Abstract
This study aimed to perform a systematic review and meta-analysis of the literature to determine the effects of the use of mouthguards (MGs) on cardiopulmonary capacity in athletes (oxygen uptake: VO 2 max, and minute ventilation: VE max). Seven electronic databases and reference lists of relevant papers were searched for randomized clinical trials (RCTs) that compared the cardiopulmonary capacity in athletes with and without the use of an MG. The risk of bias tool of the Cochrane Collaboration was used for quality assessment. Fourteen studies were included. For both the overall VO2 max and VE max analyses, significant differences were observed between the MG and no MG conditions, favoring no MG, which presented the highest VO2 max values (p=0.0001; 95% CI; –2.638 to –1.728) and the highest VE max values (p=0.0001; 95% CI; –4.103 to –1.354). When the results were analyzed separately for each subgroup (type of MG and place of use), the meta-analysis showed that the effect of the use of an MG on VO2 max and VE max was not significant when custom-made MGs were used. The use of an MG overall decreased VO2 max and VE max compared to the control. Nevertheless, custom-made MGs seem to have no effect on these parameters.
Key words: sports, mouth protectors, pulmonary gas exchange
Introduction
The practice of contact sports, such as rugby, hockey, boxing, martial arts, basketball, handball, soccer, and others can lead to an increased risk of orofacial injuries 3 16 23 25 . Thus, it has been recommended to use mouthguards (MG) during practice. They are designed to minimize the occurrence and severity of oral and dental injuries through the absorption of the energy associated with blows to the mouth 5 29 40 . Besides orofacial trauma prevention, some MGs also may offer mandibular repositioning 14 31 .
On the other hand, despite the clear potential of MGs to reduce the risk of injury, some athletes find it difficult to wear MGs because of instability, oral dryness, difficulties in breathing and speaking, nausea, and the perception that it hinders their performance 8 11 30 .
There are different types of MGs and they can be divided into three main types: custom-made, stock, and boil-and-bite. Custom-made MGs are fabricated personally for each individual using a model of the patient’s mouth, usually taken by a dental professional. These MGs are more expensive than other versions but usually offer a better fit. Stock MGs are inexpensive and come preformed. They are essentially plastic trays that fit loosely over the teeth. Also available commercially, boil-and-bite MGs are made from a thermoplastic material that is immersed in hot water and then formed in the mouth by the athlete using finger, tongue and biting pressure 34 . The type of MG may impact the athlete’s comfort and ability to speak or breathe during activities 10 21 .
Previous clinical studies assessed the effect of the use of different types of MGs on some physiological parameters, such as gas exchange, muscle strength, agility, and others. Garner and McDivitt 20 found the use of an MG promotes an increase of oropharynx width and diameter and a decrease of lactate levels during endurance exercises, suggesting the airway openings could contribute to performance enhancement. However, this finding remains controversial in the literature because Bailey et al. 4 did not observe differences in gas exchange if an MG was used.
There are different parameters that could be used to assess the cardiopulmonary capacity, for example, respiratory oxygen uptake (VO 2 ), carbon dioxide production (VCO 2 ), and ventilatory measures during a symptom-limited exercise test 1 . Oxygen consumption increases with activity and there is an upper limit during exercise requiring maximal effort. Maximal VO 2 is defined as the point at which no further increase in measured VO 2 occurs despite an increase in work rate (a plateau is reached) during graded exercise testing 33 . Direct measures of VO 2 are reliable, reproducible, and provide the most accurate assessment of functional capacity. Thus, VO 2 max has become the preferred laboratory measure of cardiorespiratory fitness and is the most important measurement during functional exercise testing 1 .
The minute ventilation increases at times of stress and exercise. This increase compensates for the increase in the demand of oxygen and the increased production of carbon dioxide.
Due to the conflicting results of the available clinical trials, a systematic review was conducted with the aim of answering the following focused question: Does the use of an MG affect cardiopulmonary capacity in athletes?
Methods
Protocol and registration
This systematic review was registered on the Prospero database and was performed according to PRISMA (Preferred Reporting Items for Systematic Review and Meta-Analysis) guidelines ( http://www.prisma-statement.org ).
Information sources and search
To identify clinical trials to be included for this review, the topic was searched (up until June, 2016) on the electronic databases MEDLINE (via PubMed), Scopus, Web of Science, Latin American and Caribbean Health Sciences Literature (LILACS), Brazilian Library in Dentistry (BBO), and The Cochrane Library ( Table 1 ). An expert librarian guided the whole search strategy. The reference lists of all primary studies were hand-searched for additional relevant publications. No restrictions were placed on the publication date or language. For the abstracts and manuscripts in languages other than English, a native speaker performed the translation. A “Search Alert” with the search strategy in the PubMed, Scopus, and Web of Science databases was created and the search was updated weekly for six months after the first search.
Table 1 Electronic database and search strategy (15 Jun 2016).
