Abstract
Background
The benefits of physical activity (PA) for health have primarily been evaluated during midlife. Whether patterns of change in late-life PA associate with overall and cause-specific mortality remains unclear.
Methods
We examined the association between PA trajectories and subsequent mortality among 3,767 men aged ≥65 years. Men self-reported PA using the Physical Activity Scale for the Elderly (PASE) at up to four time points from 2000 through 2009 (Year 7); mortality was assessed over an average of 7.1 years after the Year 7 contact. Group-based trajectory modeling identified patterns of PA change. Cox proportional hazards models described associations between patterns of change in PA, Year 7 PA, and subsequent mortality risk.
Results
Three discrete PA patterns were identified, all with declining PA. Compared to low-activity declining men, moderate (hazard ratio [HR] = 0.78; 95% confidence interval [CI]: 0.70, 0.88) and high-activity (HR = 0.69, 95% CI: 0.57, 0.83) declining groups were associated with lower risk of all-cause mortality. Among models with a single time point, the last time point (Year 7 PA score) was a strong predictor of mortality with HR = 0.85 (95% CI: 0.78, 0.93) per SD increase in PASE score. PA patterns were not a risk factor for mortality after adjustment for the Year 7 PA score.
Conclusions
Recent PA levels are a stronger indicator of subsequent mortality risk than PA patterns reported over the prior 7 years or prior PA level, suggesting that current PA rather than history of PA is the most relevant parameter in clinical settings.
Keywords: Physical activity, Patterns, Mortality, Older men
The benefits of physical activity (PA) for health are well established (1–5). Previous studies linking higher PA with lower risk of mortality among older men and women have largely considered PA at a single point in time (6–10). Some studies have examined the association between patterns of change in late-life PA and overall and cause-specific mortality, but with varying methodology. Several of these studies have approached identification of patterns of change using a categorical analysis with clinical cut-points distinguishing those who maintain levels of PA (low or high) from those who change PA levels (increase or decrease) (11–13), while others have used different approaches to examine patterns of PA change as a predictor (14,15). Data-driven methods such as latent class analysis or group-based trajectory models may also be used to identify relevant subgroups for a given population (16,17). We have previously identified novel patterns of PA change in a longitudinal study of older men using group-based trajectory models (18); however, these groups were largely determined by initial PA level and thus are qualitatively different than previously identified groups. The purpose of the current study is to determine the association between patterns of PA change over time and subsequent mortality among older men, and whether the association between patterns and mortality is independent of final level of PA. We hypothesized there would be a strong link between patterns of PA change over time and subsequent mortality, but that this association would at least partially depend on the final level of PA.
Methods
Study Population
We studied participants enrolled in the Osteoporotic Fractures in Men (MrOS) Study, a prospective cohort study of community-dwelling older men. From 2000–2002, 5,994 community-dwelling men ≥65 years old were recruited from six geographic areas of the United States (19,20). Men with bilateral hip replacements and men who were unable to walk without the assistance of another person were not eligible for the study.
PA Measurements
PA was assessed by self-report using the Physical Activity Scale for the Elderly (PASE) questionnaire which ascertains the intensity, frequency, and duration of a variety of activities over a period of 7 days. The PASE questionnaire includes walking; strenuous, moderate, and light sports; muscle strength and endurance; occupational activities, including standing or walking; lawn work and gardening; caring for another person; home repairs; and heavy and light housework. The frequency and duration of each activity was multiplied by an empirically derived item weight and summed to compute the total PASE score. PASE scores have no units and provide a relative rather than absolute measure of PA levels. PASE has been previously validated with objective measures of PA and has high test–retest reliability (21). We used data from following study contacts: Baseline visit (2000–2002), Year 3.5 visit (sleep sub-study in selected participants, 2003–2005), the Year 5 visit (all participants, 2005–2006), and Year 7 visit (all participants, 2007–2009). Men who returned to the Year 7 visit and completed a PASE questionnaire at least one of the above study contacts were included in PA trajectory analysis (N = 4,681).
