Abstract
Supplemental Digital Content is available in the text
Editor,
Following delivery, active management of the third stage of labour is an effective strategy to prevent postpartum blood loss, the major cause of avoidable maternal mortality. Importantly, there is a lack of consensus amongst obstetric societies regarding the dosing regimens for oxytocin prophylaxis, with only the British Guidelines making a dose recommendation, advising routine administration of 5 IU oxytocin.1 However, anaesthetists are increasingly aiming for exact physiological control by administering lower doses.2
Efficacy studies that aimed to assess the minimum effective dose in 90% of the population for oxytocin bolus3–5 and an infusion,6,7 all found that a low dose of oxytocin is sufficient to initiate adequate uterine tone for nonlabouring and labouring women undergoing caesarean section. This evidence questions the use of a 5 IU bolus for initiating adequate uterine tone.
However, effectiveness studies are required that examine the use of low-dose oxytocin under real-world conditions as efficacy trials examining dose–responses may overestimate an intervention's effect.3–7 Administering a too low dose may result in uterine atony, which can deteriorate into a major obstetric haemorrhage risking severe maternal morbidity. Moreover, a study that compared four national guidelines for the prevention and management of postpartum haemorrhage identified a need, not only for stronger evidence, but also for more consistent synthesis of the available evidence used to develop guidelines and recommendations, given that obstetric haemorrhage is the leading cause of maternal mortality.1
To address the uncertainty on the effectiveness of low-dose oxytocin, we sought to undertake a systematic review and meta-analysis of data from randomised controlled trials (RCTs). We examined the effectiveness of prophylactic low-dose oxytocin protocols (<5 IU) compared with 5 IU (delivered as a bolus alone, or bolus and continuous infusion, or continuous infusion alone) on the volume of blood loss in women undergoing elective caesarean section.
A systematic review of RCTs from 1946 until March 2017 was conducted according to Preferred Reporting Items for Systematic Reviews and Meta-analyses and an a priori designed protocol. Two independent reviewers (N.C.S.T., D.S.P.) performed a systematic search in PubMed, EMBASE, CENTRAL, CINAHL and Web of Science, and screened the title and abstract of all articles obtained from the search. A research librarian assisted with constructing the search strategy, which combined all synonyms regarding the intervention, ‘oxytocin’ and the domain, ‘caesarean section’ (Supplementary material 1). No limitations were applied to the search. Reference lists from identified studies, associated with the most retrieved citations, were hand-searched to increase the sensitivity of the search. Finally, a search of trial registries including the Australian New Zealand Clinical Trials Registry, ClinicalTrials.gov and the International Clinical Trials Platform was conducted.
Full-length publications of RCTs of patients undergoing elective caesarean section were accepted for systematic review if they compared 5 IU oxytocin with less than 5 IU oxytocin prophylaxis at delivery (whether delivered as a bolus dose, a bolus and continuous infusion or a continuous infusion alone), and reported postpartum blood loss. For the standard-dose group, the total oxytocin dose administered should not exceed 5 IU. For the low-dose group, the total oxytocin dose should be less than 5 IU. Studies were excluded if the population was nonhuman patients who were not undergoing caesarean section, and oxytocin was not investigated. The remaining studies were reviewed in full. There were no restrictions on the language or follow-up duration.
The primary outcome was the mean volume of postpartum blood loss (measured or estimated). The following secondary outcomes were examined. Major obstetric blood loss (measured or estimated blood loss of more than 1000 ml); the use of additional therapeutic uterotonics to supplement the oxytocin intervention (Yes/No); hypotension (a decrease in mean arterial pressure of at least 10% or 10 mmHg); vomiting (the ejection of stomach content); nausea (assessed by directly questioning the patient) (Any/None); adequate uterine tone (uterine tone assessed as adequate by the attending obstetrician) (Yes/No).
A risk of bias assessment and also a data extraction and statistical analysis plan was specified a priori for meta-analysis of the data but was not enacted due to lack of eligible studies and, therefore, is not detailed here (Supplemental material 1).
The literature search returned 10 383 studies (Fig. 1, Supplemental material 1) with 2690 studies excluded due to duplication, resulting in 7693 studies that had been checked for title and abstract. Another 7681 were excluded resulting in 12 studies for full-text review. After full-text review, all 12 were excluded. As no study matched our inclusion criteria, we were not able to analyse our postulated primary outcome criteria.
Fig. 1.
