Abstract
Objectives:
The annual number of women with HIV infection who delivered infants in the United States was estimated to be 8700 in 2006. An accurate, current estimate is important for guiding perinatal HIV prevention efforts. Our objective was to analyze whether the 2006 estimate was consistent with the number of infants with HIV infection observed in the United States and with other data on perinatal HIV transmission.
Methods:
We compared the number of infants born with HIV in 2015 (n = 53) with data on interventions to prevent perinatal HIV transmission (eg, maternal HIV diagnosis before and during pregnancy and prenatal antiretroviral use). We also estimated the annual number of deliveries to women living with HIV by using the number of women of childbearing age living with HIV during 2008-2014 and the estimated birth rate among these women. Finally, we determined any changes in the annual number of infants born to women with HIV from 2007-2015, among 19 states that reported these data.
Results:
The low number of infants born in the United States with HIV infection and the uptake of interventions to prevent perinatal HIV transmission were not consistent with the 2006 estimate (n = 8700), even with the best uptake of interventions to prevent perinatal HIV transmission. Given the birth rate among women with HIV (estimated at 7%) and the number of women aged 13-44 living with HIV during 2008-2014 (n = 111 273 in 2008, n = 96 363 in 2014), no more than about 5000 women with HIV would be giving birth. Among states consistently reporting the annual number of births to women with HIV, the number declined about 14% from 2008 to 2014.
Conclusion:
The current annual number of women with HIV infection delivering infants in the United States is about 5000, which is substantially lower than the 2006 estimate. More accurate estimates would require comprehensive reporting of perinatal HIV exposure.
Keywords: HIV, women, birth, pregnancy, delivery
The number of infants born in the United States with perinatally acquired HIV infection declined from 99 in 2010 to 53 in 2015.1 This decrease supports the notion that perinatal HIV transmission can be eliminated in the United States. To eliminate perinatal HIV transmission, it is important to know the annual number of women with HIV who give birth. This information can increase understanding of the uptake and impact of interventions designed to prevent perinatal transmission and can be used to determine how many women must be linked to and retained in HIV care postpartum. It is also needed to estimate a national perinatal HIV transmission rate (ie, the number of infants with infection divided by the number of deliveries to women with HIV), which is directly related to 2 goals of the Centers for Disease Control and Prevention’s (CDC’s) framework to eliminate perinatal HIV transmission: (1) a perinatal HIV transmission rate <1% among HIV-exposed infants and (2) an annual incidence of <1 per 100 000 live births.2
The annual number of HIV-exposed infants in the United States was accurately known from 1988-1995 from CDC’s Survey of Childbearing Women, in which heel-stick blood specimens, obtained for metabolic screening from all newborns in the United States, were anonymously tested for HIV antibodies.3-5 However, the survey was discontinued in 1995 after the benefit of zidovudine prophylaxis was established.6 Since then, the number of women with HIV infection who delivered infants was estimated to be 6249 in 20 007 and 8700 in 2006.8
Surveillance data from 50 states on HIV infections in infants have been published since 2011; in recent years, however, the number of infants has seemed incompatible with the 2006 estimate of 8700 exposed infants. We sought to determine whether the 2006 estimate of the number of women with HIV giving birth (ie, the number of HIV-exposed births) in the United States was supported by current data. Accordingly, we asked 3 questions: (1) Is the current number of infants born with HIV infection in the United States consistent with current corroborating data and the estimated annual number of deliveries to women with HIV? (2) Is the annual, estimated number of deliveries to women with HIV consistent with the estimated birth rate among women of childbearing age currently living with HIV? and (3) Has the annual number of infants born to women with HIV among states that report these data changed in the past decade?
