Abstract
Background:
A rapidly increasing BMI trajectory throughout childhood is associated with negative health outcomes in adulthood such as obesity, cardiovascular disease, and diabetes. The purpose of the current study was to assess whether BMI trajectories from age 5-15 predicted changes in weight and BMI from adolescence to adulthood, and dieting-related behaviors in young adulthood.
Methods:
Non-Hispanic White female participants from Early Dieting in Girls (n=182), a longitudinal cohort study, were followed from age 5 to 15 and completed a follow-up survey at age 24. Participants were classified by age 5-15 BMI trajectory groups: UPC, accelerated weight gain from age 5-9; DDPC, accelerated weight gain from 5-9 followed by a decrease; 60PT, weight tracked along 60th percentile; 50PT, weight tracked along 50th percentile. Data at age 24 included self-reported weight, height, dietary restraint, disinhibition, and dieting.
Results:
Majority of participants (80.8%) completed the follow-up survey; of these participants, 60% in UPC group had obesity at age 24, compared to <10% in the other 3 groups. Participants in the UPC group had greater increases in BMI since age 15, compared to the 50PT group, and trend-level greater weight increases than those in the DDPC and 60PT groups. Dietary restraint, but not disinhibition, differed across the groups.
Conclusions:
Children with accelerated weight gain continued to have the greatest weight gain from adolescence to adulthood and the highest prevalence of obesity in adulthood.
Keywords: childhood obesity, adults, dieting, longitudinal
1. Introduction
Children with obesity are 5 times more likely to have obesity as adults, compared to children without obesity; however, despite this strong link, 70% of adults with obesity did not have overweight or obesity as children 1. Taken together, these findings suggest that there are factors such eating behaviors and weight gain trajectories that occur during adolescence and early adulthood that contribute to later-life obesity. The National Longitudinal Study of Adolescent Health reported that the prevalence of obesity doubles during the transition from adolescence to young adulthood 2. During the period of emerging adulthood (roughly ages 18-25)3, lifestyle changes that include transitioning from the parents’ home into independent living, postsecondary education, and employment can result in positive 3, as well as negative long-term health outcomes such as increased risk for weight gain 4, disordered eating, and unhealthy weight control behaviors (e.g., diet pills, vomiting)5. However, despite the importance of both childhood and young adulthood as critical periods for development of obesity, little research has investigated how weight and weight-related behaviors track from childhood to adulthood.
To characterize the tracking of weight status over time, studies often quantify an individual’s rate of weight gain using body mass index (BMI) trajectories. More rapidly increasing BMI trajectories throughout childhood are associated with negative health outcomes including adult obesity 6, 7, cancer 8, cardiovascular disease 9, and diabetes 10. Utilizing data from Early Dieting in Girls, an observational study of the longitudinal development of eating and weight-related behaviors of 197 non-Hispanic White girls from ages 5 to 15 years, Ventura et al. identified four distinct within-person BMI trajectory groups, characterized by different patterns of growth from 5 to 15 years 11. These four groups also differed in some familial risk factors for obesity (e.g. parent BMI, breastfeeding duration), and girls with the most accelerated growth trajectory (i.e., upward BMI percentile crossing) were more likely to have elevated metabolic indicators at age 15, including higher fasting insulin, triglycerides, and blood pressure compared to girls in the other trajectory groups. However, the long-term relevance of these trajectories for adult weight and health behaviors has not been assessed. The objectives of this follow-up study were to re-locate participants from Early Dieting in Girls at age 24, approximately 10 years after last contact, and assess whether BMI trajectories from age 5 to 15, originally described by Ventura et al. 11 predicted change in BMI from adolescence to adulthood, and BMI and dieting-related behaviors in young adulthood. These analyses will help to elucidate the relationship between early life BMI trajectories and critical health-related outcomes in adulthood (e.g., weight status).
