Abstract
Objectives:
We examined trends in prevalence rates of smoking and smoking cessation during pregnancy among women in the United States to assess achievement of Healthy People 2020 prevention targets.
Methods:
We assessed the smoking habits of 30 667 mothers whose children were born between 1985 and 2014 and who were sampled by the National Health and Nutrition Examination Survey, 1999-2014. Sampled participants were children aged 0-15 at the time of interview; however, an adult proxy—usually the biological mother—responded on the child’s behalf and reported information about maternal tobacco use during pregnancy. We calculated prevalence rates, adjusted odds ratios (aORs), and predicted annual increase or decrease of smoking and quitting smoking during pregnancy, adjusting for mother’s age at delivery and income level and child’s race/ethnicity and sex.
Results:
The average annual prevalence of smoking at any time during pregnancy decreased from 25.7% (95% confidence interval [CI], 15.3%-36.0%) in 1985 to 10.1% (95% CI, 7.1%-13.0%) in 2014 (P < .001), and quitting smoking at any time during the index pregnancy increased from 36.6% (95% CI, 20.3%-52.9%) in 1985 to 54.9% (95% CI, 44.4%-65.4%) in 2008 (P = .002). The adjusted annual risk of smoking during pregnancy decreased significantly by 3% (aOR = 0.97; 95% CI, 0.95-0.98; P < .001). The prevalence rate of smoking in the year 2020 extrapolated from the current trend would be 6.1%.
Conclusions:
Smoking during pregnancy in the United States is declining. However, renewed public health measures are needed to achieve the Healthy People 2020 objectives of preventing smoking among pregnant women in the United States.
Keywords: maternal smoking, pregnancy, United States, Healthy People 2020
Smoking during pregnancy is associated with increased risk of stillbirths, premature births, sudden infant death syndrome, and growth retardation as well as long-term effects on a child’s health and development, all of which are preventable.1,2 Healthy People 2020, which provides 10-year objectives for improving the health of all Americans, identified the reduction of smoking during pregnancy as a nationwide health improvement priority and provided at least 3 measurable objectives to monitor the progress made in smoking control among perinatal women. The 3 objectives are to increase abstinence from cigarette smoking, increase the proportion of women delivering a live birth who did not smoke before pregnancy, and reduce postpartum relapse of smoking among women who quit smoking during pregnancy.3
Since 2014, national estimates of prenatal smoking have been compiled by using the National Vital Statistics System through certificates of live birth, which include information about maternal cigarette smoking before and during pregnancy.4 However, other than a 2003 study using data from birth certificates excluding California (10% of the US population),5 a study using data from the 2000-2010 Pregnancy Risk Assessment Monitoring System covering 40 states and New York City,6 and the 2009-2010 Cancer Trends Progress Report using data from the general population,7 the most recent study reporting on national smoking trends among pregnant women is from 1987-1996.8 Since then, several smoking-related public policy events have occurred. These events include the Centers for Disease Control and Prevention’s (CDC’s) addition of the prevalence of smoking to the list of nationally notifiable health conditions reported by states to CDC,9 the US Department of Justice’s lawsuit against the tobacco industry under the Racketeer Influenced and Corrupt Organizations Act,10 and legislation granting the US Food and Drug Administration regulatory authority over tobacco products.11
We used the most recently released data from the National Health and Nutrition Examination Survey (NHANES) to examine trends in maternal smoking and smoking cessation during pregnancy in the United States from 1985 through 2014 to (1) address the gap in data on national trends in pregnancy-related smoking, (2) assess attainment of pregnancy-related smoking prevention targets, and (3) verify trends observed from non-national representative data such as the Pregnancy Risk Assessment Monitoring System.
