Abstract
Background:
This paper provides statewide estimates on health care access and utilization patterns and physical and behavioral health by citizenship and documentation status among Latinos in California.
Methods:
This study used data from the 2011–2015 California Health Interview Survey to examine health care access and utilization and physical and behavioral health among a representative sample of all nonelderly Latino and US-born non-Latino white adults (N=51,386). Multivariable regressions estimated the associations between the dependent measures and citizenship/documentation status among Latinos (US-born, naturalized citizen, green card holder, and undocumented).
Results:
Adjusted results from multivariable analyses observed worse access and utilization patterns among immigrant Latinos compared with US-born Latinos, with undocumented immigrants using significantly less health care. Undocumented Latinos had lower odds of self-reporting excellent/very good health status compared with US-born Latinos, despite them having lower odds of having several physical and behavioral health outcomes (overweight/obesity, physician-diagnosed hypertension, asthma, self-reported psychological distress, and need for behavioral health services). Among those reporting a need for behavioral health services, access was also worse for undocumented Latinos when compared with US-born Latinos.
Conclusions:
Patterns of poor health care access and utilization and better physical and behavioral health are observed across the continuum of documentation status, with undocumented immigrants having the worst access and utilization patterns and less disease. Despite fewer reported diagnoses and better mental health, undocumented Latinos reported poorer health status than their US-born counterparts.
Key Words: immigrants, Hispanic Americans, citizenship, health care access, health care reform
Access to publicly funded health services for immigrants, particularly for those who are undocumented, is a politically polarizing issue. Undocumented immigrants are explicitly excluded from the Patient Protection and Affordable Care Act’s (ACA) health insurance exchanges, cost-sharing reductions, health insurance mandate, tax credits, and the expansion of Medicaid’s traditional provisions. While the ACA has reduced racial/ethnic and income-based health care disparities, it has the potential to exacerbate disparities among undocumented immigrants.1–3
Congress and the Trump Administration have discussed a range of policy and enforcement options that have the potential to impact both legally authorized (eg, reducing levels of legal immigration) and undocumented (eg, a pathway to citizenship for “DREAMers” and increased attention on deportation) immigrants. A key motivator is the belief among some constituents that immigrants overutilize resources, such as health care,4,5 despite evidence that undocumented immigrants and immigrants without insurance use less health care than others.1,6–10 Similarly, an analysis by the nonpartisan Institute on Taxation and Economic Policy found that undocumented immigrants collectively pay nearly $12 billion per year in state and local taxes, including over $3 billion annually in California alone.11 They also contribute $2 to $4 billion into the Medicare Trust Fund and $12 billion net into Social Security annually, even though they are unable to claim benefits from these programs.12,13
Immigrants, especially those who are undocumented, face a number of unique barriers14–21 that contribute to poor access and utilization of health services.1,6–10,15,16,22,23 The few population-based studies that have examined health care access and utilization by citizenship and documentation status have shown that undocumented immigrants had the worst patterns of access to care before 2010 when the ACA was passed.1,6–9,15 While the ACA was not implemented nationally until 2014, California began implementing several provisions as early as 2010. To our knowledge, no peer-reviewed studies have examined access to care among the undocumented after the ACA was passed and implemented. Furthermore, there are limited data on the physical and behavioral health status of undocumented immigrants, which can inform population health strategies targeting this group of 11 million people.24
In this study, we use the 2011–15 California Health Interview Survey (CHIS) to examine patterns of health care access and utilization based on citizenship and documentation status. We also examine physical and behavioral health outcomes over the same period to understand how variation in the underlying health status of immigrant populations may generate differential need for health care services. We focus on Latinos because they are the largest ethnic group of immigrants nationwide and because over 80% of undocumented immigrants in California are Latino.24 Moreover, studies have found that Latinos have worse patterns of health care access and utilization than other racial and ethnic groups in the United States,25 and that among Latinos there are disparities, with Mexican and Central American heritage Latinos being the worst on most measures.26,27 In California, over 30% of the state’s population is of Mexican heritage, and it also has the largest Central American population in the country.28
METHODS
Study Population and Data Source
We use data from 51,386 nonelderly adult participants in the 2011–2015 waves of the CHIS. CHIS is a cross-sectional, dual-frame random digit dial survey composed of both a landline and cellphone sample of the noninstitutionalized population in California. The survey is administered in 5 languages including Spanish. Since 2011, CHIS has been an ongoing survey with data collected continuously during a 2-year data collection cycle. More details on CHIS are available elsewhere.29
Measures
Immigrant Authorization and Citizenship
CHIS asks participants their race, ethnicity (eg, Latino), and nativity. Foreign-born participants are asked “Are you a citizen of the United States?” Citizens are then asked “When did you become naturalized?” and noncitizens are asked “Are you a permanent resident with a green card?” We classify noncitizens without a green card as undocumented. We created the following mutually exclusive groups among Latinos: US-born (n=8303), naturalized (n=3879), green card (n=3369), undocumented (n=3053). This approach has been used in prior peer-reviewed studies.6,7,15 It has been estimated that the undercount of undocumented immigrants using this approach is low; it is in the 5% range for undocumented Mexicans in CHIS.30 We also examined US-born non-Latino whites (n=32,782).