Analysis sample
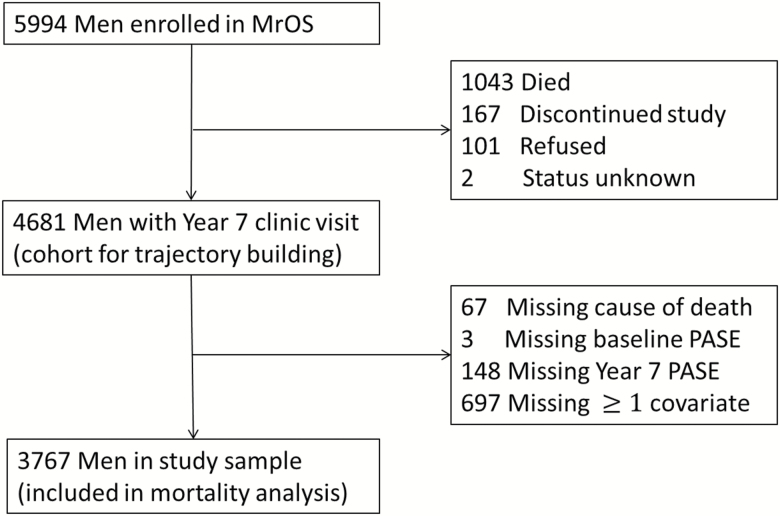
The analyses included those who had non-missing PASE score and covariates at the Year 7 visit and had vital status assessment after that visit (n = 3,767). Complete study flow diagram is shown in Figure 1.
Figure 1.
Flow chart describing Osteoporotic Fractures in Men (MrOS) Study sample subject characteristics using the 4,681 for physical activity (PA) trajectory building, and the final n = 3,767 for non-missing values of adjusted covariates used in the final multivariate model for mortality risk.
Mortality
Participants were contacted every 4 months after the Year 7 visit, and all reported deaths were confirmed with death certificates and additionally with discharge summaries when available. The average follow-up time for the 3,767 men in the cohort was 7.1 ± 2.5 years. Underlying cause of mortality was centrally adjudicated and grouped into three basic categories: cardiovascular disease (CVD), cancer, and other (non-CVD non-cancer).
Other Covariates
At baseline, participants reported their age, race/ethnicity, education, marital status, smoking status, alcohol use, self-rated health status, depression (Geriatric Depression Scale [GDS] score), and cognitive function (Teng 3MS). Participants were asked to self-report a number of medical conditions, including cancer, congestive heart failure, myocardial infarction, chronic obstructive pulmonary disease, diabetes, and osteoporosis. Weight was measured on a balance beam or digital scale, and height by wall-mounted stadiometers. Body mass index (BMI) was calculated as weight (kg)/height2 (m2).
Statistical Methods
Group-based trajectory modeling was applied using PROC TRAJ in SAS to the repeated PA scores (PASE score). Group-based trajectory modeling assumes that the population contains an unspecified number of groups, each with a different probability of following a longitudinal sequence (e.g., trajectory or pattern) for the dependent variable. Men who returned to the Year 7 visit, and who had completed at least one PASE questionnaire during the assessment period (baseline-Year 7 Visit), were included in the trajectory models. We compared models with different numbers of groups (minimum = 3) using two times the change in the Bayesian Information Criterion (2DBIC); values of 10 or greater were considered evidence of better fit. We also assessed models to ensure adequate sample size in each subgroup for assessing the risk of subsequent mortality. For generalizability, we only included specific groups comprised of at least 1% of the analytic cohort. Thus, the final analytic model included three PA groups.
Probabilities in each group were calculated. We plotted the mean estimated PASE score by age along with plots of individual values against the overall trajectory to visually confirm that trajectory analysis successfully grouped men with similar longitudinal patterns. We used Cox proportional hazards models to determine the association between the patterns of PA change and risk of all-cause and cause-specific (CVD, cancer, non-CVD non-cancer) mortality. The proportional hazards assumption was not violated for all mortality outcomes.
