Abstract
Introduction
Unsafe abortion past the first trimester disproportionately accounts for the majority of global abortion-related morbidity and mortality; research that documents the safety, feasibility and acceptability of existing models for providing information and support to women who self-manage outside of formal clinic settings is needed.
Methods
This study is a retrospective analysis of anonymised electronic client records from callers to a safe abortion hotline in Indonesia. Between July 2012 and October 2016, a total of 96 women contacted the hotline for information on medication abortion beyond 12 weeks' gestation and are included in this study. Descriptive statistics were calculated regarding pregnancy termination status, client experience with warning signs of potential complications, and medical care seeking and treatment.
Results
Ninety-six women with pregnancies beyond the first trimester called the hotline for information on medication abortion; 91 women received counselling support from the hotline. Eighty-three women (91.2%) successfully terminated their pregnancies using medication and did not seek medical care. Five women exhibited warning signs of potential complications and sought medical care; one woman sought care after a failed abortion. Two women were lost to follow-up and the outcomes of their pregnancies are unknown.
Conclusions
Evidence from our analysis suggests that a model of remote provision of support for abortions later in pregnancy by non-medically trained, skilled abortion counsellors could be a safe alternative for women in need of abortions beyond 12 weeks' gestation in a legally restrictive context. Further examination and documentation of the model is warranted.
Keywords: safe abortion, self-managed abortion, self-induced abortion, accompaniment, safe abortion hotlines, second-trimester abortions, medication abortion
Key messages.
Women face many barriers to safe abortion care, especially later in pregnancy.
Research documenting the safety of out-of-clinic models of medication abortion provision before and after 12 weeks gestation is needed.
This analysis demonstrates that out-of-clinic models could be a safe alternative for women in need of abortions beyond 12 weeks gestation in legally restrictive contexts.
Introduction
Even where abortion is legal, structural and institutional barriers can delay women from accessing abortion care.1–3 Research has demonstrated that young women, poor women, unmarried women, and women who live further from abortion providers have heightened risk for experiencing delays in accessing abortion care such as later pregnancy recognition, difficulty deciding, fear of judgement, lack of autonomy, and difficulty paying for and travelling to abortion services.1 2 4–7 In settings where abortion is legally restricted or illegal, such delays are compounded by the lack of legal and/or safe options, often pushing women later into pregnancy before they obtain care. While only a small proportion of all abortions occur in the second trimester,8 access to safe abortion beyond the first trimester is an integral component of comprehensive reproductive healthcare.
Globally, the use of medications for abortion outside of formal health systems is on the rise.9 10 Increasingly, data from around the world suggest that women who use misoprostol to self-manage abortions can do so safely and effectively.11–13 In light of this evidence, women’s health advocates have utilised a harm-reduction model to combat mortality and morbidity from unsafe abortion by providing women with counselling and information about early medication abortion (<12 weeks' gestation) through websites, hotlines, and social media platforms.14 15 For women in restrictive settings who need services later in pregnancy, however, equivalent safe options are limited or non-existent; as a result, unsafe abortion past the first trimester disproportionately accounts for the majority of global abortion-related morbidity and mortality.8 Because medications for abortion are safe and effective in the second trimester, and are among WHO recommended methods for later abortion,16 17, some hotlines and organisations in restrictive settings have begun to provide counselling and accompaniment services beyond the first trimester for women who do not have a safe legal option.18 In these contexts, accompaniment services include providing support for women along every step of their abortion process, including but not limited to texts and calls to check in during the process, reminders, emotional support and follow-up.
WHO guidelines aimed at expanding the cadres of abortion providers do not include task-shifting recommendations for medication abortion beyond the first trimester due to lack of evidence.19 Given the barriers that women face in obtaining safe abortions in restrictive settings and the risks that accompany unsafe abortion later in pregnancy, there is a compelling need for research that documents the safety, feasibility and acceptability of existing models that expand the cadres of providers for abortion after 12 weeks gestation, including those providing information and support to women who self-manage second trimester abortions outside of formal clinic settings. This article presents an analysis of electronic client records from a safe abortion hotline in Indonesia that provides information and accompaniment services to women seeking abortion beyond the first trimester.