Dependent Measures
We examined dependent variables across 3 domains: (1) health care access and utilization; (2) physical health status; and (3) behavioral health status and unmet need. We measured health care access using 2 binary measures indicating if the participant has a usual source of care other than the emergency department (ED) and if the participant’s insurance was refused by a provider in the past year. We measured health care utilization using binary measures indicating whether the participant had at least 1 ED visit in the past year and whether the participant had seen a medical doctor within the past year, as well as a continuous measure indicating the total number of provider visits over the past year. These measures of access and utilization are also found in the National Health Interview Survey (NHIS) and are consistent with a widely used framework regarding these domains.31,32
We assessed physical health via dichotomous measures of self-reported excellent or very good versus good/fair/poor health status and overweight and obesity based on self-reported height and weight. We also measure chronic illness through binary outcomes indicating previous diagnosis of high blood pressure, diabetes, any kind of heart disease, and asthma.
Behavioral health is measured through six binary measures. We use the Kessler Psychological Distress Scale (K6) to indicate if the participant experienced serious psychological distress (a score of 13 or higher) over the past year. We also created 2 binary indicators of perceived need and use of behavioral health services in the past year. For those who reported a need for behavioral health services and who were insured (n=9140), we created an indicator measuring if the participant’s insurance covered mental health treatment. For participants who perceived a need for, but did not get, treatment (n=3240), we measured whether this was due to concern about cost of the treatment. For participants who reported having entered treatment (n=3067), we examined whether they had completed their full course of recommended behavioral health treatment.
Independent Measures
We adjusted for demographic and socioeconomic factors which have been shown to affect health care access and utilization, physical health, and mental health. These factors include sex, age, education, employment status, marital status, federal poverty level, location of residence, health insurance coverage and type, and survey year.
Statistical Analysis
We used survey weights and design variables to adjust all analyses for the complex CHIS design and participant nonresponse. We used χ2 and analysis of variance to assess variation across the citizenship and documentation status groupings and the independent measures, health care access and utilization, physical health, and behavioral health/unmet need. We used multivariable logistic regression analyses to assess the association between citizenship and documentation status and dichotomous health and health care outcomes, after adjustment for the control variable. We used Poisson regression to conduct similar analyses using the indicator of annual provider visits because of its skewed distribution. We report odds ratios (ORs) and 95% confidence intervals (CIs) for all logistic regressions, and estimated coefficients and 95% CI’s are reported for Poisson regressions.