2. Methods
2.1. Participants and Procedure for Early Dieting in Girls
Early Dieting in Girls was an observational study of the longitudinal development of eating and weight-related behaviors of girls across childhood and adolescence. Previous publications from this data have examined the etiology and development of dieting and eating behavior in these girls 12-17, trajectories of their growth and development 11, 18, and child and familial characteristics as predictors of weight status 19-21. Participants in the original sample (N=197) were non-Hispanic White girls residing in Central Pennsylvania and enrolled in 1996-1997 at age 5 (mean age: 5.4 ± 0.4 years). Parents and their 5-year old daughters were recruited using flyers and newspaper advertisements. In addition, families with age-eligible female children within a five-county radius of the Pennsylvania State University received mailings and follow-up phone calls (Metromail Inc.). Eligibility criteria for girls’ participation at study entry included: 1) living with their biological mother and father, 2) absence of severe food allergies or chronic medical problems affecting food intake, and 3) absence of dietary restrictions involving animal products. The sample was not recruited based on weight status or eating behavior.
Assessments started when girls were 5 years of age (baseline) and biennially thereafter, until age 15. At each assessment time point, girls visited the clinical research center for a “day-camp” visit where data were collected using parent and child-reported questionnaires (e.g., parent- and child-reports of child feeding practices), trained research staff administered interviews, laboratory-based tasks (e.g., Eating in the Absence of Hunger 21), and clinical assessments (e.g., blood glucose). To make the girl’s visit enjoyable and engaging, there was a developmentally-appropriate theme at each assessment time point; for example, at age 9, the theme was “Space and Time Travel” where the girls made tie-dyed t-shirts. The sample size at each assessment time point was as follows: daughter age 7 (n=192), 9 (n=183), 11 (n=177), 13 (n=168), and 15 (n=167). Attrition between the ages of 5 and 15 was primarily due to family relocation outside of the area. The Pennsylvania State University Institutional Review Board approved all study procedures, and parents provided consent for their family’s participation.
2.2. Follow-up to Early Dieting in Girls
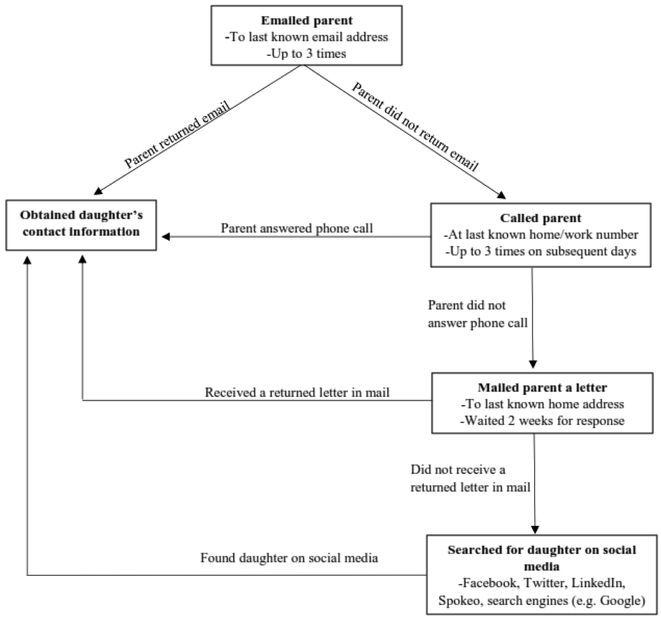
Follow-up measures on this sample were collected in 2015-2016. In order to retain as much of the original sample as possible, all of the 197 girls who participated at age 5 were eligible for the follow-up. The process for obtaining the girls’ 2015/2016 contact information is shown in Figure 1. Once a girl’s contact information was obtained, she was emailed the follow-up survey using REDCap 22, with up to 3 email and phone call reminders. If the girl did not complete the survey electronically, she was mailed a paper copy of the survey to increase completion rates. Girls provided consent before completing the follow-up survey. While all 197 of the original participants were contacted, only the 182 participants that were included in the original analyses of BMI trajectories from 5-15 years described by Ventura et al. 11 were included in the current paper as the primary aim is to examine the BMI trajectory group differences at age 24 .
Figure 1.
Process for obtaining daughters contact information.
2.3. Measures
2.3.1. Demographics.
At ages 5-15, girl’s height and weight were measured in triplicate by a trained staff member and were used to calculate BMI scores (weight (kg)/height (m)2). At age 24, women reported their height and weight, which were used to calculate self-reported BMI. Women were classified as having: underweight (BMI < 18.5), normal weight (BMI 18.5 – 24.9), overweight (BMI 25-29.9), or obesity (BMI ≥ 30). In addition, at age 24, women reported their education level, work status, relationship status, and how many children they have.