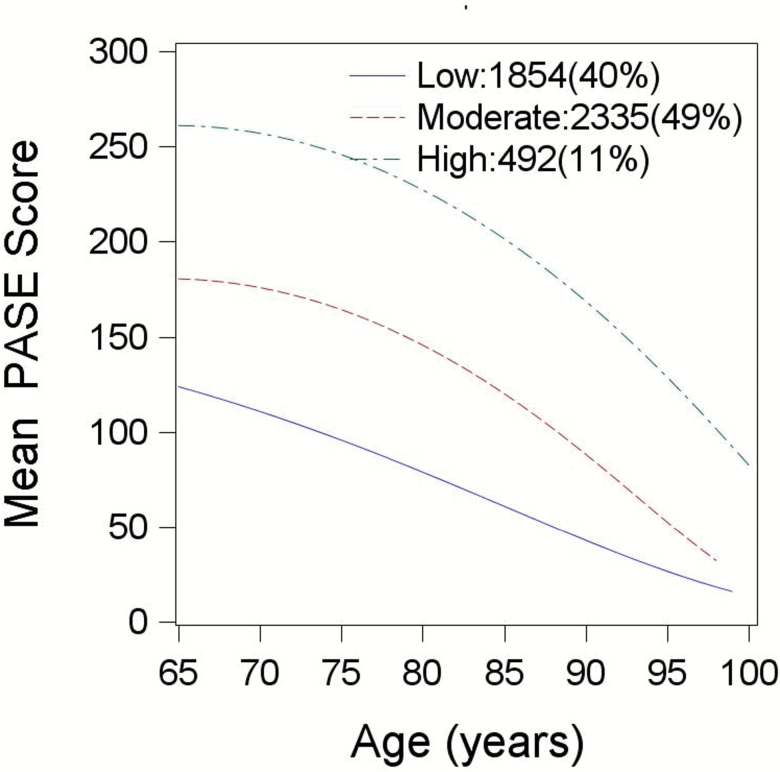
Characteristics of the participants were summarized by means and SD for continuous variables, and counts and percentages for categorical variables. Covariates at the Year 7 visit were selected a priori. Multivariate trajectory models were adjusted for base model, alcoholic use, depression (GDS score), cognitive function (Teng 3MS), marital status, education, self-rated health, at least one co-morbidity (yes/no), smoking status, and BMI (Figure 2).
Figure 2.
Physical activity (PA) trajectories by age; total N = 4,681 men who were alive at Year 7 visit and contributed at least one Physical Activity Scale for the Elderly (PASE) score measure during the PA assessment period (baseline to Year 7 visit).
All analysis was performed using SAS 9.4.
Results
Three discrete patterns of PA change, all of declining PA (PASE score) were identified in this cohort, based primarily on mean PA levels over time: low-activity declining (n = 1,399), moderate-activity declining (n = 1,938), and high-activity declining (n = 430), representing 37.1%, 51.4%, and 11.4%, of the total sample, respectively. There was a decline over time in PA for each of the three patterns of PA change (Figure 2). Body weight, BMI, depressive symptoms, and prevalence of comorbidities varied by patterns of PA change (p < .001; Table 1).
Table 1.