RESULTS
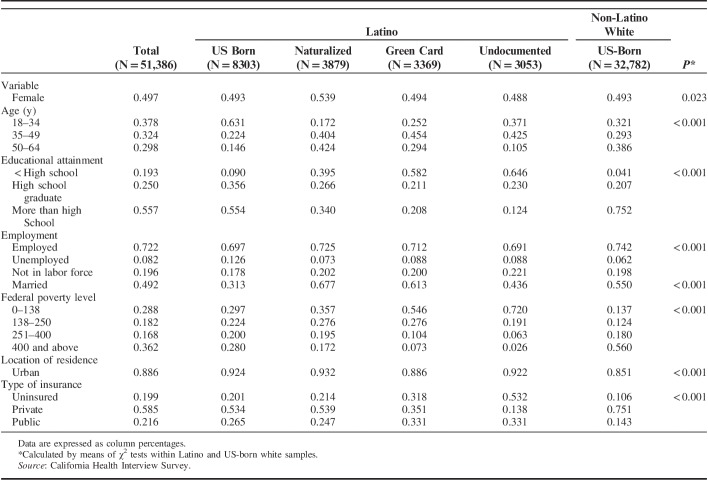
Table 1 shows sample characteristics stratified by citizenship and documentation status. Undocumented Latinos were younger and had the lowest levels of education relative to other groups. All groups had high rates of employment and were likely to be in the workforce. US-born Latinos were the least likely to be married. Almost 3-quarters of undocumented Latinos had incomes <138% FPL, which is 2.4 times the proportion of US-born Latinos and 5.3 times that of US-born non-Latino whites. The majority (53%) of undocumented immigrants in the sample were uninsured. Approximately one third of Latinos who were undocumented or with green cards had public health insurance.
TABLE 1.
Descriptive Statistics by Race/Ethnicity, and Citizen/Documentation Status, Ages 18–64, California, 2011–2015
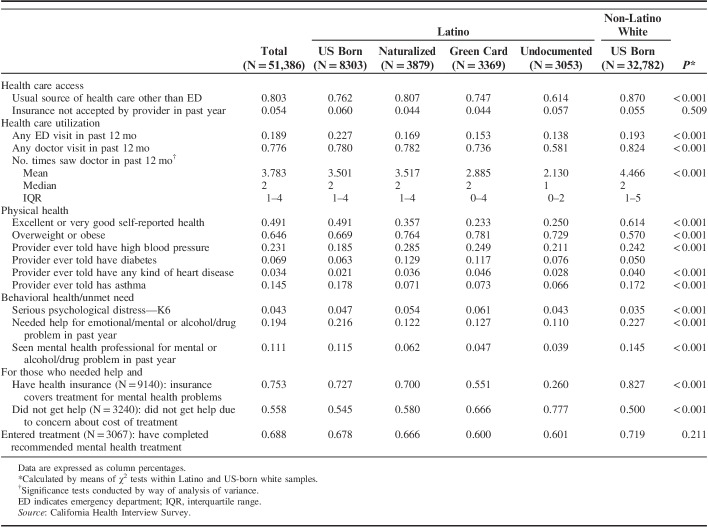
Table 2 shows the unadjusted associations of health care access and utilization and physical and behavioral health/unmet need by citizenship/documentation status. Undocumented Latinos had the worst health care access and lower levels of utilization relative to other groups, while the opposite was true for US-born Latinos. In the past year, undocumented Latinos were the least likely to have a usual source of care other than the ED (61%), were the least likely to have visited the ED (14%), the least likely to have had a doctor visit (58%), and reported having the fewest mean number of doctor visits ( ).
).
TABLE 2.
Health Care Access, Utilization, Physical Health, and Behavioral Health Status and Unmet Need by Race/Ethnicity and Citizen/Documentation Status, Ages 18–64, California 2011–2015
Non-Latino whites were the most likely to report excellent/very good health (61%), while 23% of green card holders and 25% of the undocumented reported excellent/very good health. Latinos with green cards were the most likely (78%) to report being obese or overweight, while US-born non-Latino whites were the least likely (57%). US-born Latinos (19%) and undocumented Latinos (21%) were the least likely to report ever having been diagnosed with high blood pressure. Naturalized Latinos had the highest rates of physician-diagnosed diabetes (13%). US-born Latinos (2.1%) and undocumented Latinos (2.8%) had the lowest rates of physician-diagnosed heart disease, and immigrant Latinos across the categories (7%) had the lowest rates of physician-diagnosed asthma.