| Pubmed | |
|---|---|
| #1 (Sports[MeSH Terms] OR Sport*[Title/Abstract] OR Athletic*[Title/Abstract] OR Athlete*[Title/Abstract] OR Player*[Title/Abstract]) | #2 (Mouth protectors[MeSH Terms] OR Protectors Mouth[Title/Abstract] OR Guards Mouth[Title/Abstract] OR Mouthguard*[Title/Abstract] OR Mouth guard*[Title/Abstract] OR Mouth Protector*[Title/Abstract] OR Mouth piece OR Mouthpiece*[Title/Abstract]) |
| #1 AND #2 | |
| Scopus | |
| #1 TITLE-ABS-KEY ( sports OR sport OR athletic OR athletics OR athlete OR athletes OR player OR players ) | #2 TITLE-ABS-KEY ( “Mouth protectors” OR “Protector Mouth” OR “Protectors Mouth” OR “Guards Mouth” OR Mouthguard OR Mouthguards OR “Mouth Protector” OR “Mouth Protectors” OR “Mouth Piece” OR “Mouth Pieces” OR Mouthpiece OR Mouthpieces OR “Mouth guard” OR “Mouth guards” ) |
| #1 AND #2 | |
| Web of Science | |
| #1 TOPIC=(Sports OR Sport OR Athletic OR Athletics OR Athlete OR Athletes OR Player OR Players) | #2 TOPIC=(Mouth protectors” OR “Protector Mouth” OR “Protectors Mouth” OR “Guards Mouth” OR Mouthguard OR “Mouthguards” OR “Mouth Protector” OR “Mouth Protectors” OR “Mouth Piece” OR “Mouth Pieces” OR Mouthpiece OR Mouthpieces OR “Mouth guard” OR “Mouth guards”) |
| #1 AND #2 | |
| Lilacs and BBO | |
| #1(MH:Sports or Sports or Desportes or Deportes or Athletics or “Atividades Esportivas” or “actividades deportivas”) | #2 (MH: “mouth protectors” or “Protetores da Boca” or “Peças Protetoras da Boca” or “Protetor bucal” or “Protectores Bucales” ) |
| #1 AND #2 | |
| Cochrane Library | |
| #1 | MeSH descriptor: [Sports] explode all trees |
| #2 | Sport* or Athletic*or Athlete*or Player* |
| #3 | #1 or #2 |
| #4 | MeSH descriptor: [Mouth Protectors] explode all trees |
| #5 | Protector Mouth or Protectors Mouth or Guards Mouth or Mouthguard or Mouthguards or Mouth Protector* or Mouth Piece* or Mouthpiece* or Mouth guard* |
| #6 | #4 or #5 |
| #7 | #3 and #6 |
The grey literature was searched using the System for Information on Grey Literature in Europe (SIGLE) database. Dissertations and theses were explored using the ProQuest Dissertations and Theses Full-Text database as well as the Periódicos Capes Theses database.
The search strategies defined for the databases described above are listed in Table 1 . The search strategy was appropriately modified for each database and performed by two reviewers to identify eligible studies. Full-text versions of the papers that appeared to meet the inclusion criteria were retrieved for further assessment and data extraction.
Eligibility criteria
The inclusion criteria outlines, according to the population, interventions, comparisons, and outcomes (PICOS), were performed as follows:
Population (P): Adult athletes;
Intervention (I): Use of an MG during sports practice;
Comparison (C): The intervention should be compared with non-use of an MG during sports practice;
Outcome (O): Cardiopulmonary capacity (VO 2 max , oxygen uptake; VE max , minute ventilation).
The null hypothesis stated that there is no difference between the use and non-use of an MG during sport practice.
Only randomized clinical trials (RCTs) comparing cardiopulmonary capacity during sports practice of adult individuals with and without an MG were eligible.
VO 2 max and VE max were the outcomes evaluated. At least one of these parameters should be assessed in each included manuscript. No restrictions regarding settings (academic university department, sports clubs, hospital, etc.) were established. Non-controlled clinical trials, pilot studies, historical reviews, editorial letters, in vitro studies, cohort, observational and descriptive studies, such as case reports and case series, were excluded. Additionally, RCTs were excluded if: (1) indirect measurement of VO 2 max and VE max were performed; and (2) there was a lack of an adequate control group.
Study selection and data collection process
All electronically identified records were scanned by title and abstract. Articles appearing in more than one database search were considered only once. Two examiners independently performed the search process. In case of a discrepancy, a decision was made by consensus with a third author. Full texts were obtained for all articles identified and judged as being potentially relevant. A manual search was performed of the references in the included studies.
Data were extracted using customized extraction forms and the following data were recorded for each included study: (1) details of the study, including author(s) and year of publication; (2) details of participants, including number, age, gender, sport type, and anthropometric data; (3) details of the interval among tests; (4) details of the type of MG used; (5) details of the arch used; and (6) details of the outcomes, including VO 2 max (ml/Kg/min or L/min) and VE max (L/min).
For absent data, the correspondence author and/or co-author were contacted in order to send the requested data. Requests were sent via electronic message.
Risk of bias in individual studies
Two review authors independently undertook the risk of bias assessment for the included trials. Disagreements were solved by discussion with a third review author until a consensus was reached. The assessment was carried out according to the criteria described in Chapter 8 of the Cochrane Handbook for Systematic Reviews of Interventions 26 . The assessment criteria contained six items: sequence generation, allocation concealment, blinding of the outcome assessors, incomplete outcome data, selective outcome reporting, and other possible sources of biases. This study considered the interval between physical tests as another possible source of bias. Three out of the six domains in the Cochrane risk of bias tool were considered the key domains for the assessment of the studies´ risk of bias. Studies were considered to be at ‘low’ risk of bias if missing outcome data were well managed, they were free of selective reporting, and a minimum of 24 h occurred between physical tests. When the study was judged as ‘unclear’ in their key domains, attempts were made to contact authors to obtain more information and allow a definitive judgment of ‘yes’ or ‘no’.
The overall risk of bias of the included studies was categorized and reported according to the following:
Low risk of bias (plausible bias unlikely to seriously alter the results) if all key domains were assessed as a low risk of bias;
Unclear risk of bias (plausible bias that raises some doubt about the results) if one or more key domains were assessed as an unclear risk of bias; or
High risk of bias (plausible bias that seriously weakens confidence in the results) if one or more key domains were assessed as a high risk of bias.
Summary measures and synthesis of results
For the meta-analysis, only the data from VO 2 max in ml/Kg/min were considered. In studies where VO 2 max was reported in L/min, the data was requested in ml/Kg/min. Data of VO 2 max in L/min were included only in the systematic review and the data were presented as a descriptive analysis. For the meta-analysis, VO 2 max (ml/Kg/min) and VE max (L/min) data (means and standard deviations) for MG vs. control were pooled and the subgroups analyzed. Pooled analyses took into account all included studies, and subgroup analyses assessed the different types of MG (boil-and-bite, custom-made, and stock) and the arch used (upper, lower, and upper/lower jaw). All analyses were conducted in Comprehensive Meta-Analysis Software 3.2 (Biostat, Englewood, NJ, USA) using a fixed-effect model. Pooled effect estimates were obtained by comparing the mean values of VO 2 max and VE max and were expressed as the raw mean difference among the groups. A p- value≤0.05 was considered statistically significant (Z-test). Statistical heterogeneity of the treatment effect among studies was assessed via the Cochran Q test, with a threshold p value of 0.1, and the inconsistency I 2 test, in which values>50% were considered indicative of high heterogeneity. For studies that evaluated more than one MG, each type was considered independently (subgrouped) for each evaluated parameter (VO 2 max and VE max ).
