INTRODUCTION
Sexual function is an important aspect of life for many women, regardless of age. Sexual function is closely correlated with overall well-being and relationship satisfaction.1–3 Most women continue to consider sexual function important as they age.4–6 However, 45% of midlife women have sexual problems,2,7 and 15% have a sexual problem that causes significant personal distress.7 Female sexual dysfunction remains under-recognized and undertreated by healthcare providers. In this article, we will review definition of female sexual dysfunction, examine how sexual function changes during the midlife transition, define factors that are associated with sexual dysfunction at midlife, and discuss new and emerging treatments.
DEFINITIONS
Sexual dysfunction, as defined in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), is a heterogeneous group of disorders characterized by clinically significant disturbances in sexual response or the experience of sexual pleasure.,8 A key element of the DSM-5 definition is significant personal distress. Revision of the DSM between versions 4 and 5 included substantive changes to female sexual dysfunction terminology (Figure 1). Notably, Hypoactive Sexual Desire Disorder and Female Sexual Arousal Disorder were combined into a single diagnosis, Female Sexual Interest and Arousal Disorder8 as there is considerable overlap between the disorders, and the concepts of desire and arousal are virtually indistinguishable for many women.9,10 These changes were controversial,11–13 and some experts still favor the older terminology. It is also essential to consider overall sexual satisfaction. For many women, the end-goal of sex is not “functional” sex where all the parts are working well, but emotional and physical satisfaction and increased intimacy with one’s partner.
Figure 1.
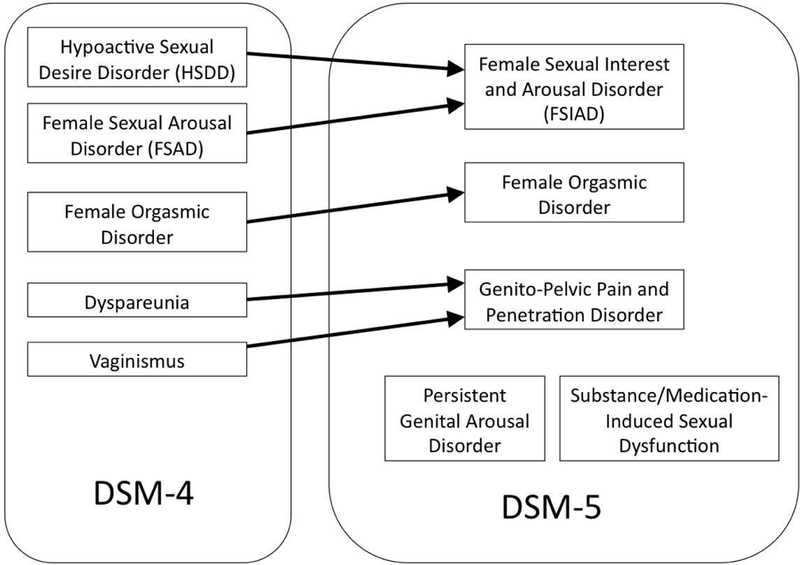
Female Sexual Dysfunction Terminology. From American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition. Washington, DC: American Psychiatric Publishing; 2000; and American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition. Washington, DC: American Psychiatric Publishing; 2013; with permission.
CHANGES IN SEXUAL FUNCTION DURING MIDLIFE
Sexual function declines during midlife. The Study of Women’s Health Across the Nation (SWAN) and others found that this decline corresponds with the menopausal transition, including in women who have hysterectomies.14,15 While symptoms such as vaginal dryness increase over the same period, changes in sexual function are independent of other symptoms associated with the menopausal transition. Declines in sexual activity during midlife are multi-factorial (discussed below). One prominent reason that women do not engage in sexual activity is lack of a partner.16
Women who are sexually active prior to menopause appear to continue to engage in sexual activities during midlife, despite poor “functional sex.”5 Lifestyle factors, including sufficient sleep and physical activity, contribute to more positive sexual functioning during midlife.16 Alternative models of sexual function may provide more insight into the impact of these changes during menopause. In contrast to the traditional linear model posited by Masters and Johnson,17 Basson suggests that the sexual response, particularly in women, is more circular and dependent on emotional connection and fulfillment.18 This model offers an explanation for the dichotomy of decline in sexual function, with endurance of sexual activities as a means to express and maintain connected partnerships.
FACTORS THAT AFFECT FEMALE SEXUAL FUNCTION AT MIDLIFE
Biologic factors - hormones, menopausal symptoms
The menopause is characterized by ovarian follicular exhaustion and hypogonadism. Reduced ovarian steroidogenesis leads to the development of genitourinary syndrome of menopause (GSM),19 which adversely affects the genital system and lower urinary tract in menopausal women and significantly contributes to sexual dysfunction.20 More than half of menopausal women experience GSM, which is responsive to local estradiolUnlike vasomotor symptoms, which often decrease over time, GSM does not resolve and recurs after discontinuation of estrogen.21,22
Vulvovaginal atrophy (VVA), also known as vulvovaginitis, is a key component of GSM, and can result in post coital vaginal bleeding, vaginal burning, irritation, and pain and discomfort with sex. Symptomatic GSM is often accompanied by diminished secretions from vulvar sebaceous glands and reduced vaginal lubrication during sexual stimulation. Hypoestrogenic menopausal women often experience a shift of the vaginal microbiome from lactic acid producing lactobacilli to gram negative and positive bacteria.23 This shift in the vaginal microbiome results in increased vaginal pH, local immune changes and increased cytokine synthesis which worsens symptoms of vaginal dryness and burning23 and contributes to sexual dysfunction. These external genital changes are covered in detail in Chapter 12-Waetjen.
Pelvic organ prolapse (POP) involves descent of one or more female genital organs (anterior and/or posterior vaginal wall, the uterus or the apex of the vagina). The incidence of pelvic floor relaxation increases with aging and is hypothesized to result from a combination of connective tissue degradation, pelvic denervation, and devascularization, all of which predispose to prolapse.24 Dyspareunia, chronic pelvic pain, and reduced self-image are associated with POP. Any one of these adverse anatomical changes can devastate sexual interest and function.25 Estrogen treatment may reduce the risk for POP, especially in postmenopausal women who have undergone hysterectomy and require transvaginal reconstructive surgery.26
Medical problems and medications
Multiple medical problems, including diabetes, hypertension, and breast cancer, have been associated with female sexual dysfunction (Box 1). These conditions become more common as women move through midlife.
