Abstract
Background
To estimate the prevalence of disability during the last 3 years prior to death among the oldest-old (≥80 years) in China.
Methods
We used data from the Chinese Longitudinal Healthy Longevity Survey (CLHLS), a nationally representative study of the oldest-old in China. The analytic sample included 23,934 decedents who died between 1998 and 2014 and had at least one interview within the last 3 years of life. Disability was defined as being incontinent or needing assistance in performing one or more of five other essential activities (bathing, transferring, dressing, eating, and toileting).
Results
About 57.8% (weighted) of the study decedents were female. The prevalence of disability increased modestly from 36 months to 24 months prior to death (20% to 23%), more rapidly from 24-months to 12-months before death (23% to 31%), and substantially from 12 months before death to the last month of life (31% to 48%). The disability rates were lowest for participants who died between 80 and 89 years, intermediate for those who died between 90 and 99 years, and highest for those who died at age 100 or older, although the patterns over the 3-year period were comparable for the three age groups. At each time point prior to death, a higher percentage of women was disabled than men.
Conclusions
In this large nationally representative sample of the oldest-old in China, the prevalence of disability during the 3 years prior to death is high and is greater in women than men and those who die at the oldest ages.
Keywords: Disability, Death, Oldest-old, End-of-life
The oldest-old (≥80 years) is the fastest-growing segment of the world’s population, including China. The dramatic aging population poses new challenges, particularly for economically booming nations, since their health care systems may not be well prepared for this expanding vulnerable population. One particularly important question is whether and to what extent the oldest-old can maintain independence with essential activities of daily living (ADL). According to the hypothesis of compression of morbidity, the time spent in dependent states (i.e., disability) could be reduced and compressed into a shorter period of time prior to death with improvements in socioeconomic status and health care (1). In contrast, another view (i.e., expansion of morbidity) posits that more frail older adults will survive to extremely old age, but with worsening health and higher rates of disability (2,3). It is difficult to determine which of these two hypotheses is true (4,5). Consequently, a rigorous evaluation of end-of-life disability in different countries is imperative not only for the oldest-old, their families, and caregivers, but also for policy makers.
To date, several studies in developed countries have demonstrated that most older adults face a period of disability in late life, lasting to the end of life (6–9). A large, population-based U.S. study of adults older than 50 years found that more than one-third experienced disability a year before death, whereas more than half experienced disability in the last month of life; and these rates were much higher for those who died at the older ages (6). Based on these results, the authors concluded that the formal and informal care systems in the United States should be redirected toward meeting end-of-life care for the disabled; and warned that even the most well-functioning older adults, together with their families and caregivers, should prepare for a period of disability at the end of life.
However, it is unknown whether these findings apply to low-income or middle-income countries like China, a developing country with a rapidly growing aging population. Therefore, we carried out a study to estimate the prevalence of disability prior to death among the oldest-old in China using unique data from the Chinese Longitudinal Healthy Longevity Survey (CLHLS), one of the largest samples of oldest-old in the world. In addition, we evaluated the distribution of end-of-life disability according to key demographic factors such as age at death and sex.
Methods
Study Participants
The CLHLS is an ongoing nationwide survey of Chinese oldest-old persons, with the major aim of collecting a comparable sample of male and female octogenarians, nonagenarians, and centenarians in a randomly selected half of the counties/cities in 23 provinces throughout China (10,11). The 23 provinces covered about 90% of the total population in China in 2010 census (11). To ensure representativeness, a targeted random-sampling design was employed, through interviews with approximately equal numbers of male and female octogenarians, nonagenarians living near to the centenarians (e.g., the same villages). This design serves well the major aim of investigating determinants of healthy longevity of different age and sex groups who live in the same social and natural environment (4).
The survey began interviewing the oldest-old from 1998; follow-up interviews of the original sample and newly added samples were carried out in 2000, 2002, 2005, 2008, 2011, and 2014. Thus, most decedents had at least one interview within the last 3 years of life, and the timing of this end-of-life interview was based on the time between the last interview and date of death. Extensive questionnaires were used to collect a comprehensive set of information, including demographic characteristics, lifestyle, self-reported health, ADL, economic resources, etc. All information was obtained during in-home interviews that lasted about 2 hours. Each respondent provided written informed consent to indicate his/her willingness to participate in the CLHLS. The informed consent was signed by the next-of-kin in the case when the respondent was not able to write. The details of the sampling design, response rates, attrition, and systematic assessments of data quality across numerous measures were described elsewhere (10). The Research Ethics Committees of Peking University and Duke University granted approval for the Protection of Human Subjects for the CLHLS. This study protocol (IRB Protocol ID: 2000021659) was approved by the Human Investigation Committee at Yale University.