2.3.2. Dieting behaviors.
At age 24, dietary restraint, external disinhibition, and emotional disinhibition were measured using the Dutch Eating Behavior Questionnaire (DEBQ) 23, while dieting was assessed by asking, “Are you currently dieting to lose weight?”
2.4. Statistical Analysis
All data analyses were performed using SAS version 9.4 (SAS Institute Inc., Cary, NC). Statistical significance was defined as p < 0.05. Descriptive statistics on mode of locating participants, demographics, and health history were obtained using PROC FREQ. Because only a small number of participants reported having children at age 24 (n=9), these women were excluded from all analyses, given that childbearing influences women’s weight trajectory. Two participants self-reported an underweight BMI and were excluded from the weight-status comparison.
In their previous study, Ventura and colleagues used latent growth mixture modeling techniques (using Mplus) to model developmental trajectories of BMI age 5 to 15 years in the original participants. Given that Mplus allows for estimation of models with missing data using maximum likelihood estimation under missing completely at random and missing at random assumptions, all participants with at least three BMI measurements from age 5 to 15 were included. The number of groups was determined by several fit indices (e.g., AIC, BIC). Posterior probabilities were used to classify girls into one of four groups based on their BMI trajectory from age 5 to 15: 1) Upward Percentile Crossing (UPC); 2) Delayed Downward Percentile Crossing (DDPC); 3) 60th Percentile Tracking (60PT); and 4) 50th Percentile Tracking (50PT). More information on these methods and results is available in the previous publication 11.
Using data from age 24 follow up survey, separate Analysis of Variance (ANOVA) models were used to understand whether these age 5 to 15 BMI trajectory groups differed in: 1) weight change from 15 to 24; 2) BMI change from 15 to 24; 3) self-reported BMI at age 24; and 4) dietary restraint and total, emotional, and external disinhibition at age 24. Chi-square analyses of independence were conducted to examine BMI trajectory group differences in demographics, self-reported dieting, and weight status at age 24.
3. Results
3.1. Participants who completed the follow-up survey
Of the 182 participants included in Ventura et al.’s original BMI trajectories, contact information at the follow-up was obtained from 155 (85.2%) girls. Of these 155 girls, 147 (94.8%) completed the survey (141 via email, and 6 via a mailed copy), for a total response rate of 80.8%. Table 1 reveals that most of the sample was well-educated (71% had a bachelor’s degree or higher) and worked ≥30 hours per week. About one-third reported being single/casually dating, about half reported being in a committed relationship/engaged, and the rest reported being married. The average age of the participants at completion of the follow-up was 23.95 ± .62 years. There were no differences between the groups in any of the demographic variables (ps > .26).
Table 1.
Demographic variables at age 24 by age 5-15 BMI trajectory group(n=136)
| Age 5-15 BMI trajectory group |
||||
|---|---|---|---|---|
| UPC (n=15) |
DDPC (n=24) |
60PT (n=46) |
50PT (n=51) |
|
| Education level | ||||
| High school | 20% | 8% | 11% | 8% |
| Vocational/technical | 0% | 0% | 4% | 4% |
| Associates | 20% | 0% | 11% | 10% |
| Bachelor’s | 47% | 88% | 63% | 67% |
| Graduate | 13% | 4% | 11% | 10% |
| Other | 0% | 0% | 0% | 2% |
| Student status | ||||
