Abstract
Objectives:
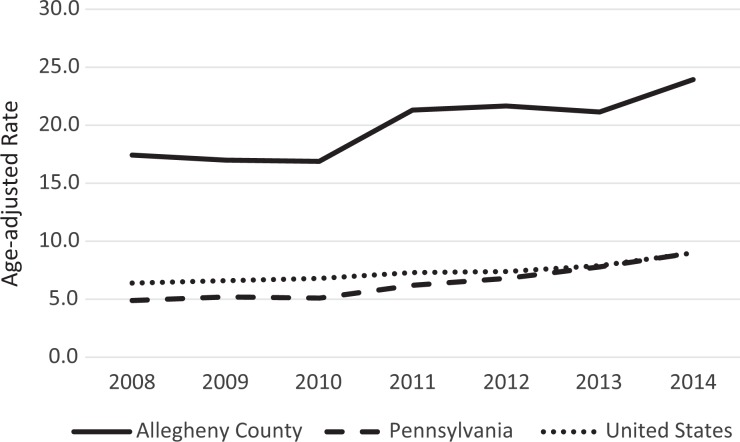
In Allegheny County, Pennsylvania, the incidence of opioid-related overdose deaths increased from 17.4 per 100 000 population in 2008 to 23.9 per 100 000 population in 2014. Our objectives were to describe local demographic characteristics of this epidemic, identify public human services targets for intervention, determine temporal relationships between use of public human services and overdose mortality, and provide recommendations about potentially beneficial interventions.
Methods:
We used autopsy data from the Allegheny County Medical Examiner to link people who died of overdoses from 2008 through 2014 to their premortem incarcerations and use of mental health services and substance use disorder services. We calculated the frequency of use of public human services by decedents and the interval between the last use of these services and overdose death.
Results:
Of the 1399 decedents, 957 (68.4%) had a public human service encounter before overdose death. Of these 957 decedents, 531 (55.5%) had ever been incarcerated, 616 (64.4%) had ever used a mental health service, and 702 (73.4%) had ever used a substance use disorder service. Of 211 decedents incarcerated in the year before their overdose death, 54 (25.6%) overdosed within 30 days of their last release from jail. Of 510 decedents using mental health services in the year before death, 231 (45.3%) overdosed within 30 days of their last use of the services. Of 350 decedents using substance use disorder services in the year before their overdose death, 134 (38.3%) overdosed within 30 days of their last use of the services.
Conclusions:
Merging data on overdose mortality with data on use of public human services can be a useful strategy to identify trends in, and factors contributing to, the opioid epidemic; to target interventions; and to stimulate collaboration to address the epidemic.
Keywords: criminal justice, human services, opioid overdoses
During 2008-2016, more than 236 000 people died from opioid overdoses in the United States.1-4 Efforts to curtail the epidemic have ranged from new policies to make naloxone more available, to prescription drug monitoring programs, to improved access to medication-assisted treatment for those who are opioid addicted.5 However, few health departments have been able to curtail the epidemic. Because of this lack of success and the relatively recent entrance of fentanyl and its derivatives into the heroin marketplace, the overdose death rate has continued to rise.3,4,6,7
Pennsylvania has been heavily affected. The rate of opioid-related overdose deaths in the state increased from 4.9 per 100 000 population in 2008 to 18.5 per 100 000 population in 2016.6,8 In Allegheny County, Pennsylvania, a jurisdiction of more than 1.2 million people that includes the city of Pittsburgh, the rate of opioid-related overdose deaths per 100 000 population has increased steeply, from 17.4 in 2008 to 23.9 in 2014 and to 46.0 in 2016. More than 3400 people in Allegheny County died from opioid-related overdoses from 2008 through 2016.9,10
Collaborators across Allegheny County, including nonprofit organizations, government entities, health care insurers and providers, and substance use disorder providers, have been working together on various interventions to slow the epidemic. They have improved surveillance, increased access to naloxone for first responders and substance use disorder providers, joined with insurers and health providers to reduce the number of opioid prescriptions written, and expanded access to medication-assisted treatment. In addition, Pennsylvania implemented a prescription drug monitoring program, provided standing orders for naloxone, and in January 2018 declared the opioid crisis a public health emergency.11 Other local partners also have collaborated on numerous reports, including one by the US Attorney for Western Pennsylvania’s Working Group on Drug Abuse and Addiction.12 However, despite these efforts, the epidemic has continued to grow. By 2014, as fentanyl and its derivatives had become more widely available, overdose fatalities had surged.13
In 2015, to better understand the epidemic and possibly identify additional opportunities for intervention, the Allegheny County Health Department and the Allegheny County Department of Human Services (ACDHS) conducted a study of opioid overdose decedents. The objectives of our study were to (1) describe the demographic characteristics and extent of the opioid epidemic in Allegheny County; (2) identify possible points for intervention, recognizing that overdose decedents may have used various public human services before their death; (3) determine the temporal relationship between overdose mortality and incarceration or the use of mental health or substance use disorder services; and (4) recommend potentially beneficial interventions.
