 0.05).
Results
Of the 138 patients approached for participation from both locations, 75 refused participation and 63 were screened. Of the 63 patients screened, 14 participants were excluded due to not filling at least one prescription every 90 days. The remaining 49 (39 community and 10 PCMH) that met eligibility criteria and consented were enrolled into the study. The greater percentage of the 49 respondents visited the pharmacy one to three times every 30 days, were 55 years of age or older and female (Table 1).
Table 1.
Characteristics of Study Sample
| Characteristics | Statistic |
|---|---|
| Age in years, n (%) | 49 (100.0) |
| 18–25 | 2 (4.0) |
| 26–35 | 6(12.2) |
| 36–44 | 9 (18.4) |
| 45–54 | 7 (14.3) |
| 55–64 | 12 (24.5) |
| ≥ 65 | 13 (26.5) |
| Gender, n (%) | 49 (100.0) |
| Male | 14 (28.6) |
| Female | 35 (71.4) |
| Race/Ethnicity, n (%) | 49 (100.0) |
| African American | 28 (57.1) |
| Caucasian | 17 (34.7) |
| Hispanic/Latino | 2 (4.1) |
| Other | 2 (4.1) |
| Educational Attainment, n (%) | 49 (100.0) |
| Grade School | 12 (24.5) |
| High School/GED | 9 (18.4) |
| Some College/Technical School | 14 (28.6) |
| Bachelor’s Degree | 7 (14.3) |
| Master’s Degree | 4 (8.2) |
| Doctorate/Professional Degree | 2 (4.1) |
| Income | 49 (100.0) |
| < $25,000 | 14 (28.6) |
| $25,000 – $34,999 | 5 (10.2) |
| $35,000 – $49,999 | 4 (8.2) |
| $50,000 – $74,999 | 5 (10.4) |
| $75,000 – $99,9999 | 0 (0.0) |
| ≥ $100,000 | 4 (8.2) |
| Unknown (prefer not to answer) | 17 (34.7) |
| History of Employment with the Healthcare Industry | 49 (100.0) |
| Yes | 18 (36.7) |
| No | 31 (63.3) |
| Health Status | Statistic |
| Asthma Prevalence (%) | 18.4 |
| Diabetes Prevalence (%) | 20.4 |
| Hypertension Prevalence (%) | 55.1 |
| Hypercholesterolemia Prevalence (%) | 36.7 |
| Overweight/Obesity Prevalence (%) | 16.3 |
| Smoking Status, n (%) | 49 (100.0) |
| Never Smoker | 28 (57.1) |
| Former Smoker | 8 (16.3) |
| Current Smoker | 13 (26.5) |
| Fill Prescription at (Study Performance Site), Yes; n (%) | 34 (69.4) |
| Average Number of Visits to the Pharmacy to Receive Prescription Medication, n (%) | 49 (100.0) |
| 1–2 Times in 90 Days | 14 (28.6) |
| 1–3 Times in 30 Days | 26 (53.1) |
| ≥ 4 Times in 30 Days | 9 (18.4) |
| Average Number of Prescriptions Received, n (%) | 49 (100.0) |
| 1–2 Prescriptions in 90 Days | 12 (24.5) |
| 1–3 Prescriptions in 30 Days | 20 (40.8) |
| ≥ 4 Prescriptions in 30 Days | 17 (34.7) |
| Ever Heard of Medication Therapy Management (MTM), yes; n (%) | 10(20.4) |
| Ever Seen a Pharmacist for any of the Following (All Applicable):* | |
| MTM – Medication Review Session, n (%) | 4 (8.2) |
| Prescription Consultation/Questions | 17 (34.7) |
| Fill Prescriptions | 49 (100.0) |
| Immunizations (e.g. Flu shot, pneumonia) | 20 (40.8) |
| Diabetes Education | 1 (2.0) |
| Over-The-Counter Recommendations/Questions | 27 (55.1) |
| Health Insurance Information | 8 (16.3) |
Note:
Responses are not mutually exclusive;
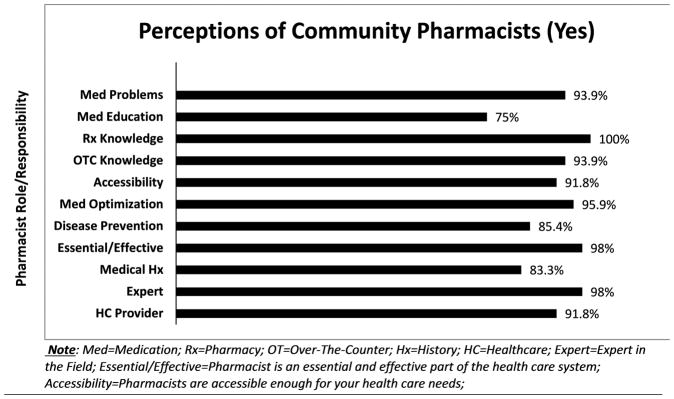
Figure 1 depicts the distributions of the various elements of perception of pharmacists being healthcare providers and performing a number of healthcare-related activities. Of the 10 elements, the lowest rate was 75% (Medication education- providing education on medical conditions) and the highest rate was 100% (pharmacy knowledge – providing education on medications). Seven out of 10 of the elements had a rate between 90% and 98%. Importantly, 91.8% of the target population perceived community pharmacists as healthcare providers.