Box 1. Medical and psychiatric conditions that are associated with female sexual dysfunction.
| Cardiovascular disease 108 |
| Diabetes mellitus 109 |
| Neurologic disease (stroke, multiple sclerosis, spinal cord injury) 110 |
| Hypertension 28 |
| Substance use disorders 111 |
| Genitourinary syndrome of menopause 57,112 |
| Breast, ovarian, uterine, and cervical cancer 113–115 |
| History of gynecologic surgery 116,117 |
| Chronic renal failure 118,119 |
| Urinary incontinence 120,121 |
Both type 1 and 2 diabetes are associated with a 2–3 times higher rate of female sexual dysfunction.27 Biologically, diabetes imparts chronic microvascular damage that could affect small nerves and blood vessels in the clitoris and associated structures, leading to impaired arousal and lubrication. Through similar mechanisms, hypertension has a 3-fold higher risk of sexual dysfunction in women,28 with the strongest effects on the domain of lubrication.29 While early studies suggested that certain antihypertensives, especially beta blockers, may negatively affect sexual function in women,30 newer studies have found no association between antihypertensives and female sexual dysfunction.31–33 In fact, antihypertensive medications that work on the renin-angiotensin system may be associated with better sexual function.31,34
Breast cancer can negatively effect sexual function in both short and long terms.35–37 Around 50% of women with a history of breast cancer report sexual problems,37 and the prevalence rises to 70% among women with invasive cancer.38 The causes are multifactorial. Receipt of chemotherapy is one of the strongest risk factors,39 particularly if it results in premature menopause.40 Aromatase inhibitors are associated with vaginal dryness and sexual pain38,41 while tamoxifen does not have strong effects on sexual function.38 Mastectomy can negatively affect body image39 and in turn sexual function.37–39,42 Among women with diabetes, hypertension, or breast cancer, depression is highly correlated with sexual dysfunction.35,37,43,44 This highlights the importance of screening for and treating mood disorders in these populations.
Other medications have been associated with female sexual dysfunction (Box 2). Among the most common offenders are antidepressants, including selective-serotonin reuptake inhibitors, serotonin-norepinephrine reuptake inhibitors, and tricyclic antidepressants.45 While depression itself is associated with sexual dysfunction, odds of sexual dysfunction are 4–6 times higher for women taking a medication.46 Sexual side effects are less common with bupropion46,47 and mirtazapine.47,48 Providers should counsel women about the potential for sexual side effects when starting these medications. Small studies have shown sildenafil and bupropion to be effective antidotes for antidepressant-associated sexual dysfunction.49,50
Box 2. Medications that are associated with female sexual dysfunction.
| Antidepressants (selective serotonin reuptake inhibitors, serotonin norepinephrine reuptake inhibitors, tricyclic antidepressants) 46,47,122,123 |
| Opiates 111 |
| Cancer therapies, especially for breast and gynecologic cancer 113,124–126 |
| Antihypertensives (mixed evidence), particularly beta-blockers 30– 127 |
| Antiepileptics 128,129 |
| Benzodiazepines 130,131 |
Psychosocial
Several psychosocial factors that are common during midlife are associated with sexual dysfunction:
Mood symptoms, such as depression and anxiety
Life stressors such as career and family demands
A history of trauma, particularly sexual trauma
The development of depression and anxiety symptoms during the menopausal transition is common.51–53 Mood disorders and sexual dysfunction are highly comorbid,54 with 25–75% of depressed women reporting sexual problems55 even when controlling for other factors.56–58 It is important for providers to screen women with sexual complaints for depression and anxiety symptoms and recognize that not all women with sexual dysfunction have a mood disorder. Everyday life stressors also have a negative impact.59–61 Midlife women may be caring for children of their own, having adult children return home, and/or be caring for aging parents.59 Job-related stress and financial concerns are also common.59 Providers should be attuned to the effects of life stressors and work with women to develop stress reduction strategies, such as mindfulness meditation.
Women who are victims of violence are at increased risk for sexual dysfunction in women,62 with those who have experienced sexual trauma—up to 44% of women over their lifetime63—at particularly high risk.64 The relationship between trauma history and sexual dysfunction is not entirely explained by mental health disorders, such as depression, anxiety, and post-traumatic stress disorder. It is important to use evidence- based, trauma-informed care techniques to screen for these events when providing care for women with sexual dysfunction.65,66
Interpersonal factors
Most midlife women are sexually active with a partner,5 and partner-associated issues can affect the woman’s sexual function:
Positive relationship aspects - Higher relationship satisfaction and intimacy are associated with better sexual function,67,68 and the ability to openly communicate with one’s partner is of key importance.59
Loss or gain of a partner - Many women experience the loss of a partner (to death, divorce, or separation) at midlife, and some gain a new partner, both of which can affect sexual function.57,69 Gain of a new partner is associated with increased desire, arousal, and emotional satisfaction with sex.57
Issues affecting aging partners - Partners may develop medical problems, medications, or sexual dysfunction that can affect the woman’s sexual function. In particular, erectile dysfunction in male partners is associated with decreased sexual function and satisfaction in female partners.59,70
NEW AND EMERGING TREATMENTS
Female sexual interest and arousal disorder
There is only one Food and Drug Administration (FDA) approved medication for the treatment of hypoactive sexual desire disorder: flibanserin. While only approved for use in premenopausal women, it is efficacious in postmenopausal women.71 Flibanserin increases satisfying sexual events by about 0.5 per month compared to placebo, with statistically significant improvements in desire, overall sexual function, and sexually- related distress.72–75 Some have questioned whether these improvements are clinically significant.75 Providers should be aware:
Common adverse effects include somnolence, dizziness, and nausea73,75
Flibanserin interacts with some common medications (macrolide antibiotics, azole antifungals, and calcium channel blockers)
Women cannot drink alcohol while using flibanserin
Healthcare providers must be certified to prescribe flibanserin
Testosterone has been studied for the treatment of hypoactive sexual desire disorder, but is not FDA approved for this purpose. Most testosterone studies were conducted among surgically menopausal women,76–78 although there a few studies included naturally menopausal women.79,80 All but two studies79,81 paired testosterone with estrogen therapy. Consistent positive effects were seen on sexual desire, overall sexual function, and sexual distress.76–80,82–84 Common adverse effects were acne and hirsutism, occurring in 5–20% of women.76–82 Negative effects on lipid parameters were not observed.77,84 However, randomized trial data beyond 24 weeks is sparse, and a recent analysis suggests only women who achieve supraphysiologic testosterone levels have a significant response85 Observational studies have suggested there may be an increased risk of cardiovascular disease86 and invasive breast cancer81,87 when testosterone is added to traditional hormone therapy, but findings are inconsistent.88,89
Behavioral interventions, most notably mindfulness-based therapies, have shown positive effects on sexual desire, sexual distress, and overall sexual function.90–92 These methods may improve sexual function by increasing bodily awareness93 and improving concordance between physiologic and psychological arousal.94 However, these studies are relatively small, limited by use of wait-list controls or no control group, and lack comparison to pharmaceutical interventions.