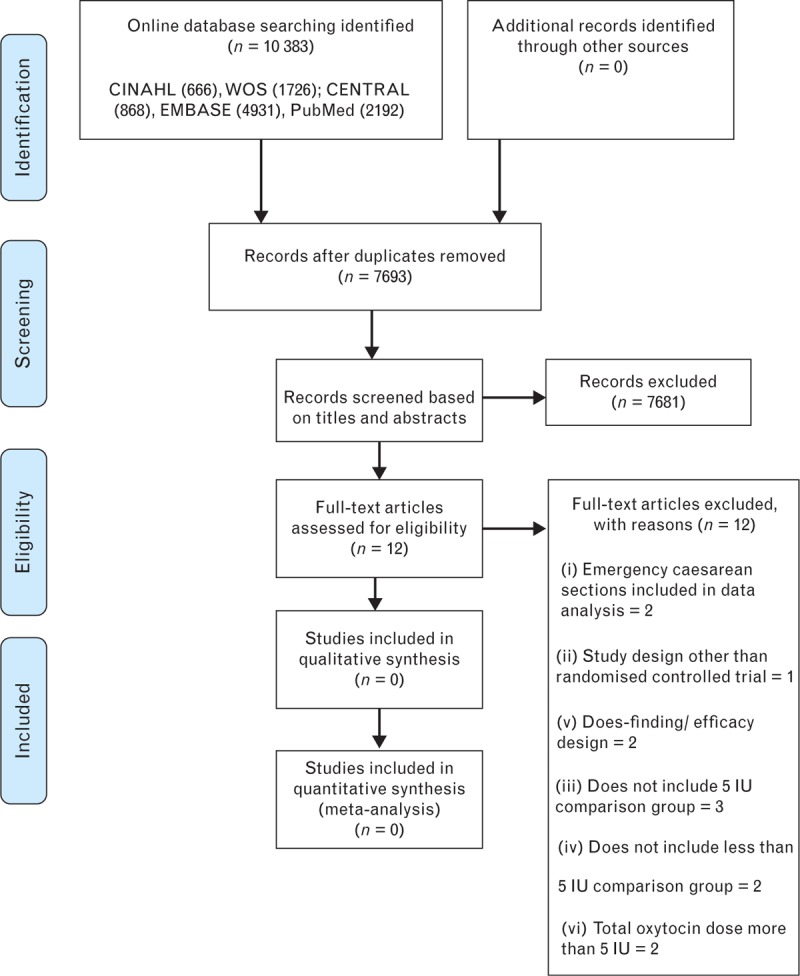
Flow chart of the studies included in the systematic review.
To our knowledge, this is the first systematic review of RCTs that sought to determine the effectiveness of lowering the oxytocin dose on postpartum blood loss in women undergoing elective caesarean section. Remarkably, despite an exhaustive search, no trial investigated exactly the oxytocin regimes under investigation; specifically, the effectiveness of prophylactically administering less than 5 IU doses in comparison with guideline recommended 5 IU on postpartum blood loss. Overall, there was no information for or against the effectiveness of 5 IU oxytocin versus a lower dose on postpartum blood loss.
Several practice surveys have identified significant variation in prophylactic oxytocin regimens (bolus and infusion) used at caesarean section. A national survey of oxytocin use showed that 52% of anaesthesia departments administered between 1 and 3 IU; 21% gave between 5 and 9 IU; 12% gave 10 IU; and 2% administered between 12 and 40 IU prophylactically at caesarean section.8 This suggests that there is a lack of consensus amongst anaesthetists regarding the optimal oxytocin dose regimen and potentially implies a lack of confidence in the evidence supporting effective oxytocin dosing. Notably, many guideline recommendations for the prevention and management of postpartum haemorrhage (16/28; 57%), including the 5 IU dose recommendation, are backed up with weak evidence,1 altogether this paucity of evidence suggests that the perfect oxytocin dose regimen is open for debate.
Supplementary Material
Acknowledgements relating to this article
Assistance with the letter: none.
Financial support and sponsorship: none.
Conflicts of interest: none.
References
- 1.Dahlke JD, Mendez-Figueroa H, Maggio L, et al. Prevention and management of postpartum hemorrhage: a comparison of 4 national guidelines. Am J Obstet Gynecol 2015; 213:76.e1–76.e10. [DOI] [PubMed] [Google Scholar]
- 2.Staikou C, Paraskeva A, Karmaniolou I, et al. Current practice in obstetric anesthesia: a 2012 European survey. Minerva Anestesiol 2014; 80:347–354. [PubMed] [Google Scholar]
- 3.Carvalho JC, Balki M, Kingdom J, et al. Oxytocin requirements at elective cesarean delivery: a dose-finding study. Obstet Gynecol 2004; 104:1005–1010. [DOI] [PubMed] [Google Scholar]
- 4.Butwick AJ, Coleman L, Cohen SE, et al. Minimum effective bolus dose of oxytocin during elective Caesarean delivery. Br J Anaesth 2010; 104:338–343. [DOI] [PubMed] [Google Scholar]
- 5.Balki M, Ronayne M, Davies S, et al. Oxytocin requirements at cesarean section for failure to progress in labor: a dose-finding study. Anesthesiology 2005; 102:A10–A20. [Google Scholar]
- 6.Lavoie A, McCarthy R, Wong C. The ED90 of prophylactic oxytocin infusion after delivery of the placenta during cesarean delivery in laboring compared with nonlaboring women: an up-down sequential allocation dose–response study. Anesth Analg 2015; 121:159–164. [DOI] [PubMed] [Google Scholar]
- 7.George RB, McKeen D, Chaplin AC, et al. Up-down determination of the ED90 of oxytocin infusions for the prevention of postpartum uterine atony in parturients undergoing Cesarean delivery. Can J Anaesth 2010; 57:578–582. [DOI] [PubMed] [Google Scholar]
- 8.Marcus HE, Fabian A, Lier H, et al. Survey on the use of oxytocin for cesarean section. Minerva Anestesiol 2010; 76:890–895. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