Methods
Data for this analysis come from electronic client records from a safe abortion hotline in Indonesia, where abortion is permitted only when a woman’s life is at risk, or in cases of rape or fetal anomaly. All records were anonymised prior to the hotline granting researchers access to them, and no personal identifying information was contained in any of the records. Ninety-six women contacted the hotline between July 2012 and October 2016 seeking information on medication abortion beyond 12 weeks' gestation and are included in this study. Ethical approval for this study was obtained from Allendale Investigational Review Board.
The hotline provides abortion counselling and accompaniment services up until 22 weeks' gestation, and employs current evidence-based guidelines for medication abortion for pregnancies above 12 weeks' gestation: 200 mg mifepristone administered orally, followed after 12 to 48 hours by 400 µg oral misoprostol, followed by 400 µ g sublingual misoprostol every 3 hours up to a maximum of five doses.17 20 In instances where women are unable to procure mifepristone, the hotline also employs misoprostol only-regimens. None of the hotline counsellors are clinically trained, but all have undergone intensive training in medication abortion protocols and abortion counselling.
All women calling the hotline to request information about medication abortion receive standardised and compassionate pre-abortion counselling about the process and what to expect. Gestational age of the caller is ascertained by last menstrual period (LMP) or independently obtained ultrasound results as reported to the hotline by the caller. To ensure women have access to reliable and effective medications, those who are not already in possession of medications are connected with an in-country organisation that can send a package with the required dosage of mifepristone and misoprostol through the mail. Once women confirm they have reliable medications in hand, they are instructed to call their hotline counsellor to begin an intensive, gestation-specific counselling session in preparation for the abortion. The counselling session covers the following topics: how the drugs function, how to manage pain, what the products of conception will look like, management of products of conception, how to manage retained products of conception, how to recognise complication signs, potential interactions with medical personnel in case of emergency treatment seeking, how to confirm abortion completion, what to expect after the abortion, management of emotions, and prevention of future unwanted pregnancy.
Once the initial counselling session is complete, women are asked to contact their counsellor by phone or text to record the time of oral administration of mifepristone, and the time of all subsequent sublingual administrations of misoprostol. Women are also asked to record the following information in a written diary: timing and description of any side effects experienced, potential warning signs of complications, timing and reported severity of cramping, timing of bleeding, descriptions of expelled products of conception, and additional medications taken for pain management, nausea or other symptoms. Women are in close touch with their counsellor throughout the abortion process and communicate the contents of the diary with their counsellor during regular phone calls. During each communication, the counsellor inputs relayed information about the abortion process into the hotline’s electronic record system. Counsellors follow-up with women for a period of 3 weeks after the start of their abortion to monitor completion and potential warning signs of complications.