Methods
We matched Allegheny County Medical Examiner autopsy data from 2008 through 2014 to public human services data from the ACDHS Data Warehouse.14 In Allegheny County, by law, all cases of unnatural or unexplained deaths come to the medical examiner’s office. Full autopsies are performed for most of these cases, but for some cases, only an external examination is performed or biological samples are taken. The medical examiner also issues death certificates for people who die of overdose and are not brought into the office or who die in hospitals. In these situations, investigators are trained to ask about any drug history or involvement in drug activity. For the purposes of this study, autopsy data included information on all opioid-related overdose deaths (ie, full autopsies, external examination cases, and cases that were not brought into the office).
People who died from an opioid-related overdose and who had a record of an encounter with a public system in the data warehouse were considered matched, and those who died from an overdose and whose death records were not found in the data warehouse were considered unmatched.
Data Sources
Medical examiner death data
We used autopsy reports from the Allegheny County Medical Examiner’s Office to identify people who died in Allegheny County from an opioid-related overdose from 2008 through 2014. We obtained data on the address of the overdose incident, the address of the decedent’s most recent residence, and the types of drugs found in the decedent’s blood, urine, or hair at the time of death that contributed to the death. Because more than 1 drug is usually found in people who die of drug overdose, we recorded all drugs found. We defined an opioid-related overdose death as an accidental overdose death in which an opioid (eg, methadone, oxycodone, fentanyl, heroin) was the primary cause or a contributing factor. Accidental deaths are identified by a thorough review of all scene, law enforcement, and family information acquired by a staff of forensic investigators. Drugs are considered to be a contributory factor if an overriding primary cause is identified, such as a death from blunt force trauma—motor vehicle accident or fall—where drugs are found at autopsy.
Human services data
We obtained data on use of mental health services and substance use disorder services, Medicaid enrollment, incarceration, involvement with child welfare services, and use of homelessness services from the ACDHS Data Warehouse.14 This unique electronic repository, created in 1999, is a central repository of social and human services data on ACDHS clients and the services they receive through ACDHS and other public entities. It contains more than 1.4 billion records on more than 1.2 million unique clients, and it includes data from 29 sources. The sources include both internal ACDHS programs and external programs, ranging from Medicaid-funded and county-funded mental health services and substance use disorder services, to programs that involve aging, public benefits, housing, criminal justice, and public schools.9 The warehouse does not include data on physical health. It links records of people from various sources via a matching algorithm, using data elements including first and last name, date of birth, social security number, and demographic information, to create a master person index. For our study, we used only 6 types of data: Medicaid enrollment, use of mental health services, use of substance use disorder services, use of child welfare services, use of (housing authority) homelessness services, and incarcerations, because these were the areas of interest for investigation. Four of the types of records we used from the data warehouse dated to 2003, although the child welfare records dated to 2002, and homelessness records generally date to 2005.
Characteristics
We used death certificate data to determine race (categorized as white, black, or other) and sex (male or female). For age, which we also obtained from death certificates, we used predefined age categories in 5- and 10-year increments (eg, 10-14, 15-19, 20-24, 25-34 years) corresponding to those used by human services systems.
We defined enrollment in Medicaid (called HealthChoices in Pennsylvania) as having been enrolled in Medicaid ≥1 day in the 90 days before death. We defined incarceration as having had ≥1 episode of incarceration in Allegheny County Jail ever and in the year before death.
We reviewed records to determine whether encounters with publicly funded services occurred among people having a primary mental health disorder or substance use disorder diagnosis as defined in the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV)15 (complete list of codes is available from authors upon request). We defined use of mental health services as having ever had ≥1 encounter with a mental health diagnosis. We further categorized people who had a mental health diagnosis in the year before death. Similarly, we defined use of substance use disorder services as having ever had ≥1 encounter with a substance use disorder diagnosis. We further categorized people who had an encounter in the year before death. We subclassified use of mental health services by type of service, including formal clinical services, peer services, or other supportive behavioral health services (ie, case management). We subclassified use of substance use disorder services by type of service, including inpatient, outpatient, detoxification, or other service. We defined use of child welfare services as any encounter with child welfare services as an adult caregiver in the 5 years before death. We defined use of justice support services as any encounter ever with services provided through the Allegheny County Adult Justice Related Services Program to those who had mental illness and were incarcerated within the criminal justice system. We defined use of homelessness services as any accessing of those services in the 5 years before death.