Results
Study selection
After the database screening and removal of duplicates, 1,070 studies were identified ( Fig. 1 ). After title screening, 65 studies remained and this number was reduced to 20 after careful examination of the abstracts. One study was included after ‘search alert’ updated the search. The full texts of these 21 studies were assessed to check if they were eligible. Among them seven were excluded due to the following reasons: (1) lack of adequate control 2 13 27 ; (2) indirect assessment of studied parameters 9 37 38 ; and (3) data presented graphically 32 .
Fig. 1.
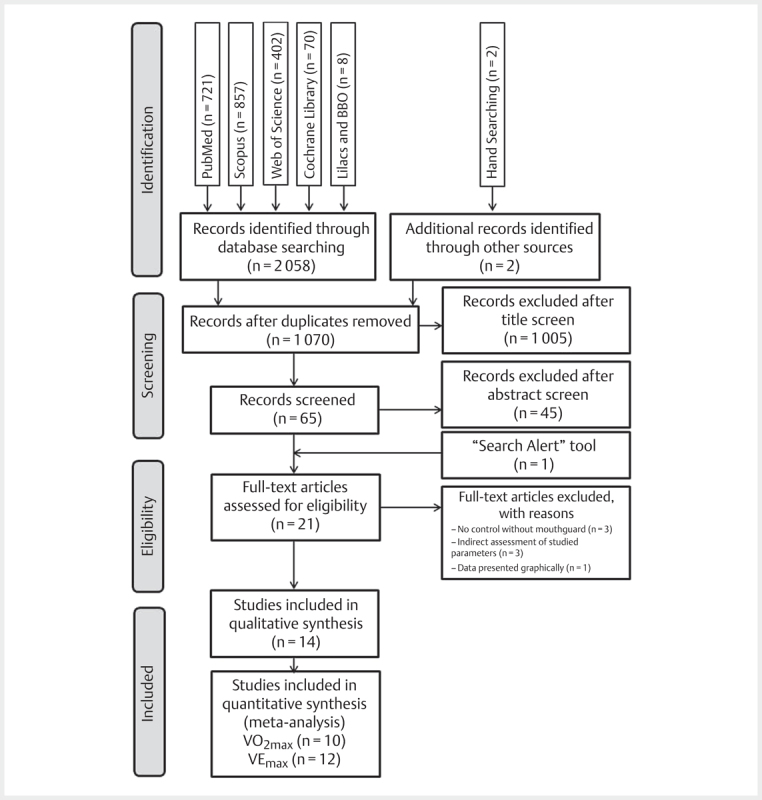
Flow Diagram of the study.
Study characteristics
The characteristics of the 14 selected studies are listed in Table 2 . All the studies that met the inclusion criteria were randomized controlled trials published in English between December 1991 and December 2015. All studies were cross-over designed. Seven studies 4 7 15 22 36 41 45 recruited male participants, two studies 10 39 recruited female participants, four studies 17 21 28 44 recruited participants of both genders, and one study 19 did not report the gender of participants. The number of athletes included in these studies ranged from 7 to 28 participants. The range of age of the athletes was 16–37 years old. Eight studies reported each sport the athletes participated in. The interval between exercise tests varied from 24 h to 10 days. The type of mouthguard also varied among the retrieved studies. Eight studies 10 21 28 32 36 41 44 45 compared the use of one type of MG with no MG. However, some studies 4 7 15 17 19 22 39 tested more than one type of MG. There was variability with respect to MG placement. Six studies 4 7 15 22 28 41 tested MGs placed over the upper jaw, two studies 19 21 tested MGs placed over the lower jaw, four studies 10 17 36 39 tested MGs placed over the upper and lower jaws, and two studies 44 45 did not report where the MG was placed. There was a great variability of the protocol of maximal exercise tests. Some studies presented the absolute data of VO 2 max in L/min 4 7 41 . The relative data in ml/Kg/min was requested, however only one author 7 answered the request. In regards to the outcomes, one study 45 assessed only VO 2 max ; the others 4 7 10 15 17 19 21 22 28 36 39 41 44 assessed both parameters.
Table 2 Summarized data collected from the selected studies.
| First Author, Year | # of subjects (gender) | Sports | Subjects’ age mean±SD [range] (yrs.), | Anthropometric data Height mean±SD (cm) Body mass±SD (Kg) Body mass index±SD (Kg m −2 ) | Interval between tests | Type of MG (description according to the studies) | Area (arch) | Cardiopulmonary Capacity | |
|---|---|---|---|---|---|---|---|---|---|
| VO 2 max Mean±SD | VE max (L/min) | ||||||||
| Bailey, 2015 4 | 15 (male) | n.r. | 24±1 [n.r] | n.r±n.r. n.r±n.r. 25.2±0.9 | At least 1 week | - (MG1) traditional boil-and-bite; - (MG2) “vented” boil-and-bite | Upper | (L/min) C*– 3.49±0.13 MG1 –3.48±0.13 MG2 –3.48±0.17 | C – 123.29±6.21 MG1 –121.94±6.45 MG2 –113.16±7.66 |
| Bourdin, 2006 7 | 19 (male) | 2 Handball, 1 ice hockey, 16 rugby | 27±4.8 [n.r.] | 180.9±8.7 91.4±18.6 n.r.±n.r. | At least 2 days | - (MG1) self-adapted thermoplastic (boil-and-bite) - (MG2) custom-made methyl methacrylate resin | Upper | (ml/Kg/min) C – 47.1±9.18 MG1 – 48.2±9.03 MG2 – 48.1±9.46 (15 subjects) | C – 144.2±19.76 MG1 – 147.4±17.21 MG2 – 148.2±18.06 (15 subjects) |
| Delaney, 2005 10 | 12 (female) | Ice hockey | 19.8±0.8 [n.r.] | 166.8±7.2 63.8±6.6 n.r.±n.r. | Average of 6.8 days | - (MG1) boil-and-bite | Upper and lower | (ml/Kg/min) C – 52.4±0.8 MG1 – 48.8±0.7 | C – 114.1±3.8 MG1 – 108.5±4.0 |