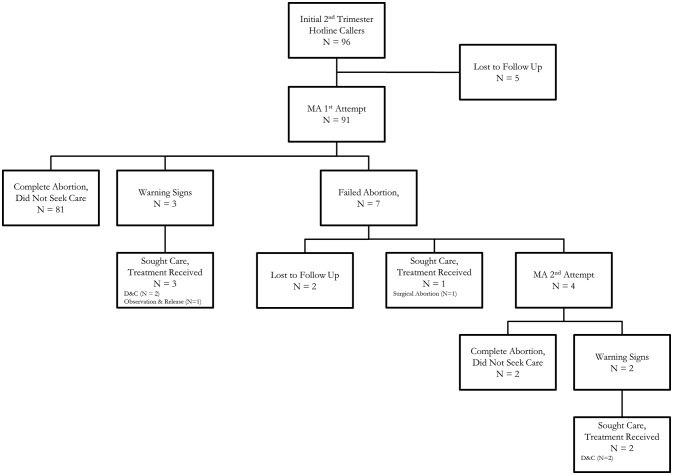
Variables were developed in keeping with protocols implemented by the hotline. In figure 1, an initial second-trimester hotline caller is defined as anyone calling the hotline seeking information about accompaniment services for second-trimester abortion. A second-trimester medication abortion client is any woman who contacted the hotline beyond 12 weeks' gestation who participates in the initial counselling session. Medication abortion attempts are classified as 1st medication abortion attempts the first time a client administers abortion medications and 2nd medication abortion attempts if, after the client has followed evidence-based protocols,17 20 the medications did not produce their intended effect and, together with their hotline counsellor, the client decides to administer a second dose of 200 mg oral mifepristone followed by 400 µg oral misoprostol and up to five doses of 400 µg sublingual misoprostol. An abortion is characterised as a failed abortion if the abortion medications did not produce their desired effect (no expulsion of the products of conception within 24 hours after the first misoprostol dose). An abortion is characterised as a complete abortion if both the client and the counsellor reported that the placenta has been expelled, the woman is in a stable condition, and the pregnancy has been successfully terminated using abortion medications. A client is categorised as having sought care if, for any reason during the medication abortion process, she decides to seek medical care in a formal health facility. Any medical care directly related to the medication abortion obtained by a medication abortion client at a formal health facility is categorised as treatment received. In the absence of clinical records to assess abortion-related complications, the hotline relies on women’s self-report of symptoms experienced that require extra monitoring and might indicate the need to seek medical care in a formal health facility. Warning signs of a potential complications include heavy bleeding, defined as soaking more than two sanitary pads per hour for more than 2 hours; high fever, defined as a recorded temperature over 38°C for more than 24 hours; and severe pain, defined as pain that inhibits normal activities and is not alleviated by over-the-counter painkillers.
Figure 1.
Second-trimester medication abortion (MA) hotline callers, July 2012 – October 2016.
Descriptive statistics were calculated using Stata Release 14.21
Patient and public involvement
The development of the research question and key outcomes was informed by previous collaborations with our hotline partner and ongoing conversations about the importance of building an evidence base to document the safety of out-of-clinic abortions, with an emphasis on documenting women’s experiences. As this article presents a secondary analysis of retrospective anonymised electronic client records from the safe abortion hotline, safe abortion hotline clients were not involved in the design, recruitment or implementation of the study.
Results
Ninety-six women with pregnancies beyond the first trimester contacted the hotline during the study period for information on medication abortion. Callers reported gestational ages ranging from 13 to 22 (mean 15.6) weeks. After receiving pre-abortion counselling from the hotline, five of the 96 initial callers did not contact the hotline again, and hotline staff were neither able to confirm receipt of medications nor provide further support through the medication abortion process (figure 1). These women are considered lost-to-follow-up, and both the status of their medication abortion attempts and the outcomes of their pregnancies are unknown.
Ninety-one women received telephone support from trained safe abortion hotline counsellors throughout their abortion process, with gestational ages ranging from 13 to 22 (mean 15.6) weeks; 47 women (50.6%) had gestational ages of 13 or 14 weeks (table 1, online figure 2, supplementary file). Overall, 83 out of the 91 women who managed their own abortions beyond the first trimester with telephone support from trained safe abortion hotline counsellors successfully terminated their pregnancies using medication abortion (91.2%). Six callers sought medical care during their medication abortion process (6.6%); these callers all successfully terminated pregnancies after seeking additional care.
Table 1.