Data Analysis
Analysis of demographic characteristics
We conducted descriptive analyses of age, sex, and race for matched and unmatched populations. We also calculated age-adjusted opioid-related overdose death rates for Allegheny County. We compared these rates with those for Pennsylvania and the United States during the same period; we obtained these data from the Kaiser Family Foundation.8
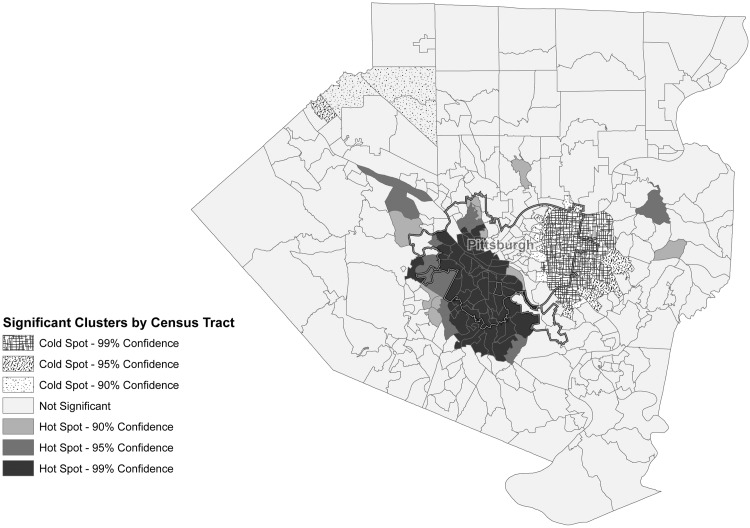
Geographic analysis
We geocoded and mapped the location of fatal opioid-related overdoses for the entire Allegheny County population, by census tract (n = 395), from 2008 through 2014, using ArcGIS version 10.3.16 We conducted a hot-spot analysis to identify census tract–level spatial clusters of fatal overdose counts that were higher than counts in the rest of the county by using the hot-spotting tool in ArcGIS version 10.3.17 ArcGIS calculated confidence intervals (CIs) of 99%, 95%, and 90%. We also conducted a separate analysis to assess traveling distance between where the person lived and died for Allegheny County residents.
Matching autopsy data with data from the ACDHS data warehouse
After matching data, we determined the numbers and types of human services encounters and then aggregated the totals for each type of encounter. We calculated frequencies and 95% CIs for demographic characteristics in both the matched and unmatched populations, and we compared these populations by using the Pearson χ2 test. For these comparisons, we set significance at α = .05. Once matched, we calculated frequencies for other characteristics (ie, Medicaid enrollment, use of mental health and substance use disorder services, and incarceration in the county jail) in the matched population. We conducted a separate analysis to assess the number of days between overdose death and the most recent mental health service, the most recent substance use disorder service, and the most recent incarceration in the year before the overdose death.
Results
Demographic Characteristics
From 2008 through 2014 in Allegheny County, 1399 cases met the definition of an opioid-related overdose death. Of those, 1355 (96.9%) deaths were Allegheny County residents, 1250 (89.3%) were among white people, 952 (68.0%) were among males, and 800 (57.2%) were among people aged 35-59 (Table 1). The Allegheny County age-adjusted rate of opioid-related overdose deaths rose from 16.9 per 100 000 population in 2010 to 23.9 per 100 000 population in 2014 (Figure 1).
Table 1.
Deaths among all people who died of an opioid-related overdose, the matched population, and unmatched population, by demographic characteristics, Allegheny County, Pennsylvania, 2008-2014a
| Demographic Characteristics | All | Matched Populationb | Unmatched Populationb | |||
|---|---|---|---|---|---|---|
| No. | % (95% CI) | No. | % (95% CI) | No. | % (95% CI) | |
| Total | 1399 | 100 | 957 | 100 | 442 | 100 |
| Race/ethnicity | ||||||
| White | 1250 | 89.3 (87.7-90.9) | 851 | 88.9 (86.8-90.8) | 399 | 90.3 (87.2-92.8) |
| Black | 141 | 10.1 (8.6-11.7) | 100 | 10.4 (8.6-12.5) | 41 | 9.3 (6.8-12.3) |
| Hispanic | 3 | 0.2 (0.1-0.6) | 2 | 0.2 (0-0.7) | 1 | 0.2 (0-1.1) |
| Asian | 4 | 0.3 (0.1-0.7) | 3 | 0.3 (0.1-0.9) | 1 | 0.2 (0-1.1) |
| Other | 1 | <0.1 | 1 | 0.1 (0-0.5) | 0 | 0 |
| Sex | ||||||
| Male | 952 | 68.0 (65.6-70.5) | 664 | 69.4 (66.4-72.2) | 288 | 65.2 (60.6-69.5) |
| Female | 447 | 32.0 (29.4-34.4) | 293 | 30.6 (27.8-33.6) | 154 | 34.8 (30.5-39.4) |
| Age, y | ||||||
| 0-4 | 1 | <0.1 | 1 | 0.1 (0-0.5) | 0 | 0 |
| 5-9 | 0 | 0 | 0 | 0 | 0 | 0 |
| 10-14 | 6 | 0.4 (0.2-0.9) | 4 | 0.4 (0.1-1.0) | 2 | 0.5 (0.1-1.5) |
| 15-19 | 54 | 3.9 (2.9-5.0) | 36 | 3.8 (2.7-5.1) | 18 | 4.1 (2.5-6.2) |
| 20-24 | 148 | 10.6 (9.0-12.3) | 98 | 10.2 (8.4-12.3) | 50 | 11.3 (8.6-14.6) |
| 25-34 | 351 | 25.2 (22.8-27.4) | 232 | 24.2 (21.6-27.0) | 119 | 26.9 (22.9-31.2) |
| 35-44 | 363 | 25.9 (23.7-28.3) | 243 | 25.4 (22.7-28.2) | 120 | 27.1 (23.2-31.4) |
| 45-54 | 362 | 25.9 (23.6-28.2) | 264 | 27.6 (24.8-30.5) | 98 | 22.2 (18.5-26.2) |
| 55-59 | 75 | 5.4 (4.3-6.6) | 55 | 5.7 (4.4-7.4) | 20 | 4.5 (2.9-6.8) |
| 60-64 | 29 | 2.1 (1.4-2.9) | 19 | 2.0 (1.2-3.0) | 10 | 2.3 (1.2-4.0) |