There were significant differences across groups in all behavioral health measures. Undocumented Latinos (4.3%) and US-born non-Latino whites (3.5%) were the least likely to report experiencing serious psychological distress over the past year, and undocumented Latinos (11%) were the least likely to report needing help for mental health, emotions, nerves, or use of alcohol or drugs in the past year. Undocumented Latinos were the least likely to have seen a mental health professional in the past year (3.9%) and were the least likely (26%) to have insurance that covered mental health treatment. Undocumented Latinos were the most likely (77%) not to seek help for mental health due to cost of treatment. There were no significant differences in entering and completing recommended mental health treatment.
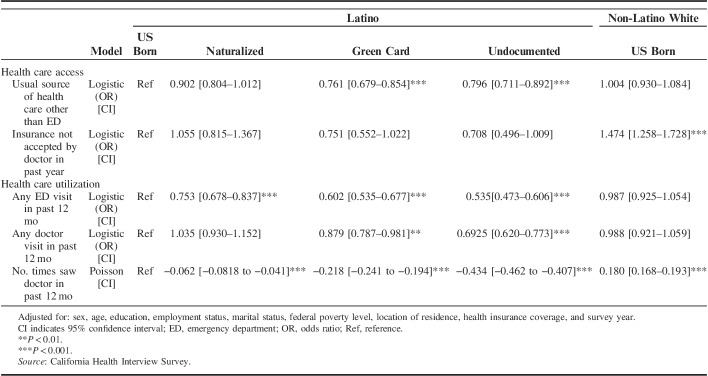
Table 3 shows the multivariable regression analyses testing the adjusted associations between our health care access and utilization measures and citizenship/documentation status, with US-born Latinos serving as the reference category. Undocumented Latinos and Latinos with green cards had significantly lower odds of having a usual source of care other than the ED. Immigrant Latinos also had significantly lower odds of having an ED visit in the past year relative to US-born Latinos, while Latinos with green cards and undocumented Latinos had lower odds of having had a doctor visit in the past year. The Poisson model indicates that all immigrant groups visited the doctor less relative to US-born Latinos, with undocumented immigrants having the largest difference in expected counts ( =−0.434; CI, −0.462 to −0.407).
=−0.434; CI, −0.462 to −0.407).
TABLE 3.
Multivariable Analyses of Health Care Access and Utilization by Citizenship Status and Race/Ethnicity, Ages 18–64, California 2011–2015
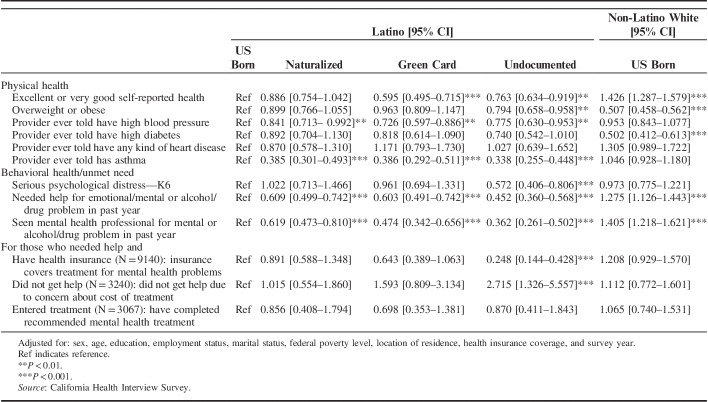
Adjusted associations from multivariable models for our physical and behavioral health and unmet need measures are in Table 4. Undocumented immigrants and green card holders had significantly lower odds of excellent/very good health relative to US-born Latinos. Only undocumented Latinos had significantly lower odds of being obese or overweight relative to US-born Latinos. Each group of immigrant Latinos had significantly lower odds of physician-diagnosed high blood pressure and asthma, with green card holders having the lowest odds of being diagnosed with high blood pressure and undocumented Latinos having the lowest odds of having been diagnosed with asthma.
TABLE 4.
