ABSTRACT
Background:
Disrespectful and undignified care during childbirth has been documented in health facilities all over the world. The purpose of this study was to develop and pretest a new instrument, the Quality of Respectful Maternity Care Questionnaire in Iran (QRMCQI), with an ensured validity and reliability to evaluate and measure Respectful Maternity Care (RMC) in three sections of labor, delivery and post-partum.
Methods:
This is a study with mixed sequential exploratory design. Here, the questionnaire design is a part of descriptive survey study and consists of five phases implemented in one year. The phases include item or questions generation, face validation, content validity assessment, confirmatory factor analysis and reliability assurance of the questionnaire. The participants were selected from the mothers referring to health care centers affiliated to Iran University of Medical Sciences in five cities after recruitment from hospital for after-care services of delivery.
Results:
The primary questionnaire was developed, face validity was performed by experts and their comments were implemented. The content validity index (CVI), Kappa index and Content Validity Ratio (CVR) were calculated for each item and they were satisfactory in an acceptable range. Confirmatory factor analysis (CFA) showed good fit of the hypothesized model for 453 participants in the interview. Testing showed an acceptable internal consistency and reliability by calculating Cronbach’s alpha coefficient for questions in labor (0.86), in delivery (0.85), and in postpartum care (0.78).
Conclusion:
We have developed a new instrument as the 59-item QRMCQI for evaluating respectful maternity care in Iran through a rigorous process of item generation and validity-reliability assessment besides confirmatory factor analysis that were in an acceptable range and can be used as a reliable instrument for RMC in Iran.
KEYWORDS: Confirmatory factor analysis , Questionnaire , Respectful maternity care , Validity , Reliability
INTRODUCTION
Disrespectful and undignified care during childbirth has been reported and documented in health facility centers all over the world.1 Over recent years, promotion of the usage of Respectful Maternity Care (RMC) has been developed gradually, emphasizing the importance of underlying professional ethics and considering psychological, social and cultural aspects of health care delivery as essential elements of care.2 While medical treatment is only one aspect of RMC, failure to focus on the well-being of women and newborns by imposing unnecessary or harmful practices can be considered abusive and disrespectful.3
Respectful maternity care obviously leads to patient satisfaction during childbirth including the quality of both physical interactions and inter-personal relations between care provider and pregnant woman.3 Considering the importance of improvement in maternity care and the necessity of planning for better health care services in RMC, evaluating the provided care with suitable tools in maternity care centers and balancing various medical and communicational aspects of treatment are the main goals.
Satisfactory evaluation in midwifery services has been investigated in many studies in Iran, but no study has clearly been done on respectful maternity care evaluation, so providing a new tool and questionnaire for RMC in Iran seems to be necessary.
RMC is an approach focusing on the personal relations during care. These relations are based on principles of ethics, respect for human rights, and increase in the importance of efforts that recognize women’s and newborns’ preferences and needs. Disrespect and Abuse (D&A) of women during facility-based childbirth is not a new phenomenon and has been an issue since 1950s. Different researchers worked on disrespect and abuse and today human rights organizations consider and document it formally. The main formal efforts are combined in World Health Organization (WHO) as a universally organized center for health. WHO published a statement for preventing disrespect and abuse against childbearing mothers.4 The categories of D&A and the corresponding rights are categorized in seven sections (Table 1).1
Table 1.
The categories of disrespect and abuse and the corresponding rights, Bowser and Hill (2010)
| Categories of Disrespect and Abuse | Categories of Corresponding Right | Items of Questionnaire |
|---|---|---|
| Physical abuse | Freedom from harm and ill treatment | 18, 26, 27, 28, 32, 33, 52 |
| Non-consented care | Right to information, informed consent and refusal, and respect for choices and preferences, including the right to companionship of choice wherever possible | 1, 4, 5, 6, 12, 13, 14, 15, 21, 22, 23, 24, 25, 29, 30, 31, 35, 36, 37, 38, 39, 42, 43, 44, 46, 47, 49, 53, 54, 55, 58 |
| Non-confidential care | Confidentiality, privacy | 19, 20, 45 |
| Non-dignified care (including verbal abuse) | Dignity, respect | 2, 3, 7, 8, 10, 11, 16, 17 |
| Discrimination based on specific attributes | Equality, freedom from discrimination, equitable care | 9, 41 |
| Abandonment or denial of care | Right to timely health care and to the highest attainable level of health | 34, 40, 48, 50, 51, 56, 57 |
| Detention in facilities | Liberty, autonomy, self-determination, and freedom from coercion | 59 |
In an analysis performed among worldwide survey data on the subject, seven categories of disrespect and abuse during childbirth developed from different qualitative reports around the world: physical abuse, delivery of care without the patient’s consent, non-confidential care, non-dignified care, discrimination, abandonment, and detention in health care facilities.1
The questionnaires in most of the reviewed studies are only based on seven D&A categories and the results of any item are described under each category. It will help to generate and develop questions; on the other hand, having a classified questionnaire based on labor, delivery and postpartum is more useful to give ideas for maternal health care planning in each section. However, in a global review of 65 studies across 34 countries, it was confirmed that few quantitative tools exist for measuring the experience of respect in maternity care.5
With respect to patients’ and clients’ rights, improving the quality of maternity care and reaching RMC must be the main goal of health care system.5 One way for reaching this goal is evaluating the provided care with suitable tools in maternity care centers, hospitals and clinics and assessing various factors, such as physical and communicational aspects of treatment which affect RMC.6
Regarding all the above-mentioned points, development of a valid and reliable tool for evaluating respectful maternity care and its quality is a critical scientific basis for studies to monitor the provision and benefits of respectful maternity health care services.
Promoting the level of maternity care in Iran is under consideration and it is planned in governmental and private sections; there is a need to determine how the current situation can be measured and make decisions based on present evaluations. Providing a reasonable instrument in RMC needs consideration of all aspects of the questionnaire and checking it scientifically in all related methods. Since there were no evidence of RMC quality measurement in Iran before starting this study, we aimed to develop and test the Quality of Respectful Maternity Care Questioner (QRMCQI) in Iran, conduct content and face validity, assess its reliability, and evaluate it based on factor analysis for assessing RMC by asking the clients who were women who had received care during labor, delivery and post-partum.