| El-Ashker, 2015 15 | 18 (male) | Elite boxer | 19.4±2.01 [17.8–24.2] | 174±7.9 74.5±5.1 n.r.±n.r. | 6–10 days | - (MG1) custom- fitted: ethylene vinyl acetate copolymer sheets, with standard thickness 4 mm - (MG2) stock MG | Upper | (ml/Kg/min) C – 47.37±5.34 MG1 – 46.48±3.65 MG2 – 40.54±5.68 | C – 99.51±13.42 MG1 – 95.71±14.82 MG2 – 92.74±11.26 |
| Francis, 1991 17 | 10 (male) 7 (female) | n.r. | 27.2±5.2 [20–37] | 175.51±9.65 72.72±15.59 n.r.±n.r. | 24–48 h | - (MG1) unfitted, made of a soft rubberized material - (MG2) unfitted, made of the same material and construction as MG - (MG3) bimaxillary guard composed of a more rigid vinyl material with a small breathing hole between the upper and lower plates. | MG1 – upper MG2 and MG3 – upper and lower | (ml/Kg/min) C – 30.46±4.37 MG1 – 27.38±5.34 MG2 – 28.1±3.47 MG3 –27.39±5.68 | C – 50.98±19.72 MG1 – 43.57±9.47 MG2 – 44.63±12.98 MG3 – 41.34±14.24 |
| Garner, 2011 21 | 13 (male) 3 (female) | n.r. | 21.2±0.75 [18–21] | 176.37±7.3 75.2±12.96 n.r.±n.r. | 2–3 days | - (MG1) custom-fitted | Lower | (ml/Kg/min) C1 – 24.8±5.8 MG1 – 31.19±7.5 (14 subjects) | C – 58.3±13.7 MG1 – 56.9±11.5 (14 subjects) |
| Garner, 2015 19 | 21 (n.r.) | n.r. | n.r. [18–21] | n.r. n.r. n.r. | At least 3 days | - (MG1) boil-and-bite - (MG2) polypropylene, custom-fit - (MG3) ethylene vinyl acetate, custom-fit | Lower | (ml/Kg/min) C – 30.59±3.24 MG1– 29.98±4.42 MG2– 30.59±4.76 MG3– 30.64±4.35 (16 subjects) | C – 45.60±7.50 MG1 – 42.93±7.11 MG2 – 46.02±8.60 MG3 – 45.26±7.67 (16 subjects) |
| Gebauer, 2011 22 | 27 (male) | Hockey or water polo | 23.5±3.8 [n.r.] | 182±0.08 81.7±8.6 24.6±2.1 | 1 week | - (MG1) custom laminated MG with normal palatal surface - (MG2) custom laminated MG with palatal coverage up to the gingival margin | Upper | (ml/Kg/min) C – 56.09±4.82 MG1 – 57.22±6.14 MG2 – 56.76±6.33 | C – 124.19±15.62 MG1 –122.51±18.80 MG2 –124.22±14.68 |
| Kececi, 2005 28 | 11 (male) 11 (female) | Elite taekwondo athletes | 16±1.11 [14–17] | n.r.±n.r. n.r.±n.r. n.r.±n.r. | 48 h | - (MG1) custom- made EVA | Upper | (ml/Kg/min) C – 51.79±2.12 MG1– 52.73±1.81 | C – 106.32±5.75 MG1 – 108±4.41 |
| Piero, 2015 36 | 10 (male) | Amateur road cyclists | 34±6 [n.r.] | 178±7 70±10 22±2 | 1 week | - (MG1) custom-made | Upper and lower | (ml/Kg/min) C – 57.8±6.5 MG1 – 58.1±5.8 | C – 140±23 MG1 – 141±22 |
| Rapisura, 2010 39 . | 11 (female) | n.r. | 22±3.3 | 159.8±4.3 n.r. 63.7±8.9 | Average of 9.1 days | - (MG1) universal self-adapted MG (boil-and-bite) - (MG2) self-adapted MG made for women (boil-and-bite) | MG1 – upper MG2 – upper and lower | (mll/Kg/min) C – 31.0±6.7 MG1 – 30.4±7.1 MG2 – 29.6±5.4 | C – 68.5±17.3 MG1 – 64.7±13.2 MG2 – 56.8±6.4 |
| von Arx, 2008 41 | 13 (male) | n.r. | 22±n.r. [18–27] | n.r.±n.r. n.r.±n.r. n.r.±n.r. | 48 h | - (MG1) multiple-EVA pressure-laminated MG | Upper | (L/min) C – 3.29±0.36 MG1 – 3.16±0.49 | C – 112.9±28.3 MG1 – 105.3±17.8 |
| Wenta, 2014 44 | 6 (male) 1 (female) | n.r. | 19.4±1.6 [n.r.] | 175±2 5 79.4±8.89 n.r. | 7 days | - (MG1) self-adapted (boil-and-bite) | n.r. | (ml/Kg/min) C – 27.8±n.r. MG1 – 27.9±n.r. | C – 57.75±n.r. MG1 – 56.77±n.r. |
| Yarar, 2013 45 | 8 (male) | Combat sports | 22±2.2 [n.r.] | 173.5±3.38 70.45±8.14 n.r. | 1 week | - (MG1) MG (non-specified) | n.r. | (ml/Kg/min) C – 53.87±6.42 MG1 – 53.37±5.57 | n.r. |
C* – Control (without mouthguard); n.r.: not reported
Risk of bias within studies
The assessment of the risk of bias of the selected studies is presented in Fig. 2 . All studies reported the randomization of the tests’ sequence, but few full-text studies reported the method of randomization employed and how the allocation concealment was performed. Authors were contacted for further information. Seven full texts were considered ‘unclear’ for the method of randomization employed and all of them were considered ‘unclear’ for the allocation concealment.
Fig. 2.