The date of death was collected from official death certificates when available; otherwise, the next-of-kin and local residential committees were consulted. The quality of mortality data in the CLHLS has been shown to be high (10). In this study, we assembled our study participants from the 1998, 2000, 2002, 2005, 2008, and 2011 waves, including 60,759 oldest-old persons with homes-based interview. As shown in Supplementary Figure S1, about 24,668 participants died before the 2014 wave; of these, we excluded 332 with missing data on date of death, 118 with missing data on ADL disability, and 284 who did not complete an interview within the last 3 years of life, leaving a final analytic sample of 23,934 decedents.
Measures
Disability
The Katz index (12) was used to assess disability in six essential ADLs: bathing, transferring, dressing, eating, toileting, and continence. The Chinese version of the scale, which has been extensively tested in pilot interviews, has been shown to yield reliable and valid responses (13,14). Interviewers asked participants if they needed personal assistance in performing five activities (bathing, transferring, dressing, eating, and toileting) or had problems with incontinence (12). ADL disability was defined as being incontinent or needing assistance in performing one or more of the five other activities (12,15,16). Severe ADL disability was defined as having disability in three or more of the six activities (7). We also estimated the prevalence of disability (i.e., unable or need assistance) in two other functional tasks prior to death: walking one kilometer and going shopping by oneself, which were available in the questionnaire from 2002 to 2011.
Sociodemographic Factors
Demographic variables included age at death, sex (men vs women), race/ethnicity (Han vs non-Han), and residence (rural vs urban). Socioeconomic status included education (any formal education), lifetime primary occupation (white collar occupation), economic independence (primary financial source from own work or pension), family in good economic standing (self-rated as rich compared with other families in the community), and being in receipt of adequate medications for any illnesses. Social contact and support measures included current marital status and co-residence with adult children. Health practices were measured by currently consuming alcohol and regular exercise. These sociodemographic factors have been well defined and studied in CLHLS, showing important effects on disability (15) and relevant outcomes such as frailty and mortality (17,18).
Statistical Analyses
To obtain population-based estimates, we incorporated a survey weight variable that was constructed according to the distribution of age, sex, and urban/rural residence in the Chinese population in the corresponding survey year (10). Characteristics of the decedents were calculated as means (±standard deviation [SD]) or percentages. We estimated the monthly prevalence of disability during the last 3 years of life using a restricted cubic spline with varied numbers and locations of knots. Standard cut points for knots suggested by Harrell (19) and other cut points (e.g., equally) were considered. Goodness of fit for the logistic regression models was verified using a modified Hosmer–Lemeshow approach. We selected the optimal model using Akaike information criterion and C statistic. As study participants were assembled from different waves of CLHLS, we also accounted for the effect of calendar/survey time by adding a time term in the model. When this time term and all sociodemographic factors were included in the model, a restricted cubic spline with three knots placed at standard cut points (in our case 30, 16, and 4 months prior to death) was optimal. The C statistic was 0.72, indicating acceptable model discrimination. We used similar methods to estimate the prevalence of severe ADL disability and disability in the two other functional tasks.
To estimate the prevalence of disability during the last 3 years of life for relevant subgroups, we reran our model for each sociodemographic factor separately while adjusting for all other factors in the models. We also calculated results stratified by age at death and sex.
To test the robustness of our estimates, we performed several sensitivity analyses. First, we reran our models by replacing the small proportion of missing data on sociodemographic factors (<2%) using multiple imputation techniques. Second, we estimated the prevalence of disability only among decedents assembled from the 2002 to 2011 waves, which spanned complete 3-year intervals. Third, we compared the characteristics of 284 decedents who did not have a home-based interview within the last 3 years of life with those who did.
All statistical analyses were performed using SAS version 9.4 (SAS Institute, Cary, NC). p <0.05 (two-tailed) was considered to indicate statistical significance.
Results
Characteristics of the decedents are provided in Table 1 according to sex. About 57.8% (weighted, hereafter) of the decedents were female. The mean (SD) age at the time of death was 86.0 (7.9) years for men and 87.0 (11.7) years for women. About 0.9% of the decedent women were centenarians, whereas only about 0.4% of the decedent men were centenarians. Compared with decedent women, decedent men were more likely to have higher proportions of formal education, white collar occupation, economic independence, co-residence with children, and regular exercise, and to be currently married and consuming alcohol. The characteristics among the three subgroups (decedents with interview in the last year of life, 1 to 2 years prior to death, and 2 to 3 years prior to death) did not differ according to sex, ethnicity, residence, and education (all p > 0.05). However, there was a small difference in age at the time of death (86.0, 86.8, and 87.6, respectively, p < 0.001).
Table 1.