Logistic Regression Analyses of Physical and Behavioral Health Status and Unmet Need by Citizenship Status and Race/Ethnicity, Ages 18–64, California, 2011–2015
Undocumented Latinos were the only group with significantly lower odds of experiencing serious psychological distress. Immigrant Latinos across all categories had significantly lower odds of reporting needing help for a behavioral health issue and had significantly lower odds of having seen a mental health professional relative to US-born Latinos. Of those reporting a need for help and who were insured, only undocumented Latinos had significantly lower odds of having an insurance plan that covered behavioral health services. Finally, among those who reported a need for help but who had not seen a mental health professional, undocumented Latinos had higher odds of reporting not seeking this treatment due to cost relative to US-born Latinos.
DISCUSSION
Consistent with earlier studies,1,6–8 we observed significant disparities in health care based on citizenship and documentation status. These disparities followed a continuum where undocumented Latinos had the worst patterns of access and utilization, and the US-born had the best. Disparities in most utilization measures persisted after adjusting for insurance and sociodemographic characteristics. Compared with findings from Ortega et al’s7 study using 2003 CHIS data, access and utilization appear to have worsened slightly across the groups over the past decade and a half, and disparities by citizenship and documentation status of a similar direction and magnitude remained.
Our study fills in a major gap in knowledge regarding the physical and behavioral health needs of Latino groups of varying citizenship and documentation statuses. Green card holders and undocumented immigrants were the least likely to report excellent or very good health. In contrast, undocumented immigrants were the least likely to be overweight or obese and were also less likely to have been diagnosed with high blood pressure and asthma. The continuum across citizenship and documentation status was also present for the odds of having a diabetes diagnosis, with undocumented immigrants having the lowest odds, although these findings were not statistically significant. Prior research suggests that poor self-reported health is not a good predictor of mortality risk among less-acculturated Latinos,33 which might explain our contradictory findings. Undocumented Latino immigrants are typically less acculturated than their immigrant counterparts, in part because they are more likely to reside in enclaves, and there are structural and political factors that inhibit them from integrating in mainstream society.34,35 Of course, another plausible explanation is that the lower odds of health care utilization resulted in lower odds of having a physician-diagnosis, which is a function of having poor access to care. We are not, however, able to test this potential mechanism with the data.
Citizenship and documentation status were also strongly associated with behavioral health and access to and need for mental health services. Importantly, behavioral health and health care also occurred along a continuum, with undocumented immigrants demonstrating the best outcomes and US-born Latinos the worst. Undocumented Latinos had significantly lower odds of psychological distress compared with US-born Latinos. All groups of immigrant Latinos were significantly less likely to report need for help or having seen a mental health professional for an emotional/mental or alcohol/drug problem, and the degree of this need again followed a continuum. While the data do not allow for testing the mechanism that drives this continuum, it is possible that lower demand for mental health services is partly due to stigma against mental illness among Latinos, especially immigrants.36 It is also possible that stress endured by undocumented immigrants manifests physically instead of behaviorally, which could explain their poorer self-reported physical health ratings.33,37 A prior study that used a smaller sample of Latinos from Los Angeles, CA found that, in adjusted analyses, documentation status was not associated with the odds for depression.38
Even though undocumented Latinos were the least likely to report need for help for mental health problems, there were disparities in access among those who did feel they needed help. Among those who were insured and reported a need for help, undocumented Latinos were the only group that were significantly less likely to report that their insurance would cover any such treatment compared with US-born Latinos. Among participants who reported need but did not receive treatment, undocumented Latinos were significantly more likely to report cost as a key barrier. This suggests that even when undocumented immigrants have health insurance, the coverage they have may not adequately cover behavioral health services. Comprehensive data on the benefits and cost-sharing mechanisms of coverage available to undocumented immigrants are needed to better understand what impact this may have on utilization disparities, for both physical and behavioral health care.