| 65-74 | 8 | 0.6 (0.3-1.1) | 5 | 0.5 (0.2-1.2) | 3 | 0.7 (0.1-0.9) |
| 75-84 | 2 | 0.1 (0-0.5) | 0 | 0 | 2 | 0.5 (0-0.7) |
a Allegheny County Medical Examiner autopsy data from 2008-2014 were matched with human services data from Allegheny County Department of Human Services Data Warehouse.9,14
b People who died from an opioid-related overdose and who had a record of an encounter with a public system in the data warehouse composed the matched population, and those who died from an overdose and whose records were not found in the data warehouse composed the unmatched population.
Figure 1.
Age-adjusted opioid-related overdose death rates in Allegheny County, Pennsylvania, and the United States, 2008-2014. Allegheny County age-adjusted opioid-related overdose death rates (per 100 000 population) were calculated by using Allegheny County Medical Examiner data and 2010 population estimates. Age-adjusted opioid-related overdose death rates (per 100 000 population) for Pennsylvania and the United States were obtained from the Kaiser Family Foundation.8
The type of drugs found in decedents’ blood, urine, or hair shifted over time from primarily heroin and prescription opioids before 2014 to also including fentanyl in a substantial number of decedents in 2014. Fentanyl contributed to <20 opioid-related overdose fatalities each year from 2008 through 2013, but it contributed to a high of 20% (52 of 255) of the opioid-related overdose fatalities in 2014. Whereas the incidence of opioid-related overdose deaths steadily increased across all age groups in Allegheny County from 2008 through 2014, the increase in the incidence of these deaths among adults aged 25-34 during this period was particularly steep (from 15 per 100 000 population in 2008 to 46 per 100 000 population in 2014).
Of the 1399 decedents, 957 (68.4%) were matched to data sources (Table 1). In this matched population, 851 (88.9%) decedents were white, 664 (69.4%) were male, and 837 (87.5%) were aged 20-54. We found no significant differences in demographic characteristics between the matched and unmatched populations.
Geospatial Analysis
The highest number of opioid-related overdose deaths in Allegheny County occurred in 8 of the 130 municipalities (Figure 2). Based on the hot-spot analysis of the addresses where overdoses occurred, significant spatial clusters of high counts of fatal overdose incidents were located in the north side and southern parts of Pittsburgh and in communities that border Pittsburgh to the south and the west. In the traveling distance analysis, we found that 1111 of 1355 (82%) people in Allegheny County died from opioid-related overdose deaths within 1 mile of the decedent’s residence.
Figure 2.
Geospatial analysis of the incident address of 1399 opioid-related overdose deaths, by census tract (n = 395), Allegheny County, Pennsylvania, 2008-2014. Hot spots are spatial clusters with significantly higher counts of fatal overdoses compared with counts in the rest of the county, and cold spots are spatial clusters with significantly lower counts of fatal overdoses. The hot spots with the greatest number of opioid-related deaths compared with other municipalities and Pittsburgh neighborhoods were Brookline, Baldwin Township, Carrick, and Overbrook (indicated by solid grays and black toward southwest). The cold spots with the least number of opioid-related deaths were the Pittsburgh neighborhood of Point Breeze and municipality of Wilkinsburg (indicated by patterns toward northeast).
Use of Public Human Services by Decedents in Matched Population
Of the 957 decedents in the matched population, 531 (55.5%) had ever been in the county jail and 211 (22.0%) had been in the county jail in the year before their death (Table 2). In this same population, 616 (64.4%) decedents had ever used a mental health service and 510 (53.3%) decedents had used a mental health service in the year before their death. In addition, 702 (73.4%) decedents had ever used a substance use disorder service, and 350 (36.6%) decedents had used a substance use disorder service in the year before their death. Finally, in the matched population, 624 (65.2%) decedents had been enrolled in HealthChoices in the 90 days before their death.
Table 2.