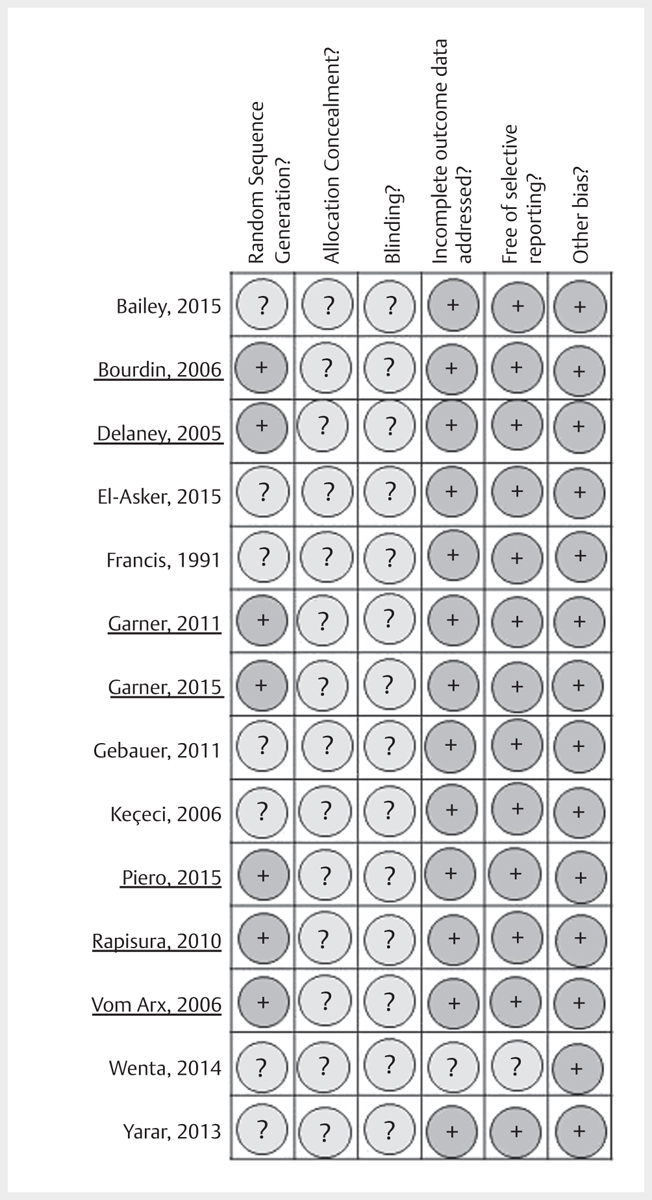
Summary of the risk of bias assessment according to the Cochrane Collaboration tool. Underlined authors provided extra information by e-mail to allow assessment of the risk of bias.
In relation to blinding of participants and evaluators, all included studies were considered ‘unclear’ because all of the studies did not address these outcomes. Nevertheless, since the respiratory assessments were performed during exercise tests, with or without use of MG, blinding would not be possible both for subjects and examiners. In the assessment of the domain “incomplete outcome data”, only one abstract 44 was considered to be ‘unclear’, because no information about dropouts was reported. Only three 7 19 21 of the 14 studies included in the qualitative analysis were missing outcome data. Despite this, they were considered as ‘low’ risk of bias for this domain because the reason for the missing outcome data was not related to the true outcome: the expiratory volumes of subjects were underestimated in one session because of full face mask displacement due to sweating.
Regarding selective reporting, all studies were considered ‘low’ risk of bias ( Fig. 2 ) because the study protocol was available, and all of the studies’ outcomes were reported, except for the one abstract 44 judged as ‘unclear’. Regarding other sources of bias, all studies were considered ‘low’ risk of bias, because there was a minimum interval of 24 h between exercise tests.
Incomplete outcome data, selective reporting, and other sources of bias were considered as key domains for this systematic review. In summary, from the 14 studies, only one abstract 44 was considered ‘unclear’ in the key domains of the Cochrane risk of bias tool.
Synthesis of the results: meta-analyses
For the meta-analysis, studies were grouped according to the kind of outcome used to report cardiopulmonary capacity (VO 2 max or VE max ). This resulted in a total of 10 studies 7 10 15 17 19 21 22 28 36 39 , which reported both outcomes and were included in the two pooled meta-analyses. Two studies 4 41 were included only in the pooled meta-analysis of VE max because the data for VO 2 max were in L/min.
For the pooled analysis of VO 2 max (each type of MG vs. control), 18 data sets were considered (subgroups), although 10 studies were included ( Fig. 3 ). It was observed that a statistical difference (p<0.05) between conditions (MG x no MG) favored the control group, which presented the higher VO 2 max values. The heterogeneity parameter I 2 was 79.344%. For the pooled analysis of VE max (each type of MG vs. control), 21 data sets were considered, although 12 studies were included ( Fig. 4 ). A statistical difference (p<0.001) was observed between conditions (MG x no MG) favoring the control group, which presented the higher VE max values. The heterogeneity parameter I 2 was 35.647%.
Fig. 3.

Forest Plot of Pooled and Subgroup Analysis of VO 2max .
Fig. 4.
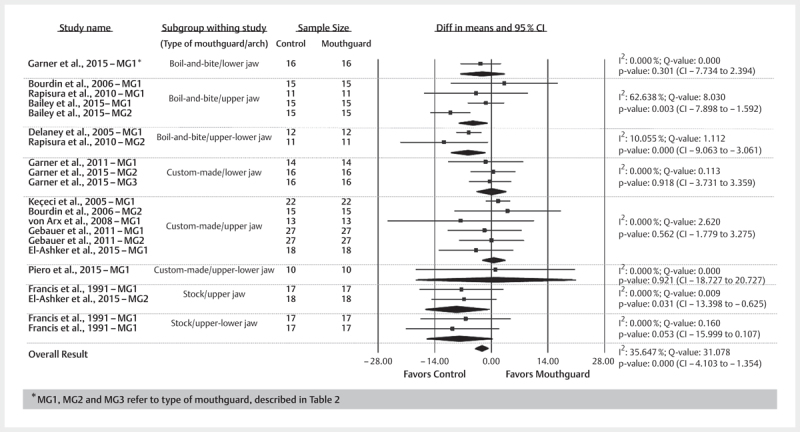
Forest Plot of Pooled and Subgroup Analysis of VE max .
When the results were analyzed separately for each subgroup (type of MG and arch used), the meta-analysis showed that the effect of the use of MG on VO 2 max was not significant when some types of MGs were used (boil-and-bite/lower jaw, boil-and-bite/upper jaw, custom-made/upper jaw, custom-made/lower jaw, custom-made/upper-lower jaw) compared to control. The subgroup analysis of VE max showed that the use of custom-made MGs had no effect on this parameter compared to control. For subgroup analyses, the heterogeneity parameter I 2 was predominantly low.
Discussion
The current systematic review and meta-analysis results rejected the null hypothesis.