Characteristics by Physical Activity Trajectory in 3,767 MrOS Men at Year 7 Visit
| Cohort (n = 3,767) | Low-Activity Declining (n = 1,854) | Moderate-Activity Declining (n = 2,335) | High-Activity Declining (n = 492) | p Valuea | |
|---|---|---|---|---|---|
| Age (years) | 79.24 ± 5.2 | 78.8 ± 5.1 | 79.4 ± 5.12 | 79.93 ± 5.72 | <.0001 |
| Weight (kg) | 81.46 ± 13.4 | 83.62 ± 14.74 | 80.42 ± 12.33 | 79.11 ± 12.5 | <.0001 |
| Height (cm) | 173.17 ± 6.83 | 173.58 ± 7.12 | 172.99 ± 6.69 | 172.62 ± 6.44 | .01 |
| Body mass index (kg/m2) | 27.12 ± 3.91 | 27.71 ± 4.36 | 26.83 ± 3.53 | 26.51 ± 3.72 | <.0001 |
| Caucasian | 3,405 (90.39) | 1,247 (89.14) | 1,766 (91.12) | 392 (91.16) | .13 |
| College education | 2,125 (56.41) | 806 (57.61) | 1,082 (55.83) | 237 (55.12) | .50 |
| Married | 3,197 (84.87) | 1,156 (82.63) | 1,674 (86.38) | 367 (85.35) | .01 |
| Alcohol (<1 drink/wk) | 1,398 (37.11) | 562 (40.17) | 681 (35.14) | 155 (36.05) | .06 |
| Alcohol (1–5 drinks/wk) | 992 (26.33) | 348 (24.87) | 526 (27.14) | 118 (27.44) | |
| Alcohol (6+ drinks/wk) | 1,377 (36.55) | 489 (34.95) | 731 (37.72) | 157 (36.51) | |
| Current smoking | 73 (1.94) | 26 (1.86) | 42 (2.17) | 5 (1.16) | .38 |
| At least one comorbidityb | 1,524 (40.46) | 689 (49.25) | 710 (36.64) | 125 (29.07) | <.0001 |
| Self-reported health status | 3,214 (85.32) | 1,086 (77.63) | 1,723 (88.91) | 405 (94.19) | <.0001 |
| GDS depression (0–15) | 1.92 ± 2.21 | 2.53 ± 2.54 | 1.64 ± 1.95 | 1.2 ± 1.7 | <.0001 |
| Teng 3 MMS score | 91.94 ± 7.18 | 91.28 ± 8.09 | 92.43 ± 6.43 | 91.93 ± 7.11 | .001 |
| PASE score | 130.53 ± 68.72 | 78.17 ± 42.83 | 146.55 ± 50.56 | 228.68 ± 64.67 | <.0001 |
| All-cause mortality | 1,435 (38.09) | 609 (43.53) | 681 (35.14) | 145 (33.72) | <.0001 |
| CVD mortality | 484 (12.85) | 202 (14.44) | 235 (12.13) | 47 (10.93) | .07 |
| Cancer mortality | 343 (9.11) | 136 (9.72) | 166 (8.57) | 41 (9.53) | .49 |
| Non-CVD/cancer mortality | 608 (16.14) | 271 (19.37) | 280 (14.45) | 57 (13.26) | .0002 |
Notes: 3 MMS = Modified Mini-Mental State; CVD = cardiovascular disease; GDS = Geriatric Depression Scale; MrOS = Osteoporotic Fractures in Men Study; PASE = Physical Activity Scale for the Elderly.
a p Values indicate the overall difference among physical activity trajectories, calculated using chi-squared tests for categorical variables and analysis of variance for continuous variables.
bComorbidities: chronic obstructive pulmonary disease, stroke, myocardial infarction, congestive heart failure, Parkinson’s, and diabetes.
Men in the high-activity declining PA trajectory had the lowest unadjusted mortality rate (45 per 1,000 person year, PY) and those in the moderate-activity declining trajectory had similar mortality (48 per 1,000 PY), while those in the low-activity declining trajectory had the highest mortality (64 per 1,000 PY).
Patterns of PA change were associated with mortality in both the minimally adjusted model (adjusted for age, race, and clinic site) and fully adjusted model, although there was substantial attenuation between the base and fully adjusted models (Table 2). Compared to men in the low activity-declining group, men in the moderate-activity declining and high-activity declining groups had a lower risk of all-cause mortality in both the unadjusted and adjusted models. Similarly, patterns of PA change were also associated with CVD and non-CVD/non-cancer mortality. Patterns of PA change were associated with cancer mortality in the base model, but not in the full multivariate model.
Table 2.