Materials and Methods
Estimating the Number of Infants With HIV
To answer the first question, we first estimated the expected number of infants with HIV infection by using various numbers of women with HIV infection who delivered infants but maintaining the current uptake of interventions. We compared that estimate with the current observed number of infants with HIV infection. We also estimated the expected range of the number of HIV-infected women likely to be giving birth rather than a single estimate, which would have required more inputs than were practical. We based our approach on various assumptions about the numbers of exposed births per year and assumptions derived from the literature.
We considered a set of variables, each of which was, in turn, considered under a “basic” case and an “optimal” case.9-14 The basic case used established data from the largest sources available (eg, CDC’s Enhanced Perinatal Surveillance [EPS]).9 The EPS enrolled women with HIV and HIV-exposed infants from 2000 through 2003 and from 2005 through 2010; most enrollees were mother-infant pairs. At enrollment, which could occur during pregnancy, during labor, or after delivery, the time of maternal HIV diagnosis was classified as before or during pregnancy, during labor or delivery, or later. The optimal case used “best-case” estimates (ie, estimates of available data, the best adherence to recommended practice), most of which were from states or cities. We describe the variables used in both cases.
Rate of HIV diagnosis before pregnancy
In the basic case, 68% of women had received a diagnosis before pregnancy9 and 32% had not. In the optimal case, we substantially increased—compared with the basic case—the percentage of women with an HIV diagnosis before pregnancy, to 82%. Data on diagnosis before pregnancy since completion of EPS have been reported in state HIV surveillance systems: 77% in Florida,14 79% in Philadelphia,15 80% in New York City (unpublished poster; Shah D, Westheimer E, Gill B, et al. Mother-to-child HIV transmission in New York City, 2005-2015. Presented at CDC Department of HIV/AIDS Prevention Surveillance Grantees’ Meeting; March 2017; Atlanta, GA), and 82% in Louisiana (unpublished poster; Hoover A. Using surveillance data to eliminate perinatal HIV transmission in Louisiana. Presented at CDC Division of HIV/AIDS Prevention Surveillance Grantees’ Meeting; March 2017; Atlanta, GA). Using the highest of these percentages (82%) for the optimal case, 18% of women with HIV need to be identified by using prenatal HIV testing.
Rate of prenatal HIV testing
In the basic case, we assumed an overall testing rate of 75%,10 which meant that 25% of pregnant women gave birth without having been tested and, thus, were not given antiretroviral prophylaxis. In the optimal case, we increased the prenatal testing rate to 85%, the maximum recently reported,11 which meant that 15% of pregnant women with HIV were not given antiretroviral prophylaxis.
Rate of prenatal antiretroviral prophylaxis
In the basic case, we assumed that 84% of pregnant women with HIV infection used antiretroviral prophylaxis (based on EPS data9); for our purposes, antiretroviral prophylaxis was considered equivalent to antiretroviral therapy, and we refer to both as “antiretrovirals” throughout the article. (There is benefit—albeit reduced—if the infant alone receives single-drug antiretroviral prophylaxis within 48 hours of birth and even more benefit with a 2- or 3-drug infant prophylaxis regimen.16,17 However, we did not attempt to account for the small number of situations in which only the infant received antiretroviral prophylaxis.) In the optimal case, we increased the maternal prenatal antiretroviral uptake rate to 95% (a high rate never documented in population-based data in the United States).
Rate of perinatal HIV transmission
In the basic case, we assumed that the transmission rate was 22% if antiretroviral prophylaxis was not used, as observed in the original placebo-controlled trial of zidovudine for perinatal prophylaxis,12 and 0.5% if antiretroviral prophylaxis was used.13 In the optimal case, we maintained the 0.5% perinatal transmission rate, a low figure, and did not attempt further optimization. Thus, the perinatal transmission rates did not differ between the 2 cases.
Estimating the Number of Deliveries
To answer question 2 and estimate the number of deliveries, we calculated the number of deliveries expected based on the number of women of childbearing age and the birth rate or pregnancy rate of these women. We determined the number of women aged 13-44 for 2014, the most recent year for which data were available from the AtlasPlus website18 of CDC’s National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention. We used published estimates of the birth rate19,20 or the pregnancy rate20,21 of women with HIV.