Figure 1.
Table 2 provides a summary of the test of difference in willingness of the population to participate in pharmacist-provided services based on the perception of pharmacists are healthcare providers. Three of the 10 willingness measures showed significant differences based on perception: Medication Therapy Management (1.42±0.72 vs. 2.50±1.00; p=0.01); Medication Optimization (1.09±0.36 vs. 1.50±0.58; p=0.04); and Travel Vaccination consultation (1.11±0.32 vs. 1.50±0.58; p=0.03). Given the small sample sizes of the two groups, a non-parametric test (Wilcoxon-Mann-Whitney U Test) was performed to validate the findings with the T-test and the findings by the two methods were consistent. Data from the Wilcoxon-Mann-Whitney U Test is not presented.
Table 2.
Willingness to participate in pharmacist-provided services by perception of pharmacists as healthcare providers among study participants
| Willingness Measure | Mean ± SD | Mean ± SD | P-value |
|---|---|---|---|
| Medication Therapy Management (MTM) | 1.42±0.72 | 2.5±1.00 | 0.0078 |
| Immunization/Vaccination | 1.58±0.89 | 2.00±0.82 | 0.3662 |
| Blood Pressure Screening | 1.13±0.46 | 1.00±0.00 | 0.0568 |
| Blood Glucose Screening | 1.36±0.74 | 1.25±0.50 | 0.7830 |
| Cholesterol Screening | 1.29±1.09 | 1.25±0.50 | 0.9095 |
| Medication Optimization | 1.09±0.36 | 1.50±0.58 | 0.0415 |
| Life-style Coaching | 1.24±1.07 | 1.50±0.58 | 0.3952 |
| Counsel on Travel Vaccination | 1.11±0.32 | 1.50±0.58 | 0.0335 |
| Counsel on Travel Health | 1.09±0.29 | 1.50±0.58 | 0.2500 |
Discussion
The majority of patients perceived community pharmacists as healthcare providers. This outcome is congruent with the Bureau of Labor and Statistics, classifying pharmacists among extensively educated health professions, but in opposition of Medicare regulations. Although this study is limited due to geographical area and sample size, our results are consistent with a 2013 American Pharmacist Association (APhA) finding that most respondents perceive pharmacists to be healthcare providers5. Despite the fact that expectations of pharmacists have traditionally been product-based3, none of the open-ended responses indicated pharmacists’ dispensing of medications as reasoning for classification as a healthcare provider. Respondents consistently pointed to cognitive attributes: medication knowledge and informative capacities.
Over 90% of patients responded affirmatively to all except three of the questions regarding perception of community pharmacists. These less favorable areas of pharmacist role (contributions to disease prevention and capability to educate on medical conditions) indicate an imbalance between patient perception and the value of pharmacists’ services. Unfortunately these findings, like the findings of Reid et al., remind us that patients may not link pharmaceutical care services to improved outcomes6. These responses indicate a core challenge to advancing the provision of clinical and cognitive services, as these services may require confidence in pharmacist capabilities, expertise, and overall health impact to be successful.
A low awareness for pharmacist-provided services was observed, particularly medication therapy management. Troung et al. noted similar results, finding that most of the study participants encountered in community pharmacies were not aware of MTM and had never participated in a medication therapy review7. The impact of MTM services on decreasing healthcare costs and improving outcomes is well documented8, 9. However, if eligibility from third party payers remains narrow, the substance and value of MTM services cannot be realized by the general population.
In 1999, Blake et al. found most patients to be uncomfortable with the idea community pharmacists providing immunizations10. Today community pharmacists are the second leading provider of adult flu vaccinations, a service that continues to grow11. If vaccinations in the community setting are any indication, then the utilization pharmacist-provided services will increase as well.
Conclusion
This pilot study found that a greater percentage of study participants currently view community pharmacists as healthcare providers; this affirmative perception positively impacts patients’ willingness to participate in pharmacist-provided services such as MTM, medication optimization and travel vaccination consultations. Additional larger scale studies are needed to establish a consistent outcome and determine best practices to increase awareness of and participation in pharmacist-provided services.
Acknowledgments
Funding Source: This research was supported partially by the Grant, 5 S21 MD 000100-12, from the National Institute on Minority Health and Health Disparities (NIMHD), National Institutes of Health (NIH), Department of Health and Human Services (DHHS); U54 GM104940 from the National Institute of General Medicine Sciences (NIGMS) of NIH; and D34HP00006-28-0 from Health Resource and Service Administration of DHHS.