The main finding of this meta-analysis is that the use of an MG overall adversely affects cardiopulmonary capacity when compared with not using an MG. However, when the types of MGs were subgrouped, this effect did not occur for some types. Nevertheless, no MG improved cardiopulmonary capacity.
Due the difficulties in finding articles that assessed several variables, the authors chose to assess VO 2 and VE. Besides proper reporting of cardiopulmonary capacity and performance, these parameters were the most commonly evaluated in the studies. In this meta-analysis, assessments of VO 2 and VE at maximal effort were included. Some studies 4 7 10 15 19 21 22 39 also evaluated these parameters at a submaximal effort, thus, sometimes different results were found and could be applicable to sports requiring maximal effort during their practice. Despite the type of sport, the analyses of cardiopulmonary capacity were done with the athletes doing specific exercises for this type of analysis.
All studies included in this systematic review and meta-analysis were cross-over designed. The essential feature distinguishing a cross-over trial from a conventional parallel-group trial is that each patient serves as his/her own control. The cross-over design thus avoids problems of comparability of study and control groups with regard to confounding variables (e. g., age and gender). Moreover, the cross-over design is advantageous regarding the power of the statistical test carried out to confirm the existence of a treatment effect, and it requires lower sample sizes than parallel-group trials. The two trial periods in which the patient receives the different treatments must be separated by a washout phase that is sufficiently long enough to rule out any carry-over effect. In fact, the effect of the first treatment must have disappeared completely before the beginning of the second period 43 . Therefore, the intervals between the exercise tests were considered an important risk of bias.
The mechanisms that could explain the reduction in ventilation and oxygen uptake when MGs are used at the higher workloads still remain unclear. Francis and Brasher 17 observed a decrease in oxygen uptake and minute ventilation when subjects used an MG and hypothesized that MGs caused “pursed-lip breathing” (PLB), which has been shown to improve respiratory efficiency during exercise in people with lung disease. During PLB, less air has to be breathed to absorb a given amount of oxygen. Peak and mean expiratory flow rates are reduced, respiratory rates are decreased, and tidal volume is increased. All these factors result in improved alveolar ventilation and the enhancement of ventilation of previously underventilated areas 6 . However, it is unclear if PLB has similar effects in people with normal lung function. This phenomenon was observed in studies in which some stock and boil-and-bite MGs were tested 15 17 . These MGs are not well fitted and need a contraction of the perioral muscles to be maintained in position.
Gardner and McDivitt 20 observed the use of a boil-and-bite upper MG, which had a greater bite opening, favored an increase in airway diameter and a decrease of blood lactate. As a result, they hypothesized that lactate was reduced because subjects had increased ventilation and thus were better able to eliminate CO 2 . However, this study did not measure gas exchange parameters during the test, so it is unclear if ventilation was increased or decreased during this investigation. Nevertheless, Amis et al. 2 found that custom-made maxillary MGs were unlikely to interfere with breathing at high ventilatory rates and where recruitment of compensatory mechanisms is possible. The degree of such compensation to the presence of an MG may vary considerably between individuals. Thus, although the obstruction associated with wearing an MG can be overcome by most individuals, some subjects may have persistent oral airway obstruction in the presence of an MG. On the other hand, Garner et al. 21 found an improvement of VO 2 and VE when a custom-made mandibular MG was tested. The authors explained that this specific MG did not create any obstruction in breathing.
In the twelve studies included in this meta-analysis, a great variety of MGs were tested. Since some studies revealed that the type of MG could affect the assessed parameters, a subgroup analysis by type and placement of mouthguards was included. By this analysis, custom-made MGs did not affect the assessed parameters. Duarte-Pereira et al. 12 showed that the custom-made MG, compared with the boil-and-bite MG, interferes less with speech, breathing, and oral dryness. It is more comfortable, better adapted, and causes less nausea. For these reasons, custom-made MGs are the favorite and have the highest level of acceptance in most of players.
Stock MGs are inexpensive and come preformed. They are essentially plastic trays that fit loosely over the teeth. Consequently, this type of MG usually does not fit very well, and the mouth should be closed for retention 11 24 . The results of this meta-analysis showed this type of MG negatively affected VO 2 max and VE max . Moreover, according to Patrick et al. 35 , this type of MG offers a less protective effect compared to the boil-and-bite and custom-made MGs.
Since the number of studies testing only lower-jaw mouthguards is small in the MG type subgroups (one study with boil-and-bite 19 , 3 studies with custom-made 19 21 , and no studies with stock), the influence of arch on the studied parameters could not be estimated. This lack of studies may be due to the fact that mouthguards are usually used in the upper jaw in order to provide better protection against tooth trauma.
In a recent systematic review and meta-analysis, Vucic et al. 42 revealed that the average proportion of field hockey players who had sustained at least one dentofacial injury varied from 12.7% among junior and senior players to 45.2% among elite players. They also showed a significantly higher proportion of players regularly wore an MG (84.5%) as compared with players 20 years ago (31.4%). The most common complaints about the MG were that it was unnecessary and uncomfortable. There was an increasing in awareness about the importance of the use of this apparatus against oral injuries. Indeed, for some sports the use of an MG during official competition is mandatory. Besides the protection against oral injuries, some studies have reported increased strength, balance, and coordination as a result of changing the maxillomandibular relationship with an MG 14 36 . Although it has been demonstrated that wearing an MG reduces orofacial injury, many athletes do not wear one during training sessions or in competition for various reasons, including speech and breathing difficulties or discomfort 18 .
Conclusion
Based on this systematic review and meta-analysis, there is scientific evidence showing the use of an MG negatively affects VO 2 and VE at maximal effort. However, custom-made MGs seem to have no effect on these parameters. Therefore, considering the importance of MGs during sport practice, the evidence collected from the present meta-analysis support the use of custom-made MGs.
Acknowledgements
The authors of this study would like to thank the following authors who kindly provided information not available in their full texts: Muriel Bourdin, J. Scott Delaney, Dena Garner, Malpezi Piero, Krystle Rapisura and Thomas von Arx.
Footnotes
Conflict of Interest The authors declare that they have no conflict of interest.