Characteristics of Decedents by Sex
| Characteristics | Overalla, N = 23,934 | Men, N = 9,131 | Women, N = 14,803 |
|---|---|---|---|
| Age at death, y | |||
| Mean (standard deviation)b | 86.6 (10.0) | 86.0 (7.9) | 87.0 (11.7) |
| 80–89 | 4,675 (80.1) | 2,323 (84.8) | 2,049 (76.7) |
| 90–99 | 9,417 (19.2) | 4,302 (14.8) | 5,115 (22.5) |
| ≥100 | 9,842 (0.7) | 2,203 (0.4) | 7,639 (0.9) |
| Ethnicity, Hanc | 22,210 (92.8) | 8,504 (93.7) | 13,706 (92.1) |
| Residence, rural | 13,952 (66.5) | 5,179 (66.7) | 8,773 (66.3) |
| ≥1 Years of educationc | 6,563 (33.5) | 5,076 (60.7) | 1,487 (13.6) |
| White collar occupationc | 1,065 (5.0) | 872 (9.4) | 193 (1.7) |
| Economic independence, yesc | 2,936 (15.9) | 2,289 (26.5) | 647 (8.2) |
| Good family economic statusd | 2,522 (13.6) | 1,057 (14.8) | 1,465 (12.7) |
| Adequate medication, yesc | 21,594 (91.8) | 8,339 (91.9) | 13,255 (91.6) |
| Married, yesc | 2,919 (23.7) | 2,387 (39.2) | 532 (12.4) |
| Co-residence with children, yesc | 20,136 (80.3) | 7,579 (82.5) | 12,557 (78.7) |
| Regular exercise, yesc | 4,718 (25.2) | 2,565 (33.3) | 2,153 (19.3) |
| Currently consuming alcohol, yesc | 4,234 (18.9) | 2,404 (29.6) | 1,830 (11.1) |
Note: Values are given as No. (percentages) unless otherwise indicated. No. was based on study samples (unweighted). Percentages were weighted population estimates that had incorporated survey weight variable that was constructed according to population distribution of age, sex, and residence. For 10,819 (weighted percentage, 25.8%) participants who were unable to answer questions for activities of daily living, proxy interviews were conducted with their next of kin.
aOf 23,934 decedents, 916 with missing data on weight variable were excluded for calculating weighted population estimates.
bWeighted population estimates.
cNumbers of missing data ranged from 10 to 206 (150 for ethnicity, 156 for education, 206 for white collar occupation, 10 for economic independence, 22 for adequate medication, 11 for married status, 11 for co-residence with children, 38 for regular exercise, and 44 for currently consuming alcohol)
dThe question about family economic status was asked starting with the 2002 wave. Among the 23,934 analytic participants in this table, 6,710 (28.0%) participants from 1998 wave and 2000 wave were not asked this question in the interview prior to death.
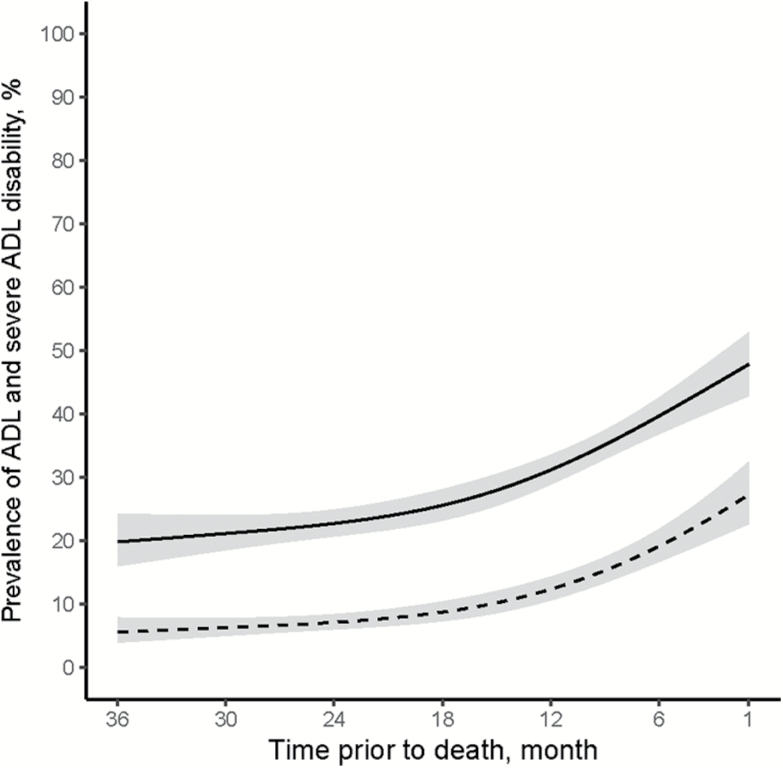
The modeled monthly prevalence of ADL and severe ADL disability during the last 3 years of life is presented in Figure 1. The prevalence of ADL disability increased modestly from 36 months to 24 months prior to death (20% to 23%), more rapidly from 24 months to 12 months before death (23% to 31%), and substantially from 12 months before death to the last month of life (31% to 48%), as shown in Table 2. This pattern was generally consistent for each of the six Katz ADLs, although the prevalence rates differed, with the highest rates observed for bathing disability (Supplementary Figure S2). For severe ADL disability, the prevalence rates were fairly flat from 36 months to 24 months prior to death (6% to 7%) before increasing modestly from 24 months to 12 months before death (7% to 12%), and substantially from 12 months before death to the last month of life (12% to 27%) (Figure 1). For both walking one kilometer and going shopping by oneself, the prevalence of disability increased progressively from 36 months prior to death to the last month prior to death, although the rates were higher for walking than shopping (Supplementary Figure S3).