MATERIALS AND METHODS
This is a study with mixed sequential exploratory design method which addressed the development, validation and evaluation of a research instrument. Following the methodological frameworks for developing measurement scales described by Streiner and Norman7 and Gronvik et al.,8 the study consisted of five phases implemented in one year.
Phase One: Questionnaire Development
Phase one was questionnaire development in order to evaluate respectful maternity care in three sections of labor, delivery and post-partum based on seven categories of disrespect and abuse developed by White Ribbon Alliance in 2011, under the charter of respectful maternity care.1 Item or questions generation, rating of the importance of items, and item presentation were the main steps in this phase.
After a detailed literature review by the research team and gathering qualitative data, a questionnaire consisting of 83 questions was generated from WHO sources and guidelines in RMC. It consisted of 6 parts, the first three parts of which contained 26 demographic questions and the next three parts were all 57 qualitative questions about respectful maternity care during labor (40 questions), delivery (9 questions) and postpartum (8 questions). The first section included personal information like age, date of birth, nationality, education level and also items about work and level of income. The second section consisted of pregnancy history information like the number of delivery or abortion. The third section of the questionnaire addressed the health service facilities like the type of the hospital, costs, and insurance type. The last three sections contained questions about respectful maternity care in Likert five-point scale. When constructing this section for 57 questions, the research team decided that each item would be rated using a Likert scale with five response categories consisting of “All the times” (4), “Most of the times” (3), “Some Times” (2), “Seldom” (1) and “Never” (0).
Phase Two: The Validation of the Tool: Face Validity
Validity, which is defined as the ability of an instrument to measure the properties of the construct under the study,9 is a vital factor in selecting or applying an instrument. Validity is not considered as the possession of an instrument and actually belongs to the scores obtained by an instrument used for a specific purpose on a special group of interviewees.10
Phase two consisted of face validation based on both qualitative and quantitative method. In qualitative face validation, the questionnaire assessed the level of difficulty, symmetry and eloquence in a panel consisting of four experts in maternity healthcare and their points organized in items. Experts attending the panel also provided comments about the number of items; similar items needed edition and some changes were necessary to make them clearer for the respondents; also, they gave some suggestions to revise the conceptual and grammatical format of the questions. Then, the questionnaire revised to address these issues and classified based on seven RMC categories.1 Quantitative face validity was assured by measuring the impact score of each item after pretest of the questionnaire by 30 interviews. If the impact score of a question was equal to or greater than 1.5 (which corresponds to a mean frequency of 50% and an importance mean of 3 on the 5-point Likert scale), it was maintained in the QRMCQI; otherwise, it was eliminated. Pretesting was used to ensure that the items were clearly written and were being interpreted correctly.7 In this phase, two questions were added to the RMC Likert-based questions and 59 items in this part were confirmed. One question was added to labor and one question to the delivery section.
Phase Three: The Validation of the Tool: Content Validity
Content validity, known as definition validity and logical validity,11 is a primary requirement for other types of validity and is essential to have the highest priority during instrument development and addresses the degree to which items of a questionnaire sufficiently represent the content area of the research.12 It can provide information on the representativeness and clarity of items and help improve an instrument through gathering recommendations from an expert panel.12
Phase three was content validity assurance by qualitative and quantitative methods. Regarding the content validity, we asked 20 experts to review the questionnaire and comment on each item based on four criteria including relevancy, clarity, simplicity, and necessity. Half of the experts (10 people) were from the Ministry of Health and Medical Education who had experience in maternity and health care management with opinions related to RMC; five experts were experienced midwives in high levels of hospital management centers and five were members of university academic staff who had experience in maternity health care.
These experts were asked to indicate (a) the extent to which the questionnaire items reflected the RMC standards and (b) the extent to which an expert could rate each questionnaire item as a learning need. Content Validity Ratio (CVR) was calculated based on the responses to the necessity of questions (Ne), and the formula of CVR= (Ne-N/2)/ (N/2) was used. To determine the cut-off point for CVR, Lawshe’s table was used.13
A Content Validity Index (CVI) determined the extent to which each questionnaire item reflected the standard(s)10 and it was used for modification or deletion of the instrument items.14 The CVI is an alpha coefficient, ranging from 0 to 1, which quantifies the extent of agreement among the content experts’ ratings. CVI was used based on Waltz and Bausell’s content validity index.10
CVI for each item was obtained by dividing the number of professionals who ranked the items as compatible or full compatible for each criterion (relevancy, clarity, and simplicity) to the total number of professionals. The average value of three criteria was used as the total CVI for each item. Minimal required amount of CVI for each item was 0.79.15 According to Lawshe, for 20 professionals, minimum required CVR for each item was 0.42.16
Having inflated values due to the chance agreement, content validity index may not consider this as it should be, and therefore, both content validity index and multi-assessor kappa statistic are proposed in content validity studies.17 To put it more clearly, Kappa statistic is an important supplement to CVI because Kappa provides information about the degree of agreement beyond chance. 17
To calculate the modified Kappa statistics, we first calculated the probability of chance agreement for each item of the questionnaire by the following formula:
Pc=[N!/A!(N-A)!]×0.5N
where N is defined as the number of experts and A is the number of assessors who agreed that the item was relevant, clear or simple. After calculating CVI for each questionnaire items, Kappa was computed by entering the numerical values of probability of chance agreement (Pc) and content validity index of each item (I-CVI) in the following formula: K=(I-CVI-Pc)/(1-Pc). Each item is considered as “excellent” if I-CVI is equal or higher than 0.78 after calculating adjusted Kappa which shows higher levels of validity.18
Evaluation criteria of Altman for Kappa are poor agreement for less than 0.20, fair agreement for 0.20 to 0.40, moderate agreement for 0.40 to 0.60, good agreement for 0.60 to 0.80 and very good agreement for 0.80 to 1.00.18
For phases four and five, after receiving legal and ethical approval of the authorities of Iran University of Medical Sciences, the participants were selected from those who referred to health centers in 30 days after recruitment from hospital for after-care services of delivery and QRMCQI completed by an interview. Health centers were located in five cities of Robat-Karim, Baharestan, Malard, Ghods and Shahriyar. The multi-stage sampling method was considered in the cities as the studied units. The sample size was determined and divided into each city according to the share of total clientele for after-care services of delivery. After determining the needed samples of each city, health centers in the north, south, east and west of the city were considered and the sample size divided equally. Then in each geographical location, two or three health centers were selected in a simple random sample selection between the number of health centers, and the eligible clients, in proportion to the number of clients referring to the center, and were continuously interviewed to complete the sample size.