References
- 1.Albouaini K, Egred M, Alahmar A, Wright D J. Cardiopulmonary exercise testing and its application. Postgrad Med J. 2007;83:675–682. doi: 10.1136/hrt.2007.121558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Amis T, Di Somma E, Bacha F, Wheatley J. Influence of intra-oral maxillary sports mouthguards on the airflow dynamics of oral breathing. Med Sci Sports Exerc. 2000;32:284–290. doi: 10.1097/00005768-200002000-00006. [DOI] [PubMed] [Google Scholar]
- 3.Azodo C C, Odai C D, Osazuwa-Peters N, Obuekwe O N. A survey of orofacial injuries among basketball players. Int Dent J. 2011;61:43–46. doi: 10.1111/j.1875-595X.2011.00009.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bailey S P, Willauer T J, Balilionis G, Wilson L E, Salley J T, Bailey E K, Strickland T L. Effects of an over-the-counter vented mouthguard on cardiorespiratory responses to exercise and physical agility. J Strength Cond Res. 2015;29:678–684. doi: 10.1519/JSC.0000000000000668. [DOI] [PubMed] [Google Scholar]
- 5.Bemelmanns P, Pfeiffer P. Shock absorption capacities of mouthguards in different types and thicknesses. Int J Sports Med. 2001;22:149–153. doi: 10.1055/s-2001-11342. [DOI] [PubMed] [Google Scholar]
- 6.Borge C R, Hagen K B, Mengshoel A M, Omenaas E, Moum T, Wahl A K. Effects of controlled breathing exercises and respiratory muscle training in people with chronic obstructive pulmonary disease: results from evaluating the quality of evidence in systematic reviews. BMC Pulm Med. 2014;14:184. doi: 10.1186/1471-2466-14-184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bourdin M, Brunet-Patru I, Hager P E, Allard Y, Hager J P, Lacour J R, Moyen B. Influence of maxillary mouthguards on physiological parameters. Med Sci Sports. 2006;38:1500–1504. doi: 10.1249/01.mss.0000228952.44850.eb. [DOI] [PubMed] [Google Scholar]
- 8.Brionnet J M, Roger-Leroi V, Tubert-Jeannin S, Garson A. Rugby players' satisfaction with custom-fitted mouthguards made with different materials. Community Dent Oral Epidemiol. 2001;29:234–238. doi: 10.1034/j.1600-0528.2001.290310.x. [DOI] [PubMed] [Google Scholar]
- 9.Collares K, Correa M B, da Silva IC M, Hallal P C, Demarco F F. Effect of wearing mouthguards on the physical performance of soccer and futsal players: A randomized cross-over study. Dent Traumatol. 2014;30:55–59. doi: 10.1111/edt.12040. [DOI] [PubMed] [Google Scholar]
- 10.Delaney J S, Montgomery D L. Effect of noncustom birnolar mouthguards on peak ventilation in ice hockey players. Clin J Sport Med. 2005;15:154–157. doi: 10.1097/01.jsm.0000158256.85664.8d. [DOI] [PubMed] [Google Scholar]
- 11.DeYoung A K, Robinson E, Godwin W C. Comparing comfort and wearability: Custom-made vs. self-adapted mouthguards. J Am Dent Assoc. 1994;125:1112–1118. doi: 10.14219/jada.archive.1994.0121. [DOI] [PubMed] [Google Scholar]
- 12.Duarte-Pereira DM V, Del Rey-Santamaria M, Javierre-Garcés C, Barbany-Cairó J, Paredes-Garcia J, Valmaseda-Castellón E, Berini-Aytés L, Gay-Escoda C. Wearability and physiological effects of custom-fitted vs self-adapted mouthguards. Dent Traumatol. 2008;24:439–442. doi: 10.1111/j.1600-9657.2008.00595.x. [DOI] [PubMed] [Google Scholar]
- 13.Duddy F A, Weissman J, Lee R A, Paranjpe A, Johnson J D, Cohenca N. Influence of different types of mouthguards on strength and performance of collegiate athletes: A controlled-randomized trial. Dent Traumatol. 2012;28:263–267. doi: 10.1111/j.1600-9657.2011.01106.x. [DOI] [PubMed] [Google Scholar]
- 14.Dunn-Lewis C, Luk H Y, Comstock B A, Szivak T K, Hooper D R, Kupchak B R, Watts A M, Putney B J, Hydren J R, Volek J S, Denegar C R, Kraemer W J. The effects of a customized over-the-counter mouth guard on neuromuscular force and power production in trained men and women. J Strength Cond Res. 2012;26:1085–1093. doi: 10.1519/JSC.0b013e31824b4d5b. [DOI] [PubMed] [Google Scholar]
- 15.El-Ashker A, El-Ashker S. Cardiopulmonary effects of using mouthguards during medium and high intensities in elite Egyptian boxing athletes. J Phys Educ Sport. 2015;15:15–19. [Google Scholar]
- 16.Emerich K, Nadolska-Gazda E. Dental trauma, prevention and knowledge concerning dental first-aid among Polish amateur boxers. J Sci Med Sport. 2013;16:297–301. doi: 10.1016/j.jsams.2012.10.002. [DOI] [PubMed] [Google Scholar]
- 17.Francis K T, Brasher J. Physiological effects of wearing mouthguards. Br J Sports Med. 1991;25:227–231. doi: 10.1136/bjsm.25.4.227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gardiner D M, Ranalli D N. Attitudinal factors influencing mouthguard utilization. Dent Clin North Am. 2000;44:53–65. [PubMed] [Google Scholar]
- 19.Garner D P. Effects of various mouthpieces on respiratory physiology during steady-state exercise in college-aged subjects. Gen Dent. 2015;63:30–34. [PubMed] [Google Scholar]
- 20.Garner D P, McDivitt E. Effects of mouthpiece use on airway openings and lactate levels in healthy college males. Compend Contin Educ Dent. 2009;30:9–13. [PubMed] [Google Scholar]
- 21.Garner D P, Scheett T P, McDivitt E J. The effects of mouthpiece use on gas exchange parameters during steady-state exercise in college-aged men and women. J Am Dent Assoc. 2011;142:1041–1047. doi: 10.14219/jada.archive.2011.0325. [DOI] [PubMed] [Google Scholar]