Number of HIV-Exposed Infants Reported by States
To answer question 3, we determined the number of HIV-exposed infants reported by states by searching for the number of HIV-exposed infants reported on the websites of state public health jurisdictions with a longstanding practice of collecting data on perinatal HIV exposure. From 2007 through 2015, no more than 19 states posted such data on perinatal HIV exposure. We obtained other data through written communications from Illinois (Anne Statton, Pediatric AIDS Chicago Prevention Initiative, April 3, 2017), New York State (Barbara Warren, New York State Department of Health, AIDS Institute, April 17, 2017), and Texas (Kacey Russell, Texas Department of Health and Human Services, April 3, 2017). Most states do not publish data on perinatal HIV exposure.
Results
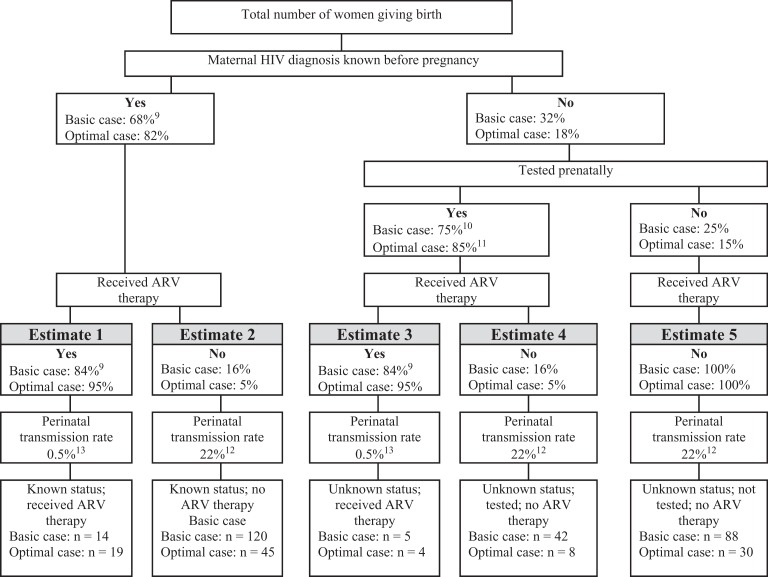
Applying various assumptions yielded various subsets of women (Figure). For example, in the basic case of estimate 5, of 5000 women known to have HIV before pregnancy and who gave birth, 1600 (0.32 × 5000) women would be unaware of their infection, 400 (0.25 × 1600) would not be tested prenatally, and none would receive prenatal antiretrovirals, resulting in 88 infants (0.22 × 400) with HIV infection. In the basic case of estimate 2, of 3400 (0.68 × 5000) women known to have HIV before pregnancy and who gave birth, 544 (0.16 × 3400) would not receive prenatal antiretrovirals, resulting in 120 infants (0.22 × 544) with HIV infection.
Figure.
Estimating the number of newborns with HIV under “basic” and “optimal” uptake of preventive interventions, based on the number of women with HIV giving birth, United States, 2008-2014. This figure illustrates a method to validate an estimated number of women with HIV delivering infants against a known number of infants born with HIV infection in a given year, incorporating what is known about women’s knowledge of their HIV status before pregnancy, the rate of prenatal HIV testing, the uptake of antiretrovirals (ARVs) for maternal treatment and perinatal prophylaxis, and the mother-to-child HIV transmission rates when ARVs are used or not used. For each factor, there is a “basic” and an “optimal” value. The basic case used established data from the largest sources available (eg, the Centers for Disease Control and Prevention’s Enhanced Perinatal Surveillance).9 The optimal case used best-case estimates (ie, estimates of available data, the best adherence to recommended practice), most of which were from states or cities. Of the women with HIV delivering infants in a given year, the number of infants with infection depends on the proportions of women with various combinations of these values. The 5 “estimates” in the bottom row of boxes are those infants. For example, estimate 1 contains the number of infants with infection born to mothers whose HIV infection status was known before pregnancy and who took ARVs. The total number of infants with infection is the sum of the numbers in the 5 boxes. In this case, the number of infants born with infection is based on 5000 women with HIV with live births in a particular year.