Genitourinary syndrome of menopause and sexual pain
Many women have been dissatisfied with prior treatment for GSM and sexual pain.95,96 These symptoms remain underrecognized and undertreated by healthcare providers.95,97,98 Newer options include ospemifene, prasterone, estradiol softfels, and carbon dioxide laser therapy.
Ospemifene is an FDA-approved selective estrogen receptor modifier that results in significant improvements in vaginal symptoms and dyspareunia.99,100 Adverse effects include hot flashes (7–10%)101,102 and endometrial proliferation (2–12%), although no cases of hyperplasia or endometrial cancer are reported.101 Prasterone, intravaginal dehydroepiandrosterone (DHEAS), was recently approved for the treatment of dyspareunia due to GSM, with the only adverse effect being vaginal discharge (6%).103 A new formulation of vaginal estradiol, a softgel tablet, has shown promising results in early trials.104,105 Finally, carbon dioxide laser use is emerging as another potential treatment;106,107 however, trials have lacked adequate control groups and further research is necessary. Data beyond 52 weeks are not available for any of these newer treatments, and it is unclear how they compare to older treatments in terms of efficacy or safety.
FUTURE DIRECTIONS
Much progress has been made in the field of women’s sexual function. However, much work remains. Sexual health education for providers in training needs to be better developed and tested. Easy-to-use, efficient screening methods for sexual problems in primary care settings are needed. Research should seek to define protective factors— ways that women adapt to the changes that occur with the midlife transition, and how they are able to maintain sexual function and satisfaction. Data on how sexual function changes with aging is needed among sexual minority groups. Research should explore how the traditional and newer treatment options for GSM compare to one another, not just placebo, and define which treatments are safest and most effective for specific patient groups. Treatments for desire and arousal difficulties remain lacking; behavioral interventions hold promise, and ongoing research should explore which aspects of these interventions are most powerful, and how they can be scaled up to reach the women in need. Helping women preserve healthy sexual function with aging is an essential component of maintaining quality of life into older adulthood.
Key Points:
A sizeable minority of women report sexual dysfunction during the perimenopause and menopausal years; about 15% endorse personal distress as a result.
Genitourinary syndrome of menopause (GSM), vulvovaginal atrophy (VVA), and pelvic organ prolapse (POP) can cause vaginal and sexual pain and remain under-recognized and under-treated.
Relationship and social factors, as well as sexual trauma, are important predictors of midlife sexual function.
A variety of pharmacologic treatments are available with varying efficacy; more information is needed to help clinicians target treatments effectively.
Synopsis:
Sexual function is an important component of quality of life for women. Midlife poses a number of challenges to optimal sexual function and intimacy for women. In addition to anatomical factors related to estrogen deficiency, such as GSM, VVA, and POP, psychosocial factors, including prior sexual trauma, play an important role in sexual function in women. A number of treatments have emerged for female sexual dysfunction; long-term studies and head-to-head comparisons are lacking.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosure Statement: Dr. Hess and Dr. Thomas report no disclosures Dr. Neal-Perry is a member of the Scientific Advisory Board for Astellas and a past Data and Safety Monitoring Board member for Ferring Pharmaceuticals
REFERENCES
- 1.Leiblum SR, Koochaki PE, Rodenberg CA, Barton IP, Rosen RC. Hypoactive sexual desire disorder in postmenopausal women: US results from the Women’s International Study of Health and Sexuality (WISHeS). Menopause. 2006;13(1):46– 56. [DOI] [PubMed] [Google Scholar]
- 2.Laumann EO, Paik A, Rosen RC. Sexual dysfunction in the United States: prevalence and predictors. Jama. 1999;281(6):537–544. [DOI] [PubMed] [Google Scholar]
- 3.Lindau ST, Gavrilova N. Sex, health, and years of sexually active life gained due to good health: evidence from two US population based cross sectional surveys of ageing. BMJ. 2010;340:c810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cain VS JC, Avis NE, Mohr B, Schocken M, Skurnick J, Ory M. Sexual functioning and practices in a multi-ethnic study of midlife women: baseline results from SWAN. Journal of Sex Research. 2003;40(3):266–276. [DOI] [PubMed] [Google Scholar]
- 5.Thomas HN, Chang CC, Dillon S, Hess R. Sexual activity in midlife women: importance of sex matters. JAMA internal medicine. 2014;174(4):631–633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Flynn KE, Lin L, Bruner DW, et al. Sexual Satisfaction and the Importance of Sexual Health to Quality of Life Throughout the Life Course of U.S. Adults. The journal of sexual medicine. 2016;13(11):1642–1650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shifren JL, Monz BU, Russo PA, Segreti A, Johannes CB. Sexual problems and distress in United States women: prevalence and correlates. Obstetrics and gynecology. 2008;112(5):970–978. [DOI] [PubMed] [Google Scholar]
- 8.American Psychiatric Association., American Psychiatric Association DSM-5 Task Force. Diagnostic and statistical manual of mental disorders: DSM-5. 5 th ed. Washington, D.C.: American Psychiatric Association; 2013. [Google Scholar]
- 9.Brotto LA. The DSM diagnostic criteria for hypoactive sexual desire disorder in women. Archives of sexual behavior. 2010;39(2):221–239. [DOI] [PubMed] [Google Scholar]
- 10.Binik YM, Brotto LA, Graham CA, Segraves RT. Response of the DSM-V Sexual Dysfunctions subworkgroup to commentaries published in JSM. The journal of sexual medicine. 2010;7(7):2382–2387. [DOI] [PubMed] [Google Scholar]