Abortion characteristics for hotline clients seeking second-trimester medication abortion (2012–2016) (n=91)
| Characteristics | % (n) |
| Gestational age (weeks) (mean (SD)) | 15.6 (2.5) |
| Complete abortion by first MA attempt without medical care | 89.0 (81.0) |
| Complete abortion by second MA attempt without medical care | 91.2 (83.0) |
| Sought medical care | 6.6 (6.0) |
| Terminated pregnancy* | 97.8 (89.0) |
*Two callers were lost to follow-up after a failed abortion on their first attempt; the outcome of their pregnancy is unknown.
MA, medication abortion.
bmjsrh-2018-200102supp001.jpg (257.4KB, jpg)
Eighty-one women had a complete abortion using medications on their first attempt (89.0%) and did not seek medical care. Three women experienced heavy bleeding after their first attempt, a warning sign of a potential complication, and sought medical care. Two of these women underwent dilation and curettage (D&C), one was observed at the hospital and not treated.
For seven women, their first attempt at self-managing a second- trimester medication abortion with support from the hotline resulted in a failed abortion (the medications had no effect). Four of these women pursued a second attempt at self managing a second trimester medication abortion with the support from hotline; two of these women had a complete abortion and did not seek medical care, while two sought medical care for heavy bleeding (figure 1, table 2). Both women who sought care after a second medication abortion attempt underwent D&C when they sought care. Two women with a failed abortion after their first attempt were lost to follow-up, and the outcomes of their pregnancies are unknown. One woman sought medical care and obtained a surgical abortion after her first medication abortion attempt.
Table 2.
Abortion trajectories of second-trimester medication abortion MA clients with failed abortion after first attempt (2012–2016) (n=7)
| Client | Gestational age (weeks) | Medications used | Abortion trajectory |
| 1 | 14 | Mifepristone and misoprostol (M&M) | Complete abortion on second MA attempt (M&M) |
| 2 | 13 | M&M | Complete abortion on second MA attempt (M&M) |
| 3 | 13 | Misoprostol alone | Lost to Follow-up |
| 4 | 14 | Misoprostol alone | Lost to Follow-up |
| 5 | 14 | Misoprostol alone | Surgical Abortion |
| 6 | 14 | Misoprostol alone | Received D&C after second MA attempt (misoprostol alone) |
| 7 | 13 | Misoprostol alone | Received D&C after second MA attempt (M&M) |
MA, medication abortion.
Characteristics of clients’ final abortion attempt are presented in table 3. Most clients (82.4%) used mifepristone and misoprostol in combination to terminate their pregnancies; 16 women (17.6%) used misoprostol alone. Complete data on the timing of medication administration is missing for 28 women. Out of the 47 women who used the combined mifepristone and misoprostol regime and reported the timing of medication administration to their counsellor, 45 women adhered to the evidence-based guidelines17 20 and took the first dose of misoprostol within 12 to 48 hours of taking mifepristone. The two clients who reported timing of medication administration outside of the evidence-based guidelines took the first dose of misoprostol 60 hours after taking mifepristone; recorded gestational ages of these clients were 17 and 19 weeks respectively, and both clients successfully completed abortions without seeking medical care.
Table 3.
Abortion characteristics of final abortion attempt for hotline clients seeking second-trimester medication abortion (2012–2016) (n=91)
| Characteristics | % (n) | N |
| Medications used | 91 | |
| Mifepristone and misoprostol in combination | 82.4 (75) | |
| Misoprostol alone | 17.6 (16) | |
| Hours between mifepristone and first dose of misoprostol (mean (range)* | 32.9 (12–60) | 47 |
| Timing of medication doses adheres to evidence-based protocols* | 95.7 (45) | 47 |
| Warning signs of potential complications† | 90 | |
| Experienced heavy bleeding | 12.2 (11) | |
| Experienced high fever | 3.3 (3) |
*Complete data on medication timing missing for 28 callers.
†Data on heavy bleeding and high fever missing for one caller. Heavy bleeding is defined as soaking more than two sanitary pads per hour for more than 2 hours; high fever is defined as recorded temperature of over 38°C for more than 24 hours.