Undocumented immigrants’ exclusion from the ACA was largely driven by a contentious debate driven by discrimination rather than evidence. An important pillar of the ACA are the subsidized and unsubsidized coverages available in the Marketplace insurance exchanges. To maintain affordable premiums, the Marketplace depends on healthy individuals to offset the cost of care for high-risk populations. Our findings show that undocumented immigrants have better health outcomes and use less care than their counterparts. Thus, they represent a potential means of improving the risk of the insurance pool in plans offered on the Marketplace.39 This is particularly important given the expected rise in premiums because of the elimination of cost-sharing reduction payments and the individual mandate.40,41 Policymakers and researchers should continue to explore the potential positive effects of allowing undocumented immigrants to participate in the ACA’s Marketplace exchanges. This would also allow undocumented immigrants access to preventive health care and potentially reduce delays in seeking needed care which could save long-run costs to health plans and improve overall population health.5
Currently, undocumented immigrants in California may access care through Emergency Medi-Cal (California’s Medicaid), which often lasts for one episode of care, for a short time period, or related to a specific diagnosis (eg, breast and cervical cancer) but not for other health care needs. Thirty-three percent of the undocumented who reported being insured had Medi-Cal coverage, likely through Emergency Medi-Cal which does not provide long-term access to insurance coverage that would address primary care and other nonurgent needs related to ongoing health maintenance. California, along with 15 other states, provides Medicaid coverage for pregnant women regardless of citizenship and documentation status through the Unborn Child Children’s Health Insurance Program federal match, which may account for some who report Medi-Cal coverage.42
This study has limitations which should be noted. CHIS has a repeated cross-sectional design and relies on self-reports of citizenship status, access to and use of health care, and physical and behavioral health and unmet need. Our method for measuring undocumented immigrants is based on participants’ reports of having a green card or being a naturalized citizen rather than a question directly assessing documentation status, which may have led us to classifying students and workers with temporary visas as undocumented. Any misclassification for documentation status, however, would result in more conservative estimates for undocumented immigrants. Moreover, undocumented Latino immigrants make up 6% of the CHIS sample, which is the same as the 2014 California estimate of undocumented immigrants reported by the Pew Hispanic Center.43 Finally, the data are limited to California, where county programs, such as Healthy Way LA, Healthy San Francisco and other indigent care investments, may improve access to care among undocumented immigrants. These programs have limitations though and may not represent comprehensive benefits, but they may result in undocumented immigrants in California having better access to care than those in other states. That issue notwithstanding, California is home to 1-quarter of all undocumented immigrants in the United States,24 and thus our study has national implications.
CONCLUSIONS
Among Latinos, undocumented immigrants continue to have the worst patterns of health care access and utilization. This study adds to the limited literature on the physical and behavioral health and unmet needs of Latino immigrant groups according to documentation status, and the findings suggest that undocumented Latinos, on average, have better behavioral health and physical health outcomes on most indicators than other Latino groups. Importantly, we find that health and health care among Latinos operates along a documentation status continuum, with better access to care among US-born Latinos but paradoxically better outcomes among the undocumented. Compared with findings from California from over a decade ago, we find that disparities in access and utilization have worsened. Given the current sociopolitical climate, these disparities can reasonably be expected to exacerbate.
Footnotes
The authors declare no conflict of interest.