- 11.DeRogatis LR, Clayton AH, Rosen RC, Sand M, Pyke RE. Should sexual desire and arousal disorders in women be merged? Archives of sexual behavior. 2011;40(2):217–219; author reply 221–215. [DOI] [PubMed] [Google Scholar]
- 12.Balon R, Clayton AH. Female sexual interest/arousal disorder: a diagnosis out of thin air. Archives of sexual behavior. 2014;43(7):1227–1229. [DOI] [PubMed] [Google Scholar]
- 13.McCabe MP, Sharlip ID, Atalla E, et al. Definitions of Sexual Dysfunctions in Women and Men: A Consensus Statement From the Fourth International Consultation on Sexual Medicine 2015. The journal of sexual medicine. 2016;13(2):135–143. [DOI] [PubMed] [Google Scholar]
- 14.Dennerstein L, Dudley E, Burger H. Are changes in sexual functioning during midlife due to aging or menopause? FertilSteril. 2001;76(3):456–460. [DOI] [PubMed] [Google Scholar]
- 15.Avis NE, Colvin A, Karlamangla AS, et al. Change in sexual functioning over the menopausal transition: results from the Study of Women’s Health Across the Nation. Menopause. 2017;24(4):379–390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hess R, Conroy MB, Ness R, et al. Association of lifestyle and relationship factors with sexual functioning of women during midlife. J Sex Med. 2009;6(5):1358–1368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Masters WH JV. Human Sexual Response. Boston: Little, Brown & Co; 1966. [Google Scholar]
- 18.Basson R. The female sexual response: a different model. J Sex Marital Ther. 2000;26(1):51–65. [DOI] [PubMed] [Google Scholar]
- 19.Portman DJ, Gass ML. Genitourinary syndrome of menopause: new terminology for vulvovaginal atrophy from the International Society for the Study of Women’s Sexual Health and the North American Menopause Society. The journal of sexual medicine. 2014;11(12):2865–2872. [DOI] [PubMed] [Google Scholar]
- 20.Cuerva MJ, Gonzalez D, Canals M, et al. The sexual health approach in postmenopause: The five-minutes study. Maturitas. 2018;108:31–36. [DOI] [PubMed] [Google Scholar]
- 21.Kroll R, Archer DF, Lin Y, Sniukiene V, Liu JH. A randomized, multicenter, doubleblind study to evaluate the safety and efficacy of estradiol vaginal cream 0.003% in postmenopausal women with dyspareunia as the most bothersome symptom. Menopause. 2018;25(2):133–138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Archer DF, Labrie F, Montesino M, Martel C. Comparison of intravaginal 6.5mg (0.50%) prasterone, 0.3mg conjugated estrogens and 10mug estradiol on symptoms of vulvovaginal atrophy. The Journal of steroid biochemistry and molecular biology. 2017;174:1–8. [DOI] [PubMed] [Google Scholar]
- 23.Hummelen R, Macklaim JM, Bisanz JE, et al. Vaginal microbiome and epithelial gene array in post-menopausal women with moderate to severe dryness. PLoS One. 2011;6(11):e26602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mannella P, Palla G, Bellini M, Simoncini T. The female pelvic floor through midlife and aging. Maturitas. 2013;76(3):230–234. [DOI] [PubMed] [Google Scholar]
- 25.Shatkin-Margolis A, Pauls RN. Sexual function after prolapse repair. Current opinion in obstetrics & gynecology. 2017;29(5):343–348. [DOI] [PubMed] [Google Scholar]
- 26.Rahn DD, Carberry C, Sanses TV, et al. Vaginal estrogen for genitourinary syndrome of menopause: a systematic review. Obstetrics and gynecology. 2014;124(6):1147– 1156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pontiroli AE, Cortelazzi D, Morabito A. Female sexual dysfunction and diabetes: a systematic review and meta-analysis. The journal of sexual medicine.2013;10(4): 1044–1051. [DOI] [PubMed] [Google Scholar]
- 28.Doumas M, Tsiodras S, Tsakiris A, et al. Female sexual dysfunction in essential hypertension: a common problem being uncovered. Journal of hypertension. 2006;24(12):2387–2392. [DOI] [PubMed] [Google Scholar]
- 29.Duncan LE, Lewis C, Jenkins P, Pearson TA. Does hypertension and its pharmacotherapy affect the quality of sexual function in women? American journal of hypertension. 2000;13(6 Pt 1):640–647. [DOI] [PubMed] [Google Scholar]
- 30.A randomized trial of propranolol in patients with acute myocardial infarction. I. Mortality results. JAMA: the journal of the American Medical Association. 1982;247(12):1707–1714. [DOI] [PubMed] [Google Scholar]
- 31.Thomas HN, Evans GW, Berlowitz DR, et al. Antihypertensive medications and sexual function in women: baseline data from the SBP intervention trial (SPRINT). Journal of hypertension. 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Grimm RH Jr, ., Grandits GA, Prineas RJ, et al. Long-term effects on sexual function of five antihypertensive drugs and nutritional hygienic treatment in hypertensive men and women. Treatment of Mild Hypertension Study (TOMHS). Hypertension. 1997;29(1 Pt 1):8–14. [DOI] [PubMed] [Google Scholar]
- 33.Wassertheil-Smoller S, Blaufox MD, Oberman A, et al. Effect of antihypertensives on sexual function and quality of life: the TAIM Study. Annals of internal medicine. 1991;114(8):613–620. [DOI] [PubMed] [Google Scholar]
- 34.Ma R, Yu J, Xu D, et al. Effect of felodipine with irbesartan or metoprolol on sexual function and oxidative stress in women with essential hypertension. Journal of hypertension. 2012;30(1):210–216. [DOI] [PubMed] [Google Scholar]
- 35.Speer JJ, Hillenberg B, Sugrue DP, et al. Study of sexual functioning determinants in breast cancer survivors. The breast journal. 2005;11(6):440–447. [DOI] [PubMed] [Google Scholar]
- 36.Broeckel JA, Thors CL, Jacobsen PB, Small M, Cox CE. Sexual functioning in long-term breast cancer survivors treated with adjuvant chemotherapy. Breast cancer research and treatment. 2002;75(3):241–248. [DOI] [PubMed] [Google Scholar]
- 37.Fobair P, Stewart SL, Chang S, D’Onofrio C, Banks PJ, Bloom JR. Body image and sexual problems in young women with breast cancer. Psycho-oncology. 2006;15(7):579–594. [DOI] [PubMed] [Google Scholar]
- 38.Panjari M, Bell RJ, Davis SR. Sexual function after breast cancer. The journal of sexual medicine. 2011;8(1):294–302. [DOI] [PubMed] [Google Scholar]
- 39.Avis NE, Crawford S, Manuel J. Psychosocial problems among younger women with breast cancer. Psycho-oncology. 2004;13(5):295–308. [DOI] [PubMed] [Google Scholar]