Figure 1.
Prevalence of ADL (activities of daily living) and severe ADL disability during the last 3 years of life. Solid line represents ADL disability, and dashed line represents severe ADL disability. Gray shading above and below the line represents modeled 95% confidence intervals. Severe ADL disability was defined as needing assistance with three or more ADL tasks. Disability prevalence was modeled as a spline with knots at 30, 16, and 4 months prior to death, adjusting for sociodemographic factors including age at death, sex, race/ethnicity, education, lifetime primary occupation, economic independence, being in receipt of adequate drugs for any illnesses, current marital status, co-residence with adult children, regular exercise, currently consuming alcohol, and calendar time term.
Table 2.
Predicted Prevalence of ADL Disability Prior to Death Across Subgroupsa
| Predicted prevalence, months prior to death, % (95% CI) | ||||||
|---|---|---|---|---|---|---|
| 36 | 24 | 12 | 6 | 1 | p value | |
| Overall | 20 (16 to 24) | 23 (21 to 25) | 31 (29 to 34) | 40 (37 to 43) | 48 (43 to 53) | |
| Age at death, y | ||||||
| 80–89 | 18 (14–22) | 20 (18–23) | 28 (26–31) | 36 (33–40) | 44 (39–50) | Reference |
| 90–99 | 30 (25–36) | 34 (31–36) | 44 (42–46) | 53 (50–56) | 61 (56–66) | <0.001 |
| ≥100 | 47 (39–55) | 52 (46–57) | 62 (57–67) | 70 (65–75) | 77 (71–82) | <0.001 |
| Sex | 0.003 | |||||
| Men | 16 (13–20) | 19 (17–21) | 26 (24–29) | 34 (31–37) | 42 (37–47) | |
| Women | 23 (18–28) | 26 (23–29) | 35 (32–38) | 44 (40–47) | 52 (47–58) | |
| Ethnicity | 0.306 | |||||
| Minority group | 18 (12–26) | 21 (15–28) | 29 (22–37) | 37 (29–46) | 45 (36–55) | |
| Han | 20 (16–24) | 23 (21–25) | 31 (29–34) | 40 (37–43) | 48 (43–53) | |
| Residence | <0.001 | |||||
| Urban | 23 (19–28) | 26 (24–29) | 36 (33–38) | 44 (41–48) | 53 (47–58) | |
| Rural | 18 (15–23) | 21 (19–24) | 29 (26–32) | 37 (34–41) | 45 (40–51) | |
| Years of education | 0.074 | |||||
| 0 | 20 (16–25) | 23 (21–26) | 32 (29–34) | 40 (37–44) | 49 (43–54) | |
| ≥1 | 19 (15–23) | 22 (19–25) | 30 (27–33) | 38 (34–42) | 46 (41–52) | |
| White collar occupation | 0.106 | |||||
| No | 20 (16–24) | 23 (20–25) | 31 (29–33) | 39 (37–42) | 48 (43–53) | |
| Yes | 24 (18–31) | 27 (22–33) | 36 (30–43) | 45 (39–52) | 54 (46–62) | |
| Economic independence | 0.163 | |||||
| No | 20 (16–24) | 22 (20–25) | 31 (28–33) | 39 (36–42) | 47 (42–53) | |
| Yes | 21 (17–27) | 24 (21–28) | 33 (29–37) | 42 (37–47) | 50 (43–56) | |
| Good family economic statusb | 0.336 | |||||
| No | 20 (16–24) | 24 (22–26) | 32 (29–34) | 38 (35–41) | 44 (38–49) | |
| Yes | 18 (14–23) | 21 (18–26) | 28 (24–33) | 34 (29–40) | 40 (33–47) | |
| Adequate medication | 0.028 | |||||
| No | 25 (19–32) | 28 (23–33) | 37 (31–44) | 46 (40–53) | 55 (47–63) | |
| Yes | 19 (16–24) | 22 (20–25) | 31 (28–33) | 39 (36–42) | 47 (42–52) | |
| Married | 0.868 | |||||
| No | 20 (16–25) | 23 (21–26) | 32 (29–34) | 40 (37–43) | 49 (44–54) | |
| Yes | 18 (14–23) | 21 (18–24) | 29 (26–33) | 38 (33–42) | 46 (39–52) | |
| Co-residence with children | <0.001 | |||||
| No | 14 (10–18) | 16 (13–20) | 23 (19–27) | 30 (25–35) | 37 (31–44) | |
| Yes | 22 (17–26) | 25 (23–27) | 33 (31–36) | 42 (36–45) | 51 (45–56) | |
| Regular exercise | <0.001 | |||||
| No | 23 (18–28) | 26 (24–28) | 35 (33–38) | 44 (41–47) | 52 (47–57) | |
| Yes | 13 (10–17) | 15 (12–18) | 21 (18–25) | 28 (24–33) | 35 (30–42) | |
| Currently consuming alcohol | <0.001 | |||||
| No | 22 (18–27) | 25 (23–28) | 34 (32–37) | 43 (40–46) | 51 (46–56) | |
| Yes | 12 (9–16) | 14 (11–17) | 20 (17–24) | 27 (22–31) | 34 (28–40) | |
Note: ADL, activities of daily living.