Use of publicly funded human services and admittance to a county jaila before death among the matched population (n = 957) who died of an opioid-related overdose, Allegheny County, Pennsylvania, 2008-2014b
| Service | People With Past Encounter, No. (%) |
|---|---|
| Enrolled in HealthChoices (Medicaid), in 90 days before death | 624 (65.2) |
| In county jail, ever | 531 (55.5) |
| In county jail, in year before death | 211 (22.0) |
| Used mental health services, ever | 616 (64.4) |
| Used mental health services, in year before death | 510 (53.3) |
| Used substance use disorder services, ever | 702 (73.4) |
| Used substance use disorder services, in year before death | 350 (36.6) |
| Used child welfare services (parents/caregivers), in 5 years before death | 119 (12.4) |
| Used criminal justice support services, ever | 82 (8.6) |
| Used aging services, in 5 years before death | 53 (5.5) |
| Used homelessness services, in 5 years before death | 100 (10.4) |
a Defined as having had ≥1 encounter.
b Allegheny County Medical Examiner autopsy data from 2008-2014 were matched with human services data from the Allegheny County Department of Human Services Data Warehouse.9,14 People who died from an opioid-related overdose and who had a record of an encounter with a public system in the data warehouse composed the matched population.
Of the 211 matched decedents who had been incarcerated in the year before their overdose death, 109 (51.7%) overdosed within 90 days and 54 (25.6%) overdosed within 30 days of their last release from jail (Table 3). Similarly, of the 510 decedents who had used mental health services in the year before their overdose death, 343 (67.3%) overdosed within 90 days and 231 (45.3%) overdosed within 30 days of their last use of the services. Of the 350 decedents who had used substance use disorder services in the year before their overdose death, 195 (55.7%) overdosed within 90 days and 134 (38.3%) overdosed within 30 days of their last use of the services.
Table 3.
Interval between last encounter involving jail, mental health services, or substance use disorder services and opioid-related overdose deaths, among people having an encounter with public human services in the year before death, Allegheny County, Pennsylvania, 2008-2014a
| Interval, Days | People in County Jail in Year Before Death, No. (%) (n = 211) | People Accessing Mental Health Services in Year Before Death, No. (%) (n = 510) | People Accessing Substance Use Disorder Services in Year Before Death, No. (%) (n = 350) |
|---|---|---|---|
| <30 | 54 (25.6) | 231 (45.3) | 134 (38.3) |
| 31-60 | 28 (13.3) | 73 (14.3) | 29 (8.3) |
| 61-90 | 27 (12.8) | 39 (7.6) | 32 (9.1) |
| 91-120 | 10 (4.7) | 31 (6.1) | 22 (6.3) |
| 121-150 | 7 (3.3) | 24 (4.7) | 26 (7.4) |
| 151-180 | 13 (6.2) | 21 (4.1) | 18 (5.1) |
| 181-210 | 15 (7.1) | 24 (4.7) | 16 (4.6) |
| 211-240 | 13 (6.2) | 17 (3.3) | 12 (3.4) |
| 241-270 | 10 (4.7) | 13 (2.5) | 15 (4.3) |
| 271-300 | 19 (9.0) | 13 (2.5) | 16 (4.6) |
| 301-330 | 3 (1.4) | 10 (2.0) | 16 (4.6) |
| 331-365 | 12 (5.7) | 14 (2.7) | 14 (4.0) |
a Allegheny County Medical Examiner autopsy data from 2008-2014 were matched with human services data from Allegheny County Department of Human Services Data Warehouse.9,14 People who died from an opioid-related overdose and who had a record of an encounter with a public system in the data warehouse composed the matched population.
The most common mental health service last received (for those 510 decedents who received those services in the year before death) was outpatient services (including clinical and nonclinical supportive services) by 135 (26.5%) decedents. Other services last received included medication management (n = 98, 19.2%), mental health services in jail (n = 72, 14.1%), inpatient services (n = 66, 12.9%), service coordination (n = 48, 9.4%), and emergency mental health services (n = 26, 5.1%).
The most common substance use disorder service last received (for those 350 who received those services in the year before death) was nonhospital rehabilitation (n = 82, 23.4%). Other services last received included methadone maintenance (n = 62, 17.7%), outpatient treatment (1 hour per week) (n = 57, 16.3%), detoxification (hospital or nonhospital) (n = 42, 12.0%), case management (n = 38, 10.9%), intensive outpatient treatment (3 hours per day, 3 days per week) (n = 18, 5.1%), and partial hospitalization (n = 14, 4.0%).
Discussion
By combining data on opioid-related overdose deaths with data on use of human services in Allegheny County, we gleaned new information that may help guide future interventions. Our results provide a better understanding of the changing demographic characteristics of the opioid epidemic in Allegheny County, of the communities in the county at highest risk for opioid-related overdose deaths, and of the temporal relationships between fatal overdoses and recent jail release and behavioral health encounters.