The Association Between Physical Activity Trajectories and All-Cause/Cause-Specific Mortality Without/With Adjustment for Final Physical Activity Measure (n = 3,767)a
| Hazard Ratio (95% CI) | Predictor | Baseb Model | Multivariatec Model | Baseb Model w/ Final PA | Multivariatec Model w/ Final PA |
|---|---|---|---|---|---|
| Deaths (all-cause) | Low-activity declining | Referent | Referent | Referent | Referent |
| Moderate-activity declining | 0.66 (0.59, 0.74) | 0.78 (0.70, 0.88) | 0.87 (0.76, 0.99) | 0.91 (0.79, 1.04) | |
| High-activity declining | 0.56 (0.47, 0.68) | 0.69 (0.57, 0.83) | 1.02 (0.79, 1.32) | 0.96 (0.74, 1.23) | |
| p trend | <.00001 | <.00001 | .36 | .38 | |
| Year 7 PASE score | NA | NA | 0.76 (0.70, 0.83) | 0.85 (0.78, 0.93) | |
| CVD deaths | Low-activity declining | Referent | Referent | Referent | Referent |
| Moderate-activity declining | 0.67 (0.55, 0.81) | 0.81 (0.66, 0.99) | 0.86 (0.68, 1.09) | 0.92 (0.72, 1.16) | |
| High-activity declining | 0.54 (0.39, 0.74) | 0.68 (0.49, 0.95) | 0.94 (0.60, 1.48) | 0.90 (0.58, 1.40) | |
| p trend | <.00001 | .0002 | .4336 | .5201 | |
| Year 7 PASE score | NA | NA | 0.77 (0.67, 0.90) | 0.87 (0.76, 1.01) | |
| Cancer deaths | Low-activity declining | Referent | Referent | Referent | Referent |
| Moderate-activity declining | 0.76 (0.60, 0.95) | 0.79 (0.63, 1.01) | 0.97 (0.73, 1.28) | 0.97 (0.73, 1.29) | |
| High-activity declining | 0.77 (0.54, 1.10) | 0.82 (0.55, 1.19) | 1.32 (0.79, 2.18) | 1.29 (0.78, 2.15) | |
| p trend | .0349 | .1161 | .5540 | .5661 | |
| Year 7 PASE score | NA | NA | 0.78 (0.66, 0.93) | 0.81 (0.68, 0.96) | |
| Non-CVD non-cancer deaths | Low-activity declining | Referent | Referent | Referent | Referent |
| Moderate-activity declining | 0.60 (0.51, 0.71) | 0.75 (0.63, 0.89) | 0.82 (0.66, 1.01) | 0.85 (0.69, 1.05) | |
| High-activity declining | 0.48 (0.36, 0.64) | 0.61 (0.45, 0.82) | 0.93 (0.62, 1.39) | 0.80 (0.54, 1.18) | |
| p trend | <.00001 | .0001 | .2328 | .1504 | |
| Year 7 PASE score | NA | NA | 0.74 (0.64, 0.84) | 0.87 (0.76, 0.99) |
Notes: Boldface indicates p <.05. CI = confidence interval; CVD = cardiovascular disease; NA = not available; PA = physical activity; PASE = Physical Activity Scale for the Elderly.
aThe final physical activity measure (of the trajectories) was the Year 7 PASE score.
bBase trajectory models adjusted for age, race, and clinic site.
cMultivariate trajectory models adjusted for base covariates and alcohol use, depression (Geriatric Depression Scale score), cognitive function (Teng 3MS), marital status, education, self-rated health, at least one co-morbidity defined categorically (yes/no; chronic obstructive pulmonary disease, stroke, myocardial infarction, congestive heart failure, Parkinson’s, diabetes), smoking status, and body mass index.
We also considered the association between trajectories and mortality after adjusting for final (Year 7 visit) PASE score. In these models, higher Year 7 PASE score was associated with lower all-cause mortality. Furthermore, inclusion of the Year 7 PASE score in the models resulted in an attenuation between the patterns of PA change and all mortality so that there was no statistically significant associations between patterns of change and all-cause or cause-specific mortality.
In order to assess time dependence over the period used to define the trajectories, we also compared models using single time point assessments of PA at the beginning and end of the trajectories, without including patterns of PA change in the model. The association between PA at a given time point varied with time-gap between assessment and outcome, with the weakest (statistically nonsignificant) association occurring for the initial baseline PASE score and strongest association occurring for Year 7 PA or the last time point in the trajectory. In fully adjusted models, the hazard ratio for all-cause mortality was 1.01 (95% confidence interval [CI]: 0.96, 1.07) per SD increase in baseline PASE score and 0.83 (95% CI: 0.78, 0.88) per SD increase in Year 7 PASE score.