aDisability prevalence was modeled as a spline with knots at 30, 16, and 4 months prior to death, adjusting for sociodemographic factors including age at death, sex, race/ethnicity, education, lifetime primary occupation, economic independence, being in receipt of adequate drugs for any illnesses, current marital status, co-residence with adult children, regular exercise, and currently consuming alcohol. Prevalence for each subgroup was calculated while adjusting for all other sociodemographic factors in the model.
bThe question about family economic status was asked starting with the 2002 wave. Among the 23,934 analytic participants, 6,710 (28.0%) participants from 1998 wave and 2000 wave were not asked this question in the interview prior to death. These disability estimates were based only on decedents whose family economic status was available.
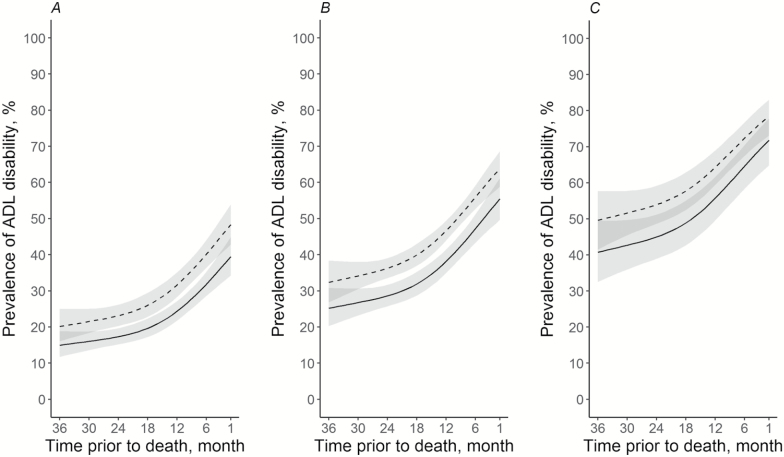
Although the patterns over the 3-year period were comparable for each of the three age groups, the disability rates were lowest for participants who died between 80 and 89 years, intermediate for those who died between 90 and 99 years, and highest for those who died at age 100 or older (Figure 2 and Table 2). At each time point prior to death, a higher percentage of women was disabled than men (Supplementary Figure S4 and Table 2). After accounting for age at death and sex, several other factors were associated with a higher prevalence of disability at each time point during the last 3 years of life, including urban residence, no adequate medication, having co-residence with children, no regular exercise, and not currently consuming alcohol (Table 2).
Figure 2.
Prevalence of ADL (activities of daily living) disability during the last 3 years of life by age at death and sex. (A) age at death 80–89 years; (B) 90–99 years; and (C) ≥100 years. Solid line represents men, and dashed line represents women. Gray shading above and below the line represents modeled 95% confidence intervals. Disability prevalence was modeled as a spline with knots at 30, 16, and 4 months prior to death, adjusting for sociodemographic factors including age at death, sex, race/ethnicity, education, lifetime primary occupation, economic independence, being in receipt of adequate drugs for any illnesses, current marital status, co-residence with adult children, regular exercise, currently consuming alcohol, and calendar time term.
In a series of sensitivity analyses, we found that (i) the results were nearly identical after missing data on sociodemographic factors were imputed; (ii) the prevalence estimates of disability changed little when only decedents from the 2002 to 2011 waves were included; and (iii) the 284 decedents who did not have home-based interview within the last 3 years of life did not differ from our study participants in sex, ethnicity, residence, and education (all p > 0.05), but they were older at the time of death (88.2 vs 86.6 years, p = 0.020).
Discussion
To the best of our knowledge, this is the first study to estimate the likelihood of being disabled prior to death among the oldest-old population in a low- to middle-income country. In a population-based sample of the oldest-old in China, we found that the predicted disability prevalence increased as death approached, with disability present in nearly one-fifth of persons at 36 months before death, nearly a quarter at 24 months before death, nearly one-third at 12 months before death, and nearly one-half in the last month of life. This pattern was generally consistent for severe disability. Disability rates were higher for women than men and were highest for the centenarians. Our findings provide important information on end-of-life disability for the rapidly aging population, and raise concerns about the ability of China and other developing countries to manage the projected tsunami of late-life disability in the coming years.