Women experienced a variety of normal side effects during the abortion process including nausea, dizziness, mild fever, heavy bleeding, and cramps (data not shown). In total, 11 women experienced heavy bleeding, and three experienced a fever over 38°C lasting more than 24 hours. Fifty-five women used over-the-counter painkillers to help manage pain.
Discussion
This is the first known documentation of the process and outcomes of second-trimester medication abortion provision outside of a clinic setting by non-clinically trained abortion counsellors. Despite data limitations, our analysis suggests that when women have access to accurate information alongside empathic and evidence-based counselling, they may be able to safely self-manage medication abortions beyond the first trimester.
Our study has some important limitations: data collected by this hotline are not collected for research purposes, nor are they collected by trained researchers – thus data suffer from missing data on sociodemographic information and secondary outcomes of interest, such as timing of medication doses. Despite data imperfections, this analysis demonstrates a clear and compelling need for abortion services beyond the first trimester, and suggests that further exploration of this model of accompaniment for self-management of later abortion is warranted. In addition, we were unable to reliably determine the incidence of abortion complications among women included in our analysis. An agreed-upon definition of and framework for abortion complications in settings where unsafe abortion persists does not exist, and the lack of such a definition stymies efforts to reliably document the safety of abortions in much of the world.22 Accurate estimates of the incidence and severity of abortion complications both in and out of facility settings are essential to developing targeted and effective programmes, policies and interventions to increase access to safe abortion and to improve women’s health. An additional limitation is the small sample size of this study; though this study includes data on all callers to the safe abortion hotline reporting gestational ages over 12 weeks during the study period, second-trimester medication abortion clients are a low percentage of overall callers. Future studies should aim to document second-trimester medication abortions across multiple contexts.
There has been little documentation of women’s experiences self-managing abortions with the support of hotlines or other non-clinically trained abortion counsellors.11 12 15 18 23 24 Evidence from Europe, Canada and the USA suggests that early in pregnancy, a ‘home-based’ medication abortion (where women take mifepristone in a clinic, and return home to take the remaining doses of misoprostol) is as safe, effective and acceptable as clinic-based medication abortion, and may increase access to care by reducing the number of clinic visits a woman is required to attend.23 Abortion beyond 12 weeks gestation, however, is qualitatively different, and objectively runs a higher risk of mortality and morbidity. While some women seeking abortion later in pregnancy express a preference for medication abortion in legal, clinic-based settings,25 26 no research has documented the preferences, expectations or experiences of women in need of later abortion in legally restricted, non-clinic based settings.
Evidence has demonstrated that the provision of second-trimester abortions using medications requires training in medication protocols, empathic counselling skills, and well-established emergency plans27 – it does not, however, require advanced clinical training or surgical skills as required for dilation and evacuation (the other WHO recommended method for abortion beyond 12 weeks gestation). Globally, evidence has shown that when women cannot access safe abortion services, they often utilise abortion methods that endanger their health.28 Given the demonstrated need for abortions later in pregnancy regardless of the legal setting, safe-abortion hotlines are providing women with essential, evidence-based information on how to self-manage medication abortions beyond 12 weeks gestation. If this model proves to be a safer alternative than existing options, these services have the potential to dramatically reduce abortion-related harms for women worldwide.
Our analysis of electronic client records from this safe-abortion hotline in Indonesia suggests that the model of providing accompaniment services for abortions later in pregnancy could be a safe alternative for women in need of abortions beyond 12 weeks gestation in legally restrictive contexts. Further research is warranted to document the safety, feasibility and acceptability of non-clinic-based second-trimester medication abortion, and accompaniment services provided by non-physician providers as a way of expanding access to safe abortion later in pregnancy.
Acknowledgments
The authors would like to thank the staff at the safe abortion hotline in Indonesia for generously providing them with access to their counselling records.