In the basic case, any of these subsets of women delivering infants (ie, women unaware of their diagnosis, who were not tested, and who therefore did not receive prenatal antiretrovirals [estimate 5] and women aware of their diagnosis and who did not receive antiretroviral prophylaxis during pregnancy [estimate 2]; 88 and 120 infants, respectively) would result in more infants with infection than had been recently observed. Thus, as indicated by all 5 estimates of the basic case, beginning with 5000 deliveries to women with HIV infection, the estimated number of infants born with HIV infection in a single year was 269 (88 + 120 + 14 + 5 + 42). Under the optimal case, beginning with 5000 deliveries to women with HIV infection, the estimated number of infants with HIV infection was 106 (30 + 45 + 19 + 8 + 4).
With 96 363 women aged 13-44 living with HIV in 2014, fewer than 8700 deliveries per year would be expected, with an estimated range of 5000-7000 deliveries based on available estimates of birth or pregnancy rates in women with HIV.
The annual number of HIV-exposed births decreased substantially during the past 10-15 years (Table). Of the 16 states that consistently recorded data on the number of HIV-exposed infants from 2008 through 2014, the number of HIV-exposed births declined by 14%, from 2798 in 2008 to 2410 as of April 2017.
Table.
Number of HIV-exposed infants born per year, as reported by 19 state public health departments, 2007-2015a
| Year Data Were Reported | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| State | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 |
| Colorado22,23 | 30 | 28 | 29 | 24 | 22 | 30 | 23 | 27 | 33 |
| Connecticut24 | 46 | 36 | 42 | 29 | 38 | 40 | 33 | 34 | 40 |
| Florida25 | 672 | 628 | 620 | 577 | 579 | 527 | 516 | 506 | — |
| Georgia26 | 104 | 108 | 116 | 69 | — | — | — | — | — |
| Illinoisb | 160 | 142 | 174 | 128 | 133 | 135 | 113 | 119 | 133 |
| Indiana28 | — | 83 | 30 | 73 | 67 | 57 | 55 | 152 | 38 |
| Iowa27 | 11 | 22 | 15 | 16 | 11 | 9 | 14 | 15 | 16 |
| Louisiana29 | 180 | 170 | 172 | 170 | 150 | 158 | 160 | 148 | 156 |
| Maryland30 | 176 | 206 | 171 | 177 | 174 | 183 | 165 | 193 | 127 |
| Michigan31 | 54 | 39 | 34 | 44 | 63 | 50 | 26 | 14 | — |
| Minnesota32 | 59 | 53 | 71 | 51 | 65 | 59 | 62 | 65 | — |
| Mississippi33 | 69 | 54 | 51 | 45 | 50 | — | — | — | — |
| Nevada34,35 | 21 | 19 | — | 38 | 33 | 20 | 18 | — | — |
| New Jersey36 | 166 | 195 | 161 | 156 | 150 | 127 | 127 | 130 | — |
| New York37 | 567 | 488 | 536 | 485 | 469 | 415 | 424 | 400 | 404 |
| Pennsylvania38 | 175 | 180 | 175 | 160 | 150 | 140 | 150 | 130 | 120 |
| South Carolina39 | 96 | 74 | 92 | 90 | 70 | 73 | 52 | 48 | — |
| Texasd | 401 | 427 | 435 | 435 | 420 | 392 | 409 | 407 | — |
| Wisconsin40 | 22 | 12 | 23 | 20 | 18 | 29 | 15 | 22 | — |
| Total | 3009 | 2964 | 2947 | 2787 | 2662 | 2444 | 2362 | 2410 | 1067 |
aData collected from the 19 state public health jurisdictions with a longstanding practice of collecting data on perinatal HIV exposure. Most states do not publish data on perinatal HIV exposure. Empty cells indicate no data were posted for those years.