- 40.Ganz PA, Rowland JH, Desmond K, Meyerowitz BE, Wyatt GE. Life after breast cancer: understanding women’s health-related quality of life and sexual functioning. J Clin Oncol. 1998;16(2):501–514. [DOI] [PubMed] [Google Scholar]
- 41.Avis NE, Crawford S, Manuel J. Quality of life among younger women with breast cancer. Journal of clinical oncology: official journal of the American Society of Clinical Oncology. 2005;23(15):3322–3330. [DOI] [PubMed] [Google Scholar]
- 42.Greendale GA, Petersen L, Zibecchi L, Ganz PA. Factors related to sexual function in postmenopausal women with a history of breast cancer. Menopause. 2001;8(2):111–119. [DOI] [PubMed] [Google Scholar]
- 43.Nascimento ER, Maia AC, Nardi AE, Silva AC. Sexual dysfunction in arterial hypertension women: The role of depression and anxiety. Journal of affective disorders. 2015;181:96–100. [DOI] [PubMed] [Google Scholar]
- 44.Foy CG, Newman JC, Berlowitz DR, et al. Blood Pressure, Sexual Activity, and Dysfunction in Women With Hypertension: Baseline Findings From the Systolic Blood Pressure Intervention Trial (SPRINT). The journal of sexual medicine. 2016;13(9):1333–1346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Montgomery SA, Baldwin DS, Riley A. Antidepressant medications: a review of the evidence for drug-induced sexual dysfunction. Journal of affective disorders. 2002;69(1–3):119–140. [DOI] [PubMed] [Google Scholar]
- 46.Clayton AH, Pradko JF, Croft HA, et al. Prevalence of sexual dysfunction among newer antidepressants. The Journal of clinical psychiatry. 2002;63(4):357–366. [DOI] [PubMed] [Google Scholar]
- 47.Serretti A, Chiesa A. Treatment-emergent sexual dysfunction related to antidepressants: a meta-analysis. Journal of clinical psychopharmacology. 2009;29(3):259–266. [DOI] [PubMed] [Google Scholar]
- 48.Gelenberg AJ, McGahuey C, Laukes C, et al. Mirtazapine substitution in SSRI-induced sexual dysfunction. The Journal of clinical psychiatry. 2000;61(5):356–360. [DOI] [PubMed] [Google Scholar]
- 49.Nurnberg HG, Hensley PL, Heiman JR, Croft HA, Debattista C, Paine S. Sildenafil treatment of women with antidepressant-associated sexual dysfunction: a randomized controlled trial. JAMA. 2008;300(4):395–404. [DOI] [PubMed] [Google Scholar]
- 50.Labbate LA, Grimes JB, Hines A, Pollack MH. Bupropion treatment of serotonin reuptake antidepressant-associated sexual dysfunction. Annals of clinical psychiatry : official journal of the American Academy of Clinical Psychiatrists. 1997;9(4) :241– 245. [DOI] [PubMed] [Google Scholar]
- 51.Cohen LS, Soares CN, Vitonis AF, Otto MW, Harlow BL. Risk for new onset of depression during the menopausal transition: the Harvard study of moods and cycles. Archives of general psychiatry. 2006;63(4):385–390. [DOI] [PubMed] [Google Scholar]
- 52.Bromberger JT, Kravitz HM, Chang YF, Cyranowski JM, Brown C, Matthews KA. Major depression during and after the menopausal transition: Study of Women’s Health Across the Nation (SWAN). Psychol Med. 2011;41(9):1879–1888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Bromberger JT, Matthews KA, Schott LL, et al. Depressive symptoms during the menopausal transition: the Study of Women’s Health Across the Nation (SWAN). Journal of affective disorders. 2007;103(1–3):267–272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Lonnee-Hoffmann RA, Dennerstein L, Lehert P, Szoeke C. Sexual function in the late postmenopause: a decade of follow-up in a population-based cohort of Australian women. The journal of sexual medicine. 2014;11(8):2029–2038. [DOI] [PubMed] [Google Scholar]
- 55.Williams K, Reynolds MF. Sexual dysfunction in major depression. CNS spectrums. 2006;11(8 Suppl 9):19–23. [DOI] [PubMed] [Google Scholar]
- 56.Dennerstein L, Guthrie JR, Hayes RD, DeRogatis LR, Lehert P. Sexual function, dysfunction, and sexual distress in a prospective, population-based sample of mid-aged, Australian-born women. The journal of sexual medicine. 2008;5(10):2291– 2299. [DOI] [PubMed] [Google Scholar]
- 57.Avis NE, Brockwell S, Randolph JF Jr., , et al. Longitudinal changes in sexual functioning as women transition through menopause: results from the Study of Women’s Health Across the Nation. Menopause. 2009;16(3):442–452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Cyranowski JM, Bromberger J, Youk A, Matthews K, Kravitz HM, Powell LH. Lifetime depression history and sexual function in women at midlife. Arch Sex Behav. 2004;33(6):539–548. [DOI] [PubMed] [Google Scholar]
- 59.Thomas HN, Hamm M, Hess R, Thurston RC. Changes in sexual function among midlife women: “I’m older... and I’m wiser”. Menopause. 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Hamilton LD, Julian AM. The relationship between daily hassles and sexual function in men and women. Journal of sex & marital therapy. 2014;40(5):379–395. [DOI] [PubMed] [Google Scholar]
- 61.Bodenmann G, Atkins DC, Schar M, Poffet V. The association between daily stress and sexual activity. J Fam Psychol. 2010;24(3):271–279. [DOI] [PubMed] [Google Scholar]
- 62.Golding JM. Sexual assault history and women’s reproductive and sexual health. Psychol Women Q. 1996;20:101–121. [DOI] [PubMed] [Google Scholar]
- 63.Breiding MJ, Smith SG, Basile KC, Walters ML, Chen J, Merrick MT. Prevalence and characteristics of sexual violence, stalking, and intimate partner violence victimization-national intimate partner and sexual violence survey, United States, 2011. MMWR Surveill Summ. 2014;63(8):1–18. [PMC free article] [PubMed] [Google Scholar]
- 64.Rellini A, Meston C. Sexual function and satisfaction in adults based on the definition of child sexual abuse. The journal of sexual medicine. 2007;4(5):1312–1321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Ghandour RM, Campbell JC, Lloyd J. Screening and counseling for Intimate Partner Violence: a vision for the future. J Womens Health (Larchmt). 2015;24(1):57–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Using trauma theory to design service systems: New directions for mental health services. San Francisco: Jossey-Bass; 2001.