The demographic characteristics of the opioid overdose epidemic from 2008 through 2014 in Allegheny County were similar to those in the rest of the nation during the same period, including that the most rapidly increasing opioid-related overdose death rates occurred in the cohort aged 25-34.18 This finding is particularly puzzling because opioid use among adolescents seems to be declining.19 With declining rates of opioid use among adolescents, one would expect a decline in opioid-related overdose deaths in the young adult population (those aged 25-34) rather than an increase. Our findings to the contrary suggest that these young adults did not begin their use in adolescence but rather began later in life. Recent hypotheses suggest that these rising rates in the cohort aged 25-34 are due to the effects of negative social determinants of health, such as isolation, economic disadvantage, and hopelessness.20 Those living with these negative social determinants in Allegheny County may be at substantial risk for opioid-related overdose deaths, a situation potentially exacerbated by the escalating use of fentanyl with heroin. Research is needed to better understand what is happening between adolescence and the mid-20 s to cause people aged 25-34 to become opioid users.
Geospatial analysis indicated that the incidence of overdose fatalities was higher in certain communities in Allegheny County than it was in the rest of the county. Community work, including discussions with community members, qualitative research to learn more about on-the-ground issues, and interviews with key stakeholders, is needed to more accurately understand the factors responsible for these findings. In addition, these results suggest the need to work with municipal government leaders to ensure that residents in these communities have ready access to opioid addiction treatment resources and naloxone.
Our finding that the time after incarceration is a period of heightened overdose risk echoes previous research.21-26 In addition, the period after abstinence from drugs is a high-risk time for both relapse and overdose.27 The high risk is likely caused by the loss of drug tolerance that occurs after periods of sobriety. And today, given the strength and increasing presence of fentanyl and its derivatives mixed in with heroin, the risk of overdose in a sober person is likely to be higher than it was in the past.28
The 90 days after using substance use disorder services or mental health services was a period of particularly high risk for opioid-related overdose deaths. Periods after or during substance use disorder treatment, similar to periods after incarceration, may be particularly risky for overdose.27,29,30 As with people leaving jail, people involved in or leaving substance use disorder treatment are more likely than those not in treatment to be abstinent or at least to have reduced their use of opioids, leading to lower tolerance. However, we do not know if all the overdose decedents in our study were in treatment, had received effective treatment, or had left treatment, nor do we know whether they had been abstinent just before their overdose deaths.
We identified a similar pattern of risk during the 90 days after the last use of mental health services. However, unlike what we found with use of substance use disorder services, we were unable to find any reports on increased risk of opioid-related overdose death after the use of mental health services. We found that those who had died of a drug overdose often had contact with mental health services as recently as 30 days before their deaths. This proximity between last use of mental health services and subsequent fatal overdose did generate several pertinent questions: Did mental health providers know their patients were using drugs? Did the providers assess overdose risk? Did the providers provide naloxone? If the patient left treatment, did the providers conduct outreach? Did the providers in Allegheny County have adequate substance use disorder training? Confidentiality laws in Pennsylvania limit communication between those who provide help for substance use disorders and their mental health colleagues, which may substantially affect how much mental health providers know about their patients’ substance use issues. In addition, training in substance use disorders has in general been lacking among mental health providers.31 Thus, more research is needed to determine how mental health professionals and providers of help for substance use disorders can best identify and communicate information about overdose risk, potentially preventing fatal overdoses.
Given the information gleaned from our study, we identified several potential opportunities for intervention. First, the high risk for opioid-related overdose deaths after incarceration suggests that jail-based programs for helping incarcerated people with substance use disorders are needed. The ACDHS enacted one such strategy by providing naloxone to at-risk inmates when they are released from jail. Pilot projects involving medication-assisted treatment, the use of medications approved by the US Food and Drug Administration, and counseling and behavioral therapies are underway in the Allegheny County Jail. Other programs are also being put in place to support the transitions of prisoners into treatment.
Second, the large number of decedents who had encounters with either mental health services or substance use disorder services close to the time of their overdose deaths suggests that these types of encounters may represent an important opportunity for intervention. Effective screening and brief intervention procedures, especially as part of mental health treatment, can identify active drug use and potential overdose risk.32-34 Also, overdose prevention education and naloxone distribution can be core components of safety plans designed for those receiving mental health services. Furthermore, evidence-based medication-assisted treatment, with motivational interviewing or cognitive behavioral treatment combined with appropriate medications (ie, buprenorphine, methadone, or naltrexone), may be offered to help reduce drug use and promote recovery. ACDHS is working with community-based housing, behavioral health, child welfare, and other service providers to adopt many of these strategies to potentially reduce overdose risks.
Third, that we identified communities at high risk for opioid-related overdose deaths suggests that an opportunity exists for the Allegheny County Health Department and the ACDHS to work with stakeholders in those communities to target interventions. The health department is collaborating with these communities to ensure access to naloxone, availability of treatment resources, and access to education. It is also addressing other pertinent factors in the epidemic, ranging from the existence of vacant housing (frequented by drug users) to physician prescribing practices, many of which affect the planning for and implementation of appropriate activities.