Methods
Data Sources and Study Participants
NHANES is designed to assess the health and nutritional status of noninstitutionalized adults and children in the United States. A unique feature of NHANES is that the sampling approaches, interviews, and physical examination methods are standardized across surveys.12 We used the Early Childhood module of NHANES, 1999-2014, which provides personal interview data on children from birth through age 15, including the age of the biological mother when the child was born and smoking habits of the mother while pregnant with the child.13 All interviews took place in the home. NHANES interview procedures require a family member aged ≥18 to respond on behalf of children aged ≤15. Therefore, an adult proxy—usually the biological mother—answered questions and, in particular, reported information about maternal tobacco use during pregnancy.12
We started with data on 30 667 biological mothers whose biological children were sampled by NHANES. We excluded 178 participants with missing data on race/ethnicity and age of the mother when the child was born, leaving 30 489 participants with complete data. This study was determined to be exempt from ethics review by the Georgia Southern University Institutional Review Board Committee.
Study Variables
The key variables of maternal smoking behaviors were (1) smoking or not smoking during pregnancy and (2) quitting smoking any time during pregnancy if the mother of the child had been smoking. The proxy of the NHANES participant was asked, “Did the biological mother smoke at any time while she was pregnant with the survey participant?” If the answer was yes, then a further question was asked: “At any time during the pregnancy, did the biological mother quit or refrain from smoking for the rest of the pregnancy?”13 The question for smoking during pregnancy (yes/no) was asked in survey cycles 1999 through 2014. However, the question for smoking cessation was asked only during cycles 1999 through 2008. The birth year of a child was calculated by subtracting the age of the child from the interview date, resulting in birth years ranging from 1985 to 2014. The child’s race/ethnicity was reported by proxy and classified as non-Hispanic white, non-Hispanic black, Hispanic, or other (includes all other races, including mixed race). Family income was assessed by the US Census Bureau using a poverty income ratio (PIR),14 which we categorized into poor (PIR <1.0), near poor (PIR 1.0 to <2), middle income (PIR 2 to <4), and high income (PIR ≥4).15 We categorized marital status as never married, previously married, or currently married.
Statistical Analyses
We used SAS version 9.4 procedures developed for nonrandom sampling.16 Preliminary analysis revealed linear trends with the birth year for prevalence rate of smoking and the percentage of smoking mothers who quit smoking during pregnancy; therefore, we developed simple linear regression equations by using birth year as the explanatory variable to estimate the annual change in prevalence rate of smoking among mothers and percentage of smoking mothers who quit smoking during the index pregnancy. We calculated the observed prevalence and the percentage of women who quit smoking during the index pregnancy by using the PROC SURVEYFREQ procedure with appropriate weighting and nesting variables. We further estimated the relative magnitude of annual change of odds (adjusted odds ratios [aORs] with 95% confidence intervals [CIs]) of smoking during pregnancy and quitting smoking at any time during pregnancy, adjusting for the mother’s age when the child was born and the child’s race/ethnicity and sex. We also included the child’s age in multivariable regression analysis to control for the potential confounding associated with remote memory. For confidentiality reasons, the National Center for Health Statistics codes mothers aged <14 as aged 14 and mothers aged >45 as aged 45. We considered 2-sided P < .05 to be significant.
Results
The average age of children was 7.6 years (range, 0-15 years). The average age of the biological mother when the survey participant was born was 27.2 years (range, 14-45 years). More than half (56.8%; 95% CI, 54.0%-59.6%) of the weighted sample of children was non-Hispanic white, followed by Hispanic (21.4%; 95% CI, 19.1%-23.7%) and non-Hispanic black (14.2%; 95% CI, 12.7%-15.8%) (Table 1).
Table 1.