- 67.Sprecher S Sexual satisfaction in premarital relationships: associations with satisfaction, love, commitment, and stability. J Sex Res. 2002;39(3):190–196. [DOI] [PubMed] [Google Scholar]
- 68.Byers ES. Relationship satisfaction and sexual satisfaction: a longitudinal study of individuals in long-term relationships. J Sex Res. 2005;42(2):113–118. [DOI] [PubMed] [Google Scholar]
- 69.Gunst A, Ventus D, Karna A, Salo P, Jern P. Female sexual function varies over time and is dependent on partner-specific factors: a population-based longitudinal analysis of six sexual function domains. Psychological medicine. 2017;47(2):341– 352. [DOI] [PubMed] [Google Scholar]
- 70.Fisher WA, Rosen RC, Eardley I, Sand M, Goldstein I. Sexual experience of female partners of men with erectile dysfunction: the female experience of men’s attitudes to life events and sexuality (FEMALES) study. The journal of sexual medicine. 2005;2(5):675–684. [DOI] [PubMed] [Google Scholar]
- 71.Portman DJ, Brown L, Yuan J, Kissling R, Kingsberg SA. Flibanserin in Postmenopausal Women With Hypoactive Sexual Desire Disorder: Results of the PLUMERIA Study. The journal of sexual medicine. 2017;14(6):834–842. [DOI] [PubMed] [Google Scholar]
- 72.Derogatis LR, Komer L, Katz M, et al. Treatment of hypoactive sexual desire disorder in premenopausal women: efficacy of flibanserin in the VIOLET Study. The journal of sexual medicine. 2012;9(4):1074–1085. [DOI] [PubMed] [Google Scholar]
- 73.Katz M, DeRogatis LR, Ackerman R, et al. Efficacy of flibanserin in women with hypoactive sexual desire disorder: results from the BEGONIA trial. The journal of sexual medicine. 2013;10(7):1807–1815. [DOI] [PubMed] [Google Scholar]
- 74.Goldfischer ER, Breaux J, Katz M, et al. Continued efficacy and safety of flibanserin in premenopausal women with Hypoactive Sexual Desire Disorder (HSDD): results from a randomized withdrawal trial. The journal of sexual medicine. 2011;8(11):3160–3172. [DOI] [PubMed] [Google Scholar]
- 75.Jaspers L, Feys F, Bramer WM, Franco OH, Leusink P, Laan ET. Efficacy and Safety of Flibanserin for the Treatment of Hypoactive Sexual Desire Disorder in Women: A Systematic Review and Meta-Analysis. JAMA internal medicine. 2016. [DOI] [PubMed] [Google Scholar]
- 76.Shifren JL, Braunstein GD, Simon JA, et al. Transdermal testosterone treatment in women with impaired sexual function after oophorectomy. N Engl J Med. 2000;343(10):682–688. [DOI] [PubMed] [Google Scholar]
- 77.Buster JE, Kingsberg SA, Aguirre O, et al. Testosterone patch for low sexual desire in surgically menopausal women: a randomized trial. Obstet Gynecol. 2005;105(5 Pt 1):944-952. [DOI] [PubMed] [Google Scholar]
- 78.Braunstein GD, Sundwall DA, Katz M, et al. Safety and efficacy of a testosterone patch for the treatment of hypoactive sexual desire disorder in surgically menopausal women: a randomized, placebo-controlled trial. Archives of internal medicine. 2005;165(14):1582–1589. [DOI] [PubMed] [Google Scholar]
- 79.Panay N, Al-Azzawi F, Bouchard C, et al. Testosterone treatment of HSDD in naturally menopausal women: the ADORE study. Climacteric: the journal of the International Menopause Society. 2010;13(2):121–131. [DOI] [PubMed] [Google Scholar]
- 80.Shifren JL, Davis SR, Moreau M, et al. Testosterone patch for the treatment of hypoactive sexual desire disorder in naturally menopausal women: results from the INTIMATE NM1 Study. Menopause. 2006;13(5):770–779. [DOI] [PubMed] [Google Scholar]
- 81.Davis SR, Moreau M, Kroll R, et al. Testosterone for low libido in postmenopausal women not taking estrogen. The New England journal of medicine. 2008;359(19):2005–2017. [DOI] [PubMed] [Google Scholar]
- 82.Achilli C, Pundir J, Ramanathan P, Sabatini L, Hamoda H, Panay N. Efficacy and safety of transdermal testosterone in postmenopausal women with hypoactive sexual desire disorder: a systematic review and meta-analysis. Fertility and sterility. 2017;107(2):475-482 e415. [DOI] [PubMed] [Google Scholar]
- 83.Elraiyah T, Sonbol MB, Wang Z, et al. Clinical review: The benefits and harms of systemic testosterone therapy in postmenopausal women with normal adrenal function: a systematic review and meta-analysis. The Journal of clinical endocrinology and metabolism. 2014;99(10):3543–3550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.El-Hage G, Eden JA, Manga RZ. A double-blind, randomized, placebo-controlled trial of the effect of testosterone cream on the sexual motivation of menopausal hysterectomized women with hypoactive sexual desire disorder. Climacteric: the journal of the International Menopause Society. 2007;10(4):335–343. [DOI] [PubMed] [Google Scholar]
- 85.Huang G, Basaria S, Travison TG, et al. Testosterone dose-response relationships in hysterectomized women with or without oophorectomy: effects on sexual function, body composition, muscle performance and physical function in a randomized trial. Menopause. 2014;21(6):612–623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Rahman HA, Malik A, Rahman A, et al. Risk of stroke in women with use of testosterone-containing hormone replacement therapy. Stroke; a journal of cerebral circulation. 2017;48(S1):197. [Google Scholar]