bWritten communication from Anne Statton, Pediatric AIDS Chicago Prevention Initiative, April 3, 2017.
cWritten communication from Barbara Warren, New York State Department of Health, AIDS Institute, April 17, 2017.
dWritten communication from Kacey Russell, Texas Department of Health and Human Services, April 3, 2017.
Discussion
The 2006 published estimate of the annual number of infants born to women with HIV in the United States is inconsistent with available data on the number of infants with HIV being born in the United States in the past 5 years.1 To reconcile the known 53 infected infants with the 8700 infants born to women with HIV annually,8 1 or more of the following changes would be required, all of which are unlikely at present:
The proportion of pregnant women with HIV infection diagnosed before pregnancy would have to be higher than the 82% cited in the optimal case. To diagnose HIV infection in a higher percentage of women before their pregnancy would require more testing of the general population than is presently conducted.
Maternal antiretroviral uptake would have to increase to more than 95%. Anecdotally, some clinicians report high percentages of antiretroviral use among pregnant women in their care, but no published population-based data show rates of antiretroviral treatment at 95%.
Prenatal HIV testing would have to be achieved at a rate higher than 85%, and such a rate was found only in New York State.37
Perinatal HIV transmission would have to occur at a rate of <0.5% among women receiving antiretroviral prophylaxis or treatment, and such rates have been found only among women with suppressed viral loads.
The observed number of women of childbearing age with HIV and the birth rate among these women are such that the annual number of births is likely lower than 8700. An annual number of births in the 5000 range is consistent with a pregnancy rate of approximately 5%, a rate similar to the birth rate19 or pregnancy rate21 described for women with HIV infection in the United States. The Women’s Interagency HIV Study reported the live-birth rate of women with HIV infection increasing to approximately 7% in more recent years20; this rate would still result in fewer than 8700 births per year.
The estimated 8700 infants born to women with HIV infection in 20068 was determined by multiplying the number of women of childbearing age living with HIV infection by the pregnancy rate of women with HIV.20 Because HIV infection was reported by name in only 34 states and 5 US dependent areas, the number of additional HIV cases was back-calculated based on the number of AIDS cases in the 50 US states and 5 dependent areas. The analysis accounted for women whose infection had not yet been diagnosed. In contrast, the annual number of HIV-exposed births in the United States could be known if the reporting of perinatal HIV exposure were comprehensive. Such reporting is recommended by CDC, the Council of State and Territorial Epidemiologists, and the American Academy of Pediatrics, and relevant data can be collected through the National HIV Surveillance System. Comprehensive perinatal HIV exposure reporting would have the additional advantage of providing detailed information about interventions to prevent perinatal transmission of HIV. An alternative means of establishing the number of births to women with HIV infection would be to match birth certificate registries with HIV surveillance registries. This practice is already underway in several HIV surveillance jurisdictions and would provide a definitive number of births to women with HIV if conducted in all HIV surveillance jurisdictions across the United States.
To eliminate perinatal HIV infection, national efforts are underway to support an integrated, comprehensive approach to perinatal HIV surveillance and prevention activities for women and children. Activities to be conducted in all jurisdictions include prenatal HIV testing, HIV case surveillance for women and children, and annual matching of birth certificates with HIV surveillance data. Jurisdictions with the highest numbers of women of childbearing age living with HIV will also implement perinatal HIV exposure reporting, coordinate perinatal HIV services, and conduct reviews of all cases of perinatal HIV infection (and selected cases of perinatal HIV exposure) and community action to improve local preventive systems, using the Fetal Infant Mortality Review—HIV Prevention Methodology (http://www.fimrhiv.org).