The inclusion criteria of the study were as follows:
1. No experience of anguished feeling, critical situation, severe stress or high anxiety that affected the subject mentally in about last eight weeks.
2. The neonates not being admitted in the hospital.
3. Having the mental and physical health and lack of involvement in drug therapy.
4. Mothers without cesarean history.
The exclusion criteria of the study were:
1. Withdrawal from the study at any time
2. Lack of clear response to questions
3. Women who have answered less than 70 percent of the questions in the questionnaire (Should answer more than 42 questions out of 59).19
Phase Four: Confirmatory Factor Analysis
Confirmatory factor analysis (CFA) is a method used to verify the structure and relations of a set of considered and observed variables. In other words, CFA allows the researcher to check the existence of the underlying structure and verify our understanding of the nature of considered structure of different variables in a hypothesized model. The model is based on theory and previous research results and considerations. In a research, we used theoretical and empirical information and constructed a pattern with reasonable relations and then tested the model statistically.20
In phase four, a CFA was performed by LISEREL software version 8.8 and each of the items was specified to load on its respective subscale as originally hypothesized in three factors: labor, delivery and postpartum and 59 items as one-process analysis. Here, the data from a total of 453 participants in the interview were used in the CFA analysis and we used Kaiser-Meyer-Olkin (KMO) index to check the suitability of the sample size for factor analysis.
Phase Five: Reliability Assurance
Phase five included reliability assurance of the questionnaire. Reliability of an instrument is the degree of consistency with which it measures the attribute it tried to measure.21 The internal consistency of each factor and the whole questionnaire was assessed using Cronbach’s alpha as intercorrelation coefficient. Internal consistency is based on the average correlation among the items within a test and assesses homogeneity or the extent to which all items measure the same construct. A Cronbach’s alpha coefficient of at least 0.70 is considered acceptable, while 0.80 or greater is desirable.7
Ethical Consideration
The local ethics committee of Iran University of Medical Sciences requested the survey to have ethics committee approval and it was accomplished. The code of research ethics is IR.IUMS.FMD.REC 1396.9211373213 which was received on August 28, 2017. Approval for the use of human subjects was obtained from appropriate ethics review boards prior to any data collection in all phases of the study. Participants were informed by describing the risks and benefits, participant responsibilities, confidentiality, and anonymity; the informed consent form of the research was signed by the mothers and the questionnaire completed by an interview. Confidentiality was assured by the use of study identification numbers rather than the addition of any private information on the documents. Data were handled anonymously and the participants’ confidentiality was maintained throughout the study.
RESULTS
In phase one, the questionnaire was developed based on seven WHO categories in RMC and classified in Table 1. In phase two which was face validity evaluation, one question was added to the labor and one to delivery section; totally, there were 41 questions in labor, 10 in delivery and 8 in post-partum which made a 59-item questionnaire; also some comments were made to make clearer items for the interviewee and those items were revised successfully. Totally, eight questions were modified to be clearer for the participants based on expert group comments. Quantitative face validity showed that all the questions’ impact scores were equal or more than 1.5.
In phase three, the questionnaire was reviewed by 20 experts and all of the comments were considered in the questionnaire for qualitative content validity. Quantitative content validity was also assessed by those experts and CVI and CVR were calculated. The CVI (relevancy, clarity, simplicity) and CVR were calculated for each item based on the ratings 1 to 4 from very relevant, clear and simple to none of them for CVI and from 1 to 3 from essential to not necessary for CVR that were marked by a group of experts. Minimum and maximum CVR were 0.60 and 1, respectively and for all items regarding “necessary”, so CVR was higher than the acceptance level (0.42). Total CVR for the whole questionnaire (average of CVRs of all items) was 0.74. Minimum and maximum CVI (average of CVIs for relevancy, clarity and simplicity criteria) were 0.80 and 1, respectively. All the items were satisfactory in terms of CVI (higher than 0.79) and no item was removed. Total CVI (average of CVIs of all items) was 0.94. Table 2 shows CVI and CVR with an average for each item of the developed questionnaire QRMCQI, and here the calculation of all items was in the range and no question was revised or omitted.
Table 2.
Calculation of CVR for items of QRMCQI after expert judgment
| Section | Item | CVRa | CVIb |
|---|---|---|---|
| Labor: CVR=0.71 and CVI=0.93 | q1 | 0.80 | 0.95 |
| q2 | 0.60 | 0.95 | |
| q3 | 0.90 | 0.98 | |
| q4 | 0.60 | 0.97 | |
| q5 | 0.80 | 0.85 | |
| q6 | 0.70 | 0.85 | |
| q7 | 0.60 | 0.80 | |
| q8 | 0.60 | 0.80 | |
| q9 | 0.70 | 0.95 | |
| q10 | 0.60 | 0.95 | |
| q11 | 0.60 | 0.95 | |
| q12 | 0.80 | 0.95 | |
| q13 | 0.60 | 0.92 | |
| q14 | 0.70 | 1.00 | |
| q15 | 0.60 | 0.90 | |
| q16 | 0.90 | 1.00 | |
| q17 | 0.60 | 0.87 | |
| q18 | 0.60 | 0.92 | |
| q19 | 1.00 | 1.00 | |
| q20 | 0.60 | 0.93 | |
| q21 | 0.80 | 0.87 | |
| q22 | 0.70 | 0.93 | |
| q23 | 0.90 | 1.00 | |
| q24 | 0.60 | 0.93 | |
| q25 | 0.70 | 0.95 | |
| q26 | 0.60 | 0.87 | |
| q27 | 0.60 | 0.87 | |
| q28 | 0.90 | 0.85 | |
| q29 | 0.60 | 0.90 | |
| q30 | 0.60 | 0.90 | |
| q31 | 0.60 | 0.88 | |
| q32 | 0.90 | 0.98 | |
| q33 | 0.90 | 0.97 | |
| q34 | 0.60 | 0.92 | |
| q35 | 0.60 | 0.97 | |
| q36 | 0.80 | 0.98 | |
| q37 | 0.90 | 1.00 | |
| q38 | 0.90 | 0.98 | |
| q39 | 0.60 | 0.95 | |
| q40 | 0.70 | 0.95 | |
| q41 | 0.80 | 1.00 | |
| Delivery: CVR=0.73 and CVI=0.93 | q42 | 1.00 | 0.97 |
| q43 | 0.70 | 0.88 | |
| q44 | 0.70 | 0.87 | |
| q45 | 0.90 | 1.00 | |
| q46 | 0.70 | 0.93 | |
| q47 | 0.70 | 0.95 | |
| q48 | 0.80 | 0.98 | |
| q49 | 0.60 | 0.92 | |
| q50 | 0.60 | 0.92 | |
| q51 | 0.60 | 0.97 | |
| Post-partum: CVR=0.88 and CVI=0.97 | q52 | 0.80 | 1.00 |
| q53 | 1.00 | 1.00 | |
| q54 | 0.60 | 0.93 | |
| q55 | 1.00 | 0.98 | |
| q56 | 1.00 | 1.00 | |
| q57 | 0.90 | 0.95 | |
| q58 | 0.90 | 1.00 | |
| q59 | 0.80 | 0.95 |
Content Validity Ratio=(Ne-N/2)/(N/2) with 20 experts (N=20)
Content Validity Index; NOTE: The items with the CVR higher than 0.42 remained at the instrument.