Characteristics of a sample of mothers with children aged 0-15 (n = 30 667) in a study of maternal smoking, NHANES, United States, 1985-2014a
| Characteristic | Unweighted Sample Size, No. | Valueb |
|---|---|---|
| Age of child when interview was completed, mean (95% CI), y | 30 667 | 7.6 (7.5-7.7) |
| Mother’s age when child was born, mean (95% CI), y | 30 489 | 27.2 (27.0-27.4) |
| Race/ethnicity of child | ||
| Non-Hispanic black | 8079 | 14.2 (12.7-15.8) |
| Hispanic | 11 477 | 21.4 (19.1-23.7) |
| Non-Hispanic white | 8686 | 56.8 (54.0-59.6) |
| Other | 2425 | 7.6 (6.8-8.4) |
| Sex of child | ||
| Male | 15 507 | 51.1 (50.3-51.9) |
| Female | 15 160 | 48.9 (48.1-49.7) |
| Family incomec,d | ||
| Poor | 10 103 | 24.7 (23.3-26.2) |
| Near poor | 7665 | 23.9 (22.7-25.1) |
| Middle income | 6352 | 27.8 (26.6-29.0) |
| High income | 4248 | 23.6 (21.8-25.4) |
| Marital statusc | ||
| Married | 19 837 | 75.9 (74.7-77.1) |
| Never married | 3930 | 8.9 (8.1-9.6) |
| Previously married | 4790 | 15.2 (14.3-16.0) |
| Smoking status | ||
| Smoked during pregnancy | 4052 | 15.6 (14.4-16.7) |
| Quit smoking any time during pregnancy | 1114 | 38.3 (35.1-41.4) |
Abbreviation: NHANES, National Health and Nutrition Examination Survey.
a Data source: National Center for Health Statistics, Centers for Disease Control and Prevention.13
b Values are expressed as percentage (95% CI) unless otherwise indicated.
c Data on family income and marital status of the head of household are for when the interview was conducted rather than when the child was born and were available only for the 1999-2010 surveys.
d Income was reported as a range for the previous calendar year. A poverty income ratio (PIR) was calculated by comparing the midpoint of the selected range value with the appropriate poverty threshold based on size and family composition. This study used 4 PIR categories: poor (PIR <1.0), near poor (PIR 1 to <2), middle income (PIR 2 to <4), and high income (PIR ≥4). PIR <1.0 was categorized as below the official poverty threshold.
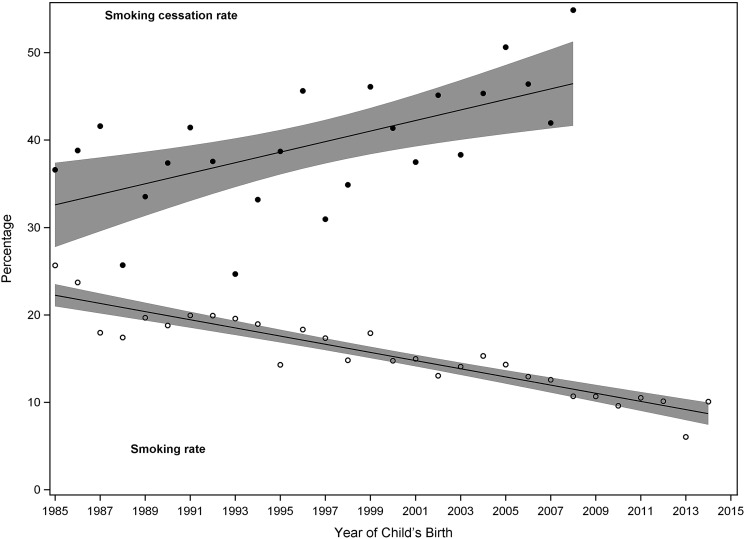
During the study period, the average annual prevalence of smoking at any time during pregnancy decreased from 25.7% (95% CI, 15.3%-36.0%) in 1985 to 10.1% (95% CI, 7.1%-13.0%) in 2014 (P < .001), and quitting any time during the index pregnancy increased from 36.6% (95% CI, 20.3%-52.9%) in 1985 to 54.9% (95% CI, 44.4%-65.4%) in 2008 (P = .002) (Figure). The simple linear regression equation to predict the prevalence rate of smoking using birth year was as follows: rate = 860.6 – 0.423 year + e [R 2 = 0.81, N = 28 (from 1985 to 2012), P for year < .001]. The equation indicates an annual decreasing prevalence rate of 0.42, equivalent to an annual decline of 2.5 percentage points relative to the overall smoking prevalence of 16.2%. Extrapolated from this equation, the predicted prevalence rate of smoking for 2020 is 6.1%. The regression equation to predict the cessation percentage among smokers was as follows: percentage = –1164 + 0.603 year + e [R 2 = 0.36, N = 24 (from 1985 to 2008), P for year = .02], indicating an annual increasing percentage of 0.60, equivalent to 1.6 percentage points relative to the overall quitting percentage of 38.3%.