- 87.Hall SA, Araujo AB, Kupelian V, Maserejian NN, Travison TG. Testosterone and breast cancer. The journal of sexual medicine. 2010;7(2 Pt 2):1035–1036; author reply 1036–1037. [DOI] [PubMed] [Google Scholar]
- 88.Dimitrakakis C, Jones RA, Liu A, Bondy CA. Breast cancer incidence in postmenopausal women using testosterone in addition to usual hormone therapy. Menopause. 2004;11(5):531–535. [DOI] [PubMed] [Google Scholar]
- 89.Davis SR, Wolfe R, Farrugia H, Ferdinand A, Bell RJ. The incidence of invasive breast cancer among women prescribed testosterone for low libido. The journal of sexual medicine. 2009;6(7):1850–1856. [DOI] [PubMed] [Google Scholar]
- 90.Brotto LA, Basson R, Luria M. A mindfulness-based group psychoeducational intervention targeting sexual arousal disorder in women. The journal of sexual medicine. 2008;5(7):1646–1659. [DOI] [PubMed] [Google Scholar]
- 91.Brotto LA, Basson R. Group mindfulness-based therapy significantly improves sexual desire in women. Behaviour research and therapy. 2014;57:43–54. [DOI] [PubMed] [Google Scholar]
- 92.Hucker A, McCabe MP. An online, mindfulness-based, cognitive-behavioral therapy for female sexual difficulties: impact on relationship functioning. Journal of sex & marital therapy. 2014;40(6):561–576. [DOI] [PubMed] [Google Scholar]
- 93.Silverstein RG, Brown AC, Roth HD, Britton WB. Effects of mindfulness training on body awareness to sexual stimuli: implications for female sexual dysfunction. Psychosomatic medicine. 2011;73(9):817–825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Brotto LA, Chivers ML, Millman RD, Albert A. Mindfulness-Based Sex Therapy Improves Genital-Subjective Arousal Concordance in Women With Sexual Desire/Arousal Difficulties. Archives of sexual behavior. 2016;45(8):1907–1921. [DOI] [PubMed] [Google Scholar]
- 95.Nappi RE, Palacios S, Panay N, Particco M, Krychman ML. Vulvar and vaginal atrophy in four European countries: evidence from the European REVIVE Survey. Climacteric : the journal of the International Menopause Society. 2016;19(2):188–197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Palma F, Volpe A, Villa P, Cagnacci A. Vaginal atrophy of women in postmenopause. Results from a multicentric observational study: The AGATA study. Maturitas. 2016;83:40–44. [DOI] [PubMed] [Google Scholar]
- 97.Kingsberg SA, Krychman M, Graham S, Bernick B, Mirkin S. The Women’s EMPOWER Survey: Identifying Women’s Perceptions on Vulvar and Vaginal Atrophy and Its Treatment. The journal of sexual medicine. 2017;14(3):413–424. [DOI] [PubMed] [Google Scholar]
- 98.Kingsberg SA, Wysocki S, Magnus L, Krychman ML. Vulvar and vaginal atrophy in postmenopausal women: findings from the REVIVE (REal Women’s VIews of Treatment Options for Menopausal Vaginal ChangEs) survey. The journal of sexual medicine. 2013;10(7):1790–1799. [DOI] [PubMed] [Google Scholar]
- 99.Constantine G, Graham S, Portman DJ, Rosen RC, Kingsberg SA. Female sexual function improved with ospemifene in postmenopausal women with vulvar and vaginal atrophy: results of a randomized, placebo-controlled trial. Climacteric: the journal of the International Menopause Society. 2015;18(2):226–232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Portman D, Palacios S, Nappi RE, Mueck AO. Ospemifene, a non-oestrogen selective oestrogen receptor modulator for the treatment of vaginal dryness associated with postmenopausal vulvar and vaginal atrophy: a randomised, placebo-controlled, phase III trial. Maturitas. 2014;78(2):91–98. [DOI] [PubMed] [Google Scholar]
- 101.Simon JA, Lin VH, Radovich C, Bachmann GA. One-year long-term safety extension study of ospemifene for the treatment of vulvar and vaginal atrophy in postmenopausal women with a uterus. Menopause. 2013;20(4):418–427. [DOI] [PubMed] [Google Scholar]
- 102.Simon J, Portman D, Mabey RG Jr., Long-term safety of ospemifene (52-week extension) in the treatment of vulvar and vaginal atrophy in hysterectomized postmenopausal women. Maturitas. 2014;77(3):274–281. [DOI] [PubMed] [Google Scholar]
- 103.Labrie F, Archer DF, Koltun W, et al. Efficacy of intravaginal dehydroepiandrosterone (DHEA) on moderate to severe dyspareunia and vaginal dryness, symptoms of vulvovaginal atrophy, and of the genitourinary syndrome of menopause. Menopause. 2016;23(3):243–256. [DOI] [PubMed] [Google Scholar]
- 104.Kingsberg SA, Kroll R, Goldstein I, et al. Patient acceptability and satisfaction with a low-dose solubilized vaginal estradiol softgel capsule, TX-004HR. Menopause. 2017;24(8):894–899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Kingsberg SA, Derogatis L, Simon JA, et al. TX-004HR Improves Sexual Function as Measured by the Female Sexual Function Index in Postmenopausal Women With Vulvar and Vaginal Atrophy: The REJOICE Trial. The journal of sexual medicine. 2016;13(12):1930–1937. [DOI] [PubMed] [Google Scholar]
- 106.Perino A, Calligaro A, Forlani F, et al. Vulvo-vaginal atrophy: a new treatment modality using thermo-ablative fractional CO2 laser. Maturitas. 2015;80(3):296– 301. [DOI] [PubMed] [Google Scholar]
- 107.Salvatore S, Nappi RE, Parma M, et al. Sexual function after fractional microablative CO(2) laser in women with vulvovaginal atrophy. Climacteric: the journal of the International Menopause Society. 2015;18(2):219–225. [DOI] [PubMed] [Google Scholar]