Limitations
This study had several limitations. First, because 2010 was the last year for which EPS data were available, our requirement that we use the largest available data sources meant that some basic case data were nearly 10 years old. Uptake of some interventions may have improved since 2010; we included large-scale data from state surveillance, when available, to attempt to account for this limitation. Second, although 95% confidence intervals were available for some of the data we used to answer questions 1 and 2, accounting for these intervals was beyond the scope of this analysis. We sought to investigate whether the 2006 estimate was still valid, not to create a precise new estimate. Finally, to answer question 3, we used data from only 16 states.
Practice Implications
It is possible—indeed, likely—that the yearly number of women with HIV infection who deliver infants in the United States is substantially lower than the 2006 estimate. A better estimate would more accurately identify the extent of the challenges in eliminating perinatal HIV transmission, provide an important context in which to evaluate clinical and public health activities, and improve estimates of mother-to-child transmission of HIV infection.
Acknowledgments
The findings and conclusions in this article are those of the authors and do not necessarily represent the views of CDC. The use of trade names and commercial sources is for identification only and does not imply endorsement by CDC.
Footnotes
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Centers for Disease Control and Prevention. Monitoring selected national HIV prevention and care objectives by using HIV surveillance data—United States and 6 dependent areas, 2016. HIV Surveill Suppl Rep. 2018;23(4):1–51. [Google Scholar]
- 2. Nesheim S, Taylor A, Lampe MA, et al. A framework for elimination of perinatal transmission of HIV in the United States. Pediatrics. 2012;130(4):738–744. [DOI] [PubMed] [Google Scholar]
- 3. Davis SF, Byers RH, Jr, Lindegren ML, Caldwell MB, Karon JM, Gwinn M. Prevalence and incidence of vertically acquired HIV infection in the United States. JAMA. 1995;274(12):952–955. [PubMed] [Google Scholar]
- 4. Davis SF, Rosen DH, Steinberg S, Wortley PM, Karon JM, Gwinn M. Trends in HIV prevalence among childbearing women in the United States, 1989-1994. J Acquir Immune Defic Syndr Hum Retrovirol. 1998;19(2):158–164. [DOI] [PubMed] [Google Scholar]
- 5. Lindegren ML, Byers RH, Jr, Thomas P, et al. Trends in perinatal transmission of HIV/AIDS in the United States. JAMA. 1999;282(6):531–538. [DOI] [PubMed] [Google Scholar]
- 6. Connor EM, Sperling RS, Gelber R, et al. Reduction of maternal-infant transmission of human immunodeficiency virus type 1 with zidovudine treatment. N Engl J Med. 1994;331(18):1173–1180. [DOI] [PubMed] [Google Scholar]
- 7. Fleming P, Lindegren M, Byers R, et al. Estimated number of perinatal HIV infections, U.S., 2000. 14th International AIDS Conference. Abstract No. TuPeC4773; July 7-12, 2002; Barcelona, Spain. [Google Scholar]
- 8. Whitmore SK, Zhang X, Taylor AW, Blair JM. Estimated number of infants born to HIV-infected women in the United States and five dependent areas, 2006. J Acquir Immune Defic Syndr. 2011;57(3):218–222. [DOI] [PubMed] [Google Scholar]
- 9. Centers for Disease Control and Prevention. Enhanced perinatal surveillance—15 areas, 2005-2008. HIV Surveill Suppl Rep. 2011;16(2):1–32. [Google Scholar]
- 10. FitzHarris LF, Taylor AW, Zhang F, et al. Factors associated with human immunodeficiency virus screening of women during pregnancy, labor and delivery. Matern Child Health J. 2014;18(3):648–656. [DOI] [PubMed] [Google Scholar]