This research was supported partially by the Grant, 5 S21 MD 000100-12, from the National Institute on Minority Health and Health Disparities (NIMHD), National Institutes of Health (NIH), Department of Health and Human Services (DHHS); U54 GM104940 from the National Institute of General Medicine Sciences (NIGMS) of NIH; and D34HP00006-28-0 from Health Resource and Service Administration of DHHS. The findings and conclusions in this report are those of the authors and do not necessarily represent the views of the NIH, NIMHD, NIGMS, HRSA or DHHS.
Footnotes
Disclosure Statement: The authors have nothing to disclose.
Declarations
Conflict of Interests
The Author(s) declare(s) that they have no conflicts of interest to disclose.
Contributor Information
Vincent Ekenga, Clinical Assistant Professor, Xavier University of Louisiana College of Pharmacy.
Janel Bailey-Wheeler, Clinical Assistant Professor, Xavier University of Louisiana College of Pharmacy, 1 Drexel Drive, New Orleans LA 70125, (504)520-5369, (504)520-7971.
Tammy Hart, Clinical Assistant Professor, Xavier University of Louisiana College of Pharmacy, 1 Drexel Drive, New Orleans LA 70125, (504)520-5347, (504)520-7971.
Daniel Sarpong, Professor, Xavier University of Louisiana College of Pharmacy, 1 Drexel Drive, New Orleans LA 70125, (504)520-7424, (504)520-7971.
Martha Earls, Clinical Assistant Professor, Xavier University of Louisiana College of Pharmacy, 1 Drexel Drive, New Orleans LA 70125, (504)520-5351, (504)520-7971.
References
- 1.Standard Occupational Classification. U.S. Bureau of Labor Statistics; 2017. Sep 27, [Accessed: 2017-09-27]. URL: http://www.bls.gov/soc/2010/soc290000.htm#29-1000. (Archived by WebCite® at http://www.webcitation.org/6tnP35VkI) [Google Scholar]
- 2.Harper PC. Pharmacist provider status legislation: Projections and prospects. Journal of the American Pharmacists Association. 2015;55(2):203–7. doi: 10.1331/JAPhA.2015.14176. [DOI] [PubMed] [Google Scholar]
- 3.Law AV, Qkamoto MP, Brock K. Perceptions of Medicare Part D enrollees about pharmacists and their role as providers of medication therapy management. Journal of the American Pharmacists Association. 2008;48(5):648–53. doi: 10.1331/JAPhA.2008.07084. [DOI] [PubMed] [Google Scholar]
- 4.Sullivan GM, Artino AR. Analyzing and Interpreting Data From Likert-Type Scales. Journal of Graduate Medical Education. 2013;5(4):541–542. doi: 10.4300/JGME-5-4-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.McDonough Randy. How are you perceived by patients and the general public? American Pharmacists Association; 2017. Sep 27, [Accessed: 2017-09-27]. URL: https://www.pharmacist.com/how-are-you-perceived-patients-and-general-public. (Archived by WebCite® at http://www.webcitation.org/6tnOe7BwF) [Google Scholar]
- 6.Ried, Douglas L, et al. Patients’ satisfaction and their perception of the pharmacist. Journal of the American Pharmacists Association. 1999;39(6):835–842. [PubMed] [Google Scholar]
- 7.Truong, Hoai-An, et al. Perceptions of patients on Medicare Part D medication therapy management services. Journal of the American Pharmacists Association. 2009;49(3):392–398. doi: 10.1331/JAPhA.2009.08008. [DOI] [PubMed] [Google Scholar]
- 8.Cranor CW, Christensen DB. The Asheville Project: Short-term outcomes of a community pharmacy diabetes care program. Journal of the American Pharmacists Association. 2012;52(6):838–50. doi: 10.1331/JAPhA.2012.12542. [DOI] [PubMed] [Google Scholar]
- 9.Bunting BA, Smith BH, Sutherland SE. The Asheville Project: Clinical and economic outcomes of a community-based long-term medication therapy management program for hypertension and dyslipidemia. Journal of the American Pharmacists Association. 2008;48(1):23–31. doi: 10.1331/JAPhA.2008.07140. [DOI] [PubMed] [Google Scholar]
- 10.Blake EW, Blair MM, Couchenour RL. Perceptions of Pharmacists as Providers of Immunizations for Adult Patients. Pharmacotherapy. 2003;23(2):248–54. doi: 10.1592/phco.23.2.248.32083. [DOI] [PubMed] [Google Scholar]
- 11.Centers for Disease Control and Prevention. National Early-Season Flu Vaccination Coverage, United States, November 2016. U.S. Department of Health and Human Services; 2017. Sep 27, [Accessed: 2017-09-27]. URL: https://www.cdc.gov/flu/fluvaxview/nifs-estimates-nov2016.htm. (Archived by WebCite® at http://www.webcitation.org/6tnPcy90g) [Google Scholar]