Abstract
HELLP syndrome is a combination of symptoms described as hemolysis, elevated liver enzymes and low platelets. HELLP is a common life-threatening complication of pregnancy thought to be a variant or complication of preeclampsia. In this case report, we aimed to present a woman with acute postpartum HELLP syndrome complicated by pulmonary edema after caesarean section following severe preeclampsia. Our experience suggests that early detection of HELLP syndrome and timely management will bring good outcomes.
Keywords: HELLP syndrome, Acute pulmonary edema, Preeclampsia, IVF, Twin pregnancy
1. Introduction
HELLP syndrome is a combination of symptoms described as hemolysis, elevated liver enzymes and low platelets, and the acronym HELLP refers to hemolysis (H), elevated liver enzymes (EL) and low platelet count (LP). HELLP occurs in 0.5-1% of all pregnancies [1]. About 70% of HELLP cases happen before delivery and the remainder after childbirth, typically within 48 hours. HELLP is a common life-threatening complication of pregnancy thought to be a variant or complication of preeclampsia. HELLP syndrome is associated with severe clinical complications, including pulmonary edema, renal failure, disseminated intravascular coagulation (DIC), and liver infarction and liver haematoma or rupture with haematoma [2]. If untreated, HELLP syndrome can lead to maternal end-organ failure and death. In this case report, we aimed to present a woman with acute postpartum HELLP syndrome complicated by pulmonary edema after caesarean section following severe preeclampsia.
2. Case presentation
A 31-year-old woman, gravida 2, para 0, was referred at 30 weeks and 3 days of gestation to our department because of heavy proteinuria and edema of the ankles and legs. Her blood pressure was in mild range at 158 systolic and 102 mm Hg diastolic. She denied any history of hypertension prior to pregnancy and denied any visual disturbances and palpitations. She reported a history of alpha thalassemia, and a laparoscopic surgery history notable for ectopic pregnancy. The present pregnancy was conceived with IVF-ET and she denied any drug allergies or contributory family history. She denied the use of tobacco or illicit substances. Exams revealed no evidence of neurologic abnormalities, and she was able to converse at her baseline mental status. Her deep tendon reflexes were normal. Fetal cardiac activity was appreciated by ultrasound examination. The laboratory exams were notable for urea 5.8–6.33 mmol /L 1 and albumin 28.1 g/L. The urinalysis revealed a proteinuria 1,352 mg/24h. She received magnesium seizure prophylaxis at 2 g/h, labetalol 100 mg q6h anti-hypertensive treatment and a dexamethasone course was used to accelerate pulmonary maturation because of the concern for preterm labor.
On day two of the admission, she complained of chest congestion, vomiting, diarrhea and right upper quadrant pain. Physical examination revealed severe hypertension (190/110 mmHg), body temperature of 37.1°C, respiratory frequency of 23 breaths per minute and heart rate of 85 beats per minute. Her two lungs were clear to auscultation. Chest radiography suggested pulmonary edema (Figure 1A). Emergency caesarean section was performed because of aggravation. Live born female and male were delivered. After surgery she received nicardipine antihypertensive and magnesium seizure prophylaxis. The postoperative course was initially inconspicuous. Ten hours postpartum she experienced sudden chest pain. The blood pressure rose to 169/118. Laboratory findings showed alanine aminotransferase (ALT) 285 units/L, aspartate aminotransferase (AST) 442 units/L and lactic dehydrogenase (LDH) 960 units/L. X-ray revealed lung texture enlargement (Figure 1B). After three hours, her urine was dark red, blood pressure was in control at 143/105. The laboratory findings were notable for haemolysis, thrombocytopenia, and an increase in serum creatinine and aminotransferases.
Figure 1.
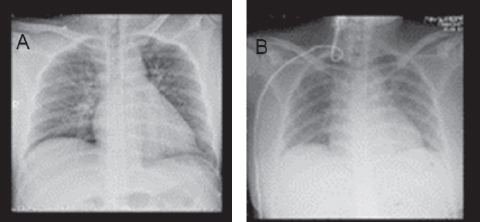
A. Double lungs exudative change. B. Lung texture enlargement.
The combination of haemolysis, thrombocytopenia, and elevated liver enzymes suggested a postpartum HELLP syndrome. She was transferred to the intensive care unit and received treatment with fresh platelets and albumin. On the ninth day of hospitalization, the patient was at a fairly stable condition. Radioactive examination did not show abnormal effusion. The patient was then discharged.