Discussion
In this large cohort of older men, patterns of PA change were associated with subsequent mortality; men in trajectories with higher levels of PA (high-activity and moderate-activity declining) had lower mortality than the men in the low-activity declining trajectory group. However, in models including both the patterns of change and the Year 7 PA measure, it was the Year 7 measure that was a predictor of subsequent mortality, while the associations between patterns of PA change and mortality were attenuated and no longer significant. In particular, we note that current PA level, rather than previous PA level or patterns of PA change, is the relevant risk factor for assessing mortality risk in older men. The clinical ramifications of these findings support assessing activity levels to determine health status and messaging that encourages PA among older men irrespective of prior levels of activity. Importantly, the practical use of the most recent PA data provides clinicians and gerontologists the necessary guidance to initiate late-life prevention strategies that encourage PA for reduced mortality risk in older, vulnerable populations, notably among those with history of low-declining PA.
In the present study, three discrete patterns of PA change were identified in this cohort of older men, PA levels declined across all three PA trajectories, consistent with national PA trends of older adults (22). Our findings contrast with previous studies which have identified subgroups with qualitatively distinct PA trajectories (increasing, stable, decreasing) (16,17). In this study population, group-based trajectory analysis did not identify subgroups with qualitatively different rates of change over time, suggesting that PA levels among older men are substantially but not completely determined by their previous level of PA, since the groups selected differed primarily by overall level of PA rather than change variables. The methodology used finds dominant patterns of PA over time, but it does not preclude individual variability in PA patterns and may lead to over-grouping with significant variation within PA trajectories.
Our findings regarding PA trajectories and mortality cannot not be directly compared to the previous literature due to the particular subgroups identified using the group-based trajectory models and other methodological differences. We note, however, that the results in this paper are largely consistent with previous studies. Higher levels of PA are in general associated with lower mortality after adjustment for confounders (6–10), and this was observed for the identified trajectories in this study, as well as the single measure of PA at Year 7. Talbot and coworkers analyzed patterns of leisure time activity in the Baltimore Longitudinal Study of Aging using mixed effects models and found that greater longitudinal declines in total and high intensity activity were predictors of all-cause mortality (15). Bembom and coworkers analyzed PA in a group of older men and women from Sonoma county using marginal structural models and found that risk of increased risk of mortality associated with low PA was independent of underlying CVD and history of activity (14).
Studies using clinical cut-points to identify subgroups with varying PA trajectories (stable low, stable high, increasing, decreasing) have shown that PA levels at earlier times matter less than PA levels at later time points and in particular that prior high PA level does not appear to mitigate risk among those who are sedentary (11–13). Using a longitudinal cohort of older men, Stessman and coworkers reported that continuing activity as well as initiating PA at age 85 years was associated with delayed functional loss and better survival (11). Another study in older Australian men using a different and more stringent cutoff for activity found that the health advantages of activity were no longer present for those who changed from active to inactive (12). Finally a study among older women found that all-cause mortality and cardiovascular mortality was associated with the most recent PA levels, but not the initial point (13). Furthermore, the benefit of increasing PA did not extend beyond age 75 or among those with poor health status. Notably, the same paper showed a different pattern for cancer mortality, indicating that longitudinal trajectories were more important for this outcome, which contrasts findings from the present study. A positive effect on survival associated with recent PA levels has similarly been shown among participants in their early 70s in both the British Heart Study (23) and the Zutphen Elderly Study (24).
Strengths and Limitations
The strengths of the present study are large sample size and sufficient follow-up to detect group level differences in all-cause and cause-specific mortality, systematic adjudication of outcomes, repeated measures of PA using a common instrument, and inclusion of many potential confounders. Study limitations include the observational design, with potential for selection bias and residual confounding (e.g., severity of comorbid conditions). In our study, men in the low-declining PA trajectory weighed significantly more, had a higher prevalence of one or more comorbid conditions, and had higher depression scores, and thus would be expected to have higher mortality. Our models included these variables, but residual confounding and subclinical declines concurrent with the trajectory model period could account for some of the observed relationships. PA and underlying health status have a strong bi-directional relationship, and thus it is unclear from this study design to what extent PA or change in PA merely reflects health status and to what extent PA has a causal impact on health status. Survival cohort bias with selective mortality of high-risk individuals may have attenuated the association between baseline PASE score and mortality after the Year 7 visit. Nonetheless, these data are consistent with the hypothesis that maintaining higher PA levels during aging may attenuate mortality associated with modifiable chronic-diseases. The generalizability of the present study is limited since the source cohort is all male, mostly non-Hispanic white, and community-dwelling.