Calculation of Kappa index showed a very good result (from 0.8 to 1 for all the questions, which is in a higher range). Table 3 demonstrates the above calculations for each item in QRMCQI.
Table 3.
Content Validity Index and Modified Kappa of CVI
| Section | Item | CVIa | |||
|---|---|---|---|---|---|
| Relevancy | Interpretation | ||||
| Number giving rating 1 or 2 | Item Relevancy | Kappa | |||
| Labor | q1 | 18 | 0.9 | 0.90 | Excellent |
| q2 | 19 | 0.95 | 0.95 | Excellent | |
| q3 | 20 | 1 | 1.00 | Excellent | |
| q4 | 20 | 1 | 1.00 | Excellent | |
| q5 | 18 | 0.9 | 0.90 | Excellent | |
| q6 | 18 | 0.9 | 0.90 | Excellent | |
| q7 | 16 | 0.8 | 0.80 | Excellent | |
| q8 | 16 | 0.8 | 0.80 | Excellent | |
| q9 | 20 | 1 | 1.00 | Excellent | |
| q10 | 20 | 1 | 1.00 | Excellent | |
| q11 | 20 | 1 | 1.00 | Excellent | |
| q12 | 19 | 0.95 | 0.95 | Excellent | |
| q13 | 17 | 0.85 | 0.85 | Excellent | |
| q14 | 20 | 1 | 1.00 | Excellent | |
| q15 | 19 | 0.95 | 0.95 | Excellent | |
| q16 | 20 | 1 | 1.00 | Excellent | |
| q17 | 16 | 0.8 | 0.80 | Excellent | |
| q18 | 20 | 1 | 1.00 | Excellent | |
| q19 | 20 | 1 | 1.00 | Excellent | |
| q20 | 19 | 0.95 | 0.95 | Excellent | |
| q21 | 19 | 0.95 | 0.95 | Excellent | |
| q22 | 20 | 1 | 1.00 | Excellent | |
| q23 | 20 | 1 | 1.00 | Excellent | |
| q24 | 18 | 0.9 | 0.90 | Excellent | |
| q25 | 20 | 1 | 1.00 | Excellent | |
| q26 | 18 | 0.9 | 0.90 | Excellent | |
| q27 | 18 | 0.9 | 0.90 | Excellent | |
| q28 | 17 | 0.85 | 0.85 | Excellent | |
| q29 | 17 | 0.85 | 0.85 | Excellent | |
| q30 | 17 | 0.85 | 0.85 | Excellent | |
| q31 | 18 | 0.9 | 0.90 | Excellent | |
| q32 | 20 | 1 | 1.00 | Excellent | |
| q33 | 20 | 1 | 1.00 | Excellent | |
| q34 | 19 | 0.95 | 0.95 | Excellent | |
| q35 | 19 | 0.95 | 0.95 | Excellent | |
| q36 | 19 | 0.95 | 0.95 | Excellent | |
| q37 | 20 | 1 | 1.00 | Excellent | |
| q38 | 20 | 1 | 1.00 | Excellent | |
| q39 | 19 | 0.95 | 0.95 | Excellent | |
| q40 | 18 | 0.9 | 0.90 | Excellent | |
| q41 | 20 | 1 | 1.00 | Excellent | |
| Delivery | q42 | 20 | 1 | 1.00 | Excellent |
| q43 | 19 | 0.95 | 0.95 | Excellent | |
| q44 | 18 | 0.9 | 0.90 | Excellent | |
| q45 | 20 | 1 | 1.00 | Excellent | |
| q46 | 20 | 1 | 1.00 | Excellent | |
| q47 | 18 | 0.9 | 0.90 | Excellent | |
| q48 | 20 | 1 | 1.00 | Excellent | |
| q49 | 18 | 0.9 | 0.90 | Excellent | |
| q50 | 17 | 0.85 | 0.85 | Excellent | |
| q51 | 18 | 0.9 | 0.90 | Excellent | |
| Post-Partum | q52 | 20 | 1 | 1.00 | Excellent |
| q53 | 20 | 1 | 1.00 | Excellent | |
| q54 | 17 | 0.85 | 0.85 | Excellent | |