Ethical approval: The research related to human use has been complied with all the relevant national regulations, institutional policies and in accordance the tenets of the Helsinki Declaration, and has been approved by the authors' institutional review board or equivalent committee.
Informed consent: Informed consent has been obtained from patient included in this study.
3. Discussion
HELLP syndrome is a poorly understood pregnancy-related condition with a rapid onset and is typically seen in patients with severe pre-eclampsia, although it can occur in the absence of pre-eclampsia in 10% of the cases. HELLP is a multisystem disease, resulting in generalized vasospasm, microthrombi formation and coagulation defects. The syndrome seems to be the final manifestation of insult that leads to microvascular endothelial damage and intravascular platelet aggregation [3]. After being activated by thrombin, fibrinogen polymerizes into strands of fibrin, which form meshlike barriers in small blood vessels, resulting in red blood cell destruction and microangiopathic hemolytic anemia characteristic of the syndrome. Platelets adhere to the fibrin structures, leading to low platelet counts. Clot formation in the hepatic vasculature leads to decreased hepatic perfusion and subsequent ischemia and, if uncorrected, infarction and liver failure. Liver dysfunction and failure result in the elevated liver enzymes characteristic of HELLP syndrome [4].
HELLP syndrome develops with a peak frequency between the 27th and 37th gestational weeks. About 30% of patients of HELLP syndrome develop the syndrome after parturition, typically within 48 hours. Women with postpartum HELLP syndrome have significantly higher incidences of complications such as pulmonary edema, renal failure, disseminated intravascular coagulation (DIC), and subcapsular liver hematoma, and HELLP syndrome is associated with serious maternal morbidity and maternal complications [2]. Maternal mortality of HELLP is reported to be high [5, 6]. Our patient satisfied all the criteria of HELLP syndrome. She had hemolysis as evidenced by anemia, raised bilirubin and LDH, elevated liver enzymes, and low platelets. Thus, our patient was adequately evaluated, diagnosed and received intensive care management, which led to a favorable outcome. Our case highlights the importance of proper preoperative evaluation of pre-eclampsia patients to the diagnosis of HELLP syndrome.
In conclusion, HELLP syndrome is associated with severe clinical complications, which cause high maternal morbidity and mortality. The early detection of HELLP syndrome and timely management will bring good outcomes.
Footnotes
Disclosure of conflict of interest: None.
References
- [1].Baxter JK, Weinstein L. HELLP syndrome: the state of the art. Obstet Gynecol Surv. 2004;59:838. doi: 10.1097/01.ogx.0000146948.19308.c5. –. [DOI] [PubMed] [Google Scholar]
- [2].Dusse LM, Alpoim PN, Silva JT, Rios DR, Brandão AH, Cabral AC. Revisiting HELLP syndrome. Clin Chim Acta. 2015;451:117. doi: 10.1016/j.cca.2015.10.024. –. [DOI] [PubMed] [Google Scholar]
- [3].Haram K, Svendsen E, Abildgaard U. The HELLP syndrome: clinical issues and management. A review. BMC Pregnancy Childbirth. 2009;9:8. doi: 10.1186/1471-2393-9-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Morikawa M, Kawabata K, Kato-Hirayama E, Oda Y, Ueda H, Kataoka S, Yamada T, Okuyama K, Sengoku K, Minakami H. Liver dysfunction in women with pregnancy-induced antithrombin deficiency. J Obstet Gynaecol Res. 2017;43:257. doi: 10.1111/jog.13210. –. [DOI] [PubMed] [Google Scholar]
- [5].Genest G, Spitzer KA, Laskin CA. Maternal and Fetal Outcomes in a Cohort of Patients Exposed to Tumor Necrosis Factor Inhibitors throughout Pregnancy. J Rheumatol. 2018;45:1109. doi: 10.3899/jrheum.171152. –. [DOI] [PubMed] [Google Scholar]
- [6].Malmström O, Morken NH. HELLP syndrome, risk factors in first and second pregnancy: a population-based cohort study. Acta Obstet Gynecol Scand. 2018;97:709. doi: 10.1111/aogs.13322. –. [DOI] [PubMed] [Google Scholar]