Conclusion
Recent PA levels are a stronger indicator of subsequent mortality risk than PA patterns reported over the prior 7 years or prior PA level, suggesting that current PA rather than history of PA is the most relevant parameter in clinical settings.
Funding
The Osteoporotic Fractures in Men (MrOS) Study is supported by National Institutes of Health funding. The following institutes provided support: the National Institute on Aging (NIA); the National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS); the National Center for Advancing Translational Sciences (NCATS); and NIH Roadmap for Medical Research (grant numbers U01 AG027810, U01 AG042124, U01 AG042139, U01 AG042140, U01 AG042143, U01 AG042145, U01 AG042168, U01 AR066160, and UL1 TR000128).
Acknowledgments
This manuscript is the result of work supported with resources and use of facilities of the Minneapolis VA Health Care System. The contents do not represent the views of the U.S. Department of Veterans Affairs or the U.S. Government.
Conflict of Interest
The authors declare no conflicts of interest and there is nothing to disclose by any of the authors. However, we would like to note that co-author, P. M. Cawthon serves on journal editorial board.
References
- 1. Li J, Siegrist J. Physical activity and risk of cardiovascular disease—a meta-analysis of prospective cohort studies. Int J Environ Res Public Health. 2012;9:391–407. doi:10.3390/ijerph9020391 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Brown JC, Winters-Stone K, Lee A, Schmitz KH. Cancer, physical activity, and exercise. Compr Physiol. 2012;2:2775–2809. doi:10.1002/cphy.c120005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Paterson DH, Warburton DE. Physical activity and functional limitations in older adults: a systematic review related to Canada’s Physical Activity Guidelines. Int J Behav Nutr Phys Act. 2010;7:38. doi:10.1186/1479-5868-7-38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Cauley JA, Harrison SL, Cawthon PM, et al. Objective measures of physical activity, fractures and falls: the Osteoporotic Fractures in Men Study. J Am Geriatr Soc. 2013;61:1080–1088. doi:10.1111/jgs.12326 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Cawthon PM, Blackwell TL, Cauley JA, et al. Objective assessment of activity, energy expenditure, and functional limitations in older men: the Osteoporotic Fractures in Men Study. J Gerontol A Biol Sci Med Sci. 2013;68:1518–1524. doi:10.1093/gerona/glt054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Arem H, Moore SC, Patel A, et al. Leisure time physical activity and mortality: a detailed pooled analysis of the dose-response relationship. JAMA Intern Med. 2015;175:959–967. doi:10.1001/jamainternmed.2015.0533 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Gebel K, Ding D, Chey T, Stamatakis E, Brown WJ, Bauman AE. Effect of moderate to vigorous physical activity on all-cause mortality in middle-aged and older Australians. JAMA Intern Med. 2015;175:970–977. doi:10.1001/jamainternmed.2015.0541 [DOI] [PubMed] [Google Scholar]
- 8. Hirsch CH, Diehr P, Newman AB, et al. Physical activity and years of healthy life in older adults: results from the cardiovascular health study. J Aging Phys Act. 2010;18:313–334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Moore SC, Patel AV, Matthews CE, et al. Leisure time physical activity of moderate to vigorous intensity and mortality: a large pooled cohort analysis. PLoS Med. 2012;9:e1001335. doi:10.1371/journal.pmed.1001335 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Paganini-Hill A, Kawas CH, Corrada MM. Activities and mortality in the elderly: the leisure world cohort study. J Gerontol A Biol Sci Med Sci. 2011;66:559–567. doi:10.1093/gerona/glq237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Stessman J, Hammerman-Rozenberg R, Cohen A, Ein-Mor E, Jacobs JM. Physical activity, function, and longevity among the very old. Arch Intern Med. 2009;169:1476–1483. doi:10.1001/archinternmed.2009.248 [DOI] [PubMed] [Google Scholar]