| Not a student | 80% | 79% | 61% | 69% |
| Part-time student | 7% | 7% | 17% | 2% |
| Full-time student | 0% | 8% | 7% | 10% |
| Graduate/professional | 13% | 13% | 15% | 19% |
| student | ||||
| Work status | ||||
| < 30 hours/week | 33% | 22% | 15% | 20% |
| 30+ hours/week | 67% | 75% | 80% | 74% |
| No answer | 0% | 3% | 4% | 6% |
| Relationship status | ||||
| Single/casually | 53% | 33% | 33% | 39% |
| dating | ||||
| Committed | 40% | 54% | 54% | 51% |
| relationship/engaged | ||||
| Married | 7% | 8% | 13% | 10% |
| Separated/divorced | 0% | 4% | 0% | 0% |
UPC = upward percentile crossing; DDPC = delayed downward percentile crossing; 60PT = 60th percentile tracking; 50PT = 50th percentile tracking
There were no significant differences between the groups in any of the demographic variables
3.2. BMI change, weight change, and weight status by BMI trajectory
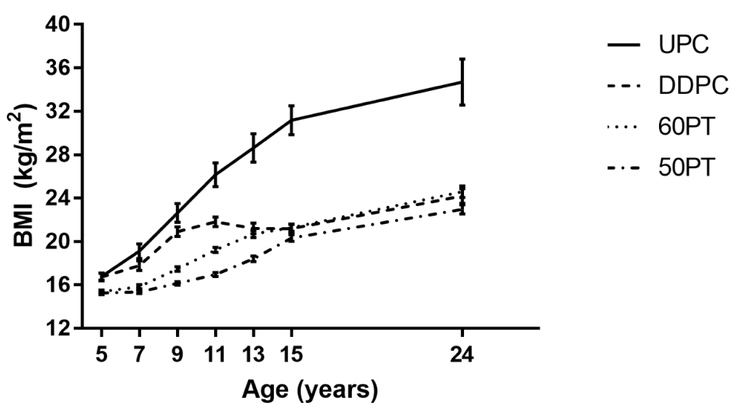
At follow-up, the frequency of participants from each of the four age 5-15 BMI trajectory groups was as follows: 1) UPC, n=15; 2) DDPC, n=24; 3) 60PT, n=46; 4) 50PT, n=51 Updated BMI trajectories from age 5-24 are shown in Figure 2. Age 24 BMI and weight status, as well as BMI change and weight change from 15 to 24 are shown in Table 2. BMI at age 24 was highest for the UPC group compared to the other 3 groups (p < 0.001), with no other group differences. The UPC group had greater BMI change from 15 to 24 than the 50PT group (p < 0.05), with no other significant group differences. Similarly, the UPC group had greater weight gain from 15 to 24 than the 50 PT group (p < 0.05), with a trend towards greater weight gain compared to the DDPC and 60PT groups (p = 0.08 and 0.07, respectively). There were no group differences in height change from 15 to 24 (p = 0.42). The groups differed in their proportion of individuals at each weight status (p < 0.0001), such that the UPC group had a different weight status distribution than the other 3 groups (p < 0.0001), with 60% of the UPC group having obesity at age 24, compared to less than 10% in either of the other three groups. Similarly, only 7% of those in the UPC group were of normal weight, compared to >60% in the other three groups.
Figure 2.
Body mass index (BMI) trajectories from 5 to 24 years of age by age 5-15 BMI trajectory group. UPC = upward percentile crossing (n=15); DDPC = delayed downward percentile crossing (n=24); 60PT = 60th percentile tracking (n=46); 50PT = 50th percentile tracking (n=51)
Table 2.
Self-reported BMI, weight change, and weight status at age 24 by age 5-15 BMI trajectory group (n=136)
| Age 5-15 BMI trajectory group |
||||
|---|---|---|---|---|
| UPC (n=15; 11%) |
DDPC (n=24; 18%) |
60PT (n=46; 34%) |
50PT (n=51; 37%) |
|
|
BMI change from 15 to 24 yrs (kg/m2) |
4.8 (5.5)a | 3.1 (4.0)ab | 3.4 (2.6)ab | 2.7 (2.3)b |
|
Weight change from 15 to 24 yrs (lbs) |
31.9 (31.8)a | 20.4 (24.2)ab | 21.0 (14.3)ab | 18.1 (13.7)b |
|
Height change from 15 to 24 yrs (in) |
0.5 (0.9)a | 0.5 (0.5)a | 0.2 (0.8)a | 0.5 (1.0)a |
| BMI, 24 yrs (kg/m2) | 34.7 (8.3)a | 24.2 (3.3)b | 24.6 (3.8)b | 22.9 (2.9)b |
| Weight Status, 24 yrs* | ||||
| Normal weight, % | 7a | 63b | 65b | 80b |
| Overweight, % | 33 | 29 | 26 | 18 |
| Obesity, % | 60 | 8 | 9 | 2 |
Data are shown as mean (SD) or as %
Body Mass Index (BMI) and weight status at 24 years calculated from self-reported height and weight
Means within a row followed by the same superscript are not significantly different
Chi-square analysis tested the distribution of cases across the 3 weight statuses for the 4 BMI trajectory groups.