| q55 | 20 | 1 | 1.00 | Excellent | |
| q56 | 20 | 1 | 1.00 | Excellent | |
| q57 | 19 | 0.95 | 0.95 | Excellent | |
| q58 | 20 | 1 | 1.00 | Excellent | |
| q59 | 19 | 0.95 | 0.95 | Excellent | |
Content Validity Index
Confirmatory Factor Analysis
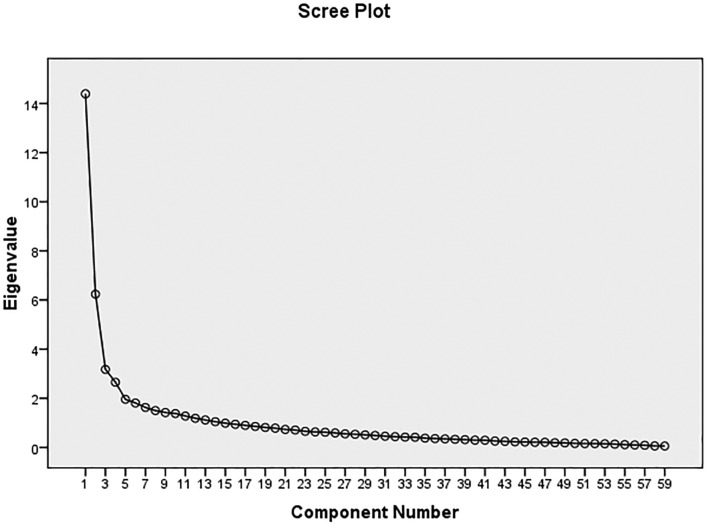
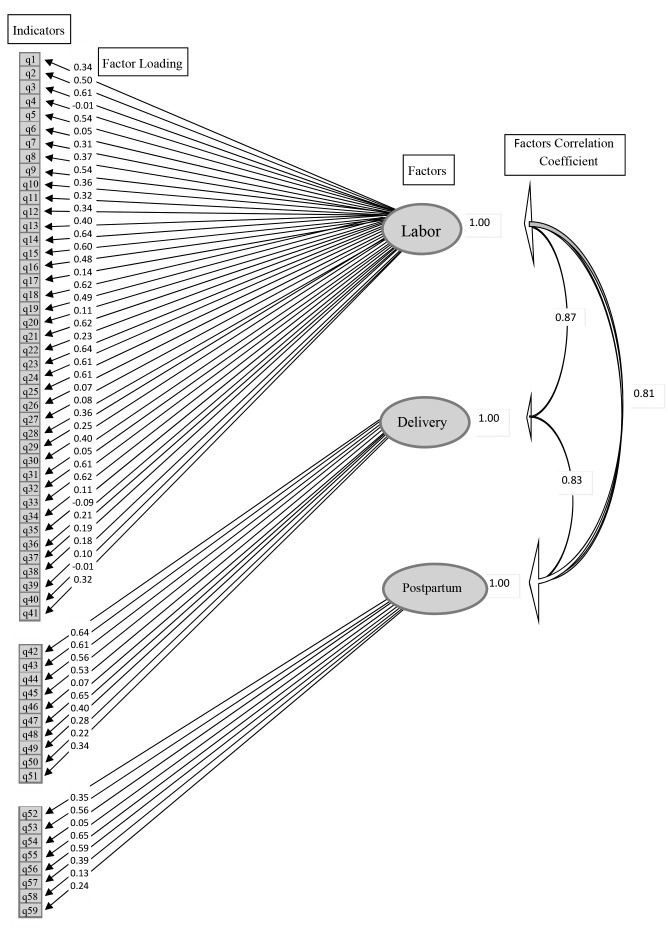
The results of CFA analysis of QRMCQI in phase four are summarized in Table 4 (Figure 1). The KMO index measure of sampling adequacy should be more than 0.5 and here it is 0.871 which is meritorious.22,23 For this model, fit was assessed using a comparative fit index (CFI), a normed-fit index (NFI), root mean square error of approximation (RMSEA), the 90% confidence interval (CI) of RMSEA.20,24,25 Ratios of <3 between minimum fit function Chi-Square (χ2) and degrees of freedom (df), CFI and NFI values equal or more than 0.90, and RMSEA values about 0.08 were considered to be indicative of a good fit and no changes were made to the questionnaire items; it can be used as a tool to evaluate respectful maternity care in Iran.26 Model of CFA analysis for QRMCQI is displayed in Figure 2. The total percentage of variance explained by three factors of labor, delivery and postpartum was 65.8.
Table 4.
Results of confirmatory factor analysis of the QRMCQI questionnaire
| Model | χ2a | dfb | χ2/df | CFIc | NFId | NNFIe | IFIf | RMSEAg | 90% CIh of RMSEA |
|---|---|---|---|---|---|---|---|---|---|
| Schumacker and Lomax26 | 3537.08 | 1649 | 2.15 | 0.91 | 0.86 | 0.91 | 0.92 | 0.087 | 0.083-0.088 |
Minimum fit function Chi-Square
Degrees of freedom
Comparative fit index
Normed-fit index
Non-normed fit index
Incremental fit index
Root mean square error of approximation
Confidence interval
Figure1.
Scree Plot
Figure2.
Model of CFA analysis for QRMCQI
In phase five, the sample for evaluating reliability assurance of the questionnaire consisted of interviews with 30 women who had referred to health centers of Iran University of Medical Sciences 30 days after recruitment from hospital for after-care services of delivery in five cities of Robat-Karim, Baharestan, Malard, Ghods and Shahriyar. The internal consistency of each factor and the whole questionnaire were assessed, using Cronbach’s alpha. Testing showed acceptable internal consistency reliability by calculating Cronbach’s alpha coefficient for questions about labor care (0.863), delivery care (0.848) and postpartum care (0.789); the overall scale for all of questions was equal to 0.93 (Table 5).
Table 5.