Figure.
Prevalence rates of smoking and percentage of mothers who quit smoking during pregnancy in a sample of mothers with children aged 0-15 (n = 30 667), National Health and Nutrition Examination Survey, United States, 1985-2014. Data source: National Center for Health Statistics, Centers for Disease Control and Prevention.13 Line indicates best-fitting line, and shading indicates mean 95% confidence intervals. Smoking cessation rate: percentage = –1164 + 0.603 year + e [R 2 = 0.36, N = 24], P = .002 (for birth year). Smoking rate: prevalence = 949.3 – 0.467 year + e [R 2 = 0.85, N = 28], P < .001 (for birth year).
The adjusted odds of smoking during pregnancy for a 1-year increase in time was 0.97 (95% CI, 0.96-0.98; P < .001), indicating a significant annual decline of 3% (Table 2). The adjusted odds of quitting smoking any time during pregnancy for a 1-year increase in time was 1.02 (95% CI, 0.98-1.07; P = .33), indicating a nonsignificant annual increase of 2%. Compared with pregnant non-Hispanic black women, pregnant non-Hispanic white women were 4.1 times more likely to smoke during pregnancy (aOR = 4.11; 95% CI, 3.38-4.99). The likelihood of quitting smoking declined with mother’s age when pregnant. Compared with women pregnant after age 35, women pregnant at age <20 were twice as likely to quit smoking during pregnancy (aOR = 2.22; 95% CI, 1.42-3.46), and women aged 20-25 were 1.60 times as likely to quit smoking during pregnancy (aOR = 1.06; 95% CI, 1.03-2.48) (P for linear trend = .009).
Table 2.
Adjusted odds ratios of smoking prevalence and percentage of quitting among a sample of mothers delivering live births (n = 30 667), NHANES, United States, 1985-2014a
| Characteristic | Maternal Smoking, aOR (95% CI) | P Valueb | Smoking Cessation, aOR (95% CI) | P Valueb |
|---|---|---|---|---|
| Calendar/birth year (continuous) | 0.97 (0.96-0.98)c | <.001 | 1.02 (0.98-1.07)d | .33 |
| Age of mother at time of delivery, y | .004 | .009 | ||
| <20 | 1.23 (0.93-1.62) | 2.22 (1.42-3.46) | ||
| 20-25 | 1.11 (0.90-1.36) | 1.60 (1.03-2.48) | ||
| 26-35 | 0.85 (0.69-1.05) | 1.40 (0.96-2.06) | ||
| >35 | 1.00 [Reference] | 1.00 [Reference] | ||
| Race/ethnicity | <.001 | .48 | ||
| Non-Hispanic white | 4.11 (3.38-4.99) | 0.89 (0.63-1.24) | ||
| Hispanic | 0.55 (0.44-0.69) | 1.23 (0.79-1.90) | ||
| Non-Hispanic black | 1.00 [Reference] | 1.00 [Reference] | ||
| Othere | 1.91 (1.42-2.57) | 1.00 (0.52-1.93) | ||
| Sex of child | .83 | .51 | ||
| Female | 0.99 (0.89-1.09) | 1.07 (0.87-1.33) | ||
| Male | 1.00 [Reference] | 1.00 [Reference] |
Abbreviations: aOR, adjusted odds ratio; NHANES, National Health and Nutrition Examination Survey.