The pattern of end-of-life disability observed in the current study is consistent with findings reported by the earlier U.S. study, which evaluated disability during the last 2 years of life (6). In both studies, the prevalence of ADL and severe ADL disability increased much more rapidly during the last year of life than during the prior year (i.e., from 24 to 12 months before death). Furthermore, our study revealed a greater prevalence of end-of-life disability in persons who died at age 100 or older, a phenomenon rarely evaluated in previous studies (6–9). Our results suggest that many adults who survive to extremely old age often need assistance with basic activities for a prolonged period of time prior to death (2,3). Given the expected increase in centenarians in the coming years, these results pose enormous challenges for the current health care systems, not only in China but also globally.
The prevalence estimates of late-life disability in the current study are slightly lower than those in the U.S. study. Our findings might be explained by differences in sociopolitical systems (e.g., health care policy), health practices, and cultural setting between China and other countries (20,21). For example, many rural Chinese had to perform labor-intensive farm work until very old age, which might have helped them maintain muscle strength and physical fitness, thereby reducing disability at the end of life (15). In addition, recent studies have demonstrated that the disabling effects of some major diseases (e.g., stroke (22) and cardiometabolic diseases) have declined during the last few decades in China (23,24). Alternatively, the lower prevalence might reflect subtle cultural differences that make it less likely that older Chinese will disclose their illnesses to nonfamily members (25). Finally, the implementation of the new Rural Co-operative Medical Care System in 2000 coupled with policies and benefits targeting the oldest-old citizens since 1995 have made medical care more accessible and affordable to the oldest-old, leading to a lower prevalence of late-life disability (26–28).
Several subgroup-specific results warrant comment. First, women were more likely than men to be disabled at each time point prior to death, a finding that was also reported in the U.S. study (6). Sex differences in chronic conditions, predisposing physiologic factors, and social support may partly explain this gender difference. However, it is important to note that Chinese women generally have less access to medical resources than men and, as a result, may have poorer overall health (29). Second, the prevalence of end-of-life disability in the oldest-old was lower in rural versus urban participants. This difference might be explained by selective attrition due to higher mortality earlier in life and by enhanced fitness from a life of farm work (15). Third, participants who resided with children had a greater prevalence of disability than those who did not. There are at least two possible explanations for this finding: first, participants who were most vulnerable were probably more likely to move in with their children (15); and second, personal assistance with essential daily activities was more readily available for participants living with children. Fourth, it is expected that participants who received adequate medication for any illnesses, exercised regularly, or were currently consuming alcohol had a lower prevalence of disability compared with those who did not. In the Chinese culture, for example, alcohol drinking “is not simply a dietary habit, but a sociocultural ritual, whereby social connections or the so-called Guanxi are built, maintained, and strengthened” (30). Therefore, alcohol-drinking behavior may serve as an indicator of maintenance of social network, which is strongly associated with better outcomes in late life (31).
Our results should inform discussions about the prevention and management of late-life disability among the oldest-old. Although the prevalence of disability was high at the end of life, a sizeable proportion, including nearly a quarter of the oldest-old, maintained their independence before death. These findings support previous studies showing that there is a subset of persons who “escape” common age-associated diseases and live to 100 years with good physical function (32,33). Additional research on these “escapers” is needed to inform the development of programs to prevent disability in the oldest-old. On the other hand, a high proportion of the oldest-old did not “escape” and had to cope with disability in their last years of life. Because older adults with disability might still have a good quality of life (34), families, caregivers, and policy makers should aim to develop and implement strategies that enhance quality of life prior to death in this vulnerable population. For example, bathing might serve as a target for future interventions (e.g., retrofitting of bathrooms) (16) since it was the most commonly disabled activity in the current study.
The availability of high-quality data from the largest nationally representative cohort of the oldest-old in the world provided us with a unique opportunity to estimate the prevalence of disability during the 3 years prior to death. By taking serial cross-sectional snapshots over time, we were simulating a longitudinal study rather than following up an inception cohort prospectively over time. Without more frequent assessments over shorter intervals, it is not possible track individual disability trajectories. Additional longitudinal studies are needed to fully understand the end-of-life disablement process and help inform the development of preventive interventions for disability in this vulnerable population. Because the CLHLS did not provide longitudinal weights, the application of survey weights could lead to biased estimates due to the nonrandom losses to follow-up. In addition, about a quarter of the disability assessments were based on proxy report. In epidemiologic studies, the use of proxy reports is considered preferable to omitting observations when older participants are unable to respond (6,35).
In conclusion, the results from this large nationally representative sample of the oldest-old in China demonstrate a high prevalence of disability during the 3 years prior to death. This prevalence was the greater in women than men and in persons who died at the oldest ages. These results may help the oldest-old, together with their families, caregivers, and policy makers, to make decisions about end-of-life care. Additional strategies will be needed to better address the care needs at the end of life for a rapidly expanding population of disabled older persons worldwide.