Limitations
Our study had several limitations. First, the ACDHS Data Warehouse is a rich source of information, but it does not contain the entire universe of mental health services and substance use disorder services. Thus, data on whether certain services were paid for out-of-pocket or by commercial insurers, for example, were not available. Second, although our matching process specified parameters, rules, and thresholds, we cannot exclude the possibility that some false-negative matches occurred. Similarly, although it is our understanding that all opioid-related overdose deaths are included in the data from the medical examiner, it is possible that some opioid-related overdose deaths were not reported and, thus, are missing from the sample. Third, we did not have access to claims data on physical health services; as such, any data on mental health services or substance use disorder services rendered by primary care physicians would be missing from our study. Fourth, we were unable to ascertain at what point people were in their mental health treatment course or substance use disorder treatment course or anything about the quality of the treatment they were receiving. These may be important aspects of study. Fifth, we did not have data on other factors that might influence overdose risk, such as work and family history. Finally, because this was a descriptive study, we were unable to make inferences about causality.
Conclusions
By combining multiple sources of data in Allegheny County, we described the demographic characteristics of the opioid epidemic in the county, identified communities at highest risk for opioid-related overdose deaths, and clarified the temporal relationships between human services encounters and fatal overdoses. As a result, we identified important opportunities for interventions to address the opioid-related overdose epidemic in Allegheny County. These results led to the Allegheny County Health Department and the ACDHS prioritizing naloxone distribution at key points in users’ lives (including when they are released from jail, during mental health treatment, and when involvement in substance use disorder services is concluding). Efforts are also underway to provide medication-assisted treatment during incarceration and through primary care providers. Furthermore, outreach by others to high-risk communities has stimulated local efforts that range from coalition development (among key stakeholders, including health care providers, law enforcement, community leaders, and parents) to drug take-back programs (programs that collect unused drugs and destroy them). Finally, active surveillance and analysis of incoming data continue. We urge other counties to conduct similar analyses linking their death and human services data to provide an enhanced picture of the opioid epidemic and highlight local opportunities for intervention.
Acknowledgments
The authors thank Catherine Jensen and Qitang Wang for their analytical support of this research. The authors also thank Karl E. Williams, MD, MPH, chief medical examiner of Allegheny County, for providing data and explanation.
Footnotes
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Centers for Disease Control and Prevention. Prescription opioid overdose data. 2017. https://www.cdc.gov/drugoverdose/data/overdose.html. Accessed December 3, 2017.
- 2. Kaiser Family Foundation. Opioid overdose deaths by gender. 2018. https://www.kff.org/other/state-indicator/opioid-overdose-deaths-by-gender/?currentTimeframe=0&selectedDistributions=total&sortModel=%7B%22colId%22:%22Location%22,%22sort%22:%22asc%22%7D. Accessed August 27, 2018.
- 3. Rudd RA, Aleshire N, Zibbell JE, Gladden RM. Increases in drug and opioid overdose deaths—United States, 2000-2014. MMWR Morb Mortal Wkly Rep. 2016;64(50-51):1378–1382. [DOI] [PubMed] [Google Scholar]
- 4. Rudd RA, Seth P, David F, Scholl L. Increases in drug and opioid-involved overdose deaths—United States, 2010-2015. MMWR Morb Mortal Wkly Rep. 2016;65(5051):1445–1452. [DOI] [PubMed] [Google Scholar]
- 5. Centers for Disease Control and Prevention. Opioid overdoses. 2018. https://www.cdc.gov/drugoverdose/index.html. Accessed January 14, 2018.
- 6. Drug Enforcement Agency, Philadelphia Division, University of Pittsburgh School of Pharmacy. Analysis of overdose deaths in Pennsylvania, 2016. 2017. https://www.duq.edu/assets/Documents/forensics/Forensic%20Fridays/OCT%2027/Handouts/DEA-PHL-DIR-034-17%20Analysis%20of%20Overdose%20Deaths%20in%20Pennsylvania%202016A[4080].pdf. Accessed September 6, 2018.
- 7. Warner M, Chen LH, Makuc DM. Increase in fatal poisonings involving opioid analgesics in the United States, 1999-2006. NCHS Data Brief. 2009;22:1–8. [PubMed] [Google Scholar]
- 8. Kaiser Family Foundation. Opioid overdose death rates and all drug overdose death rates per 100,000 population (age-adjusted). 2016. https://www.kff.org/other/state-indicator/prescription-opioid-overdose-deaths-and-death-rate-per-100000-population-age-adjusted/?activeTab=map¤tTimeframe=0&selectedDistributions=prescription-opioid-overdose-deaths&sortModel=%7B%22colId%22:%22Location%22,%22sort%22:%22asc%22%7D. Accessed June 26, 2018.
- 9. Allegheny County. Allegheny County analytics. 2017. https://www.alleghenycountyanalytics.us. Accessed December 3, 2017.