UPC = upward percentile crossing; DDPC = delayed downward percentile crossing; 60PT = 60th percentile tracking; 50PT = 50th percentile tracking
3.3. Dieting and weight control behaviors and characteristics by BMI trajectory
At age 24, 29% of the participants reported currently dieting to lose weight. Dieting to lose weight differed among the BMI trajectory groups (p < 0.01); post-hoc comparisons revealed that a significantly lower proportion of 50PT group reported dieting to lose weight (16%) compared to the other 3 groups, with no other significant differences between the groups (at 50%, 44%, and 30% for UPC, DDPC, and 60PT, respectively).
Dietary restraint, total disinhibition, external disinhibition, and emotional disinhibition for each of the BMI trajectory groups are shown in Table 3. Dietary restraint differed across the groups (p < 0.01). The DPPC group had a higher level of restraint than the 60PT and 50PT groups (p’s < 0.05), but did not differ from the UPC group (p > 0.10). The UPC group had higher restraint than participants in the 50PT group (p < 0.05). There were no other group differences in restraint. Total disinhibition (p= 0.29), external disinhibition (p = 0.81), and emotional disinhibition (p = 0.15) did not differ across the groups.
Table 3.
Dietary restraint and disinhibition at age 24 by age 5-15 BMI trajectory group (n=136)
| BMI trajectory group |
||||
|---|---|---|---|---|
| UPC (n=15; 11%) |
DDPC (n=24; 18%) |
60PT (n=46; 34%) |
50PT (n=51; 37%) |
|
|
Dietary Restraint |
2.9 (0.8)ab | 2.9 (0.7)a | 2.5 (0.7)bc | 2.3 (0.9)c |
|
Total disinhibition |
2.9 (0.9)a | 2.7 (0.6)a | 2.7 (0.6)a | 2.6 (0.6)a |
|
External disinhibition |
3.0 (0.8)a | 3.1 (0.7)a | 3.0 (0.6)a | 2.9 (0.6)a |
|
Emotional disinhibition |
2.8 (1.3)a | 2.3 (0.8)a | 2.4 (0.8)a | 2.2 (0.7)a |
Data are shown as mean (SD)
Means within a row followed by the same superscript are not significantly different UPC = upward percentile crossing; DDPC = delayed downward percentile crossing; 60PT = 60th percentile tracking; 50PT = 50th percentile tracking
4. Discussion
This follow-up study extended findings from Early Dieting in Girls by characterizing weight status at age 24 based on BMI trajectories obtained when girls were ages 5-15 11. The main outcomes of this study indicate that at age 24, three of the four BMI trajectory groups (DDPC, 60PT, and 50PT) had similar mean self-reported BMI, all in the normal weight range. However, the UPC group, who had higher BMIs and the greatest increases in BMI during childhood and adolescence, remained heavier than these other groups. In addition, participants in the UPC group had higher prevalence of overweight/obesity than the other 3 groups, with 93% having overweight/obesity compared to 20-35% in the other three groups. Findings from the current study are consistent with findings from previous studies that weight status is relatively stable over time 24, 25.
As shown in Ventura et al.11, participants in both the UPC and DDPC groups had accelerated weight gain from ages 5 to 9, but the two groups diverged in adolescence with the accelerated weight gain persisting into adolescence only for the UPC group. Results from our follow-up analyses indicate that this pattern continued into adulthood, with participants in the UPC group remaining at a higher weight status than the other groups. In addition, participants in the UPC group experienced greater weight gain between ages 15 and 24 than the other 3 groups, albeit at a trend level when compared to those in the DDPC and 60PT groups. Given that individuals with obesity are more likely to underreport their weight 26, weight gain differences in the current study may have been attenuated, with even greater differences seen if using measured weight.