Funding
This work was supported by the China National Natural Science Foundation (grant number 81571372). The data used in this study were from the Chinese Longitudinal Healthy Longevity Survey (CLHLS), which is managed by the Center for Healthy Aging and Development Studies, Peking University. The CLHLS was supported by funds from the U.S. National Institutes on Aging (grant number R01AG023627), China National Natural Science Foundation (grant numbers 71233001, 71110107025), China Social Science Foundation, and UNFPA. Dr. Liu is the recipient of a James Hudson Brown–Alexander B. Coxe Fellowship from Yale School of Medicine, and he also received support from the U.S. National Institutes on Aging (grant number U01AG022376). The study was conducted at the Yale Claude D. Pepper Older Americans Independence Center (grant number P30AG021342). Dr. Gill is the recipient of an Academic Leadership Award (grant number K07AG043587) from the National Institute on Aging.
Supplementary Material
Acknowledgments
We thank Drs. Heather Allore, George Agogo, and Darce Costello for their help with the statistical analyses and writing.
Conflict of Interest
None reported.
References
- 1. Fries JF. Aging, natural death, and the compression of morbidity. N Engl J Med. 1980;303:130–135. doi:10.1056/NEJM198007173030304 [DOI] [PubMed] [Google Scholar]
- 2. Gruenberg EM. The failures of success. Milbank Mem Fund Q Health Soc. 1977;55:3–24. doi:10.2307/3349592 [PubMed] [Google Scholar]
- 3. Waidmann T, Bound J, Schoenbaum M. The illusion of failure: trends in the self-reported health of the U.S. elderly. Milbank Q. 1995;73:253–287. doi:10.2307/3350259 [PubMed] [Google Scholar]
- 4. Zeng Y, Feng Q, Hesketh T, Christensen K, Vaupel JW. Survival, disabilities in activities of daily living, and physical and cognitive functioning among the oldest-old in China: a cohort study. Lancet. 2017;389:1619–1629. doi:10.1016/S0140-6736(17)30548-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Robine JM, Michel JP. Looking forward to a general theory on population aging. J Gerontol A Biol Sci Med Sci. 2004;59:M590–M597. doi:10.1093/gerona/59.6.M590 [DOI] [PubMed] [Google Scholar]
- 6. Smith AK, Walter LC, Miao Y, Boscardin WJ, Covinsky KE. Disability during the last two years of life. JAMA Intern Med. 2013;173:1506–1513. doi:10.1001/jamainternmed.2013.8738 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Gill TM, Gahbauer EA, Han L, Allore HG. Trajectories of disability in the last year of life. N Engl J Med. 2010;362:1173–1180. doi:10.1056/NEJMoa0909087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Ferrucci L, Turchi A, Fumagalli S, et al. . Sex-related differences in the length of disability prior to death in older persons. Aging Clin Exp Res. 2003;15:310–314. doi:10.1007/BF03324515 [DOI] [PubMed] [Google Scholar]
- 9. Lunney JR, Lynn J, Foley DJ, Lipson S, Guralnik JM. Patterns of functional decline at the end of life. JAMA. 2003;289:2387–2392. doi:10.1001/jama.289.18.2387 [DOI] [PubMed] [Google Scholar]
- 10. Zeng Y, Poston DLJ, Vlosky DA, Gu D.. Healthy Longevity in China: Demographic, Socioeconomic, and Psychological Dimensions. Dordrecht: Springer Netherlands; 2008. [Google Scholar]
- 11. Zhang X, Dupre ME, Qiu L, Zhou W, Zhao Y, Gu D. Urban-rural differences in the association between access to healthcare and health outcomes among older adults in China. BMC Geriatr. 2017;17:151. doi:10.1186/s12877-017-0538-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Katz S, Ford AB, Moskowitz RW, Jackson BA, Jaffe MW. Studies of illness in the aged. The index of ADL: a standardized measure of biological and psychosocial function. JAMA. 1963;185:914–919. doi:10.1001/jama.1963.03060120024016 [DOI] [PubMed] [Google Scholar]
- 13. Gu D. General data assessment of the Chinese longitudinal healthy longevity survey in 2002. In: Zeng Y, Poston D, Smith J, Vlosky DA, Gu D, eds. Healthy Longevity in China: Demographic, Socioeconomic, and Psychological Dimensions. Dordrecht, Netherlands: Springer; 2008:39–59. [Google Scholar]
- 14. Zeng Y, Vaupel JW, Xiao ZY, Zhang CY, Liu YZ. The Healthy Longevity Survey and the active life expectancy of the oldest old in China. Population: An English Selection. 2001;13:95–116. [Google Scholar]
- 15. Gu D, Zeng Y. Sociodemographic effects on the onset and recovery of ADL disability among Chinese oldest-old. 2004;11:1–42. doi:10.4054/DemRes.2004.11.1 [Google Scholar]