a The question “Did biological mother smoke at any time while she was pregnant with the survey participant?” was asked during 1999-2014. The question “At any time during the pregnancy, did biological mother quit or refrain from smoking for the rest of the pregnancy?” was asked during 1999-2008 only. Data source: National Center for Health Statistics, Centers for Disease Control and Prevention.13 Child’s age was included to control for recall bias caused by memory failure of the proxy (usually the mother). Residual confounding may remain because memory failure may not be equal between smokers and nonsmokers.
b P values for age of mother were generated for the linear trend, and all other P values were estimated from global Wald χ2 test because of the nominal nature of the variables. Two-sided P values < .05 were considered significant.
c Adjusted odds of being a smoker during pregnancy for a 1-year increase in time.
d Adjusted odds of quitting smoking any time during pregnancy for a 1-year increase in time.
e Other includes all other races including mixed race.
Discussion
Spanning more than 2 decades, these nationally representative data indicate a steady decline in the rate of pregnancy-related smoking through 2014. This prevalence rate of smoking among pregnant woman was similar to the rates reported in other sources for various years,6,8,17 including the prevalence rate used in Healthy People 2020 baseline data.3 We also showed a significant trend in smoking cessation during pregnancy. However, at the current pace, the projected prevalence of smoking during pregnancy in 2020 is expected to be 6.1%, which is higher than the Healthy People 2020 target of 1.4% (ie, 98.6% of females delivering a live birth who report abstaining from smoking cigarettes during pregnancy in the year 2020).3 Among the 4 age groups examined, pregnant women aged >35 were the least likely to quit smoking and pregnant women aged <20 were the most likely to quit smoking; however, women aged <20 also had the highest prevalence of maternal smoking. This finding is consistent with the findings of Curtin and Mathews, who used data from the 2003 US Standard Certificate of Live Birth and observed that women and girls aged <20 had the highest rates of smoking cessation before (26.4%) and during (27.2%) pregnancy and the second-highest rates of smoking before (13.5%) and during (10.1%) pregnancy. Women aged 20-24 had the highest prevalence of smoking during pregnancy (13.0%).18
Highlighted by the data for our study is a need to revitalize strategies to change the smoking behaviors of pregnant women, ideally during preconception. In addition to proven comprehensive tobacco control programs, financial incentives (eg, lowering out-of-pocket costs for cessation treatments as part of contingency management interventions) have had success in increasing smoking cessation among pregnant women.6 Since 2014, the Affordable Care Act has precluded states from excluding tobacco cessation drugs from coverage for traditional Medicaid enrollees. It also mandates that employers provide health insurance coverage and not impose any cost-sharing requirements for counseling and pharmacotherapy for tobacco cessation and other effective evidence-based preventive services.19 As a result, the prevalence of smoking among women of childbearing age may decline more sharply and should be evaluated in a timely manner to fine-tune current smoking control strategies.
Limitations
This study had several limitations. First, the overall prevalence of smoking among pregnant women may be underestimated because NHANES surveyed live births and did not sample children who may have been institutionalized because of severe medical consequences of maternal smoking. Second, responses were collected via mothers’ self-reporting and may have been subject to social desirability bias, thereby resulting in nondisclosure. Hence, self-reports may need to be validated using biomarkers of smoking exposure. In a study comparing self-reports with serum cotinine levels, Dietz and colleagues20 observed that rates of nondisclosure of smoking were higher among pregnant women who were active smokers than among nonpregnant women who were active smokers and that this nondisclosure of smoking was highest among pregnant women aged 20-24. Their findings suggest that up to 25% of pregnant women who smoke may not self-report smoking during pregnancy. On the basis of the potential for nondisclosure, it is possible that the observed smoking and smoking cessation trends in our study were a product of inflated rates (ie, underreporting of smoking and overreporting of smoking cessation) influenced by increasing efforts to promote smoking cessation during pregnancy.21 In contrast with the high nondisclosure rates observed by Dietz et al, in a retrospective study involving a cohort of women 8-10 years after giving birth, Liu et al22 found that maternal recall of tobacco smoking was in excellent agreement with medical records (κ = 0.6-1.00). Similarly, Pickett et al23 observed that women had accurate and reliable recall of their smoking behavior during pregnancy more than 10 years after the pregnancy. However, unlike the nationally representative sample in the study by Dietz et al,20 samples in the Liu et al22 and Pickett et al23 studies were regional. Finally, we did not exclude data collected from proxies other than biological mothers. Proxies who were not the biological mother may not have known the behaviors of the biological mothers and, therefore, may have contributed to underreporting or overreporting of smoking. However, about 90% of the interviewees were biological mothers in NHANES 1988-1994,24 and the US Census Bureau reported that about 95% of children live with their biological mother.25 Hence, we anticipated a similar percentage of biological mothers acting as proxies in our study.