REFERENCES
- 1.Wallace SP, Torres J, Sadegh-Nobari T, et al. Undocumented Immigrants and Health Care Reform. Los Angeles, CA: UCLA Center for Health Policy Research; 2012. [Google Scholar]
- 2.Sommers B. Stuck between health and immigration reform—care for undocumented immigrants. N Engl J Med. 2013;369:593–595. [DOI] [PubMed] [Google Scholar]
- 3.Fernandez A, Rodriguez RA. Undocumented immigrants and access to health care. JAMA Intern Med. 2017;177:536–537. [DOI] [PubMed] [Google Scholar]
- 4.Jones B. Americans’ Views of Immigrants Marked by Widening Partisan, Generational Divides. Washington, DC: Pew Research Center; 2016. Available at: www.pewresearch.org/fact-tank/2016/04/15/americans-views-of-immigrants-marked-by-widening-partisan-generational-divides/#. Accessed June 14, 2018. [Google Scholar]
- 5.Ortega AN. When politics trumps health: undocumented Latino immigrants and US health care. MEDICC Rev. 2015;17:59. [DOI] [PubMed] [Google Scholar]
- 6.Bustamante AV, Fang H, Garza J, et al. Variations in healthcare access and utilization among Mexican immigrants: the role of documentation status. J Immigr Minor Health. 2012;14:146–155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ortega AN, Fang H, Perez VH, et al. Health care access, use of services, and experiences among undocumented Mexicans and other Latinos. Arch Intern Med. 2007;167:2354–2360. [DOI] [PubMed] [Google Scholar]
- 8.Pourat N, Wallace SP, Hadler MW, et al. Assessing health care services used by California’s undocumented immigrant population in 2010. Health Aff (Project Hope). 2014;33:840–847. [DOI] [PubMed] [Google Scholar]
- 9.Rodríguez MA, Bustamante AV, Ang A. Perceived quality of care, receipt of preventive care, and usual source of health care among undocumented and other Latinos. J Gen Intern Med. 2009;24:508–513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Berk ML, Schur CL. The effect of fear on access to care among undocumented Latino immigrants. J Immigr Minor Health. 2001;3:151–156. [DOI] [PubMed] [Google Scholar]
- 11.Gee L, Gardner M, Hill M, et al. Undocumented Immigrants’ State & Local Tax Contributions. Washington, DC: The Institute on Taxation & Economic Policy; 2017. [Google Scholar]
- 12.Zallman L, Wilson FA, Stimpson JP, et al. Unauthorized immigrants prolong the life of Medicare’s Trust Fund. J Gen Intern Med. 2016;31:122–127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gross S, Wade A, Skirvin JP, et al. Actuarial note number 151: Effects of unauthorized immigration on the actuarial status of the Social Security Trust Funds. Baltimore, MD: Social Security Administration Office of the Chief Actuary, 2013.
- 14.Hacker K, Anies M, Folb BL, et al. Barriers to health care for undocumented immigrants: a literature review. Risk Manag Healthc Policy. 2015;8:175–183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Vargas Bustamante A, Chen J, Fang H, et al. Identifying health insurance predictors and the main reported reasons for being uninsured among US immigrants by legal authorization status. International J Health Plann Manage. 2014;29:e83–e96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hacker K, Chu J, Leung C, et al. The impact of Immigration and Customs Enforcement on immigrant health: perceptions of immigrants in Everett, Massachusetts, USA. Soc Sci Med. 2011;73:586–594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Maldonado MM. Latino incorporation and racialized border politics in the Heartland. Am Behav Sci. 2014;58:1927–1945. [Google Scholar]
- 18.Sabo S, Shaw S, Ingram M, et al. Everyday violence, structural racism and mistreatment at the US-Mexico border. Soc Sci Med. 2014;109:66–74. [DOI] [PubMed] [Google Scholar]
- 19.Martinez O, Wu E, Sandfort T, et al. Evaluating the impact of immigration policies on health status among undocumented immigrants: a systematic review. J Immigr Minor Health. 2015;17:947–970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rhodes SD, Mann L, Simán FM, et al. The impact of local immigration enforcement policies on the health of immigrant Hispanics/Latinos in the United States. Am J Public Health. 2015;105:329–337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fortuny K, Chaudry A. A Comprehensive Review of Immigrant Access to Health and Human Services. Washington, DC: Urban Institute; 2011. [Google Scholar]
- 22.Guendelman S, Angulo V, Oman D. Access to health care for children and adolescents in working poor families recent findings from California. Med Care. 2005;43:68–78. [PubMed] [Google Scholar]
- 23.Cleaveland C, Ihara ES. “They Treat us Like Pests:” undocumented immigrant experiences obtaining health care in the wake of a “crackdown” ordinance. J Hum Behav Soc Environ. 2012;22:771–788. [Google Scholar]
- 24.Passel JS, Cohn D. Overall number of US unauthorized immigrants holds steady since 2009. Washington, D.C.: Pew Hispanic Center; 2016.
