Inhaled NO (iNO) is an approved therapy for pulmonary hypertension (PH) in term infants and its use is now increasing in preterm infants with hypoxemic respiratory failure (HRF) and, or, PH, despite the lack of sustained benefits.
In the current issue of Acta Paediatrica, Dixon et al report that iNO use in the neonatal intensive care unit (NICU) may increase childhood cancer (1). In an earlier publication, Naumburg et al found that delivery room oxygen may increase childhood leukemia (2). Spector et al agree confirmed this association (3).
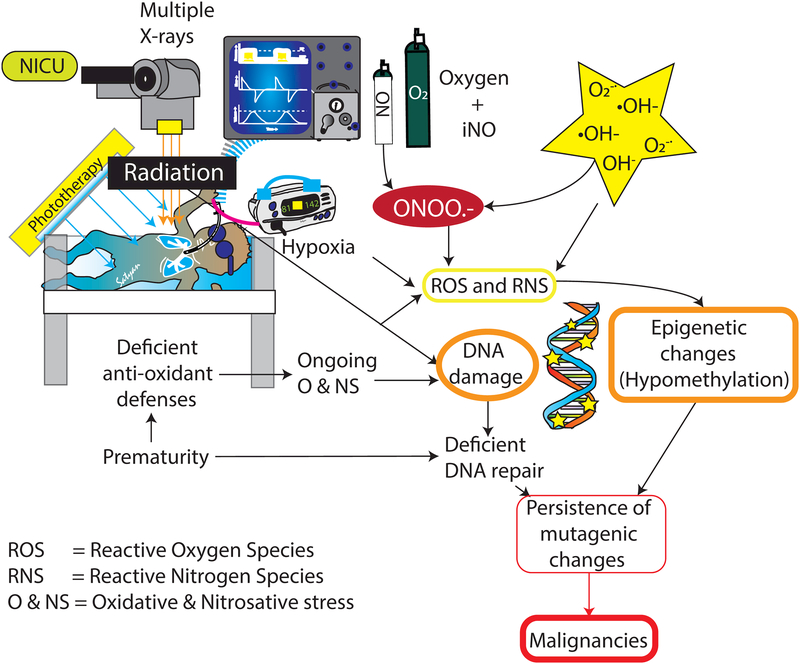
Newborn infants, particularly those born preterm, lack robust anti-oxidant defence systems and are more susceptible to free radical injuries. Oxygen toxicity leading to accumulations of superoxide anions and hydroxyl radicals can cause irreversible cell damage. Similarly, NO is a highly reactive free radical and using excessive, exogenous NO with oxygen leads to reactive nitrogen species, which can induce durable, irreversible cell changes. Furthermore, oxygen and nitrogen free radicals combine to generate peroxynitrite, a powerful oxidant known to trigger apoptosis or necrosis. Free radicals can damage DNA in various ways and premature infants tend to have persistent mutagenic changes due to their immature enzymatic repair system (e.g. DNA glycosylases) (4). Long-lasting DNA changes favour epigenome hypomethylation, which leads to chronic conditions and cancer (5).
One hundred percent oxygen was the main therapeutic option for newborn infants with respiratory distress until research showed that prolonged exposure to high concentrations increased the risk of blindness. The full risks posed by even brief exposure to hyperoxia are becoming apparent. Neonatologists may now face similar conundrums administering iNO to newborn infants with HRF and PH.
Current evidence suggests that NO can lead to nitrosative stress and Dixon et al’s observation of a possible link between iNO and cancer in NICU patients, is a stark reminder that premature infants are highly vulnerable to free radical damage. We really need to know what nitrogen reactive species are most harmful and what biological pathways are implicated. Continuously monitoring preterm infants in NICUs using novel markers of oxidative and nitrosative stress is necessary to detect the cumulative effect of X-ray irradiation, phototherapy, hyperoxic ventilation and iNO (Figure 1).
Figure 1.
The cumulative effect of various NICU factors may increase the risk of childhood malignancies.
Acknowledgments
FINANCE
NIH 2 R01 HD072929 06 (SL)
ABBREVIATIONS
- iNO
inhaled nitric oxide
- NICU
neonatal intensive care unit
Footnotes
CONFLICTS OF INTEREST
None to declare.
References
- 1.Dixon F, Ziegler DS, Bajuk B, Wright I, Hilder L, Abdel Latif ME, et al. Treatment with nitric oxide in the neonatal intensive care unit is associated with increased risk of childhood cancer. Acta Paediatr 2018. [DOI] [PubMed] [Google Scholar]
- 2.Naumburg E, Bellocco R, Cnattingius S, Jonzon A, Ekbom A. Supplementary oxygen and risk of childhood lymphatic leukaemia. Acta Paediatr 2002; 91 12:1328–33. [DOI] [PubMed] [Google Scholar]
- 3.Spector LG, Klebanoff MA, Feusner JH, Georgieff MK, Ross JA. Childhood cancer following neonatal oxygen supplementation. J Pediatr 2005;147:27–31. [DOI] [PubMed] [Google Scholar]
- 4.Vande Loock K, Ciardelli R, Decordier I, Plas G, Haumont D, Kirsch-Volders M. Preterm newborns show slower repair of oxidative damage and paternal smoking associated DNA damage. Mutagenesis 2012;27:573–80. [DOI] [PubMed] [Google Scholar]
- 5.Eden A, Gaudet F, Waghmare A, Jaenisch R. Chromosomal instability and tumors promoted by DNA hypomethylation. Science 2003;300:455. [DOI] [PubMed] [Google Scholar]