- 22.Gebauer D P, Williamson R A, Wallman K E, Dawson B T. The effect of mouthguard design on respiratory function in athletes. Clin J Sport Med. 2011;21:95–100. doi: 10.1097/JSM.0b013e31820428b0. [DOI] [PubMed] [Google Scholar]
- 23.Gialain I O, Coto N P, Dias R B. University student’s dental and maxillofacial fractures characteristics and epidemiology in sports. Acta Sci Health Sci. 2014;36:293–296. [Google Scholar]
- 24.Guevara P H, Hondrum S O, Reichl R B. A comparison of commercially available mouthguards and a custom mouthguard. Gen Dent. 2001;49:402–406. [PubMed] [Google Scholar]
- 25.Hawke J E, Nicholas N K. Dental injuries in rugby football. N Z Dent J. 1969;65:173–175. [PubMed] [Google Scholar]
- 26.Higgins JPT, Green S. Cochrane Handbook for Systematic Reviews of Interventions version 5.1.0: The Cochrane Collaboration. 2011;Available from www.cochrane-handbook.org
- 27.Ishida J I, Wada Y, Imai Y, Hirata Y, Yamashita M, Kirita T. Influence of mouth guards on autonomic nervous system activities: a quantitative study of pupillary flash responses. Oral Sci Int. 2012;9:38–42. [Google Scholar]
- 28.Keçeci A D, Çetin C, Eroǧlu E, Baydar M L. Do custom-made mouth guards have negative effects on aerobic performance capacity of athletes? Dent Traumatol. 2005;21:276–280. doi: 10.1111/j.1600-9657.2005.00354.x. [DOI] [PubMed] [Google Scholar]
- 29.Lieger O, von Arx T. Orofacial/cerebral injuries and the use of mouthguards by professional athletes in Switzerland. Dent Traumatol. 2006;22:1–6. doi: 10.1111/j.1600-9657.2006.00328.x. [DOI] [PubMed] [Google Scholar]
- 30.McClelland C, Kinirons M, Geary L. A preliminary study of patient comfort associated with customised mouthguards. Br J Sports Med. 1999;33:186–189. doi: 10.1136/bjsm.33.3.186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Milani R S, De Periere D D, Lapeyre L, Pourreyron L. Relationship between dental occlusion and posture. Cranio. 2000;18:127–134. doi: 10.1080/08869634.2000.11746124. [DOI] [PubMed] [Google Scholar]
- 32.Morales J, Busca B, Solana-Tramunt M, Miro A. Acute effects of jaw clenching using a customized mouthguard on anaerobic ability and ventilatory flows. Hum Mov Sci. 2015;44:270–276. doi: 10.1016/j.humov.2015.09.008. [DOI] [PubMed] [Google Scholar]
- 33.Nelson N, Asplund C A. Exercise testing: who, when, and why? PM R. 2016;8:S16–S23. doi: 10.1016/j.pmrj.2015.10.019. [DOI] [PubMed] [Google Scholar]
- 34.Newsome P R, Tran D C, Cooke M S. The role of the mouthguard in the prevention of sports-related dental injuries: a review. Int J Paediatr Dent. 2001;11:396–404. doi: 10.1046/j.0960-7439.2001.00304.x. [DOI] [PubMed] [Google Scholar]
- 35.Patrick D G, van Noort R, Found M S. Scale of protection and the various types of sports mouthguard. Br J Sports Med. 2005;39:278–281. doi: 10.1136/bjsm.2004.012658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Piero M, Simone U, Jonathan M, Maria S, Giulio G, Francesco T, Gabriella C, Laura A, Eva B, Gianni M, Francesco C, Giovanni G. Influence of a custom-made maxillary mouthguard on gas exchange parameters during incremental exercise in amateur road cyclists. J Strength Cond Res. 2015;29:672–677. doi: 10.1519/JSC.0000000000000695. [DOI] [PubMed] [Google Scholar]
- 37.Prieto R P, Fernandez-Ranada M B, Gonzalez-Lamuno Leguina D. The influence of mouth protector on max. VO2 and on heart rate in field hockey players. Arch Med Deporte. 2000;17:327–330. [Google Scholar]
- 38.Queiróz AFV R, de Brito R B, Jr, Ramacciato J C, Motta RH L, Flório F M. Influence of mouthguards on the physical performance of soccer players. Dent Traumatol. 2013;29:450–454. doi: 10.1111/edt.12026. [DOI] [PubMed] [Google Scholar]
- 39.Rapisura K P, Coburn J W, Brown L E, Kersey R D. Physiological variables and mouthguard use in women during exercise. J Strength Cond Res. 2010;24:1263–1268. doi: 10.1519/JSC.0b013e3181d1572d. [DOI] [PubMed] [Google Scholar]
- 40.Takeda T, Ishigami K, Mishima O, Karasawa K, Kurokawa K, Kajima T, Nakajima K. Easy fabrication of a new type of mouthguard incorporating a hard insert and space and offering improved shock absorption ability. Dent Traumatol. 2011;27:489–495. doi: 10.1111/j.1600-9657.2011.01029.x. [DOI] [PubMed] [Google Scholar]
- 41.von Arx T, Flury R, Tschan J, Buergin W, Geiser T. Exercise capacity in athletes with mouthguards. Int J Sports Med. 2008;29:435–438. doi: 10.1055/s-2007-965341. [DOI] [PubMed] [Google Scholar]
- 42.Vucic S, Drost R W, Ongkosuwito E M, Wolvius E B. Dentofacial trauma and players’ attitude towards mouthguard use in field hockey: A systematic review and meta-analysis. Br J Sports Med. 2016;50:298–304. doi: 10.1136/bjsports-2015-094896. [DOI] [PubMed] [Google Scholar]
- 43.Wellek S, Blettner M. On the proper use of the crossover design in clinical trials: Part 18 of a series on evaluation of scientific publications. Dtsch Arztebl Int. 2012;109:276–281. doi: 10.3238/arztebl.2012.0276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Wenta M R, Curry D, Havrilla C, Blowers E, Parks K. The effects of mouthguard use on respiratory and aerobic function in college athletes. Med Sci Sports Exerc. 2014;46:741. [Google Scholar]
- 45.Yarar H, Karli U, Aydin K, Erdem H, Uzum H. Effect of using mouth guard on anaerobic and aerobic performance of combat sport athletes. IJSS. 2013;3:719–725. [Google Scholar]