- 11. Ross CE, Tao G, Patton M, Hoover KW. Screening for human immunodeficiency virus and other sexually transmitted diseases among U.S. women with prenatal care. Obstet Gynecol. 2015;125(5):1211–1216. [DOI] [PubMed] [Google Scholar]
- 12. Sperling RS, Shapiro DE, Coombs RW, et al. Maternal viral load, zidovudine treatment, and the risk of transmission of human immunodeficiency virus type 1 from mother to infant. Pediatric AIDS Clinical Trials Group Protocol 076 Study Group. N Engl J Med. 1996;335(22):1621–1629. [DOI] [PubMed] [Google Scholar]
- 13. Townsend CL, Byrne L, Cortina-Borja M, et al. Earlier initiation of ART and further decline in mother-to-child HIV transmission rates, 2000-2011. AIDS. 2014;28(7):1049–1057. [DOI] [PubMed] [Google Scholar]
- 14. Trepka MJ, Mukherjee S, Beck-Sague C, et al. Missed opportunities for preventing perinatal transmission of human immunodeficiency virus, Florida, 2007-2014. South Med J. 2017;110(2):116–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Anderson EA, Momplaisir FM, Corson C, Brady KA. Assessing the impact of perinatal HIV case management on outcomes along the HIV care continuum for pregnant and postpartum women living with HIV, Philadelphia 2005-2013. AIDS Behav. 2017;2(9):2670–2681. [DOI] [PubMed] [Google Scholar]
- 16. Wade NA, Birkhead GS, Warren BL, et al. Abbreviated regimens of zidovudine prophylaxis and perinatal transmission of the human immunodeficiency virus. N Engl J Med. 1998;339(20):1409–1414. [DOI] [PubMed] [Google Scholar]
- 17. Nielsen-Saines K, Watts DH, Veloso VG, et al. Three postpartum antiretroviral regimens to prevent intrapartum HIV infection. N Engl J Med. 2012;366(25):2368–2379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Centers for Disease Control and Prevention. AtlasPlus. https://gis.cdc.gov/grasp/nchhstpatlas/main.html. Accessed March 20, 2017.
- 19. Sharma A, Feldman JG, Golub ET, et al. Live birth patterns among human immunodeficiency virus-infected women before and after the availability of highly active antiretroviral therapy. Am J Obstet Gynecol. 2007;196(6):541.e1-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Haddad LB, Wall KM, Mehta CC, et al. Trends of and factors associated with live-birth and abortion rates among HIV-positive and HIV-negative women. Am J Obstet Gynecol. 2017;216(1):71.e1-71.e16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Blair JM, Hanson DL, Jones JL, Dworkin MS. Trends in pregnancy rates among women with human immunodeficiency virus. Obstet Gynecol. 2004;103(4):663–668. [DOI] [PubMed] [Google Scholar]
- 22. Colorado Department of Public Health and Environment. Integrated HIV/AIDS epidemiologic profile of HIV and AIDS prevention and care planning reported through December 2010. https://www.colorado.gov/pacific/cdphe/sti-and-hivaids-epidemiology-reports. Accessed March 3, 2017.
- 23. Colorado Department of Public Health and Environment. Integrated HIV/AIDS epidemiology annual report for cases diagnosed through December 2015. 2017. https://www.colorado.gov/pacific/cdphe/sti-and-hivaids-epidemiology-reports. Accessed March 3, 2017.
- 24. Connecticut Department of Public Health. Connecticut Department of Public Health HIV Surveillance Program Trends in Perinatal Exposure to HIV, by Year of Birth and HIV Status of the Child, Connecticut, 1995-2015 Hartford, CT: Connecticut Department of Public Health; 2016. [Google Scholar]
- 25. Florida Department of Health. Epidemiologic profile on pediatric HIV/AIDS surveillance in Florida, 2014. http://www.floridahealth.gov/diseases-and-conditions/aids/surveillance/epi-profiles/pediatric-epiprofilereport-2014.pdf. Accessed March 31, 2017.