Results of reliability analysis of the QRMCQI questionnaire
| Section | Item Statistics for Reliability Analysis | |||
|---|---|---|---|---|
| Item | Questions | Mean±SD | αa | |
| Labor | q1 | Did the service providers introduce themselves to you? | 2.3±1.51 | 0.86 |
| q2 | Did the staff address you with your name? | 2.43±1.36 | ||
| q3 | Was the staff attitude with you politely? | 3.03±0.89 | ||
| q4 | Did you have the right to choose? | 0.8±1.24 | ||
| q5 | Did the staff request you to ask your questions? | 2.63±1.43 | ||
| q6 | Did the staff request your companion to ask your questions? | 1.33±1.42 | ||
| q7 | Did the staff disagree with your beliefs? | 3.07±1.39 | ||
| q8 | Did the staff disagree with your companion’s beliefs? | 3.1±1.35 | ||
| q9 | Did the staff speak to you in a language you easily understand? | 2.73±1.36 | ||
| q10 | Any insults or threats happened against you? | 3.4±1.1 | ||
| q11 | Any insults or threats happened against your companion? | 3.33±1.21 | ||
| q12 | Did you forced to do what you did not want? | 3.27±1.28 | ||
| q13 | Did your companion forced to do what he/she did not want? | 3.1±1.3 | ||
| q14 | Were your questions answered politely? | 3.03±1 | ||
| q15 | Have your questions answered honestly? | 2.9±1.18 | ||
| q16 | Did the staff screamed over you? | 2.77±1.41 | ||
| q17 | Were you allowed to take the hands of the staff or touch them? | 1.1±1.56 | ||
| q18 | Did the care provider and staff consider your comfort? | 2.6±1.16 | ||
| q19 | Was your privacy maintained during the medical examinations using the curtain? | 3.23±0.9 | ||
| q20 | Have you been told that your recorded information will be kept safe and secure (so that no one can access it)? | 0.77±1.19 | ||
| q21 | Have you explained what to do? | 2.57±1.43 | ||
| q22 | Did the staff explain what might have happened to you in the labor process? | 1.9±1.4 | ||
| q23 | Did the staff explain to you before any action and practice? | 2.4±1.52 | ||
| q24 | Did the staff ask for your permission before any action and practice? | 2.33±1.54 | ||
| q25 | Did the staff have regular monitoring of your delivery progress? | 3.03±1.1 | ||
| q26 | Did they limit your drinking? | 1.73±1.53 | ||
| q27 | Did they limit your eating? | 1.7±1.56 | ||
| q28 | Did they injure you physically? | 3.57±1.04 | ||
| q29 | Have you forced to stay in your bed? | 2.3±1.58 | ||
| q30 | Were you allowed to move? | 2.4±1.48 | ||
| q31 | Were you allowed to choose your desired status on the bed or outside it? | 1.73±1.53 | ||
| q32 | If the discomfort was felt, would the care providers fix it? | 2.13±1.8 | ||
| q33 | If the pain was expressed, would the care providers resolve it? | 2.17±1.8 | ||
| q34 | Did the staff use non-pharmacological pain relief methods (massage, heat therapy, hot water compression / ice compress / aroma therapy / pressure on the waist region) for you? | 0.17±0.38 | ||
| q35 | Did the care provider use pain reliever (oxytocin) in your serum? | 1.77±1.48 | ||
| q36 | Were you allowed to choose the type of delivery? | 0.63±1.38 | ||
| q37 | Did the staff describe the benefits of your chosen delivery type? | 0.83±1.42 | ||
| q38 | Did the staff describe the disadvantages of your chosen delivery type? | 0.53±1.22 | ||
| q39 | Did the staff suggest you the physiological delivery (without intervention)? | 0.1±0.31 | ||
| q40 | Did the staff offer you a cesarean? | 3.93±0.25 | ||
| q41 | Were you discriminated because of ethnicity, race, economic situation and etc. from rest of admitted women? | 3.43±1.1 | ||
| DELIVERY | q42 | Did the staff describe to you about what you need to do? | 2.6±1.3 | 0.84 |
| q43 | Did the staff explain to you about possible events that may have occurred in the process of delivery? | 2.2±1.47 | ||
| q44 | Have you been allowed to choose your desired condition in the bed during childbirth? | 2.27±1.48 | ||
| q45 | Did the staff manage your privacy using a curtain or parlor during the delivery, whether in the public room or in private? | 3±1.2 | ||
| q46 | Have you been informed that you have permission to attend a trained female companion during childbirth? | 0.17±0.53 | ||
| q47 | Did the staff ask for your permission before any action and practice? | 2.5±1.46 | ||
| q48 | Was the skin of the baby contacted with your skin Immediately after birth? | 2.67±1.49 | ||
| q49 | Was your tendency considered in case of skin contact with your baby Immediately after birth? | 2.47±1.46 | ||
| q50 | Was the skin contact with your baby last for the first hour of the birth? | 2.7±1.37 | ||
| q51 | Did you breastfeed your baby during the first hour? | 2.77±1.33 | ||
| Post-Partum | q52 | Were you admitted to your baby during the whole day in a room? | 3.43±0.97 | 0.78 |
| q53 | Did the staff provide you necessary explanations for breastfeeding your baby? | 3.23±1.1 | ||
| q54 | Did the staff force you to breastfeed your baby? | 3.67±0.66 | ||
| q55 | Did the staff tell you to call them if you need help? | 3.1±0.96 | ||
| q56 | Were the staff quickly responding to your need in case of any help and information? | 3.23±0.97 | ||
| q57 | Have you ever been completely abandoned and keep alone? | 2.77±1.22 | ||
| q58 | Did you have permission to attend a companion with yourself? | 2.67±1.71 | ||
| q59 | Have you been hospitalized too much due to the delay or non-payment of the related costs? | 3.83±0.38 | ||
Cronbach’s alpha coefficient (overall is 0.93)
DISCUSSION
We have developed a new instrument for considering respectful maternity care in Iran through a rigorous process of item generation and validity-reliability assessment. Other related studies in Iran have developed and assessed instruments to evaluate satisfaction in maternity care services among mothers.
International research and case studies that developed survey instruments and questionnaires about D&A and respectful maternity care mainly contained seven WHO categories of D&A and some others evaluated all the processes of labor to delivery. No similar sections were observed in other surveys as we did in this research for components of labor, delivery and postpartum.
In addition, most of articles reviewed implemented questionnaires based on categories of disrespect and abuse criteria (Table 1) for mothers and care providers’ behavior and the results were described based on each item of D&A. Some other articles developed question items after primary interviews by health care providers, experts and considering other surveys based on the scale of mothers’ satisfaction, dignity, autonomy and communication during care. In the current study, categories of disrespect and abuse and WHO guidelines in maternity care quality helped us to prepare and generate questions in the first phase beside other materials and experiences and then decided to categorize the items in three sections of labor, delivery and postpartum for having better idea of RMC condition in each section. In other words, some items of disrespect and abuse in all aspects of care belong to labor, whereas other care considerations are in delivery and there are items that have the ability to scale the level of respectful maternity care postpartum.