Footnotes
Contributors: CG and IH originated the study question. RTJ conducted the analysis. CG and RTJ wrote the original draft of the manuscript. CG, RTJ, SB and IH all contributed in reviewing and editing the manuscript. All authors read and approved the final manuscript.
Funding: This work was supported in part by the David and Lucile Packard Foundation. The funders were not involved in study design; in the collection, analysis and interpretation of data; in the writing of the report; or in the decision to submit the article for publication.
Competing interests: None declared.
Patient consent: Not required.
Ethics approval: Ethical approval for this study was obtained from Allendale Investigational Review Board. As the data were collected in the process of routine service provision, and the authors only had access to data that were completely anonymised, informed consent was not collected from callers to the safe abortion hotline.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: Data are available upon reasonable request; please contact rjayaweera@ibisreproductivehealth.org.
References
- 1. Drey EA, Foster DG, Jackson RA, et al. Risk factors associated with presenting for abortion in the second trimester. Obstet Gynecol 2006;107:128–35. 10.1097/01.AOG.0000189095.32382.d0 [DOI] [PubMed] [Google Scholar]
- 2. Foster DG, Kimport K. Who seeks abortions at or after 20 weeks? Perspect Sex Reprod Health 2013;45:210–8. 10.1363/4521013 [DOI] [PubMed] [Google Scholar]
- 3. Swanson M, Karasek D, Drey E, et al. Delayed pregnancy testing and second-trimester abortion: can public health interventions assist with earlier detection of unintended pregnancy? Contraception 2014;89:400–6. 10.1016/j.contraception.2013.12.008 [DOI] [PubMed] [Google Scholar]
- 4. Baum S, DePiñeres T, Grossman D. Delays and barriers to care in Colombia among women obtaining legal first- and second-trimester abortion. Int J Gynaecol Obstet 2015;131:285–8. 10.1016/j.ijgo.2015.06.036 [DOI] [PubMed] [Google Scholar]
- 5. Finer LB, Frohwirth LF, Dauphinee LA, et al. Timing of steps and reasons for delays in obtaining abortions in the United States. Contraception 2006;74:334–44. 10.1016/j.contraception.2006.04.010 [DOI] [PubMed] [Google Scholar]
- 6. Gerdts C, Fuentes L, Grossman D, et al. Impact of clinic closures on women obtaining abortion services after implementation of a restrictive law in Texas. Am J Public Health 2016;106:857–64. 10.2105/AJPH.2016.303134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Kiley JW, Yee LM, Niemi CM, et al. Delays in request for pregnancy termination: comparison of patients in the first and second trimesters. Contraception 2010;81:446–51. 10.1016/j.contraception.2009.12.021 [DOI] [PubMed] [Google Scholar]
- 8. Harris LH, Grossman D. Confronting the challenge of unsafe second-trimester abortion. Int J Gynaecol Obstet 2011;115:77–9. 10.1016/j.ijgo.2011.05.018 [DOI] [PubMed] [Google Scholar]
- 9. Sedgh G, Bearak J, Singh S, et al. Abortion incidence between 1990 and 2014: global, regional, and subregional levels and trends. Lancet 2016;388:258–67. 10.1016/S0140-6736(16)30380-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Wainwright M, Colvin CJ, Swartz A, et al. Self-management of medical abortion: a qualitative evidence synthesis. Reprod Health Matters 2016;24:155–67. 10.1016/j.rhm.2016.06.008 [DOI] [PubMed] [Google Scholar]
- 11. Foster AM, Arnott G, Hobstetter M. Community-based distribution of misoprostol for early abortion: evaluation of a program along the Thailand-Burma border. Contraception 2017;96:242–7. 10.1016/j.contraception.2017.06.006 [DOI] [PubMed] [Google Scholar]