- 26. Georgia Department of Public Health. Enhanced perinatal HIV/AIDS surveillance (EPS), Georgia, 2005-2010. 2013. http://dph.georgia.gov/enhanced-perinatal-hivaids-surveillance-eps . Accessed March 31, 2017.
- 27. Iowa Department of Public Health. 2015 HIV epidemiological profile for Iowa. 2016. https://idph.iowa.gov/Portals/1/Files/HIVSTDHEP/2015%20HIV%20Epidemiological%20Profile%20for%20Iowa.pdf. Accessed March 31, 2017.
- 28. Indiana State Department of Health. Spotlight on HIV/STD/viral hepatitis semi-annual reports. Perinatal HIV transmission. 2015. http://www.in.gov/isdh/23266.htm. Accessed March 31, 2017.
- 29. Louisiana Department of Health. 2014. STD/HIV surveillance report. http://ldh.louisiana.gov/assets/oph/HIVSTD/2014_STDHIV_SURVEILLANCE_REPORT.pdf. Accessed March 31, 2017.
- 30. Maryland Department of Health and Mental Hygiene. Maryland HIV annual epidemiological profile—2015. http://phpa.dhmh.maryland.gov/OIDEOR/CHSE/SiteAssets/Pages/statistics/Maryland-HIV-Annual-Epidemiological-Profile-2015.pdf. Accessed March 31, 2017.
- 31. Michigan Department of Health and Human Services. HIV/AIDS statewide annual analyses. http://www.michigan.gov/mdhhs/0,5885,7-339-71550_2955_2982_46000_46003-35962--,00.html#current. Accessed March 31, 2017.
- 32. Minnesota Department of Health. HIV surveillance report. 2016: HIV/AIDS surveillance system, tables 5a and 5b. http://www.health.state.mn.us/divs/idepc/diseases/hiv/stats/2016/increport2016.pdf. Accessed March 31, 2017.
- 33. Mississippi State Department of Health. State of Mississippi. 2010. STD/HIV epidemiologic profile. http://msdh.ms.gov/msdhsite/_static/14,0,150,63.html . Accessed March 31, 2017.
- 34. Nevada Division of Public and Behavioral Health. HIV/AIDS surveillance program: special report on children born to HIV-positive women in Nevada: 2000-2008. http://dpbh.nv.gov/Programs/HIV-OPHIE/Docs/2009-03-19_PerinatalReport . Accessed March 31, 2017.
- 35. Nevada Division of Public and Behavioral Health. HIV/AIDS epidemiological profile: 2009-2013. http://dpbh.nv.gov/Programs/HIV-OPHIE/Docs/HIV_Epi_Profile_2013 . Accessed March 31, 2017.
- 36. New Jersey Department of Health. New Jersey HIV/AIDS report 2015. https://www.nj.gov/health/hivstdtb/documents/newsletter/semi0615.pdf. Accessed March 31, 2017.
- 37. New York State Department of Health. Maternal-Pediatric HIV Prevention and Care Program. https://www.health.ny.gov/diseases/aids/general/about/perinatal.htm. Accessed January 17, 2018.
- 38. Pennsylvania Department of Health. Annual HIV surveillance summary report. 2015. http://www.health.pa.gov/My%20Health/Diseases%20and%20Conditions/E-H/HIV%20And%20AIDS%20Epidemiology/Pages/HIV-AIDS-Annual-Summary-and-Other-Reports.aspx#.WPi5kFUpC70. Accessed March 31, 2017.
- 39. South Carolina Department of Health and Environmental Control. An epidemiologic profile of HIV and AIDS in South Carolina. 2016. https://www.scdhec.gov/health/docs/stdhiv/pp_CH1-EpiProfile.pdf. Accessed March 31, 2017.
- 40. Wisconsin Department of Health Services. Wisconsin HIV integrated epidemiology profile, 2010-2014. 2016. https://www.dhs.wisconsin.gov/publications/p01294.pdf. Accessed March 31, 2017.