An online questionnaire studied the maternity care experiences among 501 Hungarian women aged 18-45 with children under the age of 5 and having experiences of natural delivery and cesarean. The effect of the method of payments on the quality of service and care was considered. The instrument contained 111 qualitative questions in different kinds of screening, prenatal care, birth care, postpartum care, care preferences, informal payments, mothers’ autonomy scale items, and open-ended questions. Eleven experts rated the items as clear and relevant to the research subject and calculated an average content validity index of 0.97 for the questions. For testing reliability, the study used a randomly selected sample for test-retest and just reported that the instrument performed well. The online questionnaire was developed based on two other surveys and adapted to use in Hungarian context. We used detailed literature review for RMC in most of the countries’ researches and developed the items according to experience, WHO related publications and Iran maternity care system. Hungarian adapted questionnaire considered the method of payment as an important scale parameter for receiving specified level of maternity care and used nine questions about informal payment that are too much and may have negative influence on the mothers’ ideas about all the processes even if they receive high quality care; it would be better to have a little contribution in the items as we, in the current study, just have one item in the postpartum section. An effort to assess the quality of maternity care far from considering payment methods, especially informal payments, helps us to have more related results as to the quality of care in mothers’ impressions and then let the experts to judge about the cause. In the current study, the result showed the mean CVI equal to 0.94 that is lower than Hungarian questionnaire and it can be attributed to different cultural views, parameter importance and number of experts in the panel.27
Another study measured the person-centered maternity care and level of satisfaction in a rural and urban Kenyan population. Their 30 descriptive item questionnaire was designed in three sub-scales to measure dignified and respectful care, communication and autonomy, and supportive care. The sample consisted of women who delivered in the 9 weeks preceding the survey (857 women for rural and 530 number for urban districts). Results showed the reliability using Cronbach’s alpha of 0.88 for the rural sample, 0.83 for the urban sample, and 0.86 for the combined sample; also, a high content validity was mentioned based on the extensive literature and expert reviews.28 After a literature review on quality of care for maternal health, the authors identified ten domains in maternity care in Kenya and items addressed one or more of the domains with 5-point response scale, while in the current study after we considered WHO categories of disrespect and abuse, each item addressed only one category and it was clearer for planning in the specific category of respect to improve in the health system both combined in rural and urban areas. Here, we calculated overall scale of Cronbach’s alpha equal to 0.93 for labor, delivery and postpartum sections that shows more correlation and internal consistency between the items. Content validity was also calculated considering CVI-CVR and Kappa index in our study and no numerical result of content validity was found in the assessment of the tool that developed in Kenya. We assessed content validity and calculated a highly acceptable index that shows it was suitable for use as a quantitative measurement tool for evaluating RMC.
A 15-item scale tool was developed to measure the women’s perception of respectful maternity care in public health facilities in Ethiopia. A questionnaire with 37 items and two additional measures of global satisfaction items on a five-point Likert scale were prepared inductively, via in depth interviews with 8 postpartum women; it was pilot tested with 40 women, subjected to expert review and tested for reliability and validity by interviewing 509 women within 7 days of being discharged from hospitals and health centers in Addis Ababa, Ethiopia. Reliability of the tool was evaluated using Cronbach’s alpha coefficient (0.85), which was lower than that of the current study (0.93). The 15-item scale tool used four components labeled as friendly care, abuse-free care, discrimination-free care, and timely care that accounted for 67.8% of the final 15-item scale. Content validity of the RMC scale was assured through review of the related literature, in-depth interviews with postpartum women, and expert review.29 Ethiopian RMC scale focuses primarily on women’s experiences of provider behavior during labor and birth, not on their ability to exercise autonomy without discrimination as they sought to participate as decision leaders over the course of maternity care. Ethiopian tool also considered seven categories of disrespect and abuse the same as what we did but no in depth interviews were performed with women in our study and we just considered the literature review and experience to develop the items; from this point of view, it would be better to design the tool from top levels of expert ideas to consider all aspects. The 15-item scale focused on the overall experience of care by health providers in a low resource institutional center and the item types could not be applicable to other countries for measuring RMC as the included items that described the situations rarely reported in high resource countries. Again, no obvious numerical results were provided in 15-item scale tool for content validity evaluation. We developed a tool that evaluates RMC in sections of labor, delivery and postpartum and can provide us with an acceptable view toward the quality of care for mothers in different sections. Based on the above points, planning and decision making for improvement of health care system and maternal care would be much oriented to the goal.
We used the QRMCQI to interview with the women in 30 days after release from hospital about RMC seven categories in labor, delivery and postpartum sections; the 59-item version of the QRMCQI demonstrated face and content validity and area reliability as well as internal consistency. The results showed good matching of the questions generated in three sections of labor, delivery and postpartum from the aspect of relevancy and clarity to the subject. Validity and reliability of the tool and confirmatory factor analysis showed appropriate selection and allocation of questions in the three sections.
CONCLUSION
The new tool, “QRMCQI”, obtained acceptable criteria as to reliability, validity and confirmatory factor analysis according to the findings of this study and will help to evaluate respectful maternity care in the health care system. It can provide us with a good tool to evaluate the RMC quality in labor, delivery and post partum in order to plan for a better oriented maternal health care system.
It would be useful to develop another questionnaire with specific categorized items in seven sections of disrespect and abuse published by WHO and White Ribbon Alliance in maternity care for the future studies on RMC in Iran; here, we just aimed to develop the questions for three sections of labor, delivery and postpartum. We also recommend that the current questionnaire be developed while considering different factors, sub-scales and items classifications such as dignity and respect, communication and autonomy, and supportive care with items evaluating the effect of governmental or private centers’ attitude toward RMC.
ACKNOWLEDGEMENT
This study was the first phase of an M.Sc. thesis at Iran University of Medical Sciences which was funded by the School of Nursing and Midwifery, Iran University of Medical Sciences. The authors gratefully acknowledge it (thesis code No. 9211373213). The research team would like to thank the participants and organizations that generously shared their time, experience, and materials for the purposes of this project. We also thank people in five area networks of health centers in Robat-Karim, Baharestan, Malard, Ghods and Shahriyar.
Conflict of Interest:None declared.