- 10. Hulsey EB, Brink L, Dalton E, et al. Opioid-Related Overdose Deaths in Allegheny County; Risks and Opportunities for Intervention. Pittsburgh, PA: Allegheny County Department of Human Services and Allegheny County Health Department; 2016. [Google Scholar]
- 11. Pennsylvania Department of Drug and Alcohol Programs. The department’s focus on addressing overdose. Updated March 2018 http://www.ddap.pa.gov/overdose/Pages/Department%20Focus%20on%20Addressing%20Overdose.aspx. Accessed September 6, 2018.
- 12. Miller T, Lauer A, Mihok B, Haywood K. Continuum of Care Approach: Western Pennsylvania’s Response to the Opioid Epidemic. Pittsburgh, PA: Institute of Politics, University of Pittsburgh; 2016. [Google Scholar]
- 13. Centers for Disease Control and Prevention. Synthetic opioid overdose data. 2016. https://www.cdc.gov/drugoverdose/data/fentanyl.html. Accessed December 3, 2017.
- 14. Allegheny County Department of Human Services. Allegheny County Data Warehouse. Updated 2018 https://www.alleghenycountyanalytics.us/index.php/dhs-data-warehouse. Accessed July 15, 2018.
- 15. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 4th Edition (DSM-IV). Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- 16. ESRI. ArcGIS Version 10.3. Redlands, CA: ESRI; 2016. [Google Scholar]
- 17. ESRI. ArcGIS Version 10.3: Hot Spot Analysis. Redlands, CA: ESRI; 2016. http://giscollective.org/tutorials/gis-techniques/spatial-statistics/hot-spot-analysis. Accessed June 13, 2018. [Google Scholar]
- 18. Hedegaard H, Chen LC, Warner M. Drug-poisoning deaths involving heroin: United States, 2000-2013. NCHS Data Brief. 2015;190:1–8. [PubMed] [Google Scholar]
- 19. Hu MC, Griesler P, Wall M, Kandel DB. Age-related patterns in nonmedical prescription opioid use and disorder in the US population at ages 12-34 from 2002 to 2014. Drug Alcohol Depend. 2017;177:237–243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Dasgupta N, Beletsky L, Ciccarone D. Opioid crisis: no easy fix to its social and economic determinants. Am J Public Health. 2018;108(2):182–186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Binswanger IA, Nowels C, Corsi KF, et al. Return to drug use and overdose after release from prison: a qualitative study of risk and protective factors. Addict Sci Clin Pract. 2012;7:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Binswanger IA, Stern MF, Deyo RA, et al. Release from prison—a high risk of death for former inmates. N Engl J Med. 2007;356(2):157–165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Binswanger IA, Stern MF, Yamashita TE, Mueller SR, Baggett TP, Blatchford PJ. Clinical risk factors for death after release from prison in Washington State: a nested case-control study. Addiction. 2016;111(3):499–510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Bird SM, Hutchinson SJ. Male drugs-related deaths in the fortnight after release from prison: Scotland, 1996-99. Addiction. 2003;98(2):185–190. [DOI] [PubMed] [Google Scholar]
- 25. Leach D, Oliver P. Drug-related death following release from prison: a brief review of the literature with recommendations for practice. Curr Drug Abuse Rev. 2011;4(4):292–297. [DOI] [PubMed] [Google Scholar]
- 26. Seaman SR, Brettle RP, Gore SM. Mortality from overdose among injecting drug users recently released from prison: database linkage study. BMJ. 1998;316(7129):426–428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Strang J, McCambridge J, Best D, et al. Loss of tolerance and overdose mortality after inpatient opiate detoxification: follow up study. BMJ. 2003;326(7396):959–960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. American Addiction Centers. Fentanyl vs. heroin: the similarities and differences between two powerful opioids. 2018. https://americanaddictioncenters.org/fentanyl-treatment/similarities/#overdose. Accessed July 14, 2018.
- 29. Sordo L, Barrio G, Bravo MJ, et al. Mortality risk during and after opioid substitution treatment: systematic review and meta-analysis of cohort studies. BMJ. 2017;357:j1550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Warner-Smith M, Darke S, Lynskey M, Hall W. Heroin overdose: causes and consequences. Addiction. 2001;96(8):1113–1125. [DOI] [PubMed] [Google Scholar]
- 31. Rasyidi E, Wilkins JN, Danovitch I. Training the next generation of providers in addiction medicine. Psychiatr Clin North Am. 2012;35(2):461–480. [DOI] [PubMed] [Google Scholar]
- 32. Fuster D, Cheng DM, Wang N, et al. Brief intervention for daily marijuana users identified by screening in primary care: a subgroup analysis of the ASPIRE randomized clinical trial. Subst Abus. 2016;37(2):336–342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Saitz R, Alford DP, Bernstein J, Cheng DM, Samet J, Palfai T. Screening and brief intervention for unhealthy drug use in primary care settings: randomized clinical trials are needed. J Addict Med. 2010;4(3):123–130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Saitz R, Palfai TP, Cheng DM, et al. Screening and brief intervention for drug use in primary care: the ASPIRE randomized clinical trial. JAMA. 2014;312(5):502–513. [DOI] [PMC free article] [PubMed] [Google Scholar]