Conclusions
As we observe the 50th anniversary of the landmark surgeon general’s report on smoking,26 the tobacco control movement is at a critical juncture. Given the evolving nature of smoking control strategies in general, ongoing surveillance will be crucial, and national trends in smoking prevalence among women of childbearing age, perinatal women in particular, will need to be monitored. To foster effective perinatal tobacco control and reduce the intergenerational effects of maternal smoking, efforts are needed to further reduce the number of young women who initiate smoking. Frontline clinical care providers can play a role in identifying women who smoke and referring them to appropriate treatment. By collecting data on smoking from women of childbearing age and providing them with cessation and relapse interventions, the burden of pregnancy-related smoking in the United States could be further reduced.
Acknowledgments
The authors thank Hongxia Li for technical assistance with the analysis and figure.
Footnotes
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Dietz PM, England LJ, Shapiro-Mendoza CK, Tong VT, Farr SL, Callaghan WM. Infant morbidity and mortality attributable to prenatal smoking in the U.S. Am J Prev Med. 2010;39(1):45–52. [DOI] [PubMed] [Google Scholar]
- 2. Mathews TJ. Smoking during pregnancy in the 1990s. Natl Vital Stat Rep. 2001;49(7):1–14. [PubMed] [Google Scholar]
- 3. Office of Disease Prevention and Health Promotion, US Department of Health and Human Services. Healthy People 2020 topics and objectives: maternal, infant, and child health. https://www.healthypeople.gov/2020/topics-objectives/topic/maternal-infant-and-child-health/objectives . Accessed January 12, 2014.
- 4. National Center for Health Statistics, Centers for Disease Control and Prevention. National Vital Statistics System: datasets and related documentation for birth data. https://www.cdc.gov/nchs/nvss/birth_methods.htm. Published 2015. Accessed May 25, 2018.
- 5. Ventura SJ, Hamilton BE, Mathews TJ, Chandra A. Trends and variations in smoking during pregnancy and low birth weight: evidence from the birth certificate, 1990-2000. Pediatrics. 2003;111(5, pt 2):1176–1180. [PubMed] [Google Scholar]
- 6. Tong VT, Dietz PM, Morrow B, et al. Trends in smoking before, during, and after pregnancy—Pregnancy Risk Assessment Monitoring System (PRAMS), United States, 40 sites, 2000-2010. MMWR Surveill Summ. 2013;62(SS06):1–19. [PubMed] [Google Scholar]
- 7. National Cancer Institute. Cancer trends progress report, 2009/2010 update. https://progressreport.cancer.gov/sites/default/files/archive/report2009.pdf. Published April 2010. Accessed January 4, 2014.
- 8. Ebrahim SH, Floyd RL, Merritt RK II, Decoufle P, Holtzman D. Trends in pregnancy-related smoking rates in the United States, 1987-1996. JAMA. 2000;283(3):361–366. [DOI] [PubMed] [Google Scholar]
- 9. Cook J, Owen P, Bender B, et al. State-specific prevalence of cigarette smoking among adults, and children’s and adolescents’ exposure to environmental tobacco smoke—United States, 1996. MMWR Morb Mortal Wkly Rep. 1997;46(44):1038–1043. [PubMed] [Google Scholar]
- 10. Pub L No. 91-452, 84 Stat 941 (1970).