REFRENCES
- 1.Bowser D, Hill K. Exploring Evidence for Disrespect and Abuse in Facility-Based Childbirth, Report of a Landscape Analysis. Harvard School of Public Health, University Research Co: United States Agency for International Development; 2010. [Google Scholar]
- 2.Selin H, Stone PK. Childbirth across cultures ideas and practices of pregnancy, childbirth and the postpartum. New York: Springer; 2009. [Google Scholar]
- 3.United States, Agency for, International Development. Respectful Maternity Care Toolkit. USA: United States Agency for International Development; 2016. [Google Scholar]
- 4.World Health Organization. The prevention and elimination of disrespect and abuse during facility-based childbirth. Geneva: World Health Organization; 2015. [Google Scholar]
- 5.Bohren MA, Vogel JP, Hunter EC, et al. The Mistreatment of Women during Childbirth in Health Facilities Globally: A Mixed-Methods Systematic Review. PLoS Medicine. 2015;12:e1001847. doi: 10.1371/journal.pmed.1001847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Reis V, Deller B, Carr C, Smith J. Respectful Maternity Care: Country Experiences, Survey Report. Washington DC: United States Agency for International Development; 2012. [Google Scholar]
- 7.Streiner DL, Norman GR, Cairney J. Health measurement scales: a practical guide to their development and use. 5th ed. United Kingdom : Oxford University Press; 2014. [Google Scholar]
- 8.Gronvik CKU, Odegard A, Bjorkly S. Factor Analytical Examination of the Evidence-Based Practice Beliefs Scale: Indications of a Two-Factor Structure. Open Journal of Nursing. 2016;6:699–711. [Google Scholar]
- 9.DeVon HA, Block ME, Moyle-Wright P. A psychometric toolbox for testing validity and reliability. J Nurs Scholarsh. 2007;39:155–64. doi: 10.1111/j.1547-5069.2007.00161.x. [DOI] [PubMed] [Google Scholar]
- 10.Waltz CF, Strickland OL, Lenz ER. Measurement in nursing and health research. 5th ed. New York: Springer Publishing Company; 2017. [Google Scholar]
- 11.Newman I, Lim J, Pineda F. Content Validity Using a Mixed Methods Approach: Its Application and Development Through the Use of a Table of Specifications Methodology. Journal of Mixed Methods Research. 2013;7:243–60. [Google Scholar]
- 12.Polit DF, Beck CT. The content validity index: are you sure you know what’s being reported? Critique and recommendations. Res Nurs Health. 2006;29:489–97. doi: 10.1002/nur.20147. [DOI] [PubMed] [Google Scholar]
- 13.Lawshe CH. A Quantitative Approach to Content Validity. Personal Psychology. 1975;28:563–75. [Google Scholar]
- 14.Polit DF, Beck CT, Owen SV. Is the CVI an acceptable indicator of content validity? Appraisal and recommendations. Res Nurs Health. 2007;30:459–67. doi: 10.1002/nur.20199. [DOI] [PubMed] [Google Scholar]
- 15.Kellar SP, Kelvin EA. Munro’s statistical Methods for Health Care Research. 6th ed. Philadelphia: Lippincott Williams & Wilkins; 2012. [Google Scholar]
- 16.Msyamboza KP, Ngwira B, Dzowela T, et al. The burden of selected chronic non-communicable diseases and their risk factors in Malawi: nationwide STEPS survey. PLoS One. 2011;6:e20316. doi: 10.1371/journal.pone.0020316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Almanasreh E, Moles R, Chen TF. Evaluation of methods used for estimating content validity. Res Social Adm Pharm. 2017 doi: 10.1016/j.sapharm.2018.03.066. [In Press] [DOI] [PubMed] [Google Scholar]
- 18.Altman DG. Practical Statistics for Medical Research. 2nd ed. London: Chapman and Hall; 2015. [Google Scholar]
- 19.Fincham JE. Response Rates and Responsiveness for Surveys, Standards, and the Journal. American Journal of Pharmaceutical Education. 2008;72:43. doi: 10.5688/aj720243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Harrington D. Confirmatory Factor Analysis. United Kingdom: Oxford University Press; 2008. [Google Scholar]
- 21.Polit DF, Beck CT. Nursing Research: Generating and Assessing Evidence for Nursing Practice. 9th ed. Philadelphia: Lippincott Williams & Wilkins; 2011. [Google Scholar]
- 22.Smith H, Perez M, Sladek MR, et al. Development and validation of makeup and sexualized clothing questionnaires. J Eat Disord. 2017;5:39. doi: 10.1186/s40337-017-0171-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Moraes JT, Amaral CFS, Borges EL, et al. Validation of an instrument for evaluating health care services to ostomized people. Rev Lat Am Enfermagem. 2016;24:e2825. doi: 10.1590/1518-8345.0748.2825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hoofs H, van de Schoot R, Jansen NWH, Kant I. Evaluating Model Fit in Bayesian Confirmatory Factor Analysis With Large Samples: Simulation Study Introducing the BRMSEA. Educational and Psychological Measurement. 2018;78:537–68. doi: 10.1177/0013164417709314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sun J. Assessing Goodness of Fit in Confirmatory Factor Analysis. Measurement and Evaluation in Counseling and Development. 2005;37:240–56. [Google Scholar]
- 26.Schumacker RE, Lomax RG. A Beginner’s Guide to Structural Equation Modeling. 3rd ed. London: Routledge; 2010. [Google Scholar]
- 27.Rubashkin N, Szebik I, Baji P, et al. Assessing quality of maternity care in Hungary: expert validation and testing of the mother-centered prenatal care (MCPC) survey instrument. Reproductive Health. 2017;14:152. doi: 10.1186/s12978-017-0413-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Afulani PA, Diamond-Smith N, Golub G, Sudhinaraset M. Development of a tool to measure person-centered maternity care in developing settings: validation in a rural and urban Kenyan population. Reproductive Health. 2017;14:118. doi: 10.1186/s12978-017-0381-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sheferaw ED, Mengesha TZ, Wase SB. Development of a tool to measure women’s perception of respectful maternity care in public health facilities. BMC Pregnancy and Childbirth. 2016;16:67. doi: 10.1186/s12884-016-0848-5. [DOI] [PMC free article] [PubMed] [Google Scholar]