The increased rates of obesity and continued accelerated weight gain seen in the UPC group is particularly concerning given that participants in this group were already presenting with metabolic outcomes in adolescence 11, 27. Previous work in the current sample found that girls with higher BMIs and greater fat mass across childhood had higher levels of metabolic syndrome indicators (e.g., high triglycerides, high waist circumference) in adolescence 21. As such, especially given that there was a large amount of overlap between girls with accelerated weight gain between childhood and adolescence and metabolic indicators in adolescence, it would be expected that these individuals would be at even higher risk for having metabolic outcomes in adulthood. However, given that metabolic measures were not obtained at follow-up, future work is needed to confirm the relationship between persistent early accelerated weight gain and/or childhood obesity and the progression of the metabolic outcomes in adulthood, especially given that an elevated weight status in adulthood increases risk of metabolic comorbidities. These findings speak to the importance of childhood obesity treatment and the prevention of rapid weight gain during youth. If given access to efficacious evidence-based obesity treatment or prevention strategies, a child’s risk of becoming an adult with obesity and the associated co-morbidities can be drastically reduced 28, 29.
There were limited differences between the groups in dietary restraint, and no differences between the groups in disinhibition. While the groups differed in their level of dietary restraint, these differences were not only due to differences in weight (i.e., restraint did not differ between the UPC and DDPC groups despite the UPC being heavier). While the current study may be limited by the relatively small sample size of the UPC group, these findings are in agreement with the majority of the extant literature that has failed to find a relationship between restraint and weight 30, 31. The lack of a relationship between weight group and disinhibition in the current study is particularly surprising and contrary to other literature 30, 31. However, the UPC group did have greater disinhibition than the other three groups, and the relatively small sample size of the UPC group may have precluded these differences from reaching statistical significance.
Roughly 30% of participants reported currently dieting to lose weight at age 24, similar to rates of recent dieting (i.e., current dieting or dieting within the past week) among young adults 32. Rates of self-reported dieting are higher among those with elevated BMIs 33, 34. However, rates of dieting were not higher for the UPC group compared to the DDPC and 60PT group, despite the UPC group having much higher rates of overweight/obesity. As such, BMI is likely not the only factor driving reports of dieting to lose weight. . It is plausible that there may be differences in what is thought of as dieting 17, and thus potentially the groups had similar rates of dieting but were engaging in different behaviors. However, future work is needed to examine the specific weight control behaviors used by these groups when they diet.
Over 80% of the original sample completed the follow-up survey at age 24, despite having no contact from the research team since age 15. The retention rate through age 15 years in the original study was very high (85%), and may have been due, in part, to the fun (i.e., the original study was conducted as a day camp) and personal (e.g., parents were given pictures of their daughter) nature of the study. Additionally, the study team made every effort to keep participants in the study despite normal life-events that occurred over the original ten-year period (e.g., death of a parent, move outside of the local area). In addition, the research team maintained contact with the participants in the two-years between every wave of data collection by sending newsletters and birthday cards. It is likely that these strategies created a positive experience for the participants and helped to yield the high retention rate. It is also possible that the positive experiences of both the participants and their parents from age 5 to 15 likely encouraged them to complete the follow-up study at age 24.
A key strength of the Early Dieting in Girls cohort includes the depth and breadth of longitudinal data that was collected on participants. Few studies have the ability to examine weight trajectories and weight-related characteristics over this duration of time and across a wide range of growth and development (i.e., from childhood to adulthood). Additionally, the retention level was extremely high over this period, which reduces traditional biases (e.g., selective dropout) of longitudinal studies. The sample is predominately non-Hispanic, White females, which limits the generalizability of these findings to other populations (i.e., males, females of more diverse populations). As such, additional work is needed to confirm these findings in other populations. The current sample, and the associated BMI trajectory groups, is also relatively small, and findings should be replicated with a larger sample. Another limitation is that all of the data included from the current study were self-reported. Some of the questions, such as those on dieting to lose and maintain weight, may be more susceptible to self-report bias. Moreover, while height and weight were measured from ages 5 to 15, both were self-reported at age 24. While prior work has found that self-reported height and weight are reliable proxies for measured height and weight 35, there is systematic error in self-reported weight, with greater underreporting for individuals with obesity 26. As such, the use of self-reported weights may underestimate the difference among the groups.