- 11. Glantz SA, Barnes R, Eubanks SY. Compromise or capitulation? US Food and Drug Administration jurisdiction over tobacco products. PLoS Med. 2009;6(7):e1000118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. National Center for Health Statistics, Centers for Disease Control and Prevention. National Health and Nutrition Examination Survey. https://wwwn.cdc.gov/nchs/data/nhanes/2015-2016/manuals/2016_Interviewer_Procedures_Manual.pdf. Updated 2018. Accessed June 7, 2018.
- 13. National Center for Health Statistics, Centers for Disease Control and Prevention. National Health and Nutrition Examination Survey: questionnaires, datasets, and related documentation: early childhood module, 1999-2014. https://wwwn.cdc.gov/nchs/nhanes/default.aspx. Accessed May 18, 2018.
- 14. US Census Bureau. How the Census Bureau measures poverty. https://www.census.gov/topics/income-poverty/poverty/guidance/poverty-measures.html. Accessed July 1, 2016.
- 15. Bloom B, Cohen RA, Freeman G. Summary health statistics for U.S. children: National Health Interview Survey, 2008. Vital Health Stat. 2009;10(244):1–81. [PubMed] [Google Scholar]
- 16. SAS Institute, Inc. SAS Version 9.3. Cary, NC: SAS Institute, Inc; 2011. [Google Scholar]
- 17. Martin JA, Hamilton BE, Sutton PD, et al. Births: final data for 2005. Natl Vital Stat Rep. 2007;56(6):1–103. [PubMed] [Google Scholar]
- 18. Curtin SC, Mathews TJ. Smoking prevalence and cessation before and during pregnancy: data from the birth certificate, 2014. Natl Vital Stat Rep. 2016;65(1):1–14. [PubMed] [Google Scholar]
- 19. US 111th Cong, HR 3590 §4205 (2010).
- 20. Dietz PM, Homa D, England LJ, et al. Estimates of nondisclosure of cigarette smoking among pregnant and nonpregnant women of reproductive age in the United States. Am J Epidemiol. 2011;173(3):355–359. [DOI] [PubMed] [Google Scholar]
- 21. Chamberlain C, O’Mara-Eves A, Oliver S, et al. Psychosocial interventions for supporting women to stop smoking in pregnancy. Cochrane Database Syst Rev. 2013;(10):CD001055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Liu J, Tuvblad C, Li L, Raine A, Baker LA. Medical record validation of maternal recall of pregnancy and birth events from a twin cohort. Twin Res Hum Genet. 2013;16(4):845–860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Pickett KE, Kasza K, Biesecker G, Wright RJ, Wakschlag LS. Women who remember, women who do not: a methodological study of maternal recall of smoking in pregnancy. Nicotine Tob Res. 2009;11(10):1166–1174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Zhang J, Muldoon MF, McKeown RE, Cuffe SP. Association of serum cholesterol and history of school suspension among school-age children and adolescents in the United States. Am J Epidemiol. 2005;161(7):691–699. [DOI] [PubMed] [Google Scholar]
- 25. US Census Bureau. Historical living arrangements of children. https://www.census.gov/data/tables/time-series/demo/families/children.html. Published November 2017. Accessed June 6, 2018.
- 26. US Department of Health and Human Services. The Health Consequences of Smoking–50 Years of Progress: A Report of the Surgeon General. Atlanta, GA: Office on Smoking and Health, National Center for Chronic Disease Prevention and Health Promotion, Centers for Disease Control and Prevention, US Department of Health and Human Services; 2014. https://www.surgeongeneral.gov/library/reports/50-years-of-progress/index.html. Accessed May 12, 2018. [Google Scholar]