- 16. Fong JH, Feng J. Patterns of functional disability in the oldest adults in China. J Am Geriatr Soc. 2016;64:1890–1894. doi:10.1111/jgs.14264 [DOI] [PubMed] [Google Scholar]
- 17. Dupre ME, Gu D, Warner DF, Yi Z. Frailty and type of death among older adults in China: prospective cohort study. BMJ. 2009;338:b1175. doi:10.1136/bmj.b1175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Gu D, Dupre ME, Sautter J, Zhu H, Liu Y, Yi Z. Frailty and mortality among Chinese at advanced ages. J Gerontol B Psychol Sci Soc Sci. 2009;64:279–289. doi:10.1093/geronb/gbn009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Harrell FE. Regression Modeling Strategies: With Applications to Linear Models, Logistic Regression, and Survival Analysis. New York: Springer-Verlag; 2001. [Google Scholar]
- 20. Fung HH. Aging in culture. Gerontologist. 2013;53:369–377. doi:10.1093/geront/gnt024 [DOI] [PubMed] [Google Scholar]
- 21. Chen YC. Chinese values, health and nursing. J Adv Nurs. 2001;36:270–273. doi:10.1046/j.1365-2648.2001.01968.x [DOI] [PubMed] [Google Scholar]
- 22. Sousa RM, Ferri CP, Acosta D, et al. . Contribution of chronic diseases to disability in elderly people in countries with low and middle incomes: a 10/66 Dementia Research Group population-based survey. Lancet. 2009;374:1821–1830. doi:10.1016/S0140-6736(09)61829-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Yang G, Wang Y, Zeng Y, et al. . Rapid health transition in China, 1990–2010: findings from the Global Burden of Disease Study 2010. Lancet. 2013;381:1987–2015. doi:10.1016/S0140-6736(13)61097-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Liang Y, Song A, Du S, Guralnik JM, Qiu C. Trends in disability in activities of daily living among Chinese older adults, 1997–2006: the China Health and Nutrition Survey. J Gerontol A Biol Sci Med Sci. 2015;70:739–745. doi:10.1093/gerona/glu204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Searight HR, Gafford J. Cultural diversity at the end of life: issues and guidelines for family physicians. Am Fam Physician. 2005;71:515–522. [PubMed] [Google Scholar]
- 26. Wagstaff A, Lindelow M, Jun G, Ling X, Juncheng Q. Extending health insurance to the rural population: an impact evaluation of China’s new cooperative medical scheme. J Health Econ. 2009;28:1–19. doi:10.1016/j.jhealeco.2008.10.007 [DOI] [PubMed] [Google Scholar]
- 27. Jiang Q, Yang S, Sanchez-Barricarte JJ. Can China afford rapid aging?Springerplus. 2016;5:1107. doi:10.1186/s40064-016-2778-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Guo J. Avenue Less Than Expenditure in Old Age Pension in 22 Provinces. China Business New; 2015. http://www.yicai.com/news/2015/11/4715255.html [Google Scholar]
- 29. Yi Z, Yuzhi L, George LK. Gender differentials of the oldest old in China. Research on Aging. 2003;25:65–80. doi:10.1177/0164027502238343 [Google Scholar]
- 30. Feng Q, Son J, Zeng Y. Prevalence and correlates of successful ageing: a comparative study between China and South Korea. Eur J Ageing. 2015;12:83–94. doi:10.1007/s10433-014-0329-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Gu D, Feng Q, Sautter J. Social network types, intimacy and healthy longevity among the Chinese elderly. In: Garner JB, Christiansen TC, eds. Social Sciences in Health Care and Medicine. New York: Nova Science Publishers; 2008:11–49. [Google Scholar]
- 32. Evert J, Lawler E, Bogan H, Perls T. Morbidity profiles of centenarians: survivors, delayers, and escapers. J Gerontol A Biol Sci Med Sci. 2003;58:232–237. doi:10.1093/gerona/58.3.M232 [DOI] [PubMed] [Google Scholar]
- 33. Gondo Y, Hirose N, Arai Y, et al. . Functional status of centenarians in Tokyo, Japan: developing better phenotypes of exceptional longevity. J Gerontol A Biol Sci Med Sci. 2006;61:305–310. doi:10.1093/gerona/61.3.305 [DOI] [PubMed] [Google Scholar]
- 34. King J, Yourman L, Ahalt C, et al. . Quality of life in late-life disability: “I don’t feel bitter because I am in a wheelchair”. J Am Geriatr Soc. 2012;60:569–576. doi:10.1111/j.1532-5415.2011.03844.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Long K, Sudha S, Mutran EJ. Elder-proxy agreement concerning the functional status and medical history of the older person: the impact of caregiver burden and depressive symptomatology. J Am Geriatr Soc. 1998;46:1103–1111. doi:10.1111/j.1532–5415.1998.tb06648.x [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.