5. Conclusions
In summary, weight status, and eating behavior data were obtained at age 24 from more than 75% of the Early Dieting in Girls sample, who were seen biennially age 5 to 15, highlighting the feasibility of collecting this information. These data show that individuals with accelerated weight gain from childhood to adolescence also had the highest levels of weight gain from adolescence to adulthood and the highest levels of overweight/obesity in adulthood, indicating children with accelerated weight gain from childhood to adolescence may benefit from obesity treatment to prevent the onset of adult obesity. Within the follow-up survey, most participants indicated that they would be interested and willing to participate in a longer follow-up study. As such, future work with this sample will assess a larger battery of psychological and physiological measures to identify how modifiable, early life predictors (i.e., both individual and parent-level characteristics) such as weight status relate to cardiometabolic risk factors and eating behaviors in adulthood. Data will provide information to identify risks and protective factors that can be used as intervention targets in the prevention and/or treatment of obesity and maladaptive eating behaviors in young adults.
Highlights.
The current study highlights the feasibility of collecting follow-up data in adulthood on a sample seen during childhood and adolescence.
Individuals with accelerated weight gain during childhood continued to have the greatest weight gain from adolescence to adulthood.
Individuals with accelerated weight gain in childhood had the highest prevalence of obesity in adulthood.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Simmonds M, Llewellyn A, Owen CG, Woolacott N. Predicting adult obesity from childhood obesity: A systematic review and meta-analysis. Obes Rev 2016; 17(2):95–107. [DOI] [PubMed] [Google Scholar]
- 2.Gordon-Larsen P, Adair LS, Nelson MC, Popkin BM. Five-year obesity incidence in the transition period between adolescence and adulthood: The national longitudinal study of adolescent health. Am J Clin Nutr 2004; 80(3):569–575. [DOI] [PubMed] [Google Scholar]
- 3.Arnett JJ. Emerging adulthood: What is it, and what is it good for? Child development perspectives 2007; 1(2):68–73. [Google Scholar]
- 4.Nelson MC, Story M, Larson NI, Neumark-Sztainer D, Lytle LA. Emerging adulthood and college aged youth: An overlooked age for weight- related behavior change. Obesity 2008; 16(10):2205–2211. [DOI] [PubMed] [Google Scholar]
- 5.Neumark-Sztainer D, Wall M, Larson NI, Eisenberg ME, Loth K. Dieting and disordered eating behaviors from adolescence to young adulthood: Findings from a 10-year longitudinal study. Journal of the American Dietetic Association 2011; 111(7): 1004–1011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Li S, Chen W, Sun D, et al. Variability and rapid increase in body mass index during childhood are associated with adult obesity. Int J Epidemiol 2015; 44(6): 1943–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Peneau S, Giudici KV, Gusto G, et al. Growth trajectories of body mass index during childhood: Associated factors and health outcome at adulthood. J Pediatr 2017. [DOI] [PubMed] [Google Scholar]
- 8.Aarestrup J, Gamborg M, Tilling K, et al. Childhood body mass index growth trajectories and endometrial cancer risk. Int J Cancer 2017; 140(2):310–315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Barker DJP, Osmond C, Forsen TJ, Kajantie E, Eriksson JG. Trajectories of growth among children who have coronary events as adults. New Engl J Med 2005; 353(17):1802–1809. [DOI] [PubMed] [Google Scholar]
- 10.Bhargava SK, Sachdev HS, Fall CH, et al. Relation of serial changes in childhood body-mass index to impaired glucose tolerance in young adulthood. N Engl J Med 2004; 350(9):865–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ventura AK, Loken E, Birch LL. Developmental trajectories of girls' bmi across childhood and adolescence. Obesity (Silver Spring) 2009; 17(11):2067–74. [DOI] [PubMed] [Google Scholar]
- 12.Balantekin KN, Birch LL, Savage JS. Eating in the absence of hunger during childhood predicts self-reported binge eating in adolescence. Eat Behav 2017; 24:7–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shunk JA, Birch LL. Girls at risk for overweight at age 5 are at risk for dietary restraint, disinhibited overeating, weight concerns, and greater weight gain from 5 to 9 years. J Am Diet Assoc 2004; 104(7): 1120–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Carper JL, Orlet Fisher J, Birch LL. Young girls' emerging dietary restraint and disinhibition are related to parental control in child feeding. Appetite 2000; 35(2):121–9. [DOI] [PubMed] [Google Scholar]