- 12. Almeida OP, Khan KM, Hankey GJ, Yeap BB, Golledge J, Flicker L. 150 minutes of vigorous physical activity per week predicts survival and successful ageing: a population-based 11-year longitudinal study of 12 201 older Australian men. Br J Sports Med. 2014;48:220–225. doi:10.1136/bjsports-2013-092814 [DOI] [PubMed] [Google Scholar]
- 13. Gregg EW, Cauley JA, Stone K, et al. ; Study of Osteoporotic Fractures Research Group Relationship of changes in physical activity and mortality among older women. JAMA. 2003;289:2379–2386. doi:10.1001/jama.289.18.2379 [DOI] [PubMed] [Google Scholar]
- 14. Bembom O, van der Laan M, Haight T, Tager I. Leisure-time physical activity and all-cause mortality in an elderly cohort. Epidemiology. 2009;20:424–430. doi:10.1097/EDE.0b013e31819e3f28 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Talbot LA, Morrell CH, Fleg JL, Metter EJ. Changes in leisure time physical activity and risk of all-cause mortality in men and women: the Baltimore Longitudinal Study of Aging. Prev Med. 2007;45:169–176. doi:10.1016/j.ypmed.2007.05.014 [DOI] [PubMed] [Google Scholar]
- 16. Barnett TA, Gauvin L, Craig CL, Katzmarzyk PT. Distinct trajectories of leisure time physical activity and predictors of trajectory class membership: a 22 year cohort study. Int J Behav Nutr Phys Act. 2008;5:57. doi:10.1186/1479-5868-5-57 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Pan LY, Hsu HC, Chang WC, Luh DL. Trajectories of physical activity and risk factors among Taiwanese older adults. Int J Behav Med. 2015;22:62–69. doi:10.1007/s12529-014-9409-3 [DOI] [PubMed] [Google Scholar]
- 18. Laddu DR, Cawthon PM, Parimi N, et al. ; Osteoporotic Fractures in Men Study Research Group Trajectories of the relationships of physical activity with body composition changes in older men: the MrOS study. BMC Geriatr. 2017;17:119. doi:10.1186/s12877-017-0506-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Blank JB, Cawthon PM, Carrion-Petersen ML, et al. Overview of recruitment for the Osteoporotic Fractures in Men Study (MrOS). Contemp Clin Trials. 2005;26:557–568. doi:10.1016/j.cct.2005.05.005 [DOI] [PubMed] [Google Scholar]
- 20. Orwoll E, Blank JB, Barrett-Connor E, et al. Design and baseline characteristics of the Osteoporotic Fractures in Men (MrOS) Study—a large observational study of the determinants of fracture in older men. Contemp Clin Trials. 2005;26:569–585. doi:10.1016/j.cct.2005.05.006 [DOI] [PubMed] [Google Scholar]
- 21. Dinger MK, Oman RF, Taylor EL, Vesely SK, Able J. Stability and convergent validity of the Physical Activity Scale for the Elderly (PASE). J Sports Med Phys Fitness. 2004;44:186–192. [PubMed] [Google Scholar]
- 22. Keadle SK, McKinnon R, Graubard BI, Troiano RP. Prevalence and trends in physical activity among older adults in the United States: a comparison across three national surveys. Prev Med. 2016;89:37–43. doi:10.1016/j.ypmed.2016.05.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Wannamethee SG, Shaper AG, Walker M. Changes in physical activity, mortality, and incidence of coronary heart disease in older men. Lancet. 1998;351:1603–1608. doi:10.1016/S0140-6736(97)12355-8 [DOI] [PubMed] [Google Scholar]
- 24. Bijnen FC, Feskens EJ, Caspersen CJ, Nagelkerke N, Mosterd WL, Kromhout D. Baseline and previous physical activity in relation to mortality in elderly men: the Zutphen Elderly Study. Am J Epidemiol. 1999;150:1289–1296. [DOI] [PubMed] [Google Scholar]