- 25.Ortega AN, Rodriguez HP, Vargas Bustamante A. Policy dilemmas in Latino health care and implementation of the Affordable Care Act. Annu Rev Public Health. 2015;36:525–544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bustamante AV, Chen J, Rodriguez HP, et al. Use of preventive care services among Latino subgroups. Am J Prev Med. 2010;38:610–619. [DOI] [PubMed] [Google Scholar]
- 27.Alcalá HE, Chen J, Langellier BA, et al. Impact of the Affordable Care Act on health care access and utilization among Latinos. J Am Board Fam Med. 2017;30:52–62. [DOI] [PubMed] [Google Scholar]
- 28.US Census Bureau. American Fact Finder. Washington, DC: U.S. Census Bureau; 2010. Available at: https://factfinder.census.gov/faces/nav/jsf/pages/index.xhtml. Accessed June 14, 2018. [Google Scholar]
- 29.UCLA Center for Health Policy Research. California Health Interview Survey: design & methods. 2017. Available at: http://healthpolicy.ucla.edu/chis/design/Pages/overview.aspx. Accessed June 14, 2018.
- 30.Viana J, Ponce N, Porteny T, et al. Measurement error in citizenship and immigration status among Mexican-born respondents in the California Health Interview Survey. Paper presented at American Public Health Association Annual Meeting, 2017.
- 31.Blewett LA, Dahlen HM, Spencer D, et al. Changes to the design of the national health interview survey to support enhanced monitoring of health reform impacts at the state level. Am J Public Health. 2016;106:1961–1966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Andersen RM, Davidson PL, Baumeister SE.Kominski GF. Improving access to care. Changing the US Health Care System. San Francisco, CA: Jossey-Bass; 2014:33–69. [Google Scholar]
- 33.Finch BK, Hummer RA, Reindl M, et al. Validity of self-rated health among Latino(a)s. Am J Epidemiol. 2002;155:755–759. [DOI] [PubMed] [Google Scholar]
- 34.Schwartz SJ, Pantin H, Sullivan S, et al. Nativity and years in the receiving culture as markers of acculturation in ethnic enclaves. J Cross Cult Psychol. 2006;37:345–353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Schwartz SJ, Unger JB, Zamboanga BL, et al. Rethinking the concept of acculturation: implications for theory and research. Am Psychol. 2010;65:237–251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Abdullah T, Brown TL. Mental illness stigma and ethnocultural beliefs, values, and norms: an integrative review. Clin Psychol Rev. 2011;31:934–948. [DOI] [PubMed] [Google Scholar]
- 37.Cabassa LJ, Zayas LH, Hansen MC. Latino adults’ access to mental health care: a review of epidemiological studies. Adm Policy Mental Health. 2006;33:316–330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Young M-EDT, Pebley AR. Legal status, time in the USA, and the well-being of Latinos in Los Angeles. J Urban Health. 2017;94:764–775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ortega AN. Could undocumented immigrants help Obamacare? The Philadelphia Inquirer, November 2, 2016. Available at: www.philly.com/philly/blogs/public_health/Could-undocumented-immigrants-help-Obamacare.html. Accessed March 5, 2018.
- 40.Levitt L, Cox C, Claxton G. The effects of ending the Affordable Care Act’s cost-sharing reduction payments. Washington, DC: Kaiser Family Foundation, 2017.
- 41.Eibner C, Saltzman E. How Does the ACA Individual Mandate Affect Enrollment and Premiums in the Individual Insurance Market. Santa Monica, CA: RAND Corporation; 2015. [Google Scholar]
- 42.Georgetown University Center for Children & Families. Medicaid and CHIP eligibility, enrollment, renewal, and cost sharing policies as of January 2017. 2017. Available at: http://ccf.georgetown.edu/wp-content/uploads/2017/01/EligibilityRelated.pdf. Accessed March 5, 2018.
- 43.Pew Research Center. US unauthorized immigration population estimates: estimated unauthorized immigrant population, by state, 2014. Washington, DC: Pew Research Center, 2016. Available at: www.pewhispanic.org/interactives/unauthorized-immigrants/. Accessed June 14, 2018.