- 15.Francis LA, Birch LL. Maternal influences on daughters' restrained eating behavior. Health Psychol 2005; 24(6):548–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Balantekin KN, Savage JS, Marini ME, Birch LL. Parental encouragement of dieting promotes daughters' early dieting. Appetite 2014; 80:190–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Balantekin KN, Birch LL, Savage JS. Patterns of weight-control behavior among 15 year old girls. Int J Eat Disord 2015; 48(6):589–600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Davison KK, Birch LL. Child and parent characteristics as predictors of change in girls' body mass index. Int J Obes Relat Metab Disord 2001; 25(12):1834–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Anzman SL, Birch LL. Low inhibitory control and restrictive feeding practices predict weight outcomes. J Pediatr 2009; 155(5):651–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Berger PK, Hohman EE, Marini ME, Savage JS, Birch LL. Girls' picky eating in childhood is associated with normal weight status from ages 5 to 15 y. Am J Clin Nutr 2016; 104(6):1577–1582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fisher JO, Birch LL. Eating in the absence of hunger and overweight in girls from 5 to 7 y of age. Am J Clin Nutr 2002; 76(1):226–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (redcap) - a metadata-driven methodology and workflow process for providing translational research informatics support. Journal of biomedical informatics 2009; 42(2):377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Van Strien T, Frijters JE, Bergers G, Defares PB. The dutch eating behavior questionnaire (debq) for assessment of restrained, emotional, and external eating behavior. International journal of eating disorders 1986; 5(2):295–315. [Google Scholar]
- 24.Evensen E, Wilsgaard T, Furberg AS, Skeie G. Tracking of overweight and obesity from early childhood to adolescence in a population-based cohort - the tromso study, fit futures. BMC pediatrics 2016; 16:64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Juonala M, Magnussen CG, Berenson GS, et al. Childhood adiposity, adult adiposity, and cardiovascular risk factors. New Engl J Med 2011; 365(20):1876–1885. [DOI] [PubMed] [Google Scholar]
- 26.Connor Gorber S, Tremblay M, Moher D, Gorber B. A comparison of direct vs. Self-report measures for assessing height, weight and body mass index: A systematic review. Obes Rev 2007; 8(4):307–26. [DOI] [PubMed] [Google Scholar]
- 27.Ventura AK, Loken E, Birch LL. Risk profiles for metabolic syndrome in a nonclinical sample of adolescent girls. Pediatrics 2006; 118(6):2434–2442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wilfley DE, Stein RI, Saelens BE, et al. Efficacy of maintenance treatment approaches for childhood overweight: A randomized controlled trial. Jama 2007; 298(14):1661–1673. [DOI] [PubMed] [Google Scholar]
- 29.Epstein LH, Paluch RA, Roemmich JN, Beecher MD. Family-based obesity treatment, then and now: Twenty-five years of pediatric obesity treatment. Health Psychology 2007; 26(4):381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.French SA, Mitchell NR, Wolfson J, et al. Questionnaire and laboratory measures of eating behavior. Associations with energy intake and bmi in a community sample of working adults. Appetite 2014; 72:50–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bellisle F, Clement K, Le Barzic M, et al. The eating inventory and body adiposity from leanness to massive obesity: A study of 2509 adults. Obesity research 2004; 12(12):2023–30. [DOI] [PubMed] [Google Scholar]
- 32.Liechty JM, Lee MJ. Longitudinal predictors of dieting and disordered eating among young adults in the us. International Journal of Eating Disorders 2013; 46(8):790–800. [DOI] [PubMed] [Google Scholar]
- 33.Neumark-Sztainer D, Story M, Hannan PJ, Perry CL, Irving LM. Weight-related concerns and behaviors among overweight and nonoverweight adolescents: Implications for preventing weight-related disorders. Archives of Pediatrics & Adolescent Medicine 2002; 156(2):171–178. [DOI] [PubMed] [Google Scholar]
- 34.López-Guimerà G, Neumark-Sztainer D, Hannan P, et al. Unhealthy weight-control behaviours, dieting and weight status: A cross-cultural comparison between north american and spanish adolescents. European eating disorders review : the journal of the Eating Disorders Association 2013; 21(4):276–283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Rowland ML. Self-reported weight and height. Am J Clin Nutr 1990; 52(6): 1125–33. [DOI] [PubMed] [Google Scholar]