- 12. Aiken ARA, Digol I, Trussell J, et al. Self reported outcomes and adverse events after medical abortion through online telemedicine: population based study in the Republic of Ireland and Northern Ireland. BMJ 2017;357:j2011 10.1136/bmj.j2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Grossman D, Baum SE, Andjelic D, et al. A harm-reduction model of abortion counseling about misoprostol use in Peru with telephone and in-person follow-up: A cohort study. PLoS One 2018;13:e0189195 10.1371/journal.pone.0189195 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Erdman JN. Access to information on safe abortion: a harm reduction and human rights approach. Harvard Journal of Law & Gender 2011;34:413–62. [Google Scholar]
- 15. Gerdts C, Hudaya I. Quality of care in a safe-abortion hotline in Indonesia: beyond harm reduction. Am J Public Health 2016;106:2071–5. 10.2105/AJPH.2016.303446 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Gemzell-Danielsson K, Lalitkumar S. Second trimester medical abortion with mifepristone-misoprostol and misoprostol alone: a review of methods and management. Reprod Health Matters 2008;16:162–72. 10.1016/S0968-8080(08)31371-8 [DOI] [PubMed] [Google Scholar]
- 17. World Health Organization. Safe abortion: technical and policy guidance for health systems. 2nd edn Geneva, Switzerland: WHO, 2012. [PubMed] [Google Scholar]
- 18. Zurbriggen R, Keefe-Oates B, Gerdts C. Accompaniment of second-trimester abortions: the model of the feminist Socorrista network of Argentina. Contraception 2018;97:108–15. 10.1016/j.contraception.2017.07.170 [DOI] [PubMed] [Google Scholar]
- 19. World Health Organization. Health worker roles in providing safe abortion care and post-abortion contraception. Geneva, Switzerland: WHO, 2015. [PubMed] [Google Scholar]
- 20. Gynuity Health Projects. Instructions for use: mifepristone plus misoprostol or misoprostol-alone for abortion induction in pregnancies 12-24 weeks’ LMP. 2014. http://gynuity.org/resources/ (22 May 2018).
- 21.Stata Statistical Software: Release 14. College Station, TX: StataCorp; 2015. [Google Scholar]
- 22. Ganatra B, Gerdts C, Rossier C, et al. Global, regional, and subregional classification of abortions by safety, 2010-14: estimates from a Bayesian hierarchical model. Lancet 2017;390:2372–81. 10.1016/S0140-6736(17)31794-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Ngo TD, Park MH, Shakur H, et al. Comparative effectiveness, safety and acceptability of medical abortion at home and in a clinic: a systematic review. Bull World Health Organ 2011;89:360–70. 10.2471/BLT.10.084046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Footman K, Scott R, Taleb F, et al. Feasibility of assessing the safety and effectiveness of menstrual regulation medications purchased from pharmacies in Bangladesh: a prospective cohort study. Contraception 2018;97:152–9. 10.1016/j.contraception.2017.08.002 [DOI] [PubMed] [Google Scholar]
- 25. Henshaw RC, Naji SA, Russell IT, et al. Comparison of medical abortion with surgical vacuum aspiration: women’s preferences and acceptability of treatment. BMJ 1993;307:714–7. 10.1136/bmj.307.6906.714 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Kerns J, Vanjani R, Freedman L, et al. Women’s decision making regarding choice of second trimester termination method for pregnancy complications. Int J Gynaecol Obstet 2012;116:244–8. 10.1016/j.ijgo.2011.10.016 [DOI] [PubMed] [Google Scholar]
- 27. Turner KL, Hyman AG, Gabriel MC. Clarifying values and transforming attitudes to improve access to second trimester abortion. Reprod Health Matters 2008;16:108–16. 10.1016/S0968-8080(08)31389-5 [DOI] [PubMed] [Google Scholar]
- 28. Grimes DA, Benson J, Singh S, et al. Unsafe abortion: the preventable pandemic. Lancet 2006;368:1908–19. 10.1016/S0140-6736(06)69481-6 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjsrh-2018-200102supp001.jpg (257.4KB, jpg)