- 108.Lewis RW, Fugl-Meyer KS, Bosch R, et al. Epidemiology/risk factors of sexual dysfunction. The journal of sexual medicine. 2004;1(1):35–39. [DOI] [PubMed] [Google Scholar]
- 109.Enzlin P, Mathieu C, Van den Bruel A, Bosteels J, Vanderschueren D, Demyttenaere K. Sexual dysfunction in women with type 1 diabetes: a controlled study. Diabetes care. 2002;25(4):672–677. [DOI] [PubMed] [Google Scholar]
- 110.Rees PM, Fowler CJ, Maas CP. Sexual function in men and women with neurological disorders. Lancet. 2007;369(9560):512–525. [DOI] [PubMed] [Google Scholar]
- 111.Peugh J, Belenko S. Alcohol, drugs and sexual function: a review. Journal of psychoactive drugs. 2001;33(3):223–232. [DOI] [PubMed] [Google Scholar]
- 112.Mishra G, Kuh D. Sexual functioning throughout menopause: the perceptions of women in a British cohort. Menopause. 2006;13(6):880–890. [DOI] [PubMed] [Google Scholar]
- 113.Falk SJ, Dizon DS. Sexual dysfunction in women with cancer. Fertility and sterility. 2013;100(4):916–921. [DOI] [PubMed] [Google Scholar]
- 114.Gilbert E, Ussher JM, Perz J. Sexuality after breast cancer: a review. Maturitas. 2010;66(4):397–407. [DOI] [PubMed] [Google Scholar]
- 115.Jensen PT, Groenvold M, Klee MC, Thranov I, Petersen MA, Machin D. Longitudinal study of sexual function and vaginal changes after radiotherapy for cervical cancer. International journal of radiation oncology, biology , physics. 2003;56(4):937–949. [DOI] [PubMed] [Google Scholar]
- 116.Thakar R, Manyonda I, Stanton SL, Clarkson P, Robinson G. Bladder, bowel and sexual function after hysterectomy for benign conditions. British journal of obstetrics and gynaecology. 1997;104(9):983–987. [DOI] [PubMed] [Google Scholar]
- 117.Carlson KJ. Outcomes of hysterectomy. Clinical obstetrics and gynecology. 1997;40(4):939–946. [DOI] [PubMed] [Google Scholar]
- 118.Strippoli GF, Vecchio M, Palmer S, et al. Sexual dysfunction in women with ESRD requiring hemodialysis. Clinical journal of the American Society of Nephrology: CJASN. 2012;7(6):974–981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Palmer BF. Sexual dysfunction in men and women with chronic kidney disease and end-stage kidney disease. Advances in renal replacement therapy. 2003;10(1):48–60. [DOI] [PubMed] [Google Scholar]
- 120.Salonia A, Zanni G, Nappi RE, et al. Sexual dysfunction is common in women with lower urinary tract symptoms and urinary incontinence: results of a cross-sectional study. European urology. 2004;45(5):642–648; discussion 648. [DOI] [PubMed] [Google Scholar]
- 121.Handa VL, Harvey L, Cundiff GW, Siddique SA, Kjerulff KH. Sexual function among women with urinary incontinence and pelvic organ prolapse. American journal of obstetrics and gynecology. 2004;191(3):751–756. [DOI] [PubMed] [Google Scholar]
- 122.Kennedy SH, Eisfeld BS, Dickens SE, Bacchiochi JR, Bagby RM. Antidepressant- induced sexual dysfunction during treatment with moclobemide, paroxetine, sertraline, and venlafaxine. The Journal of clinical psychiatry. 2000;61(4):276–281. [DOI] [PubMed] [Google Scholar]
- 123.Coleman CC, King BR, Bolden-Watson C, et al. A placebo-controlled comparison of the effects on sexual functioning of bupropion sustained release and fluoxetine. Clinical therapeutics. 2001;23(7):1040–1058. [DOI] [PubMed] [Google Scholar]
- 124.Baumgart J, Nilsson K, Evers AS, Kallak TK, Poromaa IS. Sexual dysfunction in women on adjuvant endocrine therapy after breast cancer. Menopause. 2013;20(2):162–168. [DOI] [PubMed] [Google Scholar]
- 125.Mok K, Juraskova I, Friedlander M. The impact of aromatase inhibitors on sexual functioning: current knowledge and future research directions. Breast. 2008;17(5):436–440. [DOI] [PubMed] [Google Scholar]
- 126.Gershenson DM, Miller AM, Champion VL, et al. Reproductive and sexual function after platinum-based chemotherapy in long-term ovarian germ cell tumor survivors: a Gynecologic Oncology Group Study. Journal of clinical oncology: official journal of the American Society of Clinical Oncology. 2007;25(19):2792–2797. [DOI] [PubMed] [Google Scholar]
- 127.Fogari R, Preti P, Zoppi A, et al. Effect of valsartan and atenolol on sexual behavior in hypertensive postmenopausal women. American journal of hypertension. 2004;17(1):77–81. [DOI] [PubMed] [Google Scholar]
- 128.Newman LC, Broner SW, Lay CL. Reversible anorgasmia with topiramate therapy for migraine. Neurology. 2005;65(8):1333–1334. [DOI] [PubMed] [Google Scholar]
- 129.Morrell MJ, Flynn KL, Done S, Flaster E, Kalayjian L, Pack AM. Sexual dysfunction, sex steroid hormone abnormalities, and depression in women with epilepsy treated with antiepileptic drugs. Epilepsy & behavior: E&B. 2005;6(3):360–365. [DOI] [PubMed] [Google Scholar]
- 130.Lydiard RB, Howell EF, Laraia MT, Ballenger JC. Sexual side effects of alprazolam. The American journal of psychiatry. 1987;144(2):254.-. [DOI] [PubMed] [Google Scholar]
- 131.Ghadirian AM, Annable L, Belanger MC. Lithium, benzodiazepines, and sexual function in bipolar patients. The American journal of psychiatry. 1992;149(6):801– 805. [DOI] [PubMed